Intrahospital Handovers before and after the Implementation of ISBAR Communication: A Quality Improvement Study on ICU Nurses’ Handovers to General Medical Ward Nurses
Abstract
1. Introduction
2. Aim
3. Materials and Methods
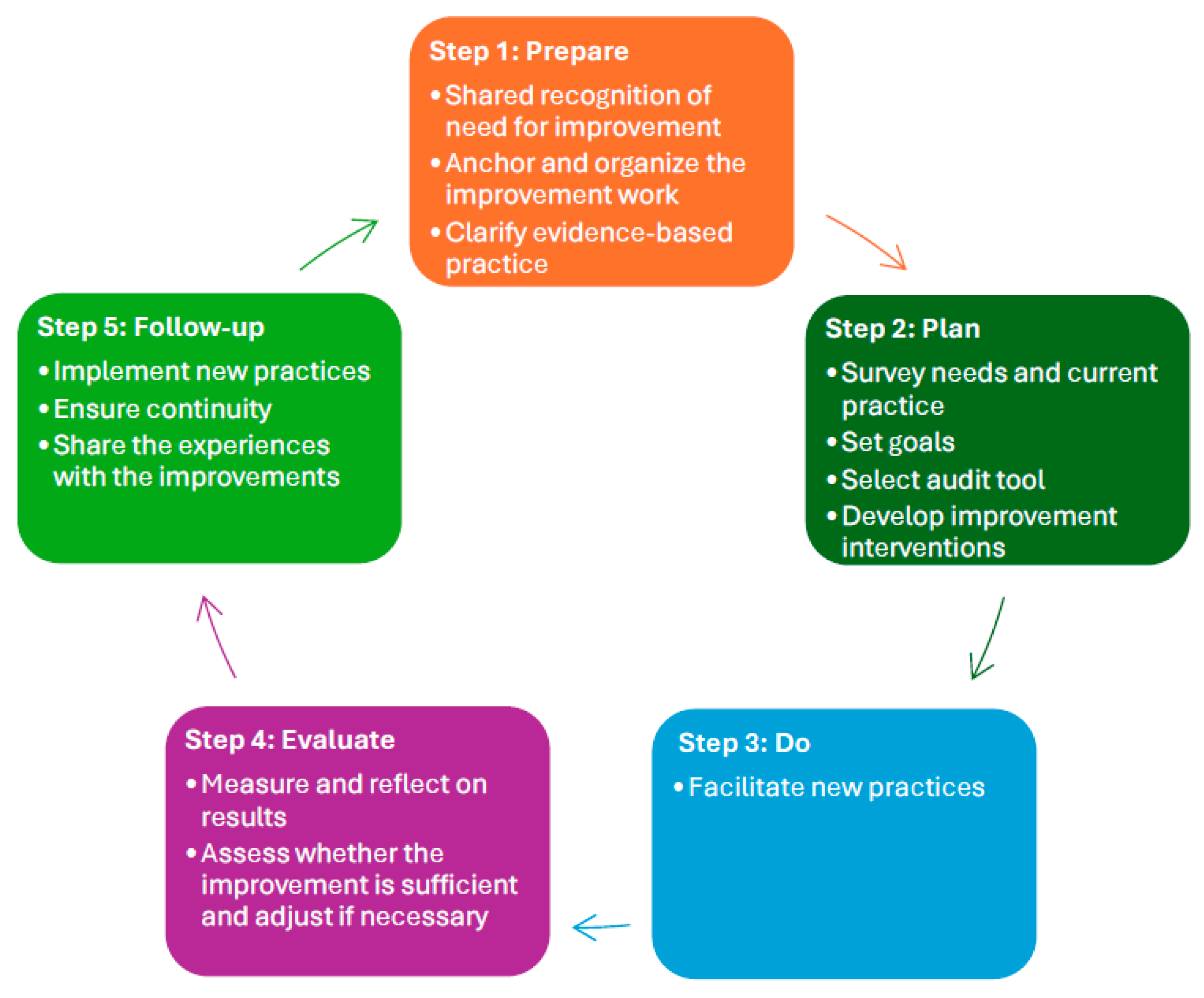
3.1. Design
3.2. Quality Improvement Method
3.3. Setting
3.4. Sample and Recruitment
3.5. Inclusion Criteria
3.6. The ISBAR Intervention
3.7. Instrument
3.8. Statistical Analysis
3.9. Ethical Considerations
4. Results
4.1. Adherence to the 26 Items in the ISBAR Scoring Tool
| Domain | ISBAR Items | Baseline (n = 25) N (%) | Post-Int (n = 25) N (%) | Difference | p-Value |
|---|---|---|---|---|---|
| Identification | 1. State patients name | 20 (80) | 24 (96) | 4 (16%) | 0.189 b |
| 2. State year of birth | 20 (80) | 23 (92) | 3 (12%) | 1.00 b | |
| Situation | 3. State reason for admission | 25 (100) | 24 (96) | −1 (−4%) | 1.00 b |
| 4. State date of admission | 23 (92) | 22 (88) | −1 (−4%) | 1.00 b | |
| 5. Give a brief summary of the treatment provided | 23 (92) | 25 (100) | 2 (8%) | 0.490 b | |
| 6. State current condition | 22 (88) | 25 (100) | 3 (12%) | 0.235 b | |
| 7. State any infection and type of isolation | 10 (40) | 4 (16) | −6 (−24%) | 0.114 b | |
| Background | 8. State previous illnesses of significance | 23 (92) | 22 (88) | −1 (−4%) | 1.00 b |
| 9. List medications of importance | 22 (88) | 21 (84) | −1 (−4%) | 1.00 b | |
| 10. State allergy if relevant | 1 (4) | 1 (4) | 0 (0%) | 1.00 b | |
| 11. Indicate significant psychological and cognitive state | 17 (68) | 20 (80) | 3 (12%) | 0.333 a | |
| 12. State physical function level and mobilisation status | 21 (84) | 22 (88) | 1 (4%) | 1.00 b | |
| 13. State care needs and any dialogue with the municipality | 16 (64) | 16 (64) | 0 (0%) | 1.00 a | |
| 14. State special conditions for relatives (children < 18 years) | 6 (24) | 8 (32) | 2 (8%) | 0.529 a | |
| Assessment Airway Breathing | 15. State observations (SaO2, RR, expectorate, blood gas) | 22 (88) | 20 (80) | −2 (−8%) | 0.702 b |
| 16. State treatment (O2 supplementation, inhalations, PEP/PEEP, pulmonary physiotherapy) | 19 (76) | 20 (80) | 1 (4%) | 0.733 a | |
| Circulation | 17. State observations (BP, HR, temperature, diuresis) | 23 (92) | 23 (92) | 0 (0%) | 1.00 b |
| 18. State treatment (IV accesses, IV treatment/infusion) | 18 (72) | 21 (84) | 3 (12%) | 0.306 a | |
| Disability | 19. State observations of level of awareness (GCS/AVPU, pupils, MR/CT, NHISS score) | 7 (28) | 11 (44) | 4 (16%) | 0.239 a |
| Exposure | 20. State elimination status and any treatment | 20 (80) | 20 (80) | 0 (0%) | 1.00 a |
| 21. State nutritional status (diet, nutrition score and treatment) | 18 (72) | 19 (76) | 1 (4%) | 0.747 a | |
| 22. State any pain (VAS and pain treatment) | 11 (44) | 9 (36) | −2 (−8%) | 0.564 a | |
| 23. State any wounds or risk of wounds | 9 (36) | 8 (32) | −1 (−4%) | 0.765 a | |
| 24. If not mentioned earlier, brief summary of examinations (performed/planned) or blood tests | 21 (84) | 20 (80) | −1 (−4%) | 1.00 b | |
| Recommendation | 25. Recommend follow-up treatment | 22 (88) | 22 (88) | 0 (0%) | 1.00 b |
| 26. State any treatment restriction (CPR/respirator minus) | 0 (0) | 3 (12) | 3 (12%) | 0.235 b |
4.2. Adherence to the Structure of the ISBAR Communication
4.3. Time Spent on the Handover
5. Discussion
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
References
- Arora, V.; Farnan, J. Patient Handoffs. UpToDate. 2024. Available online: https://www.uptodate.com/contents/patient-handoffs (accessed on 10 August 2024).
- Flemming, D.; Hübner, U. How to improve change of shift handovers and collaborative grounding and what role does the electronic patient record system play? Results of a systematic literature review. Int. J. Med. Inform. 2013, 82, 580–592. [Google Scholar] [CrossRef] [PubMed]
- Kitch, B.T.; Cooper, J.B.; Zapol, W.M.; Hutter, M.M.; Marder, J.; Karson, A.; Campbell, E.G. Handoffs causing patient harm: A survey of medical and surgical house staff. Jt. Comm. J. Qual. Saf. 2008, 34, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.; Jürgens, J.; Redaèlli, M.; Klingberg, K.; Hautz, W.E.; Stock, S. Impact of the communication and patient hand-off tool SBAR on patient safety: A systematic review. BMJ Open 2018, 8, e022202. [Google Scholar] [CrossRef]
- Segall, N.; Bonifacio, A.S.; Schroeder, R.A.; Barbeito, A.; Rogers, D.; Thornlow, D.K.; Emery, J.; Kellum, S.; Wright, M.C.; Mark, J.B. Can we make postoperative patient handovers safer? A systematic review of the literature. Anesth. Analg. 2012, 115, 102–115. [Google Scholar] [CrossRef]
- World Health Organization. Patient Safety Solutions Preamble; World Health Organization: Geneva, Switzerland, 2007. Available online: https://cdn.who.int/media/docs/default-source/patient-safety/psf/patient-safety-solutions/patient-safety-solutions-preamble.pdf (accessed on 10 August 2024).
- Stewart, K.R. SBAR, Communication, and Patient Safety: An Integrated Literature Review. Departmental Honors Thesis, University of Tennessee at Chattanooga, Chattanooga, TN, USA, 30 March 2016. Available online: https://scholar.utc.edu/honors-theses/66/ (accessed on 15 April 2024).
- Joint Commission International. Communicating Clearly and Effectively to Patients. How to Overcome Common Communication Challenges in Health Care. Available online: https://store.jointcommissioninternational.org/assets/3/7/jci-wp-communicating-clearly-final_(1).pdf (accessed on 5 April 2024).
- Ong, M.S.; Coiera, E. A systematic review of failures in handoff communication during intrahospital transfers. Jt. Comm. J. Qual. Patient Saf. 2011, 37, 274–284. [Google Scholar] [CrossRef]
- Shahid, S.; Thomas, S. Situation, background, assessment, recommendation (SBAR) communication tool for handoff in health care–a narrative review. Saf. Health 2018, 4, 7. [Google Scholar] [CrossRef]
- Foronda, C.; MacWilliams, B.; McArthur, E. Interprofessional communication in healthcare: An integrative review. Nurse Educ. Pract. 2016, 19, 36–40. [Google Scholar] [CrossRef]
- Mannix, T.; Parry, Y.; Roderick, A. Improving clinical handover in a paediatric ward: Implications for nursing management. J. Nurs. Manag. 2017, 25, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Desmedt, M.; Ulenaers, D.; Grosemans, J.; Hellings, J.; Bergs, J. Clinical handover and handoff in healthcare: A systematic review of systematic reviews. Int. J. Qual. Health C 2021, 33, mzaa170. [Google Scholar] [CrossRef]
- Fealy, G.; Donnelly, S.; Doyle, G.; Brenner, M.; Hughes, M.; Mylotte, E.; Nicholson, E.; Zaki, M. Clinical handover practices among healthcare practitioners in acute care services: A qualitative study. J. Clin. Nurs. 2019, 28, 80–88. [Google Scholar] [CrossRef]
- O’Neill, K.; Powell, M.; Lovell, T.; Brown, D.; Walsham, J.; Calleja, P.; Nielsen, S.; Mitchell, M. Improving the handover of complex trauma patients by implementing a standardised process. Aust Crit Care. 2023, 36, 799–805. [Google Scholar] [CrossRef]
- Ahn, J.W.; Jang, H.Y.; Son, Y.J. Critical care nurses’ communication challenges during handovers: A systematic review and qualitative meta-synthesis. J. Nurs. Manag. 2021, 29, 623–634. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.R.; Morgan, L.; Bird, S.; Catchpole, K.; McCulloch, P. Interventions employed to improve intrahospital handover: A systematic review. BMJ Qual. Saf. 2014, 23, 600–607. [Google Scholar] [CrossRef]
- Graan, S.M.; Botti, M.; Wood, B.; Redley, B. Nursing handover from ICU to cardiac ward: Standardised tools to reduce safety risks. Aust. Crit. Care 2016, 29, 165–171. [Google Scholar] [CrossRef]
- Verholen, N.; Vogt, L.; Klasen, M.; Schmidt, M.; Beckers, S.; Marx, G.; Sopka, S. Do digital handover checklists influence the clinical outcome parameters of intensive care unit patients? A randomized controlled pilot study. Front. Med. 2021, 8, 489. [Google Scholar] [CrossRef]
- Lazzara, E.H.; Simonson, R.J.; Gisick, L.M.; Griggs, A.C.; Rickel, E.A.; Wahr, J.; Lane-Fall, M.B.; Keebler, J.R. Does standardisation improve post-operative anaesthesia handoffs? Meta-analyses on provider, patient, organisational, and handoff outcomes. Ergonomics 2022, 65, 1138–1153. [Google Scholar] [CrossRef] [PubMed]
- Finnigan, M.A.; Marshall, S.D.; Flanagan, B.T. ISBAR for clear communication: One hospital’s experience spreading the message. Aust. Health Rev. 2010, 34, 400–404. [Google Scholar] [CrossRef]
- Burgess, A.; Van Diggele, C.; Roberts, C.; Mellis, C. Teaching clinical handover with ISBAR. BMC Med. Educ. 2020, 20, 459. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Patient Safety Curriculum Guide: Multi-Professional Edition; World Health Organization: Geneva, Switzerland, 2011. Available online: https://iris.who.int/handle/10665/44641 (accessed on 1 April 2024).
- Institute for Healthcare Improvement. SBAR Tool: Situation-Background-Assessment-Recommendation. Available online: http://www.ihi.org/resources/Pages/Tools/SBARToolkit.aspx (accessed on 2 June 2024).
- National Health Service. SBAR Communication Tool-Situation, Background, Assessment, Recommendation. Available online: https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/SBAR-Implementation-and-Training-Guide.pdf (accessed on 5 August 2024).
- Kaltoft, A.; Jacobsen, Y.I.; Tangsgaard, M.; Jensen, H.I. ISBAR as a structured tool for patient handover during postoperative recovery. J. Perianesth. Nurs. 2022, 37, 34–39. [Google Scholar] [CrossRef]
- Randmaa, M.; Mårtensson, G.; Swenne, C.L.; Engström, M. SBAR improves communication and safety climate and decreases incident reports due to communication errors in an anaesthetic clinic: A prospective intervention study. BMJ Open 2014, 4, e004268. [Google Scholar] [CrossRef]
- Blom, L. The situation, background, assessment and recommendation (SBAR) model for communication between health care professionals: A clinical intervention pilot study. Int. J. Caring Sci. 2015, 8, 530. [Google Scholar]
- Pun, J. Using a simulation-based approach to promote structured and interactive nursing clinical handover: A pre-and post-evaluation pilot study in bilingual Hong Kong. BMC Nurs. 2023, 22, 38. [Google Scholar] [CrossRef] [PubMed]
- Haddeland, K.; Marthinsen, G.N.; Söderhamn, U.; Flateland, S.M.; Moi, E.M. Experiences of using the ISBAR tool after an intervention: A focus group study among critical care nurses and anaesthesiologists. Intensiv. Crit. Care Nur. 2022, 70, 103195. [Google Scholar] [CrossRef]
- Abbaszade, A.; Assarroudi, A.; Armat, M.R.; Stewart, J.J.D.; Rakhshani, M.H.; Sefidi, N.M.; Sahebkar, M. Evaluation of the impact of handoff based on the SBAR technique on quality of nursing care. J. Nurs. Care Qual. 2021, 36, E38–E43. [Google Scholar] [CrossRef] [PubMed]
- Chaica, V.; Marques, R.; Pontífice-Sousa, P. ISBAR: A Handover Nursing Strategy in Emergency Departments, Scoping Review. Healthcare 2024, 12, 399. [Google Scholar] [CrossRef] [PubMed]
- Lazzari, C. Implementing the Verbal and Electronic Handover in General and Psychiatric Nursing Using the Introduction, Situation, Background, Assessment, and Recommendation Framework: A Systematic Review. Iran. J. Nurs. Midwifery Res. 2024, 29, 23–32. [Google Scholar] [PubMed]
- Leonardsen, A.-C.; Moen, E.K.; Karlsøen, G.; Hovland, T. A quantitative study on personnel’s experiences with patient handovers between the operating room and the postoperative anesthesia care unit before and after the implementation of a structured communication tool. Nurs. Rep. 2019, 9, 8041. [Google Scholar] [CrossRef]
- Lo, L.; Rotteau, L.; Shojania, K. Can SBAR be implemented with high fidelity and does it improve communication between healthcare workers? A systematic review. BMJ Open 2021, 11, e055247. [Google Scholar] [CrossRef]
- Bunkenborg, G.; Bitsch Hansen, T.; Hølge-Hazelton, B. Handing over patients from the ICU to the general ward: A focused ethnographical study of nurses’ communication practice. J. Adv. Nurs. 2017, 73, 3090–3101. [Google Scholar] [CrossRef]
- Whittaker, J.; Ball, C. Discharge from intensive care: A view from the ward. Intensiv. Crit. Care Nur. 2000, 16, 135–143. [Google Scholar] [CrossRef]
- Enger, R.; Andershed, B. Nurses’ experience of the transfer of ICU patients to general wards: A great responsibility and a huge challenge. J. Clin. Nurs. 2018, 27, e186–e194. [Google Scholar] [CrossRef]
- Wibrandt, I.; Lippert, A. Improving patient safety in handover from intensive care unit to general ward: A systematic review. J. Patient Saf. 2020, 16, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Bressan, V.; Mio, M.; Palese, A. Nursing handovers and patient safety: Findings from an umbrella review. J. Adv. Nurs. 2020, 76, 927–938. [Google Scholar] [CrossRef] [PubMed]
- Buus, N.; Hoeck, B.; Hamilton, B.E. Nurses’ shift reports: A systematic literature search and critical review of qualitative field studies. J. Clin. Nurs. 2017, 26, 2891–2906. [Google Scholar] [CrossRef] [PubMed]
- Spooner, A.; Aitken, L.; Corley, A.; Fraser, J.; Chaboyer, W. Nursing team leader handover in the intensive care unit contains diverse and inconsistent content: An observational study. Int. J. Nurs. Stud. 2016, 61, 165–172. [Google Scholar] [CrossRef]
- Tangvik, L.S.; Kinn-Mikalsen, M.A.; Johnsgaard, T.; Reime, M.H. Observasjonsskjema for måling av ISBAR. Observation form for measuring ISBAR. Inspira 2020, 15, 5–13. [Google Scholar] [CrossRef]
- Ogrinc, G.; Davies, L.; Goodman, D.; Batalden, P.; Davidoff, F.; Stevens, D. SQUIRE 2.0 (S tandards for QU ality I mprovement R eporting E xcellence): Revised publication guidelines from a detailed consensus process. J. Contin. Educ. Nurs. 2015, 46, 501–507. [Google Scholar] [CrossRef]
- Langley, G.J.; Moen, R.D.; Nolan, K.M.; Nolan, T.W.; Norman, C.L.; Provost, L.P. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Helsedirektoratet. Veileder til Forskrift om Ledelse og Kvalitetsforbedring i Helse-og Omsorgstjenesten. Available online: https://www.helsedirektoratet.no/veiledere/ledelse-og-kvalitetsforbedring-i-helse-og-omsorgstjenesten (accessed on 1 August 2024).
- Helsebiblioteket. Modell for Kvalitetsforbedring. 2021. Available online: https://www.helsebiblioteket.no/innhold/artikler/kvalitetsforbedring/kvalitetsforbedring#oversikt-over-metoder-og-verktoy-overordnede-metoder-modell-for-kvalitetsforbedring (accessed on 1 August 2024).
- Helsedirektoratet. Tidlig Oppdagelse og Rask Respons ved Forverret Somatisk Tilstand-Nasjonale Faglige Råd. Available online: https://www.helsedirektoratet.no/faglige-rad/tidlig-oppdagelse-og-rask-respons-ved-forverret-somatisk-tilstand/om-de-faglige-radene-del-av-i-trygge-hender-24-7 (accessed on 10 April 2024).
- Herling, S.F.; Brix, H.; Andersen, L.; Jensen, L.D.; Handesten, R.; Knudsen, H.; Bove, D.G. A qualitative study portraying nurses’ perspectives on transitional care between intensive care units and hospitals wards. Scand. J. Caring Sci. 2022, 36, 947–956. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2017; Volume 10. [Google Scholar]
- Cantín, M. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. Reviewing the latest version. Int. J. Med. Surg. 2014, 1, 339–346. [Google Scholar] [CrossRef]
- Fischer, F.; Lange, K.; Klose, K.; Greiner, W.; Kraemer, A. Barriers and strategies in guideline implementation—A scoping review. Healthcare 2016, 4, 36. [Google Scholar] [CrossRef] [PubMed]
- Elliott, M.; Worrall-Carter, L.; Page, K. Intensive care readmission: A contemporary review of the literature. Intensiv. Crit. Care Nur. 2014, 30, 121–137. [Google Scholar] [CrossRef] [PubMed]
- Kellett, J.; Sebat, F. Make vital signs great again—A call for action. Eur. J. Intern. Med. 2017, 45, 13–19. [Google Scholar] [CrossRef]
- Beigmoradi, S.; Pourshirvani, A.; Pazokian, M.; Nasiri, M. Evaluation of nursing handoff skill among nurses using situation-background-assessment-recommendation checklist in general wards. Evid. Based Care 2019, 9, 63–68. [Google Scholar] [CrossRef]
- Helsedirektoratet. Meldeordningen for Uønskede Hendelser i Spesialisthelsetjenesten. Årsrapport. 2017. Available online: https://www.helsedirektoratet.no/rapporter/meldeordningene-arsrapporter/%C3%85rsrapport%202017%20Meldeordningene.pdf/_/attachment/inline/31a9b3cc-e5f1-4835-8d6a-dd6be52d36ab:499880da53042b4e352d83b0abb6daec179bf644/%C3%85rsrapport%202017%20Meldeordningene.pdf (accessed on 5 April 2024).
- Helsedirektoratet. Tiltakspakke for Tidlig Oppdagelse av Forverret Tilstand. 2018. Available online: https://pasientsikkerhetsprogrammet.no/om-oss/innsatsomrader/tidlig-oppdagelse-av-forverret-tilstand/_/attachment/inline/8f4cc88e-8b93-4cb4-a359-38dbd0336c9a:c8f15b3a356e409fb5c56d983f1484bcd39e2b50/tiltakspakke-for-tidlig-oppdagelse-av-forverret-tilstand-sykehjem.pdf (accessed on 10 April 2024).
- Smith, G.; Redfern, O.; Pimentel, M.; Gerry, S.; Collins, G.; Malycha, J.; Prytherch, D.; Schmidt, P.; Watkinson, P. The national early warning score 2 (NEWS2). Clin. Med. 2019, 19, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Häggström, M.; Fjellner, C.; Öhman, M.; Holmström, M.R. Ward visits-one essential step in intensive care follow-up. An interview study with critical care nurses’ and ward nurses’. Intensiv. Crit. Care Nur. 2018, 49, 21–27. [Google Scholar] [CrossRef]
- Doğu, C.; Doğan, G.; Kayir, S.; Yağan, Ö. Importance of the National Early Warning Score (NEWS) at the time of discharge from the intensive care unit. Turk. J. Med. Sci. 2020, 50, 1203–1209. [Google Scholar] [CrossRef] [PubMed]
- Klepstad, P.K.; Nordseth, T.; Sikora, N.; Klepstad, P. Use of National Early Warning Score for observation for increased risk for clinical deterioration during post-ICU care at a surgical ward. Ther. Clin. Risk Manag. 2019, 15, 315–322. [Google Scholar] [CrossRef]
- Uppanisakorn, S.; Bhurayanontachai, R.; Boonyarat, J.; Kaewpradit, J. National Early Warning Score (NEWS) at ICU discharge can predict early clinical deterioration after ICU transfer. J. Crit. Care 2018, 43, 225–229. [Google Scholar] [CrossRef]
- Flaatten, H.; Beil, M.; Guidet, B. Elderly patients in the intensive care unit. In Seminars in Respiratory and Critical Care Medicine; Thieme Medical Publishers: New York, NY, USA, 2020; Volume 1, pp. 10–19. [Google Scholar]
- Cornell, P.; Gervis, M.T.; Yates, L.; Vardaman, J.M. Improving shift report focus and consistency with the situation, background, assessment, recommendation protocol. JONA 2013, 43, 422–428. [Google Scholar] [CrossRef]
- Uhm, J.Y.; Lim, E.Y.; Hyeong, J. The impact of a standardized inter-department handover on nurses’ perceptions and performance in Republic of Korea. J. Nurs. Manag. 2018, 26, 933–944. [Google Scholar] [CrossRef]
- Petrovic, M.A.; Aboumatar, H.; Scholl, A.T.; Gill, R.S.; Krenzischek, D.A.; Camp, M.S.; Senger, C.M.; Deng, Y.; Chang, T.Y.; Xie, Y.; et al. The perioperative handoff protocol: Evaluating impacts on handoff defects and provider satisfaction in adult perianesthesia care units. J. Clin. Anesth. 2015, 27, 111–119. [Google Scholar] [CrossRef]
- Reason, J. Human error: Models and management. BMJ 2000, 320, 768–770. [Google Scholar] [CrossRef] [PubMed]
- James, S.; Quirke, S.; McBride-Henry, K. Staff perception of patient discharge from ICU to ward-based care. Nurs. Crit. Care 2013, 18, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Tangvik, L.; Kinn-Mikalsen MAJohnsgaard, T.; Reime, M. The experiences of registered nurses and specialist ICU nurses before and after implementation of ISBAR—A survey. Sykepl. Forsk. 2021, 16, e87550. [Google Scholar] [CrossRef]
- Manias, E.; Geddes, F.; Watson, B.; Jones, D.; Della, P. Perspectives of clinical handover processes: A multi-site survey across different health professionals. J. Clin. Nurs. 2016, 25, 80–91. [Google Scholar] [CrossRef]
| Mean (Seconds) | Median (Seconds) | Percentiles (25–75%) | p-Value | |
|---|---|---|---|---|
| Baseline | 293 | 277 | 93–591 | 0.184 a |
| Post-intervention | 246 | 216 | 70–592 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reime, M.H.; Tangvik, L.S.; Kinn-Mikalsen, M.A.; Johnsgaard, T. Intrahospital Handovers before and after the Implementation of ISBAR Communication: A Quality Improvement Study on ICU Nurses’ Handovers to General Medical Ward Nurses. Nurs. Rep. 2024, 14, 2072-2083. https://doi.org/10.3390/nursrep14030154
Reime MH, Tangvik LS, Kinn-Mikalsen MA, Johnsgaard T. Intrahospital Handovers before and after the Implementation of ISBAR Communication: A Quality Improvement Study on ICU Nurses’ Handovers to General Medical Ward Nurses. Nursing Reports. 2024; 14(3):2072-2083. https://doi.org/10.3390/nursrep14030154
Chicago/Turabian StyleReime, Marit Hegg, Linda Skaug Tangvik, Mats Aleksander Kinn-Mikalsen, and Tone Johnsgaard. 2024. "Intrahospital Handovers before and after the Implementation of ISBAR Communication: A Quality Improvement Study on ICU Nurses’ Handovers to General Medical Ward Nurses" Nursing Reports 14, no. 3: 2072-2083. https://doi.org/10.3390/nursrep14030154
APA StyleReime, M. H., Tangvik, L. S., Kinn-Mikalsen, M. A., & Johnsgaard, T. (2024). Intrahospital Handovers before and after the Implementation of ISBAR Communication: A Quality Improvement Study on ICU Nurses’ Handovers to General Medical Ward Nurses. Nursing Reports, 14(3), 2072-2083. https://doi.org/10.3390/nursrep14030154






