Facilitators and Barriers to Receiving Palliative Care in People with Kidney Disease: Predictive Factors from an International Nursing Perspective
Abstract
1. Introduction
2. Literature Review
- to investigate the facilitators and barriers to PC in people with kidney disease from the perspective of renal nurses;
- to explore predictive factors associated with these perceived facilitators and barriers.
3. Materials and Methods
3.1. Participants
3.2. Ethical Consideration
3.3. Statistical Analysis
4. Results
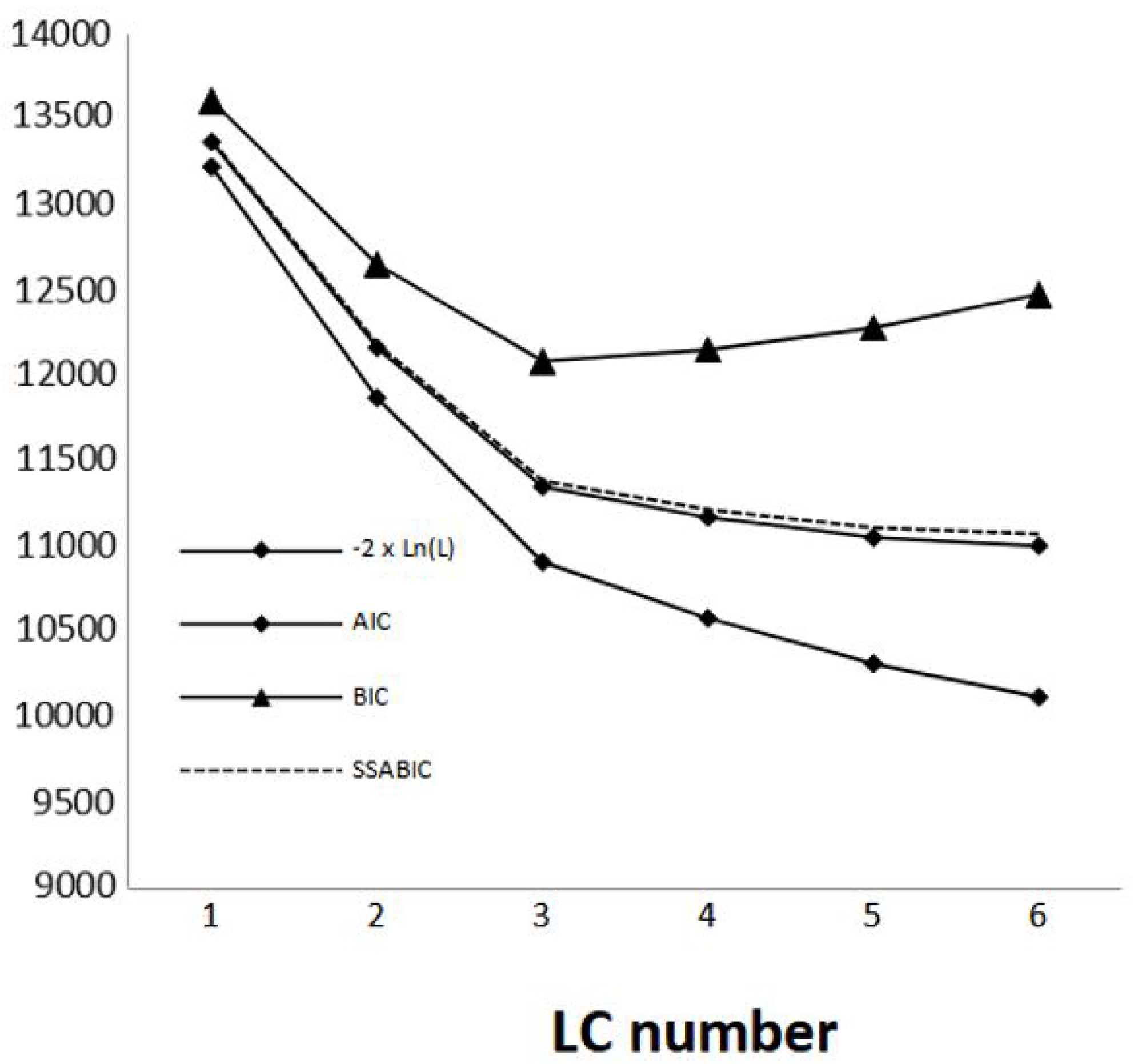
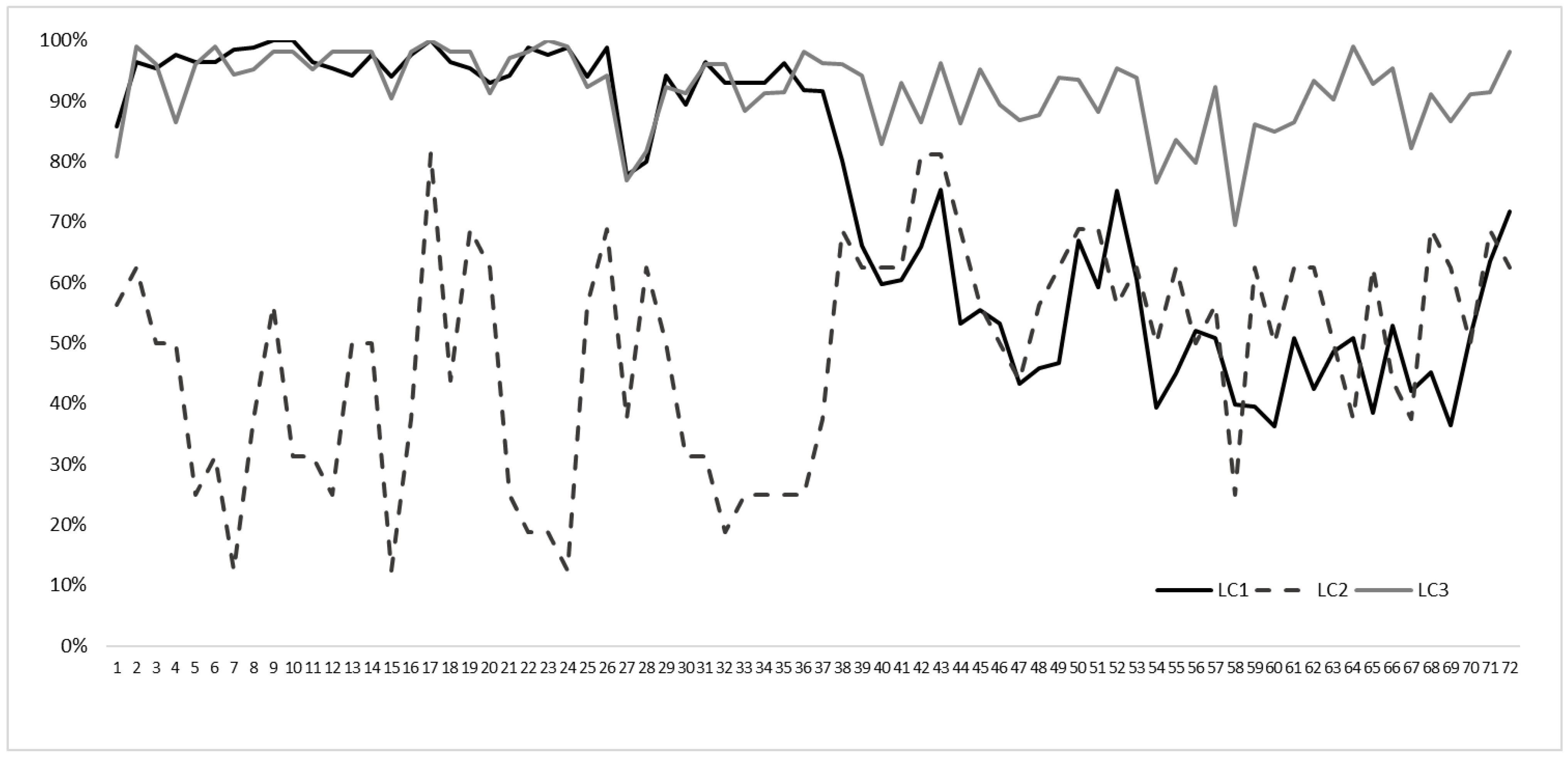
Latent Class Analysis
5. Discussion
5.1. Limitations
5.2. Implications for Clinical Practice
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Conflicts of Interest
References
- Sarafi, S.; Forouzi, M.A.; Tirgari, B. Priorities of palliative care: Comparison of perspectives of patients and nurses in a haemodialysis ward in Iran. Int. J. Palliat. Nurs. 2020, 26, 22–31. [Google Scholar] [CrossRef] [PubMed]
- WHO. Definition of Palliative Care. 2020. Available online: www.who.int/cancer/palliative/definition/en/ (accessed on 4 August 2021).
- Davison, S.N. End-of-life care preferences and needs: Perceptions of patients with chronic kidney disease. Clin. J. Am. Soc. Nephrol. 2010, 5, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Tavares, A.P.d.S.; Santos, C.G.d.S.; Tzanno-Martins, C.; Neto, J.B.; da Silva, A.M.M.; Lotaif, L.; Souza, J.V.L. Kidney supportive care: An update of the current state of the art of palliative care in CKD patients. Braz. J. Nephrol. 2021, 43, 74–87. [Google Scholar] [CrossRef]
- Holley, J.L. Palliative care in end-stage renal disease: Focus on advance care planning, hospice referral, and bereavement. Semin. Dial. 2005, 18, 154–156. [Google Scholar] [CrossRef] [PubMed]
- Grubbs, V.; Moss, A.H.; Cohen, L.M.; Fischer, M.J.; Germain, M.J.; Jassal, S.V.; Perl, J.; Weiner, D.E.; Mehrotra, R. A palliative approach to dialysis care: A patient-centered transition to the end of life. Clin. J. Am. Soc. Nephrol. 2014, 9, 2203–2209. [Google Scholar] [CrossRef] [PubMed]
- Holley, J.L. Palliative care in end stage renal disease: Illness trajectories, communication and hospice use. Adv. Chronic Kidney Dis. 2007, 14, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Davison, S.N.; Levin, A.; Moss, A.H.; Jha, V.; Brown, E.A.; Brennan, F.; Murtagh, F.E.; Naicker, S.; Germain, M.J.; O’Donoghue, D.J.; et al. Executive summary of the KDIGO Controversies Conference on Supportive Care in Chronic Kidney Disease: Developing a roadmap to improving quality care. Kidney Int. 2015, 88, 447–459. [Google Scholar] [CrossRef] [PubMed]
- Bull, R.; Youl, L.; Robertson, I.K.; Mace, R.; Challenor, S.; Fassett, R.G. Pathways to palliative care for patients with chronic kidney disease. J. Ren. Care 2014, 40, 64–67. [Google Scholar] [CrossRef]
- Noble, H.; Agus, A.; Brazil, K.; Burns, A.; Goodfellow, N.A.; Guiney, M.; McCourt, F.; McDowell, C.; Normand, C.; Roderick, P.; et al. PAlliativeCare in chronic Kidney diSease: The PACKS study-quality of life, decision making, costs and impact on carers in people managed without dialysis. BMC Nephrol. 2015, 11, 104. [Google Scholar]
- Johnson, A.; Bonner, A. Palliative care challenges: Implications for nurses’ practice in renal settings. Contemp. Nurse 2004, 17, 95–101. [Google Scholar] [CrossRef][Green Version]
- de Barbieri, I.; Strini, V.; Noble, H.; Amatori, S.; Sisti, D. Nurse-perceived facilitators and barriers to palliative care in patients with kidney disease: A European Delphi survey. J. Ren. Care 2021, 48, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Young, S. Rethinking and integrating nephrology palliative care: A nephrology nursing perspective. CANNT J. 2009, 19, 36–44. [Google Scholar]
- Cohen, L.M.; Moss, A.H.; Weisbord, S.D.; Germain, M.J. Renal Palliative Care. J. Palliat. Med. 2006, 9, 977–992. [Google Scholar] [CrossRef] [PubMed]
- Price, C.A. Resources for planning palliative and end-of-life care for patients with kidney disease. Nephrol. Nurs. J. 2003, 30, 649. [Google Scholar] [PubMed]
- Sellars, M.; Tong, A.; Luckett, T.; Morton, R.L.; Pollock, C.A.; Spencer, L.; Silvester, W.; Clayton, J.M. Clinicians’ perspective on Advance Care Planning for Patients with CKD in Australia: An interview study. Am. J. Kidney Dis. 2017, 70, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Haras, M.S. Planning for a good death: A neglected but essential part of ESRD care. Nephrol. Nurs. J. 2008, 35, 451–458+483. [Google Scholar]
- Lazenby, S.; Edwards, A.; Samuriwo, R.; Riley, S.; Murray, M.A.; Carson-Stevens, A. End-of-life care decisions for haemodialysis patients–‘We only tend to have that discussion with them when they start deteriorating’. Health Expect. 2016, 20, 260–273. [Google Scholar] [CrossRef]
- Yee, A.; Seow, Y.Y.; Tan, S.H.; Goh, C.; Qu, L.; Lee, G. What do renal health-care professionals in Singapore think of advance care planning for patients with end-stage renal disease? Nephrology 2011, 16, 232–238. [Google Scholar] [CrossRef]
- Deodhar, J.; Nagaraju, S.P.; Kirpalani, A.L.; Nayak, A.M. Shared Decision-Making, Advance Care Planning for Chronic Kidney Disease Patients. Indian J. Palliat. Care 2021, 27 (Suppl. S1), S33–S36. [Google Scholar] [CrossRef]
- Sturgill, D.; Bear, A. Unique palliative care needs of patients with advanced chronic kidney disease—The scope of the problem and several solutions. Clin. Med. 2019, 19, 26–29. [Google Scholar] [CrossRef]
- Hermann, C.P. The Degree to Which Spiritual Needs of Patients Near the End of Life Are Met. Oncol. Nurs. Forum 2007, 34, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Rak, A.; Raina, R.; Suh, T.T.; Krishnappa, V.; Darusz, J.; Sidoti, C.W.; Gupta, M. Palliative care for patients with end-stage renal disease: Approach to treatment that aims to improve quality of life and relieve suffering for patients (and families) with chronic illnesses. Clin. Kidney J. 2017, 10, 68–73. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Butler, R.; Monsalve, M.; Thomas, G.W.; Herman, T.; Segre, A.M.; Polgreen, P.M.; Suneja, M. Estimating Time Physicians and Other Health Care Workers Spend with Patients in an Intensive Care Unit Using a Sensor Network. Am. J. Med. 2018, 131, 972.e9–972.e15. [Google Scholar] [CrossRef]
- Shevlin, M.; Dorahy, M.J.; Adamson, G. Trauma and psychosis: An analysis of the National Comorbidity Survey. Am J Psychiatry. 2007, 164, 166–169. [Google Scholar] [CrossRef] [PubMed]
- Akaike, H. Factor analysis and AIC. Psychometrika 1987, 52, 317–332. [Google Scholar] [CrossRef]
- Schwarz, G. Estimating the Dimension of a Model. Ann. Statist. 1978, 6, 461–464. [Google Scholar] [CrossRef]
- Sclove, L. Application of Model-Selection Criteria to Some Problems in Multivariate Analysis. Psychometrika 1987, 52, 333–343. [Google Scholar] [CrossRef]
- Fassett, R.G.; Robertson, I.K.; Mace, R.; Youl, L.; Challenor, S.; Bull, R. Palliative care in end-stage kidney disease. Nephrology 2011, 16, 4–12. [Google Scholar] [CrossRef]
- Quinn, B.; Connolly, M. Spirituality in palliative care. BMC Palliat. Care 2023, 22, 1. [Google Scholar] [CrossRef]
- Ceccarelli, C.M.; Castner, D.; Haras, M.S. Advance care planning for patients with chronic kidney disease-Why aren’t nurses more involved? Nephrol. Nurs. J. 2008, 35, 553–557. [Google Scholar]
- Shah, K.K.; Murtagh, F.E.M.; McGeechan, K.; Crail, S.M.; Burns, A.; Morton, R.L. Quality of life among caregivers of people with end-stage kidney disease managed with dialysis or comprehensive conservative care. BMC Nephrol. 2020, 21, 160. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.; Baur, N.; Clelland, D.; Garralda, E.; López-Fidalgo, J.; Connor, S.; Centeno, C. Mapping Levels of Palliative Care Development in 198 Countries: The Situation in 2017. J. Pain Symptom Manag. 2020, 59, 794–807.e4. [Google Scholar] [CrossRef] [PubMed]
- Sleeman, K.E.; de Brito, M.; Etkind, S. The escalating global burden of serious health-related suffering: Projections to 2060 by world regions, age groups, and health conditions. Lancet Glob. Health 2019, 7, e883–e892. [Google Scholar] [CrossRef] [PubMed]
- Enzer, S.; Boucher, W.I.; Lazer, F.D. Future Research as an Aid to Government Planning in Canada: Four Workshop Demonstrations; Institute for the Future: Middletown, CT, USA, 1971. [Google Scholar]
| N | % | ||
|---|---|---|---|
| Gender | Male | 28 | 14.5% |
| Female | 161 | 85.5% | |
| Geographical Area | Central Europe | 35 | 17.1% |
| Eastern Europe | 58 | 28.3% | |
| Southern Europe | 66 | 32.2% | |
| Northern Europe | 15 | 7.3% | |
| Non-European countries | 31 | 15.1% | |
| Working Organization | Public | 136 | 70.5% |
| Private | 57 | 29.5% | |
| Practicing | Unbeliever | 50 | 24.4% |
| Non-practicing believer | 64 | 31.2% | |
| Practicing believer | 91 | 44.4% | |
| Religion | Christian Catholic | 120 | 71.4% |
| Christian Orthodox | 19 | 11.3% | |
| Christian Protestant | 25 | 14.9% | |
| Islamic | 4 | 2.4% | |
| Mean | S.D. | ||
| Age | 47.7 | 9.8 | |
| Years of overall clinical practice | 25.2 | 10.5 | |
| Years of clinical practice in nephrology | 20.1 | 10.1 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Barbieri, I.; Strini, V.; Noble, H.; Carswell, C.; Rocchi, M.B.L.; Sisti, D. Facilitators and Barriers to Receiving Palliative Care in People with Kidney Disease: Predictive Factors from an International Nursing Perspective. Nurs. Rep. 2024, 14, 220-229. https://doi.org/10.3390/nursrep14010018
de Barbieri I, Strini V, Noble H, Carswell C, Rocchi MBL, Sisti D. Facilitators and Barriers to Receiving Palliative Care in People with Kidney Disease: Predictive Factors from an International Nursing Perspective. Nursing Reports. 2024; 14(1):220-229. https://doi.org/10.3390/nursrep14010018
Chicago/Turabian Stylede Barbieri, Ilaria, Veronica Strini, Helen Noble, Claire Carswell, Marco Bruno Luigi Rocchi, and Davide Sisti. 2024. "Facilitators and Barriers to Receiving Palliative Care in People with Kidney Disease: Predictive Factors from an International Nursing Perspective" Nursing Reports 14, no. 1: 220-229. https://doi.org/10.3390/nursrep14010018
APA Stylede Barbieri, I., Strini, V., Noble, H., Carswell, C., Rocchi, M. B. L., & Sisti, D. (2024). Facilitators and Barriers to Receiving Palliative Care in People with Kidney Disease: Predictive Factors from an International Nursing Perspective. Nursing Reports, 14(1), 220-229. https://doi.org/10.3390/nursrep14010018









