Methadone, Metoclopramide and Metronidazole Interaction Causing Torsades de Pointes
Abstract
1. Introduction
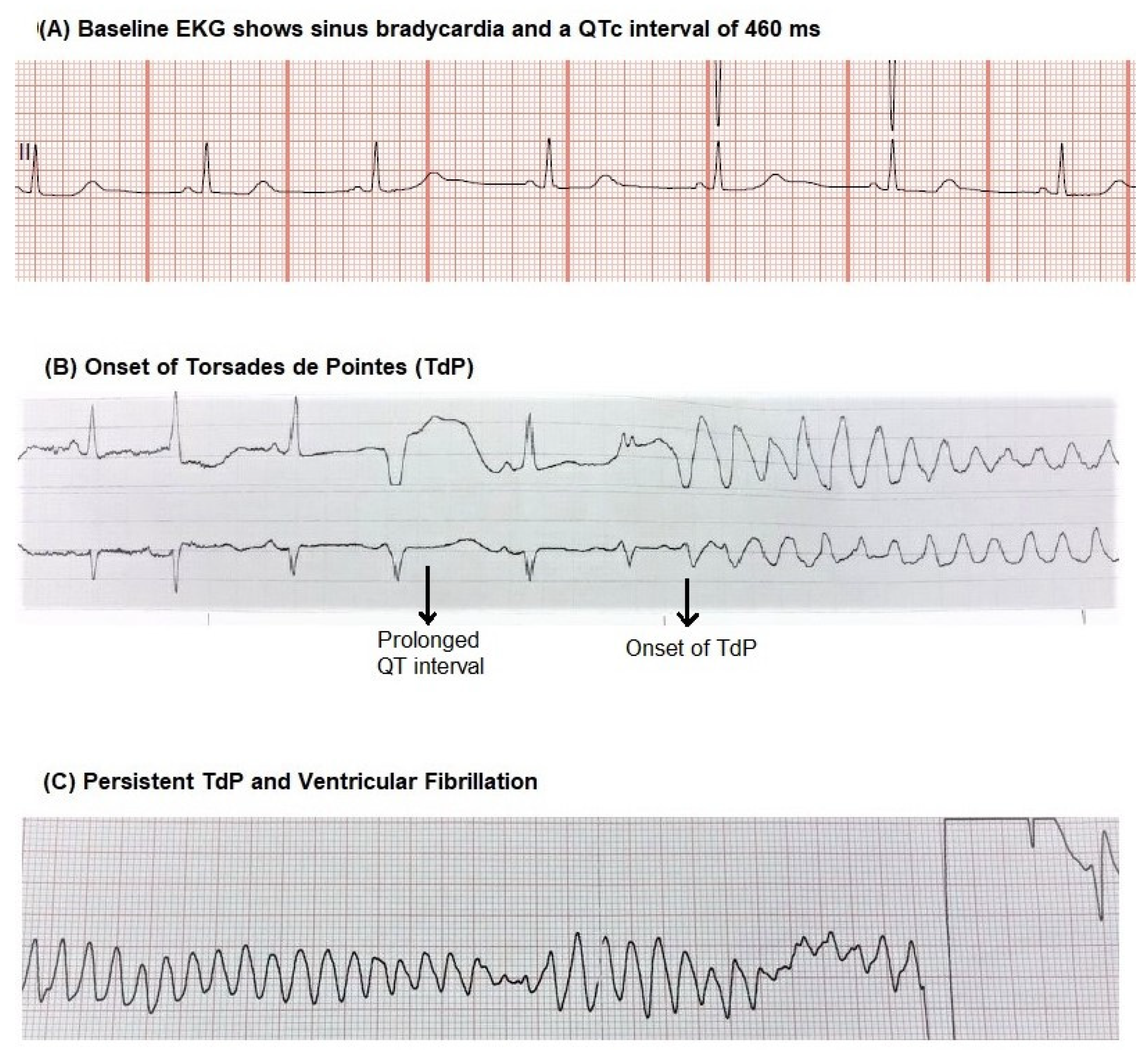
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Roden, D.M. Drug-Induced Prolongation of the QT Interval. N. Engl. J. Med. 2004, 350, 1013–1022. [Google Scholar] [CrossRef] [PubMed]
- Yap, Y.G.; Camm, A.J. Drug induced QT prolongation and torsades de pointes. Heart 2003, 89, 1363–1372. [Google Scholar] [CrossRef] [PubMed]
- Drew, B.J.; Ackerman, M.J.; Funk, M.; Gibler, W.B.; Kligfield, P.; Menon, V.; Philippides, G.J.; Roden, D.M.; Zareba, W. Prevention of torsade de pointes in hospital settings: A scientific statement from the American heart association and the American college of cardiology foundation. Circulation 2010, 121, 1047–1060. [Google Scholar] [CrossRef] [PubMed]
- Baumert, M.; Porta, A.; Vos, M.A.; Malik, M.; Couderc, J.P.; Laguna, P.; Piccirillo, G.; Smith, G.L.; Tereshchenko, L.G.; Volders, P.G. QT interval variability in body surface ECG: Measurement, physiological basis, and clinical value: Position statement and consensus guidance endorsed by the European Heart Rhythm Association jointly with the ESC Working Group on Cardiac Cellular Electrophysiology. Europace 2016, 18, 925–944. [Google Scholar] [PubMed]
- Pourmand, A.; Mazer-Amirshahi, M.; Chistov, S.; Sabha, Y.; Vukomanovic, D.; Almulhim, M. Emergency department approach to QTc prolongation. Am. J. Emerg. Med. 2017, 35, 1928–1933. [Google Scholar] [CrossRef] [PubMed]
- Chou, C.C.; Wu, D. Torsade de pointes induced by metoclopramide in an elderly woman with preexisting complete left bundle branch block. Chang. Gung. Med. J. 2001, 24, 805–809. [Google Scholar] [PubMed]
- Siddique, S.M.; Shariff, N.; Vesuwala, N.; Hafiz, T. Metoclopramide as a possible cause of prolonged QT syndrome and torsade de pointes in a patient with heart failure and renal insufficiency. Ann. Intern. Med. 2009, 150, 502–504. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.; Parish, D.; Thompson, L.; Cavaliere, M. Cocaine induced prolongation of the QT interval. Emerg. Med. J. 2004, 21, 252–253. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Magnano, A.R.; Talathoti, N.B.; Hallur, R.; Jurus, D.T.; Dizon, J.; Holleran, S.; Bloomfield, D.M.; Collins, E.; Garan, H. Effect of Acute Cocaine Administration on the QTc Interval of Habitual Users. Am. J. Cardiol. 2006, 97, 1244–1246. [Google Scholar] [CrossRef] [PubMed]
- Krantz, M.J.; Martin, J.; Stimmel, B.; Mehta, D.; Haigney, M.C. QTc interval screening in methadone treatment. Ann. Intern. Med. 2009, 150, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Alinejad, S.; Kazemi, T.; Zamani, N.; Hoffman, R.S.; Mehrpour, O. A systematic review of the cardiotoxicity of methadone. EXCLI J. 2015, 14, 577–600. [Google Scholar] [PubMed]
- Behzadi, M.; Joukar, S.; Beik, A. Opioids and Cardiac Arrhythmia: A Literature Review. Med. Princ. Pract. 2018, 27, 401–414. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, A.; Coccia, C.P.R.; Bertolini, A.; Sternieri, E. Methadone—Metabolism, pharmacokinetics and interactions. Pharmacol. Res. 2004, 50, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Kounas, S.P.; Letsas, K.P.; Sideris, A.; Efraimidis, M.; Kardaras, F. QT interval prolongation and torsades de pointes due to a coadministration of metronidazole and amiodarone. Pacing Clin. Electrophysiol. 2005, 28, 472–473. [Google Scholar] [CrossRef] [PubMed]
- Franchi, C.; Ardoino, I.; Rossio, R.; Nobili, A.; Biganzoli, E.M.; Marengoni, A.; Marcucci, M.; Pasina, L.; Tettamanti, M.; Corrao, S.; et al. Prevalence and Risk Factors Associated with Use of QT-Prolonging Drugs in Hospitalized Older People. Drugs Aging 2016, 33, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Woosley, R.L.; Black, K.; Heise, C.W.; Romero, K. CredibleMeds.org: What does it offer? Trends Cardiovasc. Med. 2018, 28, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Banai, S.; Tzivoni, D. Drug Therapy For Torsade de Pointes. J. Cardiovasc. Electrophysiol. 1993, 4, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Al Khatib, S.M.; Stevenson, W.G.; Ackerman, M.J. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2018, 72, e91–e220. [Google Scholar] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gnanapandithan, K.; Karthik, N.; Gerber, J. Methadone, Metoclopramide and Metronidazole Interaction Causing Torsades de Pointes. Clin. Pract. 2021, 11, 101-105. https://doi.org/10.3390/clinpract11010015
Gnanapandithan K, Karthik N, Gerber J. Methadone, Metoclopramide and Metronidazole Interaction Causing Torsades de Pointes. Clinics and Practice. 2021; 11(1):101-105. https://doi.org/10.3390/clinpract11010015
Chicago/Turabian StyleGnanapandithan, Karthik, Nishrutha Karthik, and Jaime Gerber. 2021. "Methadone, Metoclopramide and Metronidazole Interaction Causing Torsades de Pointes" Clinics and Practice 11, no. 1: 101-105. https://doi.org/10.3390/clinpract11010015
APA StyleGnanapandithan, K., Karthik, N., & Gerber, J. (2021). Methadone, Metoclopramide and Metronidazole Interaction Causing Torsades de Pointes. Clinics and Practice, 11(1), 101-105. https://doi.org/10.3390/clinpract11010015




