Health Plans for Suicide Prevention in Spain: A Descriptive Analysis of the Published Documents
Abstract
1. Introduction
Health care Plans as a Preventive Measure against Suicide
2. Materials and Methods
3. Results
3.1. Comparison of the Proposed Objectives
3.2. Comparison of Proposed Interventions
3.2.1. General Interventions
3.2.2. Training Interventions
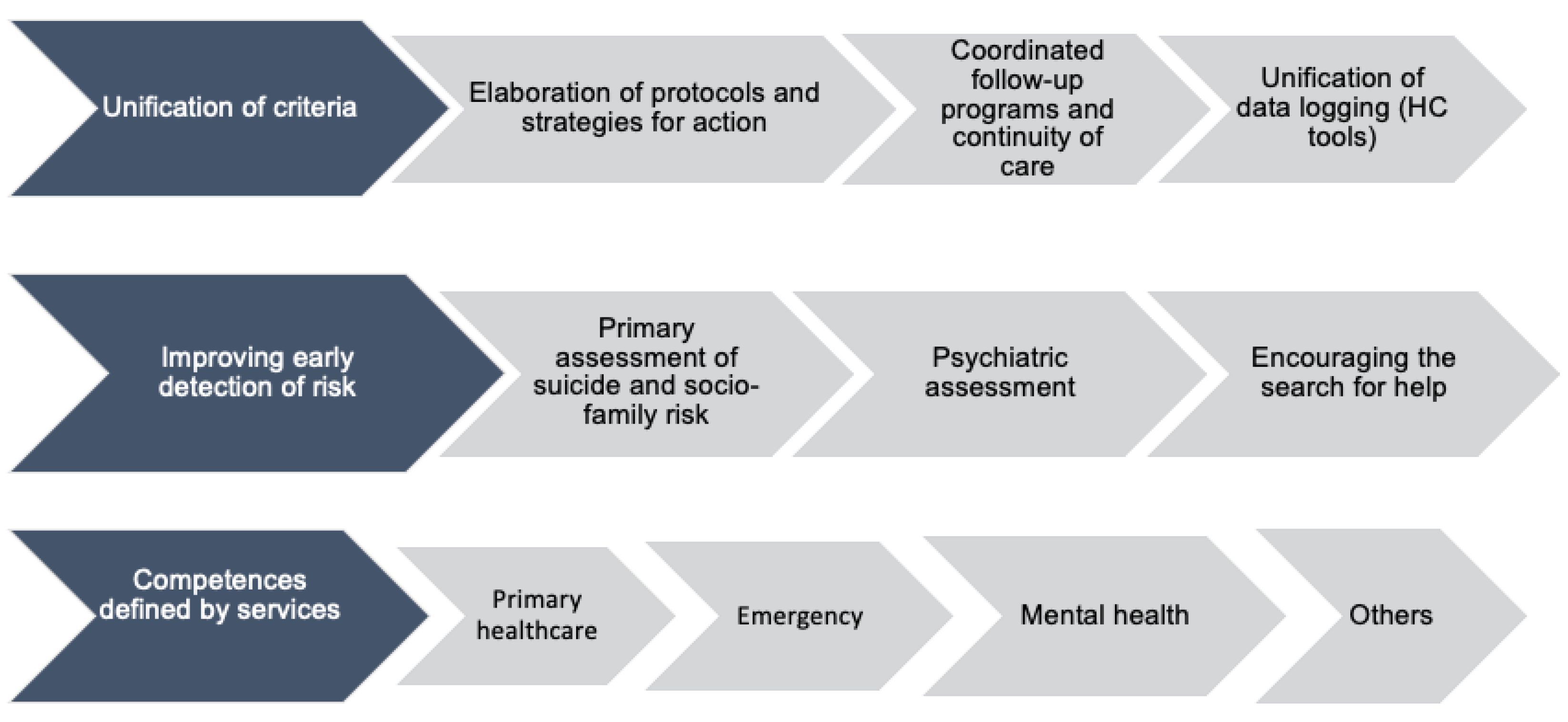
3.2.3. Health Interventions
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Saxena, S.; Krug, E.G. Suicide Prevention: A Global Imperative; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- World Health Organization. Suicide: Data and Figures. Available online: https://www.who.int/es/news-room/fact-sheets/detail/suicide (accessed on 24 April 2021).
- Clayton, P.J. MSD Manual, Version for Professionals, 1st ed.; University of Minnesota School of Medicine: Delaware, MN, USA, 2019. [Google Scholar]
- Sisti, D.A.; Joffe, S. Implications of zero suicide for suicide prevention research. JAMA 2018, 320, 1633–1634. [Google Scholar] [CrossRef] [PubMed]
- Gabilondo, A. Suicide prevention, review of the WHO model and reflection on its development in Spain: SESPAS Report. Gac. Sanit. 2020, 34, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Dumon, E.; Portzky, G. General Guidelines for Suicide Prevention; European Regions Enforcing Actions Against Suicide; Universidad de Gante: Gante, Belgium, 2013. [Google Scholar]
- Spanish Foundation for Suicide Prevention. Observatory of Suicide in Spain. Available online: https://www.fsme.es/observatorio-del-suicidio/ (accessed on 27 May 2021).
- National Statistics Institute. Statistical Organisation in Spain. España. Available online: https://www.ine.es/CDINEbase/consultar.do?mes=&operacion=Defunciones+seg%FAn+la+Causa+de+Muerte&id_oper=Ir (accessed on 16 April 2021).
- Working Group for the revision of the Clinical Practice Guideline on the prevention and treatment of suicidal behaviour. Revision of the Clinical Practice Guideline on the Prevention and Treatment of Suicidal Behaviour of the NHS CPG Programme, 1st ed.; Galician Agency for Health Technology Assessment (AVALIA-T): Madrid, Spain, 2020. [Google Scholar]
- General Council of Psychology of Spain. Published the revision of the Clinical Practice Guideline on Prevention and Treatment of Suicidal Behaviour. Available online: http://www.infocop.es/view_article.asp?id=15063&cat=47 (accessed on 1 May 2021).
- Xunta de Galicia. Suicide Prevention Plan in Galicia, 1st ed.; Conselleria de Sanidade: Santiago de Compostela, Spain, 2017; p. 65. [Google Scholar]
- Servicio Andaluz de Salud. Recommendations on the Detection, Prevention and Intervention of Suicidal Behaviour, 1st ed.; Escuela Andaluza de Salud Pública: Granada, Spain, 2010; 113p. [Google Scholar]
- Professional Association of Psychology of Aragon, Aragon Telephone of Hope, Association of Journalists of Aragon, National Association of Health Informants. Information guide for the detection and prevention of suicide: Concepts and guidelines for citizens, family members and those affected in Aragon. 2020. Available online: https://www.cop.es/pdf/Guia-digital.pdf (accessed on 16 December 2021).
- Working Group of the Suicide Prevention Strategy in Aragon. Estrategia de Prevención del Suicidio en Aragón, 1st ed.; Gobierno de Aragón: Aragón, Spain, 2020. [Google Scholar]
- Working group of the Protocol for the detection and management of cases of people at risk of suicide. Protocol for the detection and management of cases of people at risk of suicide. Regional Ministry of Health (Coordination Unit of the Mental Health Framework Programme SESPA), 2018. Available online: https://cendocps.carm.es/documentacion/2019_Protocolo_deteccion_manejo_caso_suicidio.pdf (accessed on 16 December 2021).
- Working Group of the Strategic Mental Health Plan of the Balearic Islands. Strategic Plan for Mental Health in the Balearic Islands 2016–2022, 1st ed.; Conselleria Servei Salut: Mallorca, Illes Balears, Spain, 2016; pp. 31–32. [Google Scholar]
- Servicio Canario de Salud. Canary Islands Mental Health Plan 2019–2023, 1st ed.; Gobierno de Canarias: Gran Canaria, Canary Island, Spain, 2019; pp. 247–255. [Google Scholar]
- Working Group of the Mental Health Plan of Cantabria. Mental Health Plan of Cantabria 2015–2019, 1st ed.; Gobierno de Cantabria, Consejería de Sanidad y Servicios Sociales: Santander, Cantabria, Spain, 2014; pp. 49–56. [Google Scholar]
- Working Group of the Process of Prevention And Care Of Suicidal Behaviour. Process of Prevention and Care of Suicidal Behaviour, 1st ed.; Junta de Castilla y León: León, Castilla y León, Spain, 2020. [Google Scholar]
- Regional Working Group on Suicide Prevention in Castilla-La Mancha. Strategies for Suicide Prevention and Intervention in the Face of Self-Harm Attempts in Castilla-La Mancha, 1st ed.; Gobierno de Castilla La Mancha: Toledo, Spain, 2018. [Google Scholar]
- Grupo de trabajo del Pla de Salut de Catalunya. Pla de Salut de Catalunya 2016–2020, un Sistema Centrat en la Persona: Públic, Universal I Just, 1st ed.; Generalitat de Catalunya, Departament de Salut: Barcelona, Cataluña, Spain, 2016. [Google Scholar]
- Grupo de trabajo del Pla de Salut de Catalunya. Plan de Salud de Cataluña 2011–2015, 1st ed.; Generalitat de Catalunya, Departament de Salut: Barcelona, Cataluña, Spain, 2012. [Google Scholar]
- Servei Català de la Salut. Atenció a Les Persones En Risc De Suïcidi: Codi Risc de Suïcidi. Available online: https://catsalut.gencat.cat/ca/detalls/articles/instruccio-10–2015 (accessed on 21 March 2021).
- Generalitat de Catalunya, Departament de Salut. European Project against Depression and Suicide Prevention; Departament de Salut, Direcció General de Planificació i Avaluació: Barcelona, Cataluña, Spain, 2007. [Google Scholar]
- Extremadura Health Service. I Plan de Acción para la Prevención y Abordaje de las Conductas Suicidas en Extremadura; Directorate General for Health Care: Extremadura, Spain, 2018.
- Working group of the Suicide Prevention Plan in La Rioja. Suicide Prevention Plan in La Rioja, 1st ed.; Gobierno de La Rioja: Logroño, La Rioja, Spain, 2018. [Google Scholar]
- Working Group of the Strategic Plan for Mental Health in the Region of Madrid. Strategic Plan for Mental Health in the Region of Madrid 2018–2020, 1st ed.; Servicio Madrileño de Salud: Madrid, Spain, 2018. [Google Scholar]
- De Concepción Salesa, A.; Hurtado López, A.M.; Martínez Serran, J.; Ortiz Martínez, A. Programme of Action for the Promotion and Improvement Of Mental Health in the CARM 2019–2022; Gerencia Regional de Salud Mental: Murcia, Spain, 2018; pp. 112–115. [Google Scholar]
- Working group of the Interinstitutional Collaboration Protocol. Suicidal Behaviour Prevention and Action: Interinstitutional Collaboration Protocol, 1st ed.; Gobierno de Navarra: Pamplona, Navarra, Spain, 2014. [Google Scholar]
- Department of Health, Basque Government and Osakidetza. Suicide Prevention Strategy in the Basque Country; Servicio Central de Publicaciones del Gobierno Vasco: Vitoria, Pais Vasco, Spain, 2019. [Google Scholar]
- Working group of the Suicide Prevention and Suicidal Behaviour Management Plan of the Valencian Community. Living is the Way Out: Suicide Prevention and Suicidal Behaviour Management Plan, 1st ed.; Conselleria de Sanitat Universal i Salut Pública: Valencia, Comunidad Valenciana, Spain, 2017. [Google Scholar]
- The Ceuta Forum editorial team. The elaboration of a National Plan for Suicide Prevention is more necessary than ever. Available online: https://elforodeceuta.es/la-elaboracion-de-un-plan-nacional-para-la-prevencion-del-suicidio-es-mas-necesaria-que-nunca/ (accessed on 3 May 2021).
- Popular Editor. FEAFES Melilla Advocates the Creation of a National Suicide Prevention Plan. Available online: http://populartvmelilla.com/archivos/2248 (accessed on 27 March 2021).
- Herrera-Ramírez, R.; Ures-Villar, M.B. The treatment of suicide in the Spanish press: The werther effect or the papageno effect? Rev. Asoc. Esp. Neuropsiq. 2015, 35, 123–134. [Google Scholar] [CrossRef][Green Version]
- Ugwu, C.V.; Medows, M. Critical Event Debriefing in a Community Hospital. Cureus 2020, 25, 12. [Google Scholar] [CrossRef] [PubMed]
- Gesteira, C.; Beunza, J.J.; Rodríguez Rey, R.; de Pascual Verdú, R.; Hurtado, C. Suicide Trends by Gender, Methods of Suicide and Age in Spain between 2005 and 2018; Universidad Pontificia Comillas: Madrid, Spain, 2021. [Google Scholar]
- Castellvi-Obiols, P.; Piqueras-Rodríguez, J.A. Adolescent suicide: A preventable and preventable public health problem. Rev. Estud. Juv. 2018, 121, 45–59. [Google Scholar]
- Hernández-Soto, P.A.; Villarreal-Casate, R.E. Some specificities around suicidal behaviour. MEDISAN 2015, 19, 1051–1058. [Google Scholar]
- Blanco, C. Suicide in Spain. Institutional and social response. Rev. Estud. Soc. 2020, 33, 79–106. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sufrate-Sorzano, T.; Jiménez-Ramón, E.; Garrote-Cámara, M.E.; Gea-Caballero, V.; Durante, A.; Júarez-Vela, R.; Santolalla-Arnedo, I. Health Plans for Suicide Prevention in Spain: A Descriptive Analysis of the Published Documents. Nurs. Rep. 2022, 12, 77-89. https://doi.org/10.3390/nursrep12010009
Sufrate-Sorzano T, Jiménez-Ramón E, Garrote-Cámara ME, Gea-Caballero V, Durante A, Júarez-Vela R, Santolalla-Arnedo I. Health Plans for Suicide Prevention in Spain: A Descriptive Analysis of the Published Documents. Nursing Reports. 2022; 12(1):77-89. https://doi.org/10.3390/nursrep12010009
Chicago/Turabian StyleSufrate-Sorzano, Teresa, Elena Jiménez-Ramón, María Elena Garrote-Cámara, Vicente Gea-Caballero, Angela Durante, Raúl Júarez-Vela, and Iván Santolalla-Arnedo. 2022. "Health Plans for Suicide Prevention in Spain: A Descriptive Analysis of the Published Documents" Nursing Reports 12, no. 1: 77-89. https://doi.org/10.3390/nursrep12010009
APA StyleSufrate-Sorzano, T., Jiménez-Ramón, E., Garrote-Cámara, M. E., Gea-Caballero, V., Durante, A., Júarez-Vela, R., & Santolalla-Arnedo, I. (2022). Health Plans for Suicide Prevention in Spain: A Descriptive Analysis of the Published Documents. Nursing Reports, 12(1), 77-89. https://doi.org/10.3390/nursrep12010009







