High Amount of Physical Activity on Work Days Is Associated with More Intense Musculoskeletal Symptoms in Nurses: Seven-Day Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Procedures
2.3.1. Assessment of Physical Activity
2.3.2. Assessment of Musculoskeletal Symptoms
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
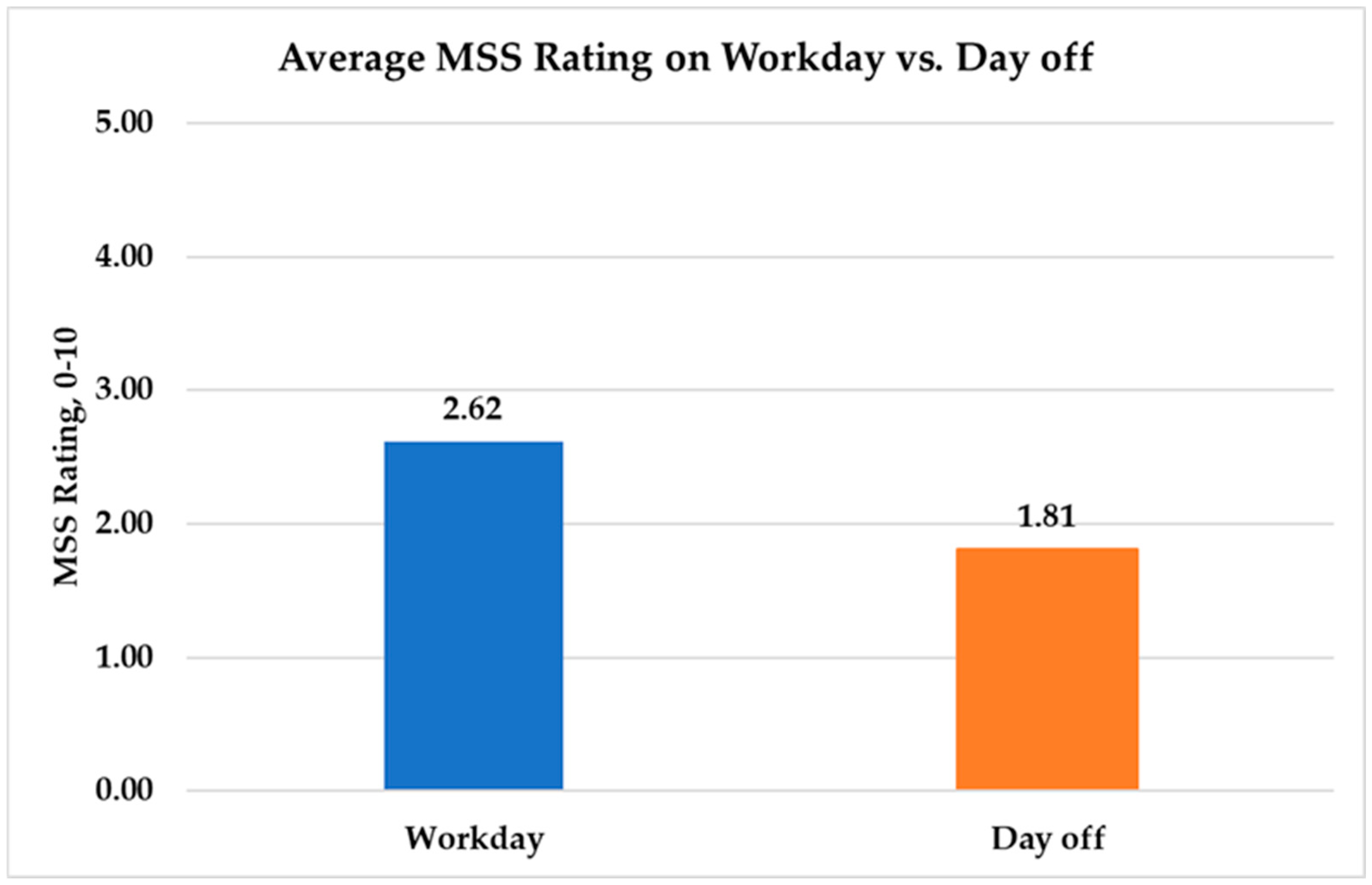
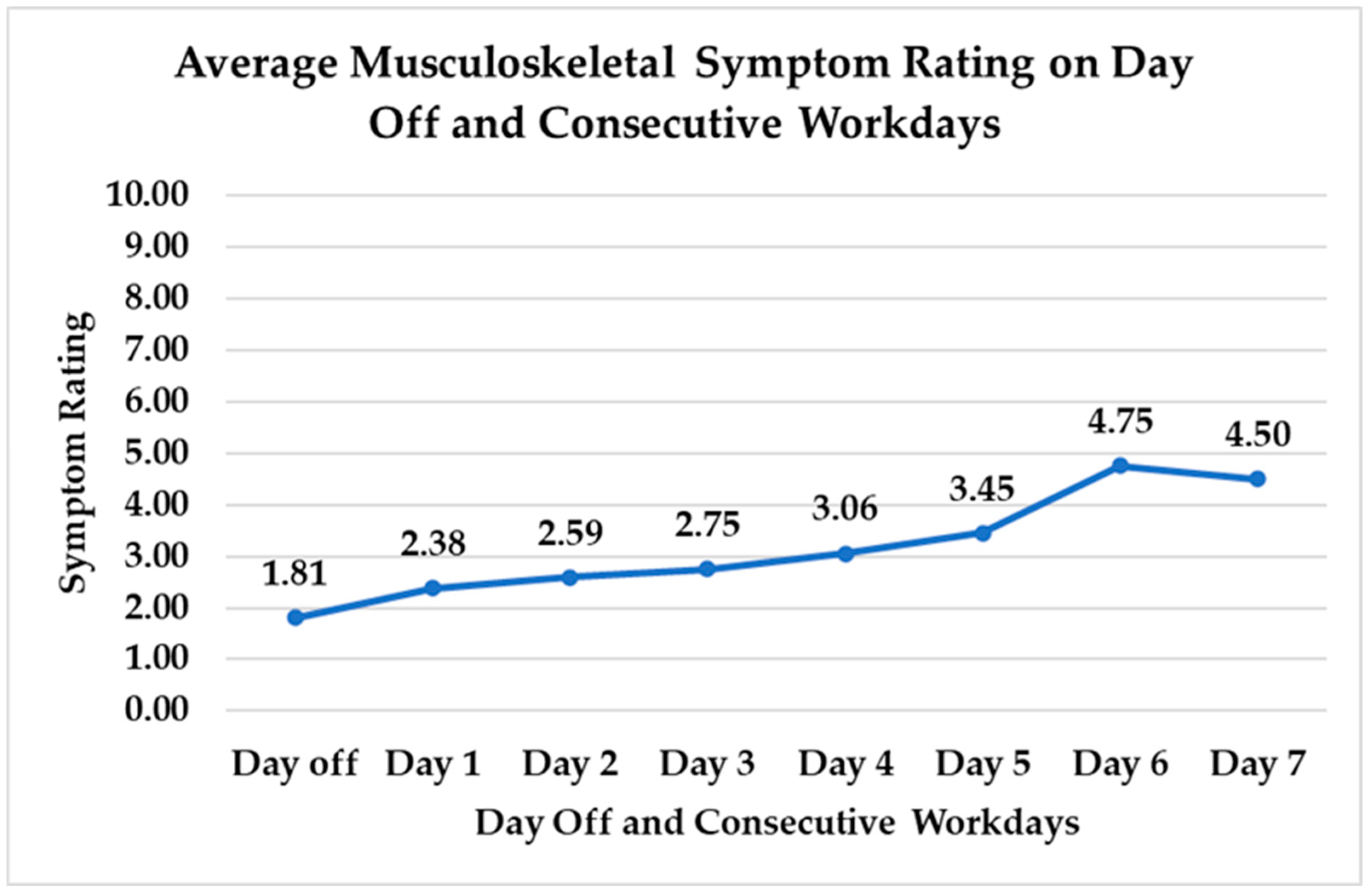
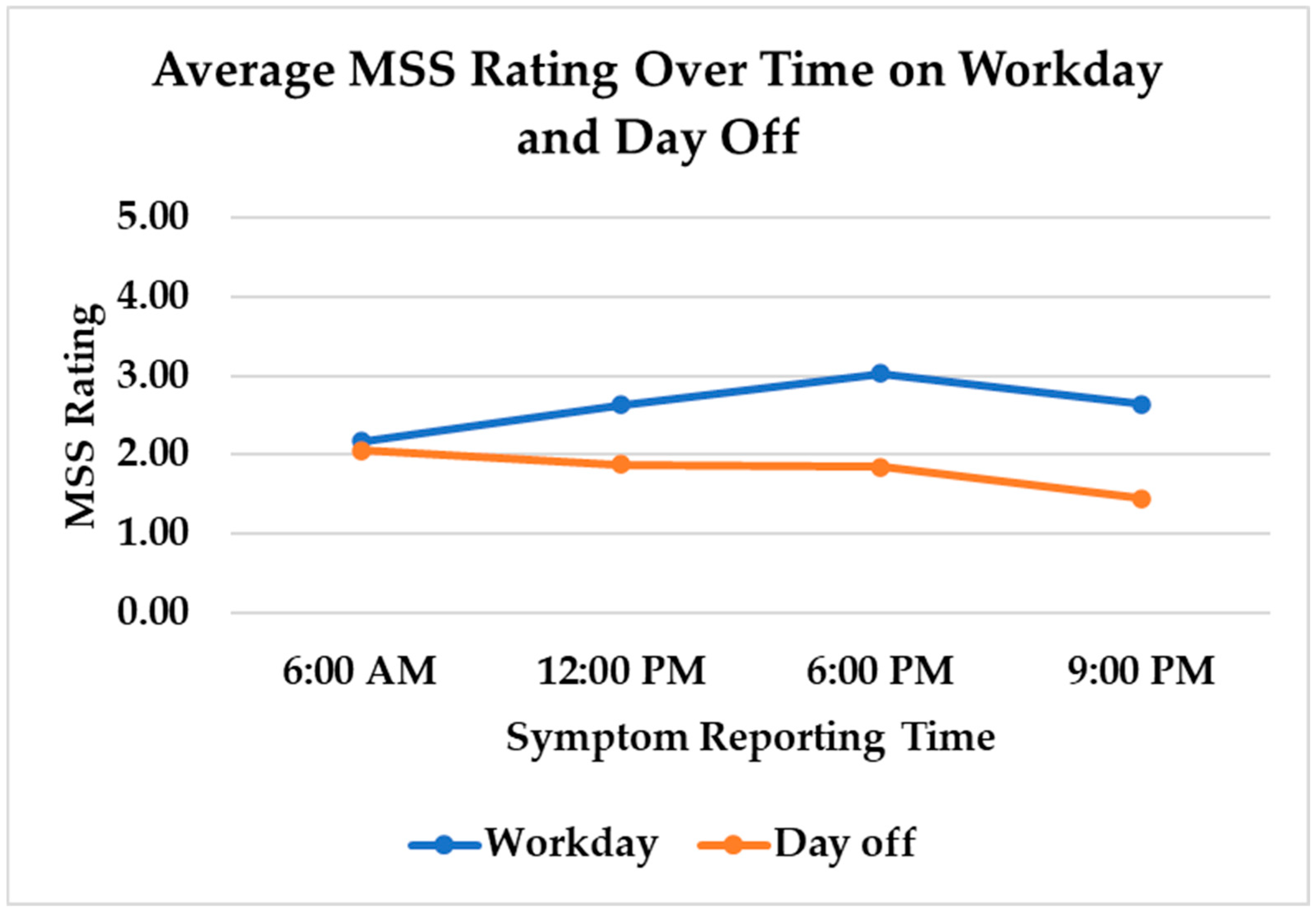
3.2. Musculoskeletal Symptoms
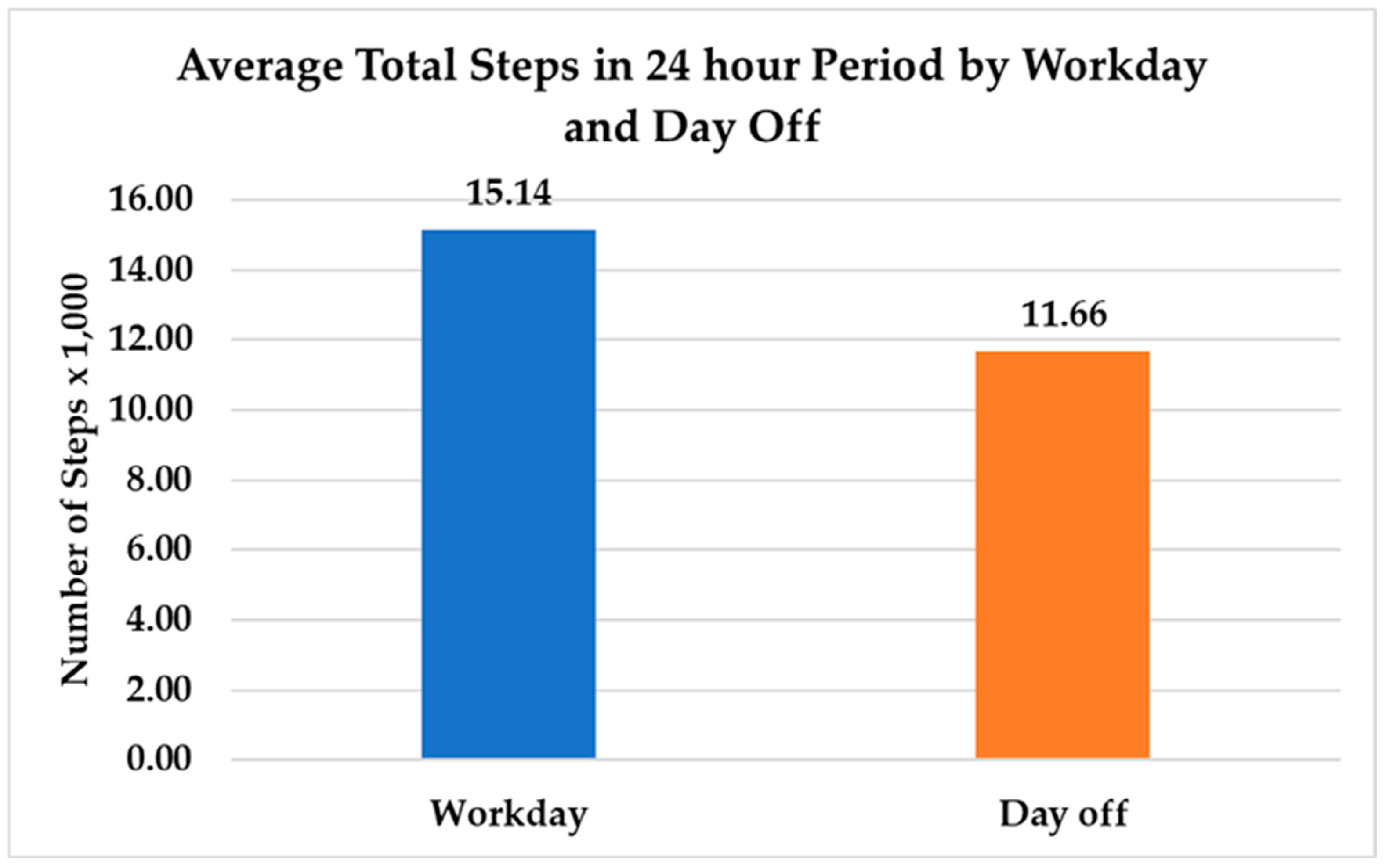
3.3. Physical Activity
3.4. Multivariable Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
Abbreviations
| MSS | Musculoskeletal Symptom |
| ANA | American Nurses Association |
| LLC | Limited Liability Corporation |
| M | Mean |
| SD | Standard Deviation |
References
- OSHA Safety and Health Topics. Healthcare—Safe Patient Handling. Available online: https://www.osha.gov/SLTC/healthcarefacilities/safepatienthandling.html (accessed on 25 November 2019).
- Davis, K.G.; Kotowski, S.E. Prevalence of Musculoskeletal Disorders for Nurses in Hospitals, Long-Term Care Facilities, and Home Health Care: A Comprehensive Review. Hum. Factors 2015, 57, 754–792. [Google Scholar] [CrossRef] [PubMed]
- Fochsen, G.; Josephson, M.; Hagberg, M.; Toomingas, A.; Lagerström, M. Predictors of Leaving Nursing Care: A Longitudinal Study among Swedish Nursing Personnel. Occup. Environ. Med. 2006, 63, 198–201. [Google Scholar] [CrossRef] [PubMed]
- Bordignon, M.; Monteiro, M.I. Predictors of Nursing Workers’ Intention to Leave the Work Unit, Health Institution and Profession. Rev. Lat. Am. Enferm. 2019, 27, e3219. [Google Scholar] [CrossRef]
- de Oliveira, D.R.; Griep, R.H.; Portela, L.F.; Rotenberg, L. Intention to Leave Profession, Psychosocial Environment and Self-Rated Health among Registered Nurses from Large Hospitals in Brazil: A Cross-Sectional Study. BMC Health Serv. Res. 2017, 17, 21. [Google Scholar] [CrossRef]
- Jakobsen, M.D.; Sundstrup, E.; Brandt, M.; Andersen, L.L. Effect of Physical Exercise on Musculoskeletal Pain in Multiple Body Regions among Healthcare Workers: Secondary Analysis of a Cluster Randomized Controlled Trial. Musculoskelet. Sci. Pract. 2018, 34, 89–96. [Google Scholar] [CrossRef]
- Morera, Á.; Calatayud, J.; López-Bueno, R.; Casaña, J.; Vinstrup, J.; Bláfoss, R.; Clausen, T.; Andersen, L.L. Can a Healthy Lifestyle Prevent Disability Pension among Female Healthcare Workers with Good and Poor Self-Rated Health? Prospective Cohort Study with 11-Year Register Follow-Up. Int. J. Environ. Res. Public Health 2022, 19, 10631. [Google Scholar] [CrossRef]
- American Nurses Association. Healthy Nurse Healthy Nation Year Four Highlights 2020–2021. Available online: https://www.healthynursehealthynation.org/globalassets/hnhn-redesign/research/03_hnhn-oct21-issue-921.pdf (accessed on 12 April 2025).
- Jirathananuwat, A.; Pongpirul, K. Physical Activity of Nurse Clinical Practitioners and Managers. J. Phys. Act. Health 2017, 14, 888–892. [Google Scholar] [CrossRef] [PubMed]
- Brunet, J.; Black, M.; Tulloch, H.E.; Pipe, A.L.; Reid, R.D.; Reed, J.L. Work-Related Factors Predict Changes in Physical Activity among Nurses Participating in a Web-Based Worksite Intervention: A Randomized Controlled Trial. BMC Nurs. 2021, 20, 224. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World. Available online: https://iris.who.int/bitstream/handle/10665/272722/9789241514187-eng.pdf (accessed on 12 April 2025).
- Chappel, S.E.; Verswijveren, S.J.J.M.; Aisbett, B.; Considine, J.; Ridgers, N.D. Nurses’ Occupational Physical Activity Levels: A Systematic Review. Int. J. Nurs. Stud. 2017, 73, 52–62. [Google Scholar] [CrossRef]
- Mo, P.K.H.; Blake, H.; Batt, M.E. Getting Healthcare Staff More Active: The Mediating Role of Self-Efficacy. Br. J. Health Psychol. 2011, 16, 690–706. [Google Scholar] [CrossRef]
- Blake, H.; Malik, S.; Mo, P.K.H.; Pisano, C. “Do as Say, but Not as I Do”: Are next Generation Nurses Role Models for Health? Perspect. Public Health 2011, 131, 231–239. [Google Scholar] [CrossRef]
- Ross, A.; Bevans, M.; Brooks, A.T.; Gibbons, S.; Wallen, G.R. Nurses and Health-Promoting Behaviors: Knowledge May Not Translate Into Self-Care. AORN J. 2017, 105, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Coenen, P.; Huysmans, M.A.; Holtermann, A.; Troiano, R.P.; Mork, P.J.; Krokstad, S.; Clays, E.; Cillekens, B.; De Bacquer, D.; Aadahl, M.; et al. Associations of Occupational and Leisure-Time Physical Activity with All-Cause Mortality: An Individual Participant Data Meta-Analysis. Br. J. Sports Med. 2024, 58, 1527–1538. [Google Scholar] [CrossRef] [PubMed]
- Merkus, S.L.; Coenen, P.; Forsman, M.; Knardahl, S.; Veiersted, K.B.; Mathiassen, S.E. An Exploratory Study on the Physical Activity Health Paradox-Musculoskeletal Pain and Cardiovascular Load during Work and Leisure in Construction and Healthcare Workers. Int. J. Environ. Res. Public Health 2022, 19, 2751. [Google Scholar] [CrossRef] [PubMed]
- Temporelli, P.L. Is Physical Activity Always Good for You? The Physical Activity Paradox. Eur. Heart J. Suppl. 2021, 23, E168–E171. [Google Scholar] [CrossRef]
- Coenen, P.; Huysmans, M.A.; Holtermann, A.; Krause, N.; van Mechelen, W.; Straker, L.M.; van der Beek, A.J. Towards a Better Understanding of the “physical Activity Paradox”: The Need for a Research Agenda. Br. J. Sports Med. 2020, 54, 1055–1057. [Google Scholar] [CrossRef]
- Coenen, P.; Huysmans, M.A.; Holtermann, A.; Krause, N.; van Mechelen, W.; Straker, L.M.; van der Beek, A.J. Do Highly Physically Active Workers Die Early? A Systematic Review with Meta-Analysis of Data from 193 696 Participants. Br. J. Sports Med. 2018, 52, 1320–1326. [Google Scholar] [CrossRef]
- Gupta, N.; Dencker-Larsen, S.; Lund Rasmussen, C.; McGregor, D.; Rasmussen, C.D.N.; Thorsen, S.V.; Jørgensen, M.B.; Chastin, S.; Holtermann, A. The Physical Activity Paradox Revisited: A Prospective Study on Compositional Accelerometer Data and Long-Term Sickness Absence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 93. [Google Scholar] [CrossRef]
- Skov, T.; Borg, V.; Orhede, E. Psychosocial and Physical Risk Factors for Musculoskeletal Disorders of the Neck, Shoulders, and Lower Back in Salespeople. Occup. Environ. Med. 1996, 53, 351–356. [Google Scholar] [CrossRef]
- Keyaerts, S.; Godderis, L.; Delvaux, E.; Daenen, L. The Association between Work-Related Physical and Psychosocial Factors and Musculoskeletal Disorders in Healthcare Workers: Moderating Role of Fear of Movement. J. Occup. Health 2022, 64, e12314. [Google Scholar] [CrossRef]
- Janssen, T.I.; Voelcker-Rehage, C. Leisure-Time Physical Activity, Occupational Physical Activity and the Physical Activity Paradox in Healthcare Workers: A Systematic Overview of the Literature. Int. J. Nurs. Stud. 2023, 141, 104470. [Google Scholar] [CrossRef] [PubMed]
- Parker, H.M.; Gallagher, R.; Duffield, C.; Ding, D.; Sibbritt, D.; Perry, L. Occupational and Leisure-Time Physical Activity Have Different Relationships with Health: A Cross-Sectional Survey Study of Working Nurses. J. Phys. Act. Health 2021, 18, 1495–1502. [Google Scholar] [CrossRef] [PubMed]
- Ngueleu, A.-M.; Barthod, C.; Best, K.L.; Routhier, F.; Otis, M.; Batcho, C.S. Criterion Validity of ActiGraph Monitoring Devices for Step Counting and Distance Measurement in Adults and Older Adults: A Systematic Review. J. Neuroeng. Rehabil. 2022, 19, 112. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Johnson, W.D.; Katzmarzyk, P.T. Accelerometer-Determined Steps per Day in US Adults. Med. Sci. Sports Exerc. 2009, 41, 1384–1391. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Brown, W.J.; Clemes, S.A.; De Cocker, K.; Giles-Corti, B.; Hatano, Y.; Inoue, S.; Matsudo, S.M.; Mutrie, N.; et al. How Many Steps/day Are Enough? For Adults. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 79. [Google Scholar] [CrossRef]
- Loef, B.; van der Beek, A.J.; Holtermann, A.; Hulsegge, G.; van Baarle, D.; Proper, K.I. Objectively Measured Physical Activity of Hospital Shift Workers. Scand. J. Work Environ. Health 2018, 44, 265–273. [Google Scholar] [CrossRef]
- Anchouche, K.; Elharram, M.; Oulousian, E.; Razaghizad, A.; Avram, R.; Marquis-Gravel, G.; Randhawa, V.K.; Nkulikiyinka, R.; Ni, W.; Fiuzat, M.; et al. Use of Actigraphy (Wearable Digital Sensors to Monitor Activity) in Heart Failure Randomized Clinical Trials: A Scoping Review. Can. J. Cardiol. 2021, 37, 1438–1449. [Google Scholar] [CrossRef] [PubMed]
- Wood, L.J.; Christian, M.; Perrin, N.; Backikenge Mirindi, A.; Heri Banywesize, J.; Murhula Mitima, C.; Kajabika Binkurhorwa, A.; Mitima Ntqali, E.; Ntakwinja Mushengezi, G.; Mpanano Remy, M.; et al. Acceptability and Feasibility of Using Actigraphy to Assess Habitual Physical Activity and Sleep Parameters in Men and Women Living in Rural Communities in Conflict-Affected Eastern Democratic Republic of Congo. Glob. Ment. Health 2020, 7, e33. [Google Scholar] [CrossRef]
- Schwab, K.E.; To, A.Q.; Chang, J.; Ronish, B.; Needham, D.M.; Martin, J.L.; Kamdar, B.B. Actigraphy to Measure Physical Activity in the Intensive Care Unit: A Systematic Review. J. Intensive Care Med. 2020, 35, 1323–1331. [Google Scholar] [CrossRef]
- Stone, A.A.; Obbarius, A.; Junghaenel, D.U.; Wen, C.K.F.; Schneider, S. High-Resolution, Field Approaches for Assessing Pain: Ecological Momentary Assessment: Ecological Momentary Assessment. Pain 2021, 162, 4–9. [Google Scholar] [CrossRef]
- Iacob, E.; Donaldson, G.; Neikrug, A.; Nakamura, Y.; Okifuji, A. Self-Report Ecological Momentary Assessment in Patients with Fibromyalgia to Examine Temporal Relationships between Pain with Mood, Fatigue, and Sleep. J. Pain 2016, 17, S6. [Google Scholar] [CrossRef]
- Mikati, N.; Suffoletto, B.; Pacella-LaBarbara, M.; Callaway, C. Comparison of Musculoskeletal Pain Severity and Pain Interference Using Ecological Momentary Assessment: A Longitudinal Analysis. J. Pain 2021, 22, 594. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Participants: Ethical Principles for Medical Research Involving Human Participants. JAMA 2024, 333, 71–74. [Google Scholar]
- Luna, S. The Relationship of Musculoskeletal Symptoms in Nurses with Psychological and Physiological Factors Influencing Health. Ph.D. Thesis, University of Texas Health Science Center at San Antonio, San Antonio, TX, USA, 2024. [Google Scholar]
- Kohn, M.A.; Senyak, J. Sample Size Calculators. UCSF CTSI. Available online: https://sample-size.net/correlation-sample-size (accessed on 26 March 2021).
- Kraus, W.E.; Janz, K.F.; Powell, K.E.; Campbell, W.W.; Jakicic, J.M.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L.; 2018 Physical Activity Guidelines Advisory Committee. Daily Step Counts for Measuring Physical Activity Exposure and Its Relation to Health. Med. Sci. Sports Exerc. 2019, 51, 1206–1212. [Google Scholar] [CrossRef]
- ActiGraph. Available online: https://theactigraph.com/ (accessed on 11 April 2025).
- Karas, M.; Bai, J.; Strączkiewicz, M.; Harezlak, J.; Glynn, N.W.; Harris, T.; Zipunnikov, V.; Crainiceanu, C.; Urbanek, J.K. Accelerometry Data in Health Research: Challenges and Opportunities. Stat. Biosci. 2019, 11, 210–237. [Google Scholar] [CrossRef] [PubMed]
- Schall, M.C.; Chen, H.; Fethke, N. Comparing Fatigue, Physical Activity, and Posture among Nurses in Two Staffing Models. Proc. Hum. Fact. Ergon. Soc. Annu. Meet. 2015, 59, 1269–1273. [Google Scholar] [CrossRef]
- About One-in-Five Americans Use a Smart Watch or Fitness Tracker. Available online: https://www.pewresearch.org/short-reads/2020/01/09/about-one-in-five-americans-use-a-smart-watch-or-fitness-tracker/#:~:text=As%202020%20begins%20%E2%80%93%20and%20health,June%203%2D17%2C%202019 (accessed on 8 April 2022).
- Henriksen, A.; Haugen Mikalsen, M.; Woldaregay, A.Z.; Muzny, M.; Hartvigsen, G.; Hopstock, L.A.; Grimsgaard, S. Using Fitness Trackers and Smartwatches to Measure Physical Activity in Research: Analysis of Consumer Wrist-Worn Wearables. J. Med. Internet Res. 2018, 20, e110. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Mâsse, L.C.; Tilert, T.; McDowell, M. Physical Activity in the United States Measured by Accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef]
- Hildebrand, M.; Van Hees, V.T.; Hansen, B.H.; Ekelund, U. Age Group Comparability of Raw Accelerometer Output from Wrist- and Hip-Worn Monitors. Med. Sci. Sports Exerc. 2014, 46, 1816–1824. [Google Scholar] [CrossRef]
- Van Hees, V.T.; Gorzelniak, L.; Dean León, E.C.; Eder, M.; Pias, M.; Taherian, S.; Ekelund, U.; Renström, F.; Franks, P.W.; Horsch, A.; et al. Separating Movement and Gravity Components in an Acceleration Signal and Implications for the Assessment of Human Daily Physical Activity. PLoS ONE 2013, 8, e61691. [Google Scholar] [CrossRef]
- Funabashi, M.; Wang, S.; Lee, A.D.; C K Duarte, F.; Budgell, B.; Stilwell, P.; Hogg-Johnson, S. Discomfort, Pain and Stiffness: What Do These Terms Mean to Patients? A Cross-Sectional Survey with Lexical and Qualitative Analyses. BMC Musculoskelet. Disord. 2022, 23, 283. [Google Scholar] [CrossRef] [PubMed]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical Activity, Exercise, and Physical Fitness: Definitions and Distinctions for Health-Related Research. Public Health Rep. 1985, 100, 126–131. [Google Scholar]
- Tullar, J.M.; Brewer, S.; Amick, B.C., 3rd; Irvin, E.; Mahood, Q.; Pompeii, L.A.; Wang, A.; Van Eerd, D.; Gimeno, D.; Evanoff, B. Occupational Safety and Health Interventions to Reduce Musculoskeletal Symptoms in the Health Care Sector. J. Occup. Rehabil. 2010, 20, 199–219. [Google Scholar] [CrossRef] [PubMed]
- 10,000 Steps a Day: Too Low? Too High? Available online: https://www.mayoclinic.org/healthy-lifestyle/fitness/in-depth/10000-steps/art-20317391 (accessed on 20 February 2025).
- CDC Benefits of Physical Activity. Available online: https://www.cdc.gov/physical-activity-basics/benefits/?CDC_AAref_Val=https://www.cdc.gov/physicalactivity/basics/pa-health/index.htm (accessed on 6 February 2024).
- Weekly, N.N. The Obesity Epidemic Has Made Its Way to Nurses: What Does This Mean? Available online: https://njsna.org/the-obesity-epidemic-has-made-its-way-to-nurses-what-does-this-mean/ (accessed on 11 April 2025).
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 11 April 2025).
- Texas Department of State Health Services. Prevalence of Obesity among Adults, by Demographic Characteristics, Risk Factors/comorbid Conditions, and Place of Residence, Texas 2020. Available online: https://www.dshs.texas.gov/sites/default/files/uploadedFiles/Content/Prevention_and_Preparedness/obesity/pdf/2020-BRFSS-Obesity-Tables.pdf (accessed on 11 April 2025).
- Chowdhury, R.; Shah, D.; Payal, A.R. Healthy Worker Effect Phenomenon: Revisited with Emphasis on Statistical Methods—A Review. Indian J. Occup. Environ. Med. 2017, 21, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Hagan, J.L.; Tyer-Viola, L.; Graves, K. Predictors of Nurses Considering Leaving the Profession due to Work-Related Stress in a Large Pediatric and Women’s Hospital in the United States. Int. J. Hosp. Tour. Adm. 2018, 8, 27. [Google Scholar] [CrossRef]
- Bae, S.-H. Noneconomic and Economic Impacts of Nurse Turnover in Hospitals: A Systematic Review. Int. Nurs. Rev. 2022, 69, 392–404. [Google Scholar] [CrossRef]

| Characteristics | N = 31 | Percent |
|---|---|---|
| Gender | ||
| Male | 1 | 3.2 |
| Female | 30 | 96.8 |
| Race/Ethnicity | ||
| Black/African American | 1 | 3.2 |
| White, non-Hispanic | 16 | 51.6 |
| White, Hispanic | 13 | 41.9 |
| Other race/ethnicity | 1 | 3.2 |
| Work setting | ||
| Hospital | 22 | 71 |
| Outpatient care, urgent care, surgery center | 3 | 9.7 |
| Home health | 4 | 12.9 |
| Other | 2 | 6.5 |
| Days of Participation | ||
| 5 days | 1 | 3.2 |
| 6 days | 1 | 3.2 |
| 7 days | 29 | 93.6 |
| Work days | ||
| 2–3 days | 14 | 45.2 |
| 4–5 days | 15 | 48.4 |
| 6–7 days | 2 | 6.4 |
| Days worked (out of 214 nurse-days) | N = 214 | Percent |
| Work day | 119 | 55.6 |
| Day off | 95 | 44.4 |
| Exercise (out of 214 nurse-days) | ||
| Exercised on work day | 10 | 4.7 |
| Exercised on day off | 23 | 10.8 |
| Did not exercise | 172 | 80.4 |
| Did not report | 9 | 4.2 |
| Days with exercise | N = 29 | Percent |
| None | 14 | 48.3 |
| 1–2 | 8 | 27.6 |
| 3–4 | 7 | 24.1 |
| Variables | Estimate | DF | t Value | p |
|---|---|---|---|---|
| Cumulative Steps | 0.0117 | 823 | 2.58 | 0.01 * |
| Time of Day | ||||
| 6:00 a.m. | −0.0863 | 823 | −1.61 | 0.11 |
| 12:00 p.m. | 0.0230 | 823 | 0.44 | 0.66 |
| 6:00 p.m. | 0.1372 | 823 | 2.70 | 0.007 ** |
| 9:00 p.m. | −0.0842 | 823 | 1.54 | 0.12 |
| Day Off vs. Work Day | 0.2420 | 823 | 4.76 | <0.0001 ** |
| Consecutive Work Days | 0.0669 | 822 | 3.76 | 0.0002 ** |
| Shift Length | 0.0389 | 439 | 2.53 | 0.01 * |
| Lunch Break | −0.2050 | 428 | −2.16 | 0.03 * |
| Bathroom Break | 0.2336 | 428 | 2.15 | 0.03 * |
| Setting | ||||
| Hospital | −0.2704 | 824 | −0.90 | 0.37 |
| Outpatient Care, Urgent Care, Surgical Center | −0.0246 | 824 | −0.05 | 0.96 |
| Home Health, Hospice | 0.5483 | 824 | 1.38 | 0.17 |
| Other | −0.0835 | 824 | −0.15 | 0.88 |
| Age | 0.0303 | 823 | 2.29 | 0.02 * |
| BMI | 0.0668 | 824 | 3.23 | 0.001 ** |
| Exercise | −0.0974 | 773 | −1.28 | 0.20 |
| Variable | Parameter Estimate | Standard Error | DF | t Value | p |
|---|---|---|---|---|---|
| Intercept | −2.02 | 0.70 | 28 | −2.90 | 0.01 |
| Cumulative Steps a | −0.02 | 0.01 | 769 | −1.99 | 0.05 * |
| Work Day | −0.01 | 0.09 | 769 | −0.14 | 0.89 |
| Day Off b | 0.00 | ||||
| Cumulative Steps a on Work Day | 0.03 | 0.01 | 769 | 3.38 | 0.001 ** |
| Cumulative Steps a on Day Off b | 0.00 | ||||
| Exercise | 0.00 | 0.08 | 769 | −0.06 | 0.95 |
| No Exercise b | 0.00 | ||||
| Age | 0.02 | 0.01 | 769 | 1.79 | 0.07 |
| BMI | 0.06 | 0.02 | 769 | 2.73 | 0.007 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luna, S.; Douphrate, D.; Choi, B.Y.; Flores, B.; Patel, R.; Pompeii, L. High Amount of Physical Activity on Work Days Is Associated with More Intense Musculoskeletal Symptoms in Nurses: Seven-Day Observational Study. Nurs. Rep. 2025, 15, 143. https://doi.org/10.3390/nursrep15050143
Luna S, Douphrate D, Choi BY, Flores B, Patel R, Pompeii L. High Amount of Physical Activity on Work Days Is Associated with More Intense Musculoskeletal Symptoms in Nurses: Seven-Day Observational Study. Nursing Reports. 2025; 15(5):143. https://doi.org/10.3390/nursrep15050143
Chicago/Turabian StyleLuna, Sarah, David Douphrate, Byeong Yeob Choi, Bertha Flores, Rupal Patel, and Lisa Pompeii. 2025. "High Amount of Physical Activity on Work Days Is Associated with More Intense Musculoskeletal Symptoms in Nurses: Seven-Day Observational Study" Nursing Reports 15, no. 5: 143. https://doi.org/10.3390/nursrep15050143
APA StyleLuna, S., Douphrate, D., Choi, B. Y., Flores, B., Patel, R., & Pompeii, L. (2025). High Amount of Physical Activity on Work Days Is Associated with More Intense Musculoskeletal Symptoms in Nurses: Seven-Day Observational Study. Nursing Reports, 15(5), 143. https://doi.org/10.3390/nursrep15050143







