Laying Open and Curettage under Local Anesthesia to Treat Pilonidal Sinus: Long-Term Follow-Up in 111 Consecutively Operated Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
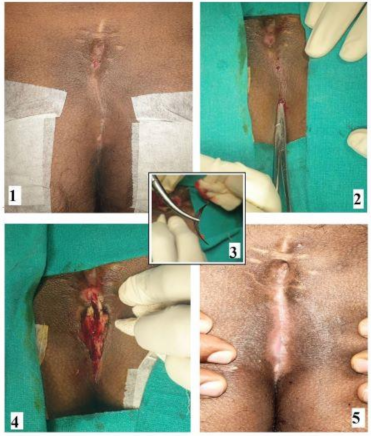
2.2. Surgical Procedure
2.3. Follow-Up
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hodges, R.M. Pilonidal sinus. Boston Med. Surg. J. 1880, 103, 485–486. [Google Scholar] [CrossRef]
- Jensen, S.L.; Harling, H. Prognosis after simple incision and drainage for a first-episode acute pilonidal abscess. Br. J. Surg. 1988, 75, 60–61. [Google Scholar] [CrossRef]
- Testini, M.; Piccinni, G.; Miniello, S.; Di Venere, B.; Lissidini, G.; Nicolardi, V.; Bonomo, G.M. Treatment of chronic pilonidal sinus with local anaesthesia: A randomized trial of closed compared with open technique. Colorectal Dis. 2001, 3, 427–430. [Google Scholar] [CrossRef]
- Bissett, I.P.; Isbister, W.H. The management of patients with pilonidal disease—A comparative study. Aust. N. Z. J. Surg. 1987, 57, 939–942. [Google Scholar] [CrossRef] [PubMed]
- Karydakis, G.E. New approach to the problem of pilonidal sinus. Lancet 1973, 2, 1414–1415. [Google Scholar] [CrossRef]
- Monro, R.S.; McDermott, F.T. The Elimination of Causal Factors in Pilonidal Sinus Treated by Z-Plasty. Br. J. Surg. 1965, 52, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, M.K.; Tezel, E. Management of pilonidal sinus with the Limberg flap. Dis. Colon Rectum 1998, 41, 775–777. [Google Scholar] [CrossRef] [PubMed]
- Bascom, J.; Bascom, T. Utility of the cleft lift procedure in refractory pilonidal disease. Am. J. Surg. 2007, 193, 606–609. [Google Scholar] [CrossRef] [PubMed]
- Dessily, M.; Dziubeck, M.; Chahidi, E.; Simonelli, V. The SiLaC procedure for pilonidal sinus disease: Long-term outcomes of a single institution prospective study. Tech. Coloproctol. 2019, 23, 1133–1140. [Google Scholar] [CrossRef]
- Giarratano, G.; Toscana, C.; Shalaby, M.; Buonomo, O.; Petrella, G.; Sileri, P. Endoscopic Pilonidal Sinus Treatment: Long-Term Results of a Prospective Series. JSLS 2017, 21, e2017.00043. [Google Scholar] [CrossRef][Green Version]
- Garg, P.; Garg, M.; Gupta, V.; Mehta, S.K.; Lakhtaria, P. Laying open (deroofing) and curettage under local anesthesia for pilonidal disease: An outpatient procedure. World J. Gastrointest. Surg. 2015, 7, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Al-Khamis, A.; McCallum, I.; King, P.M.; Bruce, J. Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst. Rev. 2010, CD006213. [Google Scholar] [CrossRef] [PubMed]
- McCallum, I.J.; King, P.M.; Bruce, J. Healing by primary closure versus open healing after surgery for pilonidal sinus: Systematic review and meta-analysis. Bmj 2008, 336, 868–871. [Google Scholar] [CrossRef]
- McCallum, I.; King, P.M.; Bruce, J. Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst. Rev. 2007, CD006213. [Google Scholar] [CrossRef]
- Matter, I.; Kunin, J.; Schein, M.; Eldar, S. Total excision versus non-resectional methods in the treatment of acute and chronic pilonidal disease. Br. J. Surg. 1995, 82, 752–753. [Google Scholar] [CrossRef] [PubMed]
- Allen-Mersh, T.G. Pilonidal sinus: Finding the right track for treatment. Br. J. Surg. 1990, 77, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Vahedian, J.; Nabavizadeh, F.; Nakhaee, N.; Vahedian, M.; Sadeghpour, A. Comparison between drainage and curettage in the treatment of acute pilonidal abscess. Saudi Med. J. 2005, 26, 553–555. [Google Scholar] [PubMed]
- Garg, P. Difference in Patient and Surgeon Perception and Preference of Surgical Procedure to treat Pilonidal Sinus Disease. Aust. N. Z. J. Surg. 2020. [Google Scholar] [CrossRef]
- Garg, P. Endoscopic Pilonidal Sinus Treatment: Long-Term Results of a Prospective Series. JSLS 2018, 22, e2017.00083. [Google Scholar] [CrossRef]
- Hull, T.L.; Wu, J. Pilonidal disease. Surg. Clin. North Am. 2002, 82, 1169–1185. [Google Scholar] [CrossRef]
- Harlak, A.; Mentes, O.; Kilic, S.; Coskun, K.; Duman, K.; Yilmaz, F. Sacrococcygeal pilonidal disease: Analysis of previously proposed risk factors. Clinics 2010, 65, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Doll, D.; Bosche, F.; Hauser, A.; Moersdorf, P.; Sinicina, I.; Grunwald, J.; Reckel, F.; Luedi, M.M. The presence of occipital hair in the pilonidal sinus cavity-a triple approach to proof. Int. J. Colorectal Dis. 2018, 33, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Bosche, F.; Luedi, M.M.; van der Zypen, D.; Moersdorf, P.; Krapohl, B.; Doll, D. The Hair in the Sinus: Sharp-Ended Rootless Head Hair Fragments can be Found in Large Amounts in Pilonidal Sinus Nests. World J. Surg. 2018, 42, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Doll, D.; Bosche, F.D.; Stauffer, V.K.; Sinicina, I.; Hoffmann, S.; van der Zypen, D.; Luedi, M.M. Strength of Occipital Hair as an Explanation for Pilonidal Sinus Disease Caused by Intruding Hair. Dis. Colon Rectum 2017, 60, 979–986. [Google Scholar] [CrossRef]
| Parameter | N = 111 |
|---|---|
| Age | 22.9 ± 5.7 years |
| Sex | 92/19 |
| Follow-up Median (months) | 36 (4–111) |
| Anesthesia | LA |
| Inclusion criteria | Chronic, Recurrent, Abscess |
| Exclusion criteria | Refused consent |
| Recurrent | 22 (19.8%) (12-After wide excision with open healing, 7-After flap surgery, 3-After wide excision and midline closure) |
| Abscess | 24 (21.6%) |
| Parameter | N = 111 |
|---|---|
| Operating time | 24 ± 7 min |
| Hospital stay | 66 ± 23 min |
| Resume normal work | 3.6 ± 2.9 days |
| Healing time | 43.8 ± 7.4 days |
| Recurrence | 4 (3.7%) |
| Healing rate: | |
| After first surgery | 104/108 (96.3%) |
| After second surgery (n = 2) | 106/108 (98.1%) |
| Healing in Abscess patients (n = 24) | 24/24 (100%) |
| Complications-Minor bleeding | 5/108 (4.6%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garg, P.; Yagnik, V.D. Laying Open and Curettage under Local Anesthesia to Treat Pilonidal Sinus: Long-Term Follow-Up in 111 Consecutively Operated Patients. Clin. Pract. 2021, 11, 193-199. https://doi.org/10.3390/clinpract11020028
Garg P, Yagnik VD. Laying Open and Curettage under Local Anesthesia to Treat Pilonidal Sinus: Long-Term Follow-Up in 111 Consecutively Operated Patients. Clinics and Practice. 2021; 11(2):193-199. https://doi.org/10.3390/clinpract11020028
Chicago/Turabian StyleGarg, Pankaj, and Vipul D. Yagnik. 2021. "Laying Open and Curettage under Local Anesthesia to Treat Pilonidal Sinus: Long-Term Follow-Up in 111 Consecutively Operated Patients" Clinics and Practice 11, no. 2: 193-199. https://doi.org/10.3390/clinpract11020028
APA StyleGarg, P., & Yagnik, V. D. (2021). Laying Open and Curettage under Local Anesthesia to Treat Pilonidal Sinus: Long-Term Follow-Up in 111 Consecutively Operated Patients. Clinics and Practice, 11(2), 193-199. https://doi.org/10.3390/clinpract11020028







