Implementation of Green Lean Six Sigma in Dutch Healthcare: A Qualitative Study of Healthcare Professionals’ Experiences
Abstract
1. Introduction
2. Study Context
3. Materials and Methods
3.1. Methodological Overview
3.2. Construction of Survey
3.3. Data Collection and Case Description
3.4. Data Analysis
4. Results
4.1. Project Initiation and Completion
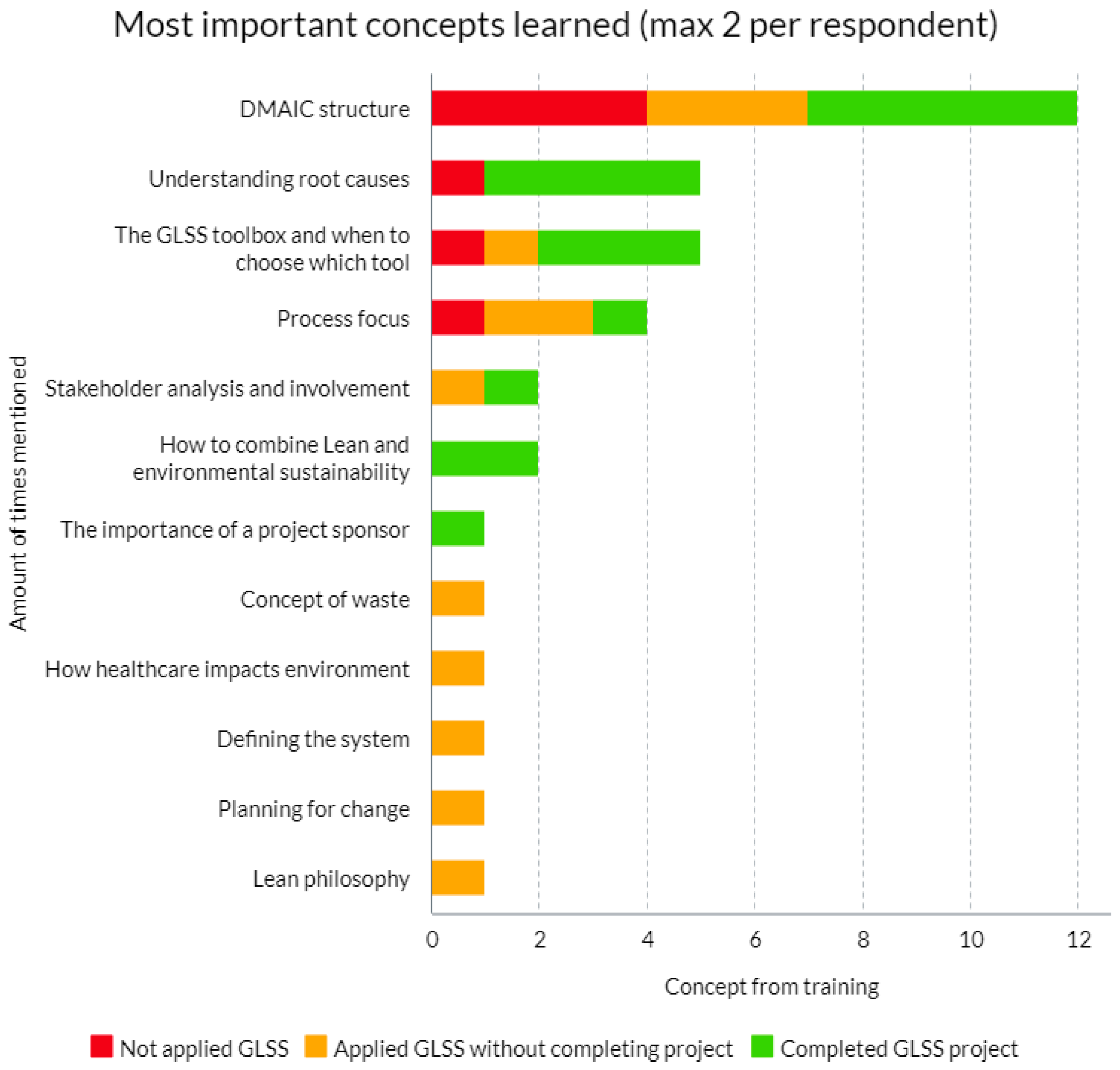
4.2. Evaluation of GLSS Tools and Concepts
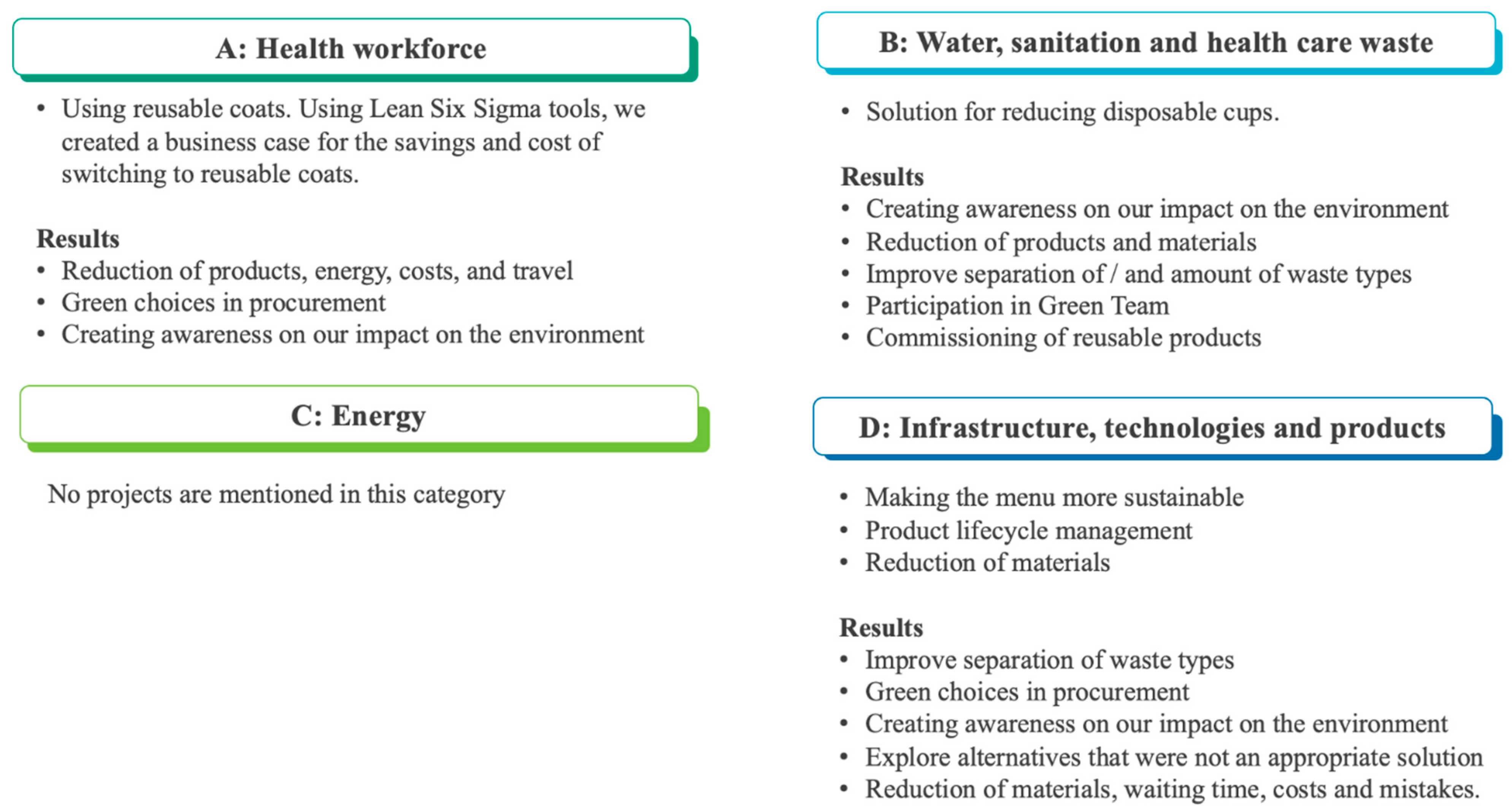
4.3. Evaluation on Results Level
4.4. Experienced Barriers and Success Factors
5. Discussion
Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
Appendix A. Training Content GLSS Training for Sustainable Healthcare
- -
- Describe the concepts, principles, and methodology of GLSS.
- -
- Choose and apply tools and techniques from the GLSS toolset to a given case study to map, measure, analyze, improve, and control a process (Define, Measure, Analyze, Improve, and Control phases of a GLSS project).
- -
- Choose an appropriate case from your work situation to apply GLSS to for the purpose of reducing climate impact.
| DMAIC Phase | Green Lean Six Sigma Tool |
|---|---|
| Define | Stakeholder analysis |
| Project charter | |
| Suppliers, input, process, outputs, and customers (SIPOC) | |
| Voice of the customer (VOC) | |
| Critical to quality (CTQ) | |
| Kano analysis | |
| Measure | Lifecycle assessment (LCA) |
| Process mapping | |
| Little’s Law | |
| Analyze | Sort, straighten, shine, standardize, and sustain (5S) |
| Forms of waste: defects, overproduction transportation waiting inventory, motion, and processing (DOTWIMP) and reduce, reuse, recycle (Ladder of Lansink) | |
| Value Add and Non-Value Add tool analysis | |
| Swimlane diagram | |
| Root cause analysis | |
| 5 WHY | |
| Fishbone | |
| Brainstorming | |
| Affinity diagrams | |
| Improvement | Improvement plan |
| DPSIR framework: Driving forces, pressure, state, impacts and responses/improvements | |
| Reduce -> reuse -> remake -> recycle cycle | |
| Select solutions: single voting multi voting | |
| Implementation plan | |
| Control | Control plan |
Appendix B. Description of Data Collected on t0 and t1
| Data Element | Data Input Format |
| Name | Free text |
| Age | Number |
| Gender at birth | M/F |
| Job function | Free text |
| Level of experience with process improvement | Likert scale 1 (no experience) to 5 (very experienced) |
| Healthcare institute | Free text |
| Highest education level completed | WO/HBO/MBO/Other: [free text] |
| How competent do you feel to implement “green” solutions at your workplace? | Likert scale 1 (not competent) to 5 (very competent) |
| Why do you want to start this training? | Free text |
| Entry test on GLSS concepts and tools | Multiple choice questions |
| Data Element | Data Input Format |
|---|---|
| Did you enjoy taking the training? | Likert scale 1 (not at all) to 5 (very much) |
| How did you experience the difficulty of the training? | Likert scale 1 (very easy) to 5 (very difficult) |
| How motivated do you feel to apply GLSS at your workplace? | Likert scale 1 (not motivated at all) to 5 (very motivated) |
| Did you gain new knowledge from the training? | Likert scale 1 (not at all) to 5 (a lot of new knowledge) |
| How empowered do you feel to apply GLSS at your workplace? | Likert scale 1 (not empowered at all) to 5 (very empowered) |
| Knowledge test GLSS concepts and tools | Multiple choice questions |
| Written exam: Case study with assignment to describe approach to follow step by step | Open text |
Appendix C. Search Strategy Kirkpatrick Questionnaires
| Pubmed |
| (Kirkpatrick[Title/Abstract]) AND (evaluation[Title/Abstract] OR assessment[Title/Abstract]) AND (questionnaire[Title/Abstract]) AND (behavior[Title/Abstract] OR behaviour[Title/Abstract] OR attitude[Title/Abstract]) |
| Education database (Proquest) |
| ab(Kirkpatrick) AND ab(questionnaire) AND ab(evaluation OR assessment) AND ab(behavior OR behaviour OR attitude) |
- Article written in English or Dutch.
- Population within the study should be students or members of the general, healthy population who take part in a training or other type of educational program.
- The article includes a questionnaire.
- The article questions in the questionnaire are applicable to Green Lean Healthcare training or can be made applicable by minor adjustment (e.g., change one or two words in the question).
- Article full text is accessible for researchers from the University of Amsterdam.
Appendix D. Original and Modified Questions for Survey
| Original Question | Adjusted Question Used in Final Questionnaire |
|---|---|
| Questions on Kirkpatrick’s Behavior level | |
| “The training programmes helped me to organise my role as head teacher more effectively”, Alsalamah and Callinan [16], p. 14. | Not included (not applicable for GLSS training) |
| “The training progammes inspired me to improve my achievement”, Alsalamah and Callinan [16], p. 14. | Q1. The GLSS training inspired me to improve my achievement in making healthcare green. |
| “The training progammes increased my ability to perform well in my job role”, Alsalamah and Callinan [16], p. 14. | Q2. The GLSS training increased my ability to perform well in my job role. |
| “The training progammes helped me to develop leadership behaviour”, Alsalamah and Callinan [16], p. 14. | Not included (not applicable for GLSS training) |
| “The training progammes developed some aspects of my behaviour”, Alsalamah and Callinan [16], p. 14. | Not included (removed after pretesting survey with one respondent due to length of survey and overlap with Q3) |
| “The training progammes helped me to prove myself in my work as head teacher”, Alsalamah and Callinan [16], p. 14. | Not included (not applicable for GLSS training) |
| “My job behaviour changed after completing the programme”, Alsalamah and Callinan [16], p. 14. | Q3. While performing my job, my behavior changed after completing the program. |
| No source.Purpose: Assess confidence of participant in application of learnings. | Q4. I feel confident about applying what I have learned on the job. |
| “What are the major concepts that you learned during this session?” Kirckpatrick & Kirckpatrick [15], p. 103. | Q5: What are the two major concepts that you learned during the GLSS training? |
| “What barriers do you anticipate that could limit your success at applying what you learned?” Kirckpatrick and Kirckpatrick [15], p. 103. | Q6: What barrier(s) did you experience that limited your success at applying GLSS in practice?
|
| Part B1. | |
| No source for question. Purpose: check if participant applied the learning tools in a real-life setting. If no they can skip the following questions and continue with X. | Q7. Did you apply learnings form the training in a real-life setting? Yes No |
| No source for question. Purpose: check category and which environmental impact problem the participant addressed in their projects. | Q8. Describe in a few sentences which root causes you addressed with solutions and the measurable impact (answer can be in Dutch) Open question |
| No source for question. Source WHO framework: Prats [18]. | Q9. Which category fits the real-life setting where you applied the learnings best? A: Health workforce B: Water, sanitation and health care waste C: Energy D: Infrastructure, technologies and products |
| No source for question. Purpose: check which environmental impact problem participants addressed in their projects, check which outcome measures are applicable for describing results of their projects at an organization level. | Q10. What are the results you achieved within your organization by applying the learnings of the training? Creating awareness on our impact on the environment Reduce water use Reduce use of products/materials (and waste) Energy reduction Reducing of direct gas emissions (anesthetics or other) Reduce travel Reduce pollution of waste water Improve separation of waste types (gescheiden afvalverzameling) Green choices in procurement Lead Time reduction Cost reduction Reducing workload of employees Reducing errors/mistakes Reduction of waiting time None Other: …. |
| Part B2. | |
| No source for question. Purpose: check which GLSS tools are used/will be used. | Q11. For each of the following Lean Six Sigma tools, please indicate your expected usage (I applied this tool, I strongly think I will apply this tool, I might apply this tool, I don’t expect to apply this tool, I don’t know) Project charter SIPOC Critical to Quality Tree Lifecycle Assessment Process Mapping DOTWIMP 5S Value Add Analysis Root Cause Analysis Fishbone Diagram Statistical analysis Stakeholder analysis Improvement plan Control plan |
| No source for question. Purpose: check if other aspects of the training will be used/are used | Q12. Apart from the GLSS tools above, what are other things you learned and currently use in your job? (insights, concepts theory, best practice, reduce reuse recycle, new contacts) Open question |
| No source for question. Purpose: check if there are any items missing in the training | Q13. What are the tools that you missed in the training? |
| “What do you see as the major reasons you took this course?” Kirkpatrick and Kirkpatrick ([14] p. 93) (Table 11.8). | No changes |
| “How can this program be improved? “ Kirkpatrick and Kirkpatrick ([14], p. 89) (Table 11.6). | Q14. What suggestions do you have to improve the training program? |
| “Please give an example of a positive outcome you have experienced since attending this training”, Kirkpatrick and Kirkpatrick ([14], p. 107). | Q15. Please mention any achievements you realized as a result of you following this training outside of you direct daily job (e.g., inspiring other departments, starting a green team. |
| “Overall, I am happy with how the program went? (Yes/No) Comments:” Kirkpatrick and Kirkpatrick ([14], p. 92) (Table 11.7). | No changes |
| “Please share any additional comments you may have?” Kirkpatrick and Kirkpatrick ([14], p. 89) (Table 11.6). | No changes |
References
- Van Daalen, K.R.; Romanello, M.; Rocklöv, J.; Semenza, J.C.; Tonne, C.; Markandya, A.; Dasandi, N.; Jankin, S.; Achebak, H.; Ballester, J.; et al. The 2022 Europe Report of the Lancet Countdown on Health and Climate Change: Towards a Climate Resilient Future. Lancet Public Health 2022, 7, e942–e965. [Google Scholar] [CrossRef]
- Trakulsunti, Y.; Antony, J.; Douglas, J.A. Lean Six Sigma Implementation and Sustainability Roadmap for Reducing Medication Errors in Hospitals. TQM J. 2020, 33, 33–55. [Google Scholar] [CrossRef]
- Zhu, Q.; Johnson, S.; Sarkis, J. Lean Six Sigma and Environmental Sustainability: A Hospital Perspective. Supply Chain Forum Int. J. 2018, 19, 25–41. [Google Scholar] [CrossRef]
- Farrukh, A.; Mathrani, S.; Taskin, N. Investigating the Theoretical Constructs of a Green Lean Six Sigma Approach towards Environmental Sustainability: A Systematic Literature Review and Future Directions. Sustainability 2020, 12, 8247. [Google Scholar] [CrossRef]
- McDermott, O.; Antony, J.; Bhat, S.; Jayaraman, R.; Rosa, A.; Marolla, G.; Parida, R. Lean Six Sigma in Healthcare: A Systematic Literature Review on Motivations and Benefits. Processes 2022, 10, 1910. [Google Scholar] [CrossRef]
- Rathi, R.; Vakharia, A.; Shadab, M. Lean Six Sigma in the Healthcare Sector: A Systematic Literature Review. Mater. Today Proc. 2022, 50, 773–781. [Google Scholar] [CrossRef]
- Garza-Reyes, J.A. Green Lean and the Need for Six Sigma. Int. J. Lean Six Sigma 2015, 6, 226–248. [Google Scholar] [CrossRef]
- Cherrafi, A.; Elfezazi, S.; Govindan, K.; Garza-Reyes, J.A.; Benhida, K.; Mokhlis, A. A Framework for the Integration of Green and Lean Six Sigma for Superior Sustainability Performance. Int. J. Prod. Res. 2017, 55, 4481–4515. [Google Scholar] [CrossRef]
- Erdil, N.O.; Aktas, C.B.; Arani, O.M. Embedding Sustainability in Lean Six Sigma Efforts. J. Clean. Prod. 2018, 198, 520–529. [Google Scholar] [CrossRef]
- Gholami, H.; Jamil, N.; Mat Saman, M.Z.; Streimikiene, D.; Sharif, S.; Zakuan, N. The Application of Green Lean Six Sigma. Bus. Strat. Env. 2021, 30, 1913–1931. [Google Scholar] [CrossRef]
- Kaswan, M.S.; Rathi, R.; Garza-Reyes, J.A.; Antony, J. Green Lean Six Sigma Sustainability—Oriented Project Selection and Implementation Framework for Manufacturing Industry. Int. J. Lean Six Sigma 2023, 14, 33–71. [Google Scholar] [CrossRef]
- Sijm-Eeken, M.; Jaspers, M.; Peute, L. Training Healthcare Professionals to Mitigate the Climate Challenge—Development of a Lean Six Sigma E-Learning. In Studies in Health Technology and Informatics; Mantas, J., Gallos, P., Zoulias, E., Hasman, A., Househ, M.S., Charalampidou, M., Magdalinou, A., Eds.; IOS Press: Amsterdam, The Netherlands, 2023. [Google Scholar] [CrossRef]
- Maltby, J.; Williams, G.; Mcgarry, J.; Day, L. Research Methods for Nursing and Healthcare; Routledge: London, UK, 2014. [Google Scholar]
- Kirkpatrick, J.D.; Kirkpatrick, W.K. Kirkpatrick’s Four Levels of Training Evaluation; ATD Press: Alexandria, VA, USA, 2016. [Google Scholar]
- Alsalamah, A.; Callinan, C. Adaptation of Kirkpatrick’s Four-Level Model of Training Criteria to Evaluate Training Programmes for Head Teachers. Educ. Sci. 2021, 11, 116. [Google Scholar] [CrossRef]
- Kirkpatrick, D.L. The Four Levels of Evaluation. In Evaluating Corporate Training: Models and Issues; Brown, S.M., Seidner, C.J., Eds.; Springer: Dordrecht, The Netherlands, 1998; pp. 95–112. [Google Scholar] [CrossRef]
- Prats, E.V. WHO Guidance for Climate-Resilient and Environmentally Sustainable Health Care Facilities; World Health Organization: Geneva, Switserland, 2020. [Google Scholar]
- Cook, J.V.; Dickinson, H.O.; Eccles, M.P. Response rates in postal surveys of healthcare professionals between 1996 and 2005: An observational study. BMC Health Serv Res. 2009, 9, 160. [Google Scholar] [CrossRef]
- Yadav, V.; Kaswan, M.S.; Gahlot, P.; Duhan, R.K.; Garza-Reyes, J.A.; Rathi, R.; Chaudhary, R.; Yadav, G. Green Lean Six Sigma for sustainability improvement: A systematic review and future research agenda. Int. J. Lean Six Sigma 2023, 14, 759–790. [Google Scholar] [CrossRef]
- Lee, S.M.; Lee, D. Developing Green Healthcare Activities in the Total Quality Management Framework. Int. J. Environ. Res. Public Health 2022, 19, 6504. [Google Scholar] [CrossRef]
- Letchumanan, L.T.; Gholami, H.; Yusof, N.M.; Ngadiman, N.H.A.B.; Salameh, A.A.; Štreimikienė, D.; Cavallaro, F. Analyzing the Factors Enabling Green Lean Six Sigma Implementation in the Industry 4.0 Era. Sustainability 2022, 14, 3450. [Google Scholar] [CrossRef]
- Mishra, M.N. Identify Critical Success Factors to Implement Integrated Green and Lean Six Sigma. Int. J. Lean Six Sigma 2022, 13, 765–777. [Google Scholar] [CrossRef]
- Kumar, S.; Kumar, N.; Haleem, A. Conceptualisation of Sustainable Green Lean Six Sigma: An Empirical Analysis. Int. J. Bus. Excell. 2015, 8, 210. [Google Scholar] [CrossRef]
- Sijm-Eeken, M.; Jaspers, M.; Peute, L. Identifying Environmental Impact Factors for Sustainable Healthcare: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 6747. [Google Scholar] [CrossRef]
- Kotter, J. Leading Change; Harvard Business Review Press: Boston, MA, USA, 2012. [Google Scholar]
- Kubiak, T.M. The Certified Six Sigma Master Black Belt Handbook; ASQ Quality Press: Milwaukee, WI, USA, 2012. [Google Scholar]
- Jin, H.; Qu, P.; Zhou, Y.; Qu, Q.; Li, H. Green Lean Six Sigma practice in the industrial and service sectors: From the systematic literature review to an integration diagram. Prod. Plan. Control. 2024, 1–26. [Google Scholar] [CrossRef]
- American Society for Quality. The ASQ Certified CSSGB Six Sigma Green Belt Body of Knowledge; American Society for Quality: Milwaukee, WI, USA, 2014. [Google Scholar]
- Kumari, S.; Gautam, H.; Nityadarshini, N.; Das, B.K.; Chaudhry, R. Online Classes versus Traditional Classes? Comparison during COVID-19. J. Educ. Health Promot. 2021, 10, 457. [Google Scholar] [CrossRef]
- Laux, C.; Mary, E.J.; Paul, C. LSS Green Belt Projects Planned versus Actual Duration. J. Technol. Manag. Appl. Eng. 2015, 31. Available online: https://www.iastatedigitalpress.com/jtmae/article/14139/galley/12903/view/ (accessed on 9 March 2024).


| Number of Participants (Total N = 21) | Percentage of Participants | |
|---|---|---|
| Age | ||
| 20–25 | 2 | 9.5% |
| 26–35 | 9 | 42.9% |
| 36–45 | 4 | 19.0% |
| 45+ | 6 | 28.6% |
| Gender at birth | ||
| Female | 15 | 71.4 |
| Male | 6 | 28.6% |
| Education level | ||
| Intermediate Vocational | 1 | 4.8% |
| Higher Vocational | 8 | 38.1% |
| Academic | 12 | 57.1% |
| Work organization | ||
| Academic hospital | 15 | 71.4% |
| General hospital | 3 | 14.3% |
| Nursing home | 2 | 9.5% |
| Pharmaceutical company | 1 | 4.8% |
| Experience with process improvement | ||
| Low | 12 | 57.1% |
| Medium | 6 | 28.1% |
| High | 3 | 14.3% |
| Question | All Participants (N = 21, 100%) | Subgroup | Variance between Groups (p-Value) 1 | ||
|---|---|---|---|---|---|
| Not Applied GLSS (N = 5, 24%) | Applied GLSS without Completing Project (N = 7, 33%) | Completed GLSS Project (N = 9, 43%) | |||
| Age–Mean (SD) | 37.1 (8.8) | 38.2 (8.6) | 35.3 (8.1) | 37.9 (10.1) | 0.815 |
| Gender, N(%) male | 6 (29%) | 2 (40%) | 0 (0%) | 4 (44%) | - |
| Higher/Academic Education—N (% of group) | 20 (95%) | 5 (100%) | 6 (86%) | 9 (100%) | - |
| Involved in direct patient care—N (% of group) | 10 (48%) | 3 (60%) | 5 (71%) | 2 (22%) | - |
| Academic hospital—N (% of group) | 14 (67%) | 3 (60%) | 4 (57%) | 7 (78%) | - |
| Experience level process improvement 2 | 2.5 (1.0) | 2.2 (0.5) | 2.4 (1.0) | 2.7 (1.3) | 0.732 |
| Question | All Participants (N = 21, 100%) | Subgroup | Variance between Groups (p-Value) 1 | ||
|---|---|---|---|---|---|
| Not Applied GLSS (N = 5, 24%) | Applied GLSS without Completing Project (N = 7, 33%) | Completed GLSS Project (N = 9, 43%) | |||
| Enjoyed the training 2 | 4.1 (0.8) | 4.5 (1.0) | 4.2 (0.8) | 3.9 (0.8) | 0.468 |
| Motivated to apply GLSS 2 | 4.3 (0.8) | 3.7 (0.6) | 4.2 (1.0) | 4.7 (0.7) | 0.173 |
| Motivated to compete GLSS project 2 | 3.7 (1.3) | 3.0 (1.8) | 4.3 (1.0) | 3.7 (1.2) | 0.307 |
| Training difficulty too high- N (% of group) | 8 (38%) | 2 (40%) | 2 (29%) | 4 (44%) | - |
| Question | All Participants (N = 21, 100%) | Subgroup | Variance between Groups (p-Value) 1 | ||
|---|---|---|---|---|---|
| Not Applied GLSS (N = 5, 24%) | Applied GLSS without Completing Project (N = 7, 33%) | Completed GLSS Project (N = 9, 43%) | |||
| Q1. The training program inspired me to improve my achievement in making healthcare green 2 | 4.0 (0.8) | 3.6 (0.5) | 4.0 (0.9) | 4.1 (0.9) | 0.557 |
| Q2. The training program increased my ability to perform well in my job role 2 | 3.2 (1.0) | 3.2 (0.8) | 2.7 (0.8) | 3.6 (1.1) | 0.244 |
| Q3. While performing my job, my behavior changed after completing the program 2 | 3.0 (1.0) | 3.2 (1.1) | 2.7 (0.5) | 3.2 (0.8) | 0.564 |
| Q4. I feel confident about applying what I have learned on the job 2 | 3.0 (0.9) | 2.6 (1.1) | 2.7 (0.5) | 3.6 (0.9) | 0.083 |
| Number of GLSS tools applied | 3.2 (3.7) | 0 (0.0) | 1.8 (0.9) | 6 (4.2) | 0.003 |
| Number of GLSS tools expected to apply in future (SD) | 7.6 (4.8) | 3.8 (5.8) | 7.4 (3.3) | 9.8 (4.3) | 0.076 |
| Participant ID | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Project Charter | # | # | * | # | # | # | ^ | ? | # | ~ | # | ? | ^ | # | * | ^ | # | # | ? | ^ | # |
| SIPOC | * | ^ | * | # | ^ | # | ^ | ? | ? | ~ | # | ? | ^ | # | * | ^ | # | * | ? | * | ^ |
| Critical to Quality Tree | * | ^ | * | # | * | * | ^ | ? | ? | ~ | ? | ? | * | # | * | * | ? | ~ | ? | ^ | ^ |
| Lifecycle Assessment | * | # | * | * | ^ | ^ | ^ | ^ | ? | ^ | ~ | * | ^ | # | ^ | * | # | * | ? | ^ | # |
| Process Mapping | * | # | * | * | * | ^ | ^ | ? | ? | ~ | ^ | ^ | ^ | ^ | ^ | * | ? | * | ? | ^ | * |
| DOTWIMP | * | * | * | * | ^ | ^ | ^ | ? | * | ~ | ~ | ? | ~ | # | ^ | * | ? | * | ? | ^ | # |
| 5S | ^ | * | ^ | * | ^ | ^ | ^ | ? | * | ~ | ^ | ? | * | ^ | * | * | ? | * | ? | ^ | # |
| Value Add Analysis | ^ | # | * | ~ | ? | ^ | ^ | ? | * | ~ | ^ | ? | * | ~ | * | * | # | ~ | ? | ^ | ^ |
| Root Cause Analysis | ^ | # | # | ^ | ^ | ^ | ^ | ? | ? | ~ | # | ? | ^ | * | ^ | * | # | ^ | ? | # | ^ |
| Fishbone Diagram | * | ^ | # | ^ | * | ^ | ^ | ? | ? | ~ | # | * | ^ | * | ^ | * | ? | ^ | ? | ^ | # |
| Statistical analysis | ^ | # | * | ~ | ? | ^ | ^ | ? | ~ | ? | ? | * | * | # | ^ | ~ | ? | * | ? | # | * |
| Stakeholder analysis | ^ | ^ | * | * | * | ^ | ^ | ? | ~ | * | # | ^ | * | # | # | ^ | # | # | ? | # | # |
| Improvement plan | ^ | # | * | ^ | ^ | ^ | ^ | ? | ? | ? | # | # | # | # | ^ | * | # | # | ? | ^ | # |
| Control plan | ^ | ^ | * | ^ | ^ | ^ | ^ | ? | ? | ? | ? | ^ | # | * | ^ | * | ? | # | ? | ^ | # |
| Achievement in Participant Organization | Frequency |
| Reduce use of products and/or materials (and waste) | 7 |
| Creating awareness on our impact on the environment | 5 |
| Green choices in procurement/ Replace disposable by reusable products | 3 |
| Cost reduction | 3 |
| Separation of waste types for recycling improved | 3 |
| Join Green Team | 1 |
| Energy reduction | 1 |
| Reduce travel | 1 |
| Reduction of waiting time | 1 |
| Reducing workload of employees | 1 |
| Reducing defects (errors/mistakes) | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sijm-Eeken, M.; Greif, A.; Peute, L.; Jaspers, M. Implementation of Green Lean Six Sigma in Dutch Healthcare: A Qualitative Study of Healthcare Professionals’ Experiences. Nurs. Rep. 2024, 14, 2877-2895. https://doi.org/10.3390/nursrep14040210
Sijm-Eeken M, Greif A, Peute L, Jaspers M. Implementation of Green Lean Six Sigma in Dutch Healthcare: A Qualitative Study of Healthcare Professionals’ Experiences. Nursing Reports. 2024; 14(4):2877-2895. https://doi.org/10.3390/nursrep14040210
Chicago/Turabian StyleSijm-Eeken, Marieke, Annick Greif, Linda Peute, and Monique Jaspers. 2024. "Implementation of Green Lean Six Sigma in Dutch Healthcare: A Qualitative Study of Healthcare Professionals’ Experiences" Nursing Reports 14, no. 4: 2877-2895. https://doi.org/10.3390/nursrep14040210
APA StyleSijm-Eeken, M., Greif, A., Peute, L., & Jaspers, M. (2024). Implementation of Green Lean Six Sigma in Dutch Healthcare: A Qualitative Study of Healthcare Professionals’ Experiences. Nursing Reports, 14(4), 2877-2895. https://doi.org/10.3390/nursrep14040210







