Developing a Virtual Reality Simulation Program for Improving Nursing Students’ Clinical Reasoning Skills in Home Settings: A Protocol Paper
Abstract
1. Introduction
2. Materials and Methods
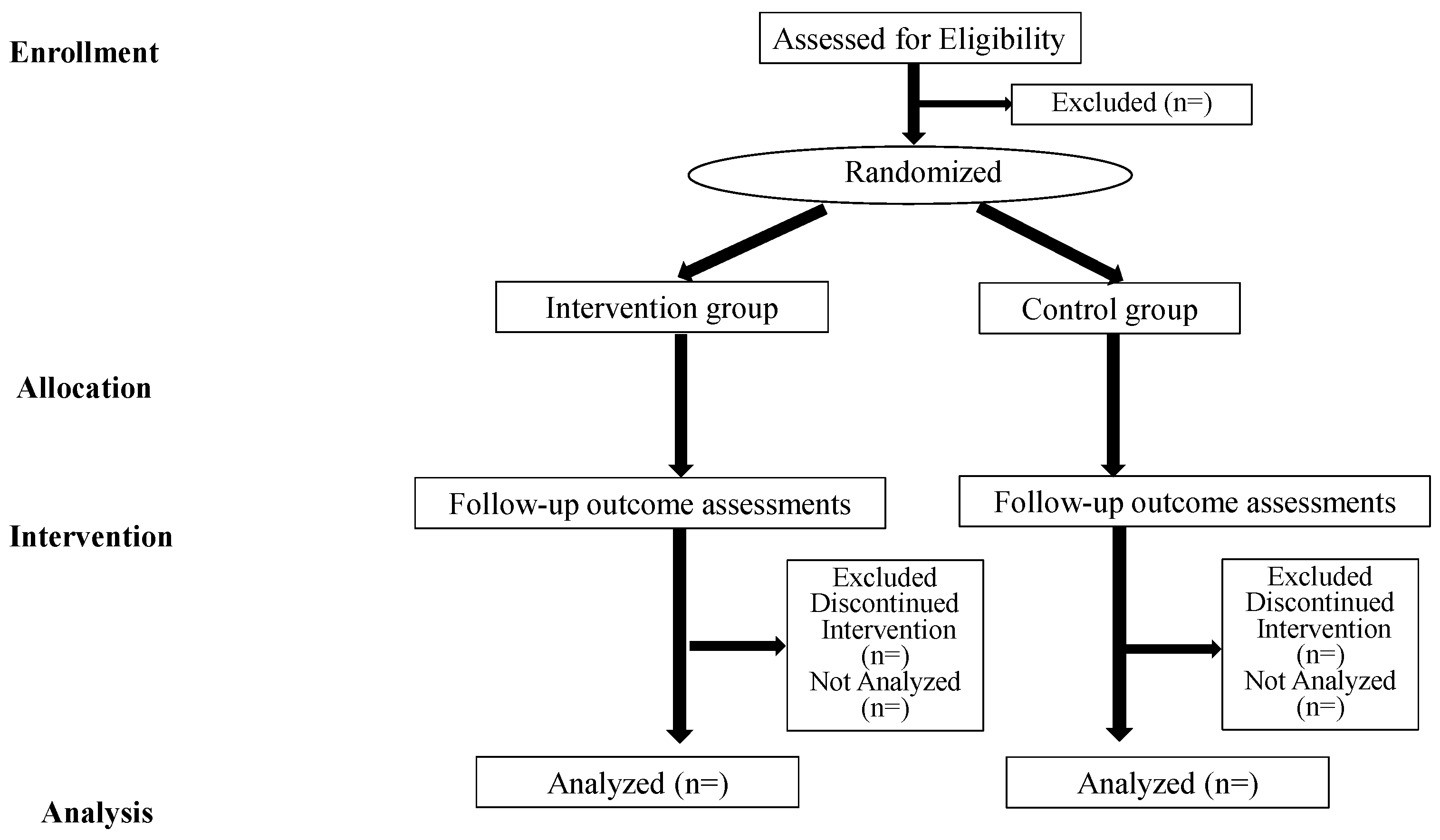
2.1. Methodology and Design
2.2. Study Setting and Recruitment
2.3. Participants
2.4. Sample Size
2.5. Randomization
2.6. The Intervention
2.6.1. The Experimental Intervention
2.6.2. The Control Intervention
2.7. Instruments and Measures
2.7.1. Demographic Data
2.7.2. Nursing Students’ Self-Assessment of Clinical Reasoning Skills
2.7.3. Student Satisfaction and Self-Confidence in Learning©
2.7.4. Simulation Design Scale© (Student Version)
2.7.5. Educational Practices Questionnaire© (Student Version)
2.7.6. Usability Metric for User Experience (UMUX)-LITE
2.7.7. Igroup Presence Questionnaire (IPQ)
2.7.8. VR Sickness
2.7.9. Free Description
2.8. Data Management
2.9. Statistical Analysis
2.10. Ethical Considerations
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Subjects | Goals of the Class | The Layout of Each Subject’s Home | Scenarios of Simulation |
|---|---|---|---|
| A household of an older person | (1) Understanding the lives of each subject in their homes. (2) Identifying living conditions that will affect the subject’s health conditions. (3) Considering concrete questions to identify or understand each subject’s health and life. |  |
|
| A household of the older couple | 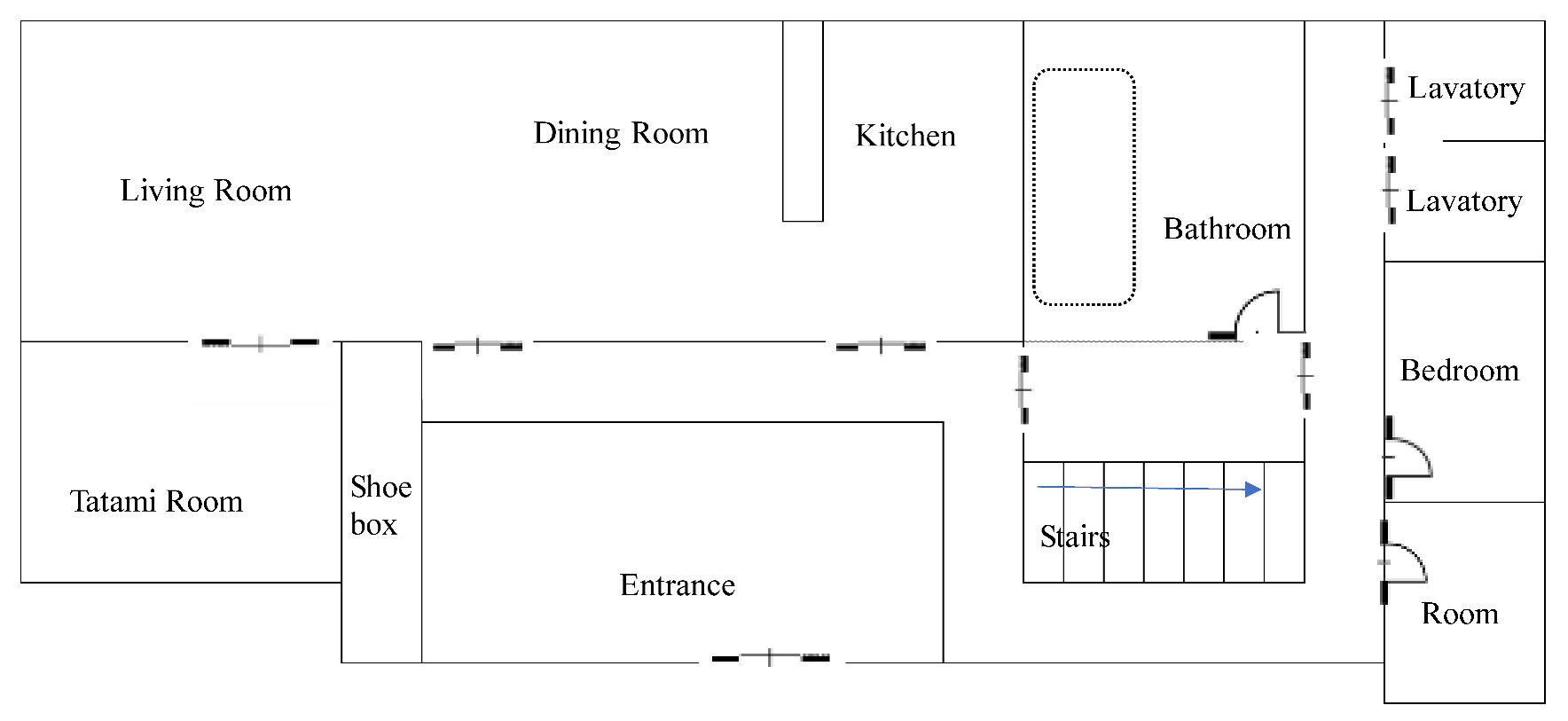 |
| |
| A household of parents with an infant |  |
|
| Program | Contents | Timetable | Measurements |
|---|---|---|---|
| Before starting the class |
| — | — |
| 15 min | — | |
| 30 min | — | |
| 10 min |
| |
| Briefing: theme 1 (household of an older person) |
| 3 min | — |
| Mini test 1 (theme 1) |
| 5 min |
|
| Simulation 1 (theme 1) |
| 4 min × 3 |
|
| Debriefing 1 (theme 1) |
| First debriefing: within 20 min Second and third debriefing: 15 min |
|
| (10 min) | — | |
| Briefing 2 and 3 (theme 2: households of the older couple; theme 3: households of parents with an infant) |
| 3 min | — |
| Mini-test 2 and 3 |
| 5 min |
|
| Simulation 2 and 3 (theme 2 and 3) |
| 4 min × 3 |
|
| Debriefing 2 and 3 (theme 2 and 3) |
| First debriefing: within 20 min Second and third debriefing: 15 min |
|
| Summary |
| 20 min | — |
| After the class |
| — |
|
References
- Chen, F.Q.; Leng, Y.F.; Ge, J.F.; Wang, D.W.; Li, C.; Chen, B.; Sun, Z.L. Effectiveness of Virtual Reality in Nursing Education: Meta-Analysis. J. Med. Internet Res. 2020, 22, e18290. [Google Scholar] [CrossRef]
- Shin, S.; Park, J.H.; Kim, J.H. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Educ. Today 2015, 35, 176–182. [Google Scholar] [CrossRef]
- Hegland, P.A.; Aarlie, H.; Stromme, H.; Jamtvedt, G. Simulation-based training for nurses: Systematic review and meta-analysis. Nurse Educ. Today 2017, 54, 6–20. [Google Scholar] [CrossRef]
- Boling, B.; Hardin-Pierce, M. The effect of high-fidelity simulation on knowledge and confidence in critical care training: An integrative review. Nurse Educ. Pract. 2016, 16, 287–293. [Google Scholar] [CrossRef]
- Kim, J.; Park, J.H.; Shin, S. Effectiveness of simulation-based nursing education depending on fidelity: A meta-analysis. BMC Med. Educ. 2016, 16, 152. [Google Scholar] [CrossRef]
- Perry, J.; Powers, S.C.; Haskell, B.; Plummer, C. Simulated Home Visit to Promote Chronic Disease Management Competencies in Prelicensure Nursing Students. Nurse Educ. 2022, 47, E132–E135. [Google Scholar] [CrossRef]
- Oliveira, S.N.; Prado, M.L.; Kempfer, S.S. Use of simulations in nursing education: An integrative review. Revista Mineira de Enfermagem. 2014, 18, 496–504. [Google Scholar] [CrossRef]
- Shaikh, F.; Inayat, F.; Awan, O.; Santos, M.D.; Choudhry, A.M.; Waheed, A.; Kajal, D.; Tuli, S. Computer-Assisted Learning Applications in Health Educational Informatics: A Review. Cureus 2017, 9, e1559. [Google Scholar] [CrossRef]
- Shin, H.; Rim, D.; Kim, H.; Park, S.; Shon, S. Educational Characteristics of Virtual Simulation in Nursing: An Integrative Review. Clin. Simul. Nurs. 2019, 37, 18–28. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality. Healthcare Simulation Dictionary; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2020; Available online: https://doi.org/10.23970/simulationv2 (accessed on 28 October 2022).
- Kyaw, B.M.; Saxena, N.; Posadzki, P.; Vseteckova, J.; Nikolaou, C.K.; George, P.P.; Divakar, U.; Masiello, I.; Kononowicz, A.A.; Zary, N.; et al. Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e12959. [Google Scholar] [CrossRef]
- Shorey, S.; Ng, E.D. The use of virtual reality simulation among nursing students and registered nurses: A systematic review. Nurse Educ. Today 2021, 98, 104662. [Google Scholar] [CrossRef]
- Yu, M.; Yang, M.; Ku, B.; Mann, J.S. Effects of Virtual Reality Simulation Program Regarding High-risk Neonatal Infection Control on Nursing Students. Asian Nurs. Res. 2021, 15, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Duchowski, A.T. A breadth-first survey of eye-tracking applications. Behav. Res. Methods Instrum. Comput. 2002, 34, 455–470. [Google Scholar] [CrossRef]
- Byrne, P.J.; Senk, P.A. Google Glass in nursing education: Accessing Knowledge at the Point of Care. Comput. Inform. Nurs. 2017, 35, 117–120. [Google Scholar] [CrossRef]
- Lubbers, J.; Rossman, C. Satisfaction and self-confidence with nursing clinical simulation: Novice learners, medium-fidelity, and community settings. Nurse Educ. Today 2017, 48, 140–144. [Google Scholar] [CrossRef]
- Zeydani, A.; Atashzadeh-Shoorideh, F.; Abdi, F.; Hosseini, M.; Zohari-Anboohi, S.; Skerrett, V. Effect of community-based education on undergraduate nursing students’ skills: A systematic review. BMC Nurs. 2021, 20, 233. [Google Scholar] [CrossRef] [PubMed]
- Birkhoff, S.D.; McCulloh Nair, J.; Bald, K.; Frankum, T.; Sanchez, S.R.; Salvatore, A.L. Facilitators and challenges in the adoption of a virtual nurse visit in the home health setting. Home Health Care Serv. Q. 2021, 40, 105–120. [Google Scholar] [CrossRef]
- Japan Ministry of Health, Labour and Welfare. Designated Rules of the Educational Institutions of Public Health Nurses, Midwives, and Nurses. 2020. Available online: https://www.mhlw.go.jp/web/t_doc?dataId=00tc5425&dataType=1&pageNo=1 (accessed on 28 October 2022).
- Calma, K.R.B.; Halcomb, E.; Stephens, M. The impact of curriculum on nursing students’ attitudes, perceptions and preparedness to work in primary health care: An integrative review. Nurse Educ. Pract. 2019, 39, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, R.; Hirai, K.; Kageyama, T.; Satoh, T.; Fukuda, H.; Kai, H.; Makino, K.; Magilvy, K.; Murashima, S. Supporting elder persons in rural Japanese communities through preventive home visits by nursing students: A qualitative descriptive analysis of students’ reports. Public Health Nurs. 2019, 36, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Miyata, T.; Hirano, M.; Saeki, K. Novice public health nurses’ home-visit skills in Japan: A one-year longitudinal study. Public Health Nurs. 2022, 39, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Joyce, B.L.; Harmon, M.; Johnson, R.G.H.; Hicks, V.; Brown-Schott, N.; Pilling, L.; Brownrigg, V. Community/public health nursing faculty’s knowledge, skills and attitudes of the Quad Council Competencies for Public Health Nurses. Public Health Nurs. 2018, 35, 427–439. [Google Scholar] [CrossRef]
- Japan Ministry of Education, Culture, Sports, Science, and Technology. Model Core Curriculum for Nursing Education: The Academic Objectives for the Acquisition of “Core Nursing Practice Competencies in the Bachelor’s Degree Program”. 2017. Available online: https://www.mext.go.jp/component/a_menu/education/detail/__icsFiles/afieldfile/2017/10/31/1217788_3.pdf (accessed on 28 October 2022).
- Michel, A.; Ryan, N.; Mattheus, D.; Knopf, A.; Abuelezam, N.N.; Stamp, K.; Branson, S.; Hekel, B.; Fontenot, H.B. Undergraduate nursing students’ perceptions on nursing education during the 2020 COVID-19 pandemic: A national sample. Nurs. Outlook. 2021, 69, 903–912. [Google Scholar] [CrossRef]
- Jeffries, P.R.; Bushardt, R.L.; DuBose-Morris, R.; Hood, C.; Kardong-Edgren, S.; Pintz, C.; Posey, L.; Sikka, N. The Role of Technology in Health Professions Education During the COVID-19 Pandemic. Acad. Med. 2022, 97, S104–S109. [Google Scholar] [CrossRef]
- Leighton, K.; Kardong-Edgren, S.; Schneidereith, T.; Foisy-Doll, C.; Wuestney, K.A. Meeting Undergraduate Nursing Students’ Clinical Needs: A Comparison of Traditional Clinical, Face-to-Face Simulation, and Screen-Based Simulation Learning Environments. Nurse Educ. 2021, 46, 349–354. [Google Scholar] [CrossRef]
- Fogg, N.; Wilson, C.; Trinka, M.; Campbell, R.; Thomson, A.; Merritt, L.; Tietze, M.; Prior, M. Transitioning from direct care to virtual clinical experiences during the COVID-19 pandemic. J. Prof. Nurs. 2020, 36, 685–691. [Google Scholar] [CrossRef]
- Kim, M.J.; Kang, H.S.; De Gagne, J.C. Nursing Students’ Perceptions and Experiences of Using Virtual Simulation during the COVID-19 Pandemic. Clin. Simul. Nurs. 2021, 60, 11–17. [Google Scholar] [CrossRef]
- Jallad, S.T.; Isik, B. The effectiveness of virtual reality simulation as learning strategy in the acquisition of medical skills in nursing education: A systematic review. Ir. J. Med. Sci. 2021, 191, 1407–1426. [Google Scholar] [CrossRef]
- Plotzky, C.; Lindwedel, U.; Sorber, M.; Loessl, B.; Konig, P.; Kunze, C.; Kugler, C.; Meng, M. Virtual reality simulations in nurse education: A systematic mapping review. Nurse Educ. Today 2021, 101, 104868. [Google Scholar] [CrossRef] [PubMed]
- Woon, A.P.N.; Mok, W.Q.; Chieng, Y.J.S.; Zhang, H.M.; Ramos, P.; Mustadi, H.B.; Lau, Y. Effectiveness of virtual reality training in improving knowledge among nursing students: A systematic review, meta-analysis and meta-regression. Nurse Educ. Today 2021, 98, 104655. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.W.; Tetzlaff, J.M.; Altman, D.G.; Laupacis, A.; Gotzsche, P.C.; Krleza-Jeric, K.; Hrobjartsson, A.; Mann, H.; Dickersin, K.; Berlin, J.A.; et al. SPIRIT 2013 statement: Defining standard protocol items for clinical trials. Ann. Intern. Med. 2013, 158, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A.; PAFS consensus group. CONSORT 2010 statement: Extension to randomized pilot and feasibility trials. Pilot Feasibility Stud. 2016, 2, 64. [Google Scholar] [CrossRef] [PubMed]
- Winum, A. BSN Students’ Satisfaction and Self-Confidence in Simulation-Based Learning. Honors Thesis, Gardner-Webb University, Boiling Springs, NC, USA, 7 April 2017. Available online: https://digitalcommons.gardner-webb.edu/cgi/viewcontent.cgi?article=1010&context=undergrad-honors (accessed on 17 November 2022).
- Kolb, D.A. Experiential Learning: Experience as the Source of Learning and Development, 2nd ed.; Pearson FT Press: Upper Saddle River, NJ, USA, 2014. [Google Scholar]
- Schön, D.A. The Reflective Practitioner—How Professionals Think in Action; Basic Books Inc.: New York, NY, USA, 1983. [Google Scholar]
- Jeffries, P.R. Simulation in Nursing Education: From Conceptualization to Evaluation, 3rd ed.; National League for Nursing: Washington, DC, USA, 2021. [Google Scholar]
- Unver, V.; Basak, T.; Watts, P.; Gaioso, V.; Moss, J.; Tastan, S.; Iyigun, E.; Tosun, N. The reliability and validity of three questionnaires: The Student Satisfaction and Self-Confidence in Learning Scale, Simulation Design Scale, and Educational Practices Questionnaire. Contemp. Nurse 2017, 53, 60–74. [Google Scholar] [CrossRef]
- The Japan Ministry of Education, Culture, Sports, Science and Technology. Goals to be Attained upon Graduation from University to Enhance the Development of Practical Nursing Skills (Report of the Committee on the State of Nursing Education). 2004. Available online: https://www.mext.go.jp/b_menu/shingi/chousa/koutou/018-15/toushin/04032601.htm (accessed on 28 October 2022).
- The Japan Ministry of Health, Labour and Welfare. Guidance Guidelines for the Operation of Training Schools for Nurses. 2015. Available online: https://www.mhlw.go.jp/web/t_doc?dataId=00tc1593&dataType=1&pageNo=1 (accessed on 28 October 2022).
- Japan Association of Nursing Programs in Universities. Core Competencies and Graduation Goals in Bachelor’s Degree Nursing Education. 2018. Available online: https://www.janpu.or.jp/file/corecompetency.pdf (accessed on 28 October 2022).
- The Japan Association of Public Health Nurse Educational Institutions. Evaluation Indicators of Public Health Nursing Education (Revised Version, 2020). 2021. Available online: https://www.zenhokyo.jp/work/doc/r3-iinkai-kyouikukatei-houkoku.pdf#view=Fit&page=1 (accessed on 28 October 2022).
- National League for Nursing. Student Satisfaction and Self-confidence in Learning©. 2005. Available online: https://www.nln.org/docs/default-source/uploadedfiles/default-document-library/instrument-2-satisfaction-and-self-confidence-in-learning.pdf?sfvrsn=6ef5d60d_0 (accessed on 28 October 2022).
- National League for Nursing. Simulation Design Scale© (Student Version). 2005. Available online: https://www.nln.org/docs/default-source/uploadedfiles/professional-development-programs/nln-instrument-simulation-design-scale.pdf?sfvrsn=56f5d60d_0 (accessed on 28 October 2022).
- National League for Nursing. Educational Practices Questionnaire© (Student Version). 2005. Available online: https://www.nln.org/docs/default-source/uploadedfiles/default-document-library/instrument-1-educational-practices-questionnaire.pdf?sfvrsn=5cf5d60d_0 (accessed on 28 October 2022).
- Lewis, J.R.; Utesch, B.S.; Maher, D.E. UMUX-LITE: When there’s no time for the SUS. In CHI ′13: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; Association for Computing Machinery: New York, NY, USA, 2013; pp. 2099–2102. Available online: https://doi.org/10.1145/2470654.2481287 (accessed on 17 November 2022).
- Schubert, T.; Friedmann, F.; Regenbrecht, H. The experience of presence: Factor analytic insights. Presence: Teleoperators Virtual Environ. 2001, 10, 266–281. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoshioka-Maeda, K.; Honda, C.; Sumikawa, Y.; Okamoto, Y.; Shimada, M.; Fujii, H.; Iwasaki-Motegi, R.; Miura, T.; Otsuki, M. Developing a Virtual Reality Simulation Program for Improving Nursing Students’ Clinical Reasoning Skills in Home Settings: A Protocol Paper. Nurs. Rep. 2022, 12, 968-979. https://doi.org/10.3390/nursrep12040093
Yoshioka-Maeda K, Honda C, Sumikawa Y, Okamoto Y, Shimada M, Fujii H, Iwasaki-Motegi R, Miura T, Otsuki M. Developing a Virtual Reality Simulation Program for Improving Nursing Students’ Clinical Reasoning Skills in Home Settings: A Protocol Paper. Nursing Reports. 2022; 12(4):968-979. https://doi.org/10.3390/nursrep12040093
Chicago/Turabian StyleYoshioka-Maeda, Kyoko, Chikako Honda, Yuka Sumikawa, Yuko Okamoto, Megumi Shimada, Hitoshi Fujii, Riho Iwasaki-Motegi, Takahiro Miura, and Mai Otsuki. 2022. "Developing a Virtual Reality Simulation Program for Improving Nursing Students’ Clinical Reasoning Skills in Home Settings: A Protocol Paper" Nursing Reports 12, no. 4: 968-979. https://doi.org/10.3390/nursrep12040093
APA StyleYoshioka-Maeda, K., Honda, C., Sumikawa, Y., Okamoto, Y., Shimada, M., Fujii, H., Iwasaki-Motegi, R., Miura, T., & Otsuki, M. (2022). Developing a Virtual Reality Simulation Program for Improving Nursing Students’ Clinical Reasoning Skills in Home Settings: A Protocol Paper. Nursing Reports, 12(4), 968-979. https://doi.org/10.3390/nursrep12040093






