Family Functioning Assessment Instruments in Adults with a Non-Psychiatric Chronic Disease: A Systematic Review
Abstract
1. Introduction
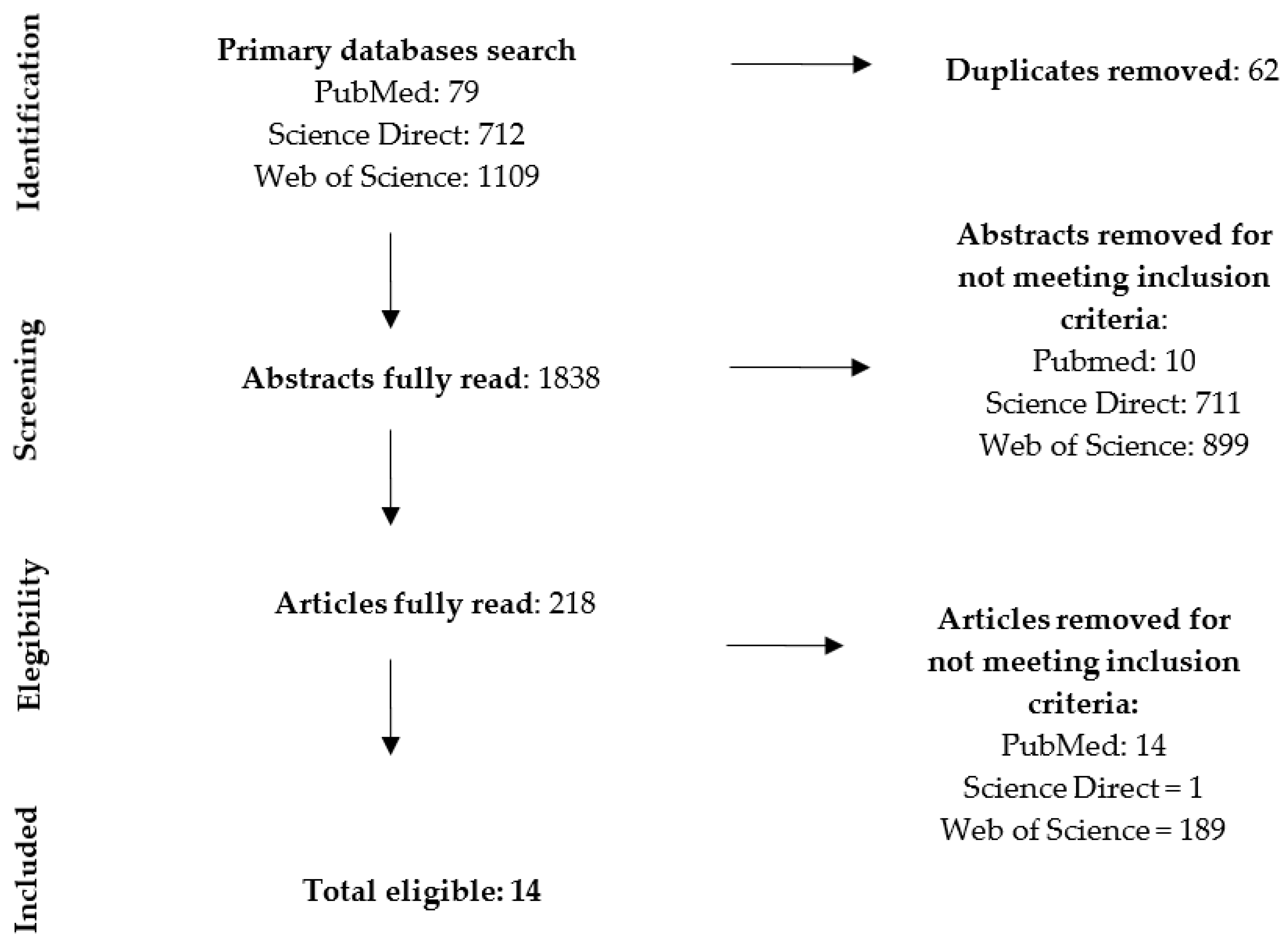
2. Materials and Methods
2.1. Search Method
2.2. Selection Criteria
2.3. Data Collection and Analysis
2.4. Quality Assessment and Risk of Bias
2.5. Working Terms: Validity and Reliability
3. Results
| N | Authors/ Year | Country | Aim | Size/Population/ Chronic Illness | Design | Main Variables | Family Function Instruments |
|---|---|---|---|---|---|---|---|
| 1 | Schmitt, 2008 [32] | Finland | To examine the factors associated with family functioning in families with children where a parent has cancer in comparison to families without cancer | 85 families including 85 cancer patients, 61 healthy spouses, 68 children, and a control group of 59 families including 105 adults and 65 children | Cross-sectional | Age and gender of family members, gender of the ill parent, diagnosis and occupation, stage of the cancer, family structure and number of children, parental depression, family resilience, and resources available to deal with the challenge of this life situation | Family Assessment Device (FAD) |
| 2 | Kugu, 2010 [38] | Turkey | To investigate whether or not there is a difference between the fibromyalgia and osteoarthritis patients with chronic pain with regard to psychopathological features, alexithymia, and the effects of these diseases on family and marital relationships | 54 women with fibromyalgia and 33 osteoarthritis patients as controls | Cross-sectional | General satisfaction level with the marriage and marital conflict. Intensity of pain, functioning, and outcome of patients with FM. Alexithymia and symptoms of psychopathology (somatization, obsessive compulsive disorder, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism) | Family Assessment Device (FAD) |
| 3 | Wang, 2015 [24] | China | To examine relationships between depressive symptoms, family functioning, and quality of life in Chinese patients with type 2 diabetes, and to explore the factors influencing their quality of life | 257 outpatients with type 2 diabetes and 259 control subjects without diabetes | Cross-sectional | Depression, quality of life, and degree of enjoyment and satisfaction experienced during the past week | Family Assessment Device (FAD) |
| 4 | Sahebihagh, 2016 [31] | Iran | To analyze the perception of family functioning by heads of families with and without cancer patients as family members | 176 control group individuals and 148 cancer case group individuals | Cross-sectional | Gender, age, job, education | Family Assessment Device (FAD) |
| 5 | Timmerby, 2018 [29] | Switzerland, Germany, United Kingdom, Finland, Austria, and Denmark | To evaluate the measurement-driven construct validity of the FAD-36 in a clinical population | 564 adult cancer patients | Cross-sectional | Gender, age measurement-driven construct validity of the FAD-36 in cancer patients’ families | Family Assessment Device (FAD) |
| 6 | Casado, 2015 [23] | Spain | To determine the prevalence of chronic obstructive pulmonary disease and smoking in a health district. To correlate real, registered, and extrapolated morbidity. To determine personal, family, and social profiles. To determine the validity of the lung function questionnaire | Random selection of 233 chronic obstructive pulmonary disease patients | Cross-sectional | Age, sex, income, lung function, and medication. Nicotine dependence and motivation to quit tobacco. Social support. | Family Adaptation, Partnership, Growth, Affection, and Resolve (APGAR) |
| 7 | Akintayo, 2019 [28] | Nigeria | To determine the prevalence of depression, the levels of family functioning, and the predictors of depression among patients with knee osteoarthritis (OA) in a multicentral setting | 250 patients with knee osteoarthritis | Cross-sectional | Age, sex, level of education marital status, ethnic group, occupation, history of smoking, alcohol use, body mass index, diabetes, hypertension, height, weight, blood pressure, depression (Patient Health Questionnaire, PHQ-9), and sleep quality (Pittsburgh Sleep Quality Index, PSQI) | Family Adaptation, Partnership, Growth, Affection, and Resolve (APGAR) |
| 8 | Astedt-Kurki, 2009 [34] | Finland | To further develop and test an instrument that can be used for assessing the association between the social support received by families, family health, and family functioning | Family members of 509 heart disease patients | Cross-sectional | Gender, age, marital status, basic training, professional training, relationship with the patient, living together, times visited in hospital, and reasons for not visiting the patient in hospital. Family health and social support | Family Functioning Family Health and Social Support (FAFHES) |
| 9 | Østergaard, 2018 [33] | Denmark | To translate the three scales of the Family Functioning, Family Health and Social Support (FAFHES) questionnaire from Finnish into Danish, to test the validity and reliability of the Danish version among outpatients with heart failure and to add to previous studies by reconstructing scales using confirmatory factor analysis | 330 patients with heart failure | Cross-sectional | Gender, age, New York Heart Association Classification, blood pressure, duration of disease, body mass index, comorbidity, living conditions, basic school, and education | Family Functioning Family Health and Social Support (FAFHES) |
| 10 | Coty, 2010 [37] | The United States | To examine the relationship between problematic social support and family functioning and measures of subjective wellbeing in a sample of women with rheumatoid arthritis | 73 women with rheumatoid arthritis | Cross-sectional | Problematic social support and unavailability of emotional support. Subjective wellbeing and satisfaction with life. Negative affect. Depressive symptoms. Pain and fatigue | Family Relationship Index (FRI) |
| 11 | Konradsen 2018 [30] | Denmark | To translate the Iceland Expressive Family Functioning Questionnaire (ICE-EFFQ) and the Iceland Family Perceived Support Questionnaire (ICE-FPSQ) into Danish, and to test the validity and reliability of the Danish versions | 81 patients with chronic diseases—cancer rehabilitation | Cross-sectional | Gender, age, family perceived support | Iceland Expressive Family Functioning (ICE-EFFQ) |
| 12 | Bennich, 2019 [35] | Denmark | Primary aim: To evaluate the association between the level of perceived family functioning and the level of glycemic control as measured by A1C levels in patients with type 2 diabetes Secondary aim: To assess associations between the family functioning, the burden of diabetes, health-related quality of life, and A1C levels and, thereby, evaluate family functioning as a unique predictor of glycemic control | 127 patients with type 2 diabetes | Cross-sectional | Age, gender, marital status, level of education, duration of diabetes, glycemic control, weight, height, abdominal and hip circumferences, and body mass index. The patients’ perceived symptoms and burdens of diabetes (Diabetes Symptom Checklist-Revised, DSC-R), health-related quality of life (Short form-36) | The Brief Family Assessment Measure-III (Brief FAM-III) |
| 13 | Astedt-Kurki, 2001 [39] | Finland | To describe testing a Finnish version of the assessment of strategies in families (ASF) instrument and its construct validity and reliability in Finnish families | 100 outpatients with pulmonary disease and 96 with rheumatic diseases | Cross-sectional | Gender, age, marital status, and education level | Assessment of Strategies in Families (ASF) |
| 14 | Takenaka, 2013 [36] | Japan | To determine the frequency and types of family issues in type 2 diabetic outpatients | 133 outpatients with type 2 diabetes | Cross-sectional | Calorie intake, body mass index, blood pressure, total calorie intake, daily lifestyle (sleeping time, working time, housekeeping time, excise time), glycemic control levels, anxiety, and depression. | Family Adaptability and Cohesion Evaluation Scale at Kwansei Gakuin IV (FACES KG IV-16) |
3.1. Identified Instruments
3.2. The FAD Questionnaire
3.3. The APGAR Questionnaire
3.4. The FAFHES Questionnaire
3.5. The FRI Questionnaire
3.6. The ICE-EFFQ Questionnaire
3.7. The Brief FAM-III
3.8. The ASF Questionnaire
3.9. The FACES KG IV-16
4. Discussion
4.1. Implications for Nursing Practice
4.2. Future Prospects
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Azmoude, E.; Tafazoli, M.; Parnan, A. Assessment of family functioning and its relationship to quality of life in diabetic and non-diabetic women. J. Caring Sci. 2016, 5, 231–239. [Google Scholar] [CrossRef][Green Version]
- Grau, C. Fomentar la resiliencia en familias con enfermedades crónicas pediátricas. Rev. Esp. Discapac. 2013, 1, 195–212. [Google Scholar] [CrossRef]
- Panganiban-Corales, A.; Medina, F. Family resources study: Part 1: Family resources, family function and caregiver strain in childhood cancer. Asia Pac. Fam. Med. 2011, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Long, K.; Marsland, A.; Alderfer, M. Cumulative family risk predicts sibling adjustment to childhood cancer. Cancer 2013, 119, 2503–2510. [Google Scholar] [CrossRef] [PubMed]
- Erker, C.; Yan, K.; Zhang, L.; Bingen, K.; Flynn, K.; Panepinto, J. Impact of paediatric cancer on family relationships. Cancer Med. 2018, 7, 1680–1688. [Google Scholar] [CrossRef]
- Quast, L.F.; Phillips, P.C.; Li, Y.; Kazak, A.E.; Barakat, L.P.; Hocking, M.C. A prospective study of family predictors of health-related quality of life in pediatric brain tumor survivors. Pediatr. Blood Cancer 2018, 65, e26976. [Google Scholar] [CrossRef]
- Modanloo, S.; Rohani, C.; Shirinabadi Farahani, A.; Vasli, P.; Pourhosseingholi, A. General Family Functioning as a Predictor of Quality of Life in Parents of Children with Cancer. J. Pediatr. Nurs. 2019, 44, e2–e8. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.; Chiarello, L.; Orlin, M.; Oeffinger, D.; Polansky, M.; Maggs, J.; Bagley, A.; Gorton, G.; Children’s Activity and Participation Group. Determinants of intensity of participation in leisure and recreational activities by children with cerebral palsy. Dev. Med. Child Neurol. 2011, 53, 142–149. [Google Scholar] [CrossRef]
- Mayoral, K.; Rajmil, L.; Murillo, M.; Garin, O.; Pont, A.; Alonso, J.; Bel, J.; Perez, J.; Corripio, R.; Carreras, G.; et al. Measurement Properties of the Online EuroQol-5D-Youth Instrument in Children and Adolescents with Type 1 Diabetes Mellitus: Questionnaire Study. J. Med. Internet Res. 2019, 21, e14947. [Google Scholar] [CrossRef] [PubMed]
- Leibach, G.G.; Everhart, R.S. Family Assessment Device: Real-world validity in urban families of children with asthma. J. Fam. Psychol. 2017, 31, 642–647. [Google Scholar] [CrossRef] [PubMed]
- Pratt, K.J.; Ferriby, M.; Brown, C.L.; Noria, S.; Needleman, B.; Skelton, J.A. Adult weight management patients’ perceptions of family dynamics and weight status. Clin. Obes. 2019, 9, e12326. [Google Scholar] [CrossRef] [PubMed]
- Warnick, J.L.; Stromberg, S.E.; Krietsch, K.M.; Janicke, D.M. Family functioning mediates the relationship between child behavior problems and parent feeding practices in youth with overweight or obesity. Transl. Behav. Med. 2019, 9, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.; Orlin, M.; Chiarello, L.; Oeffinger, D.; Polansky, M.; Maggs, J.; Gorton, G.; Bagley, A.; Tylkowski, C.; Vogel, L.; et al. Determinants of intensity of participation in leisure and recreational activities by youth with cerebral palsy. Arch. Phys. Med. Rehabil. 2011, 92, 1468–1476. [Google Scholar] [CrossRef] [PubMed]
- Kang, L.-J.; Palisano, R.J.; Orlin, M.N.; Chiarello, L.A.; King, G.A.; Polansky, M. Determinants of social participation with friends and others who are not family members for youth with cerebral palsy. Phys. Ther. 2010, 90, 1743–1757. [Google Scholar] [CrossRef] [PubMed]
- Herzer, M.; Denson, L.A.; Baldassano, R.N.; Hommel, K.A. Family functioning and health-related quality of life in adolescents with pediatric inflammatory bowel disease. Eur. J. Gastroenterol. Hepatol. 2011, 23, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Kaczynski, K.; Gambhir, R.; Caruso, A.; Lebel, A. Depression as a mediator of the relation between family functioning and functional disability in youth with chronic headaches. Headache J. Head Face Pain 2016, 56, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Nissen, K.G.; Trevino, K.; Lange, T.; Prigerson, H.G. Family Relationships and Psychosocial Dysfunction Among Family Caregivers of Patients with Advanced Cancer. J. Pain Symptom Manag. 2016, 52, 841–849.e1. [Google Scholar] [CrossRef] [PubMed]
- Hai, S.; Wang, H.; Cao, L.; Liu, P.; Zhou, J.; Yang, Y.; Dong, B. Association between sarcopenia with lifestyle and family function among community-dwelling Chinese aged 60 years and older. BMC Geriatr. 2017, 17, 187. [Google Scholar] [CrossRef]
- Shamali, M.; Konradsen, H.; Lauridsen, J.T.; Østergaard, B. Translation and validation of the Danish version of the brief family assessment measure III in a sample of acutely admitted elderly medical patients. Scand. J. Caring Sci. 2018, 32, 1247–1253. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009, 6. [Google Scholar] [CrossRef]
- Cabello López, J.B. Lectura Crítica de la Evidencia Clínica; Elsevier: Barcelona, Spain, 2015. [Google Scholar]
- Vandenbroucke, J.P.; Von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. Gac. Sanit. 2009, 23, 158.e1–158.e28. [Google Scholar] [CrossRef] [PubMed]
- Casado, V.; Álvarez, A.; Benéitez, S.; Marcos, B.; Navarro, S.; Spaans, N.; Grupo de investigación ParquEPOC. ¿Los estudios de prevalencia de zona básica de salud tienen sentido en medicina familiar y comunitaria? A propósito de un caso: La enfermedad pulmonar obstructiva crónica. Aten Prim. 2015, 47, 581–588. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, J.; He, M.; Zhao, X. Depressive symptoms, family functioning and quality of life in chinese patients with type 2 diabetes. Can. J. Diabetes 2015, 39, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Polit, D.F.; Hungler, B.P.; Palacios Martínez, R.; Feher de la Torre, G. Investigación Científica en Ciencias de la Salud. Principios y Métodos; Williams & Wilkins: Philadelphia, PA, USA, 2000. [Google Scholar]
- Nunnally, J. Psychometric Theory; McGraw Hill: Mexico City, Mexico, 1987. [Google Scholar]
- Hernández, R.; Fernández-Collado, C.; Baptista, P. Metodología de la Investigación; McGraw Hill: Mexico City, Mexico, 2006. [Google Scholar]
- Akintayo, R.O.; Yerima, A.; Olaosebikan, H.B.; Uhunmwangho, C.; Akpabio, A.A. How much gloom is in groans? Depression and its determinants in Nigerian patients with knee osteoarthritis: A multi-center cross-sectional study. Clin. Rheumatol. 2019, 38, 1971–1978. [Google Scholar] [CrossRef]
- Timmerby, N.; Cosci, F.; Watson, M.; Csillag, C.; Schmitt, F.; Steck, B.; Bech, P.; Thastum, M. A confirmative clinimetric analysis of the 36-item Family Assessment Device. Nord. J. Psychiatry 2018, 72, 268–272. [Google Scholar] [CrossRef] [PubMed]
- Konradsen, H.; Dieperink, K.B.; Lauridsen, J.; Sorknaes, A.D.; Ostergaard, B. Validity and reliability of the Danish version of the Ice Expressive Family Functioning and Ice Family Perceived Support questionnaires. Scand. J. Caring Sci. 2018, 32, 1447–1457. [Google Scholar] [CrossRef] [PubMed]
- Sahebihagh, M.H.; Amani, L.; Salimi, S.; Feizi, A.; Khalkhali, H.R.; Atri, S.B. Comparative Analysis of the Perception of Family Functioning by Heads of Families with and without Cancer Members During Illness. Asian Pac. J. Cancer Prev. 2016, 17, 4275–4279. [Google Scholar] [PubMed]
- Schmitt, F.; Santalahti, P.; Saarelainen, S.; Savonlahti, E.; Romer, G.; Piha, J. Cancer families with children: Factors associated with family functioning—A comparative study in Finland. Psychooncology 2008, 17, 363–372. [Google Scholar] [CrossRef]
- Østergaard, B.; Pedersen, K.S.; Lauridsen, J.; Nørgaard, B.; Jeune, B. Translation and field testing of the family functioning, family health and social support questionnaire in Danish outpatients with heart failure. Scand. J. Caring Sci. 2018, 32, 554–566. [Google Scholar] [CrossRef] [PubMed]
- Astedt-Kurki, P.; Tarkka, M.; Rikala, M.; Lehti, K.; Paavilainen, E. Further testing of a family nursing instrument (FAFHES). Int. J. Nurs. Stud. 2009, 46, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Bennich, B.B.; Munch, L.; Egerod, I.; Konradsen, H.; Ladelund, S.; Knop, F.K.; Vilsbøll, T.; Røder, M.; Overgaard, D. Patient Assessment of Family Function, Glycemic Control and Quality of Life in Adult Patients with Type 2 Diabetes and Incipient Complications. Can. J. Diabetes 2019, 43, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Takenaka, H.; Sato, J.; Suzuki, T.; Ban, N. Family issues and family functioning of Japanese outpatients with type 2 diabetes: A cross-sectional study. BioPsychoSocial Med. 2013, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Coty, M.-B.; Wallston, K. Problematic social support, family functioning, and subjective well-being in women with rheumatoid arthritis. Women Health 2010, 50, 53–70. [Google Scholar] [CrossRef]
- Kugu, N.; Kaptanoglu, E.; Kavakcr, O.; Gulera, E. Psychopathology, family functioning and marital relationship in female patients with fibromyalgia syndrome. Neurol. Psychiatry Brain Res. 2010, 16, 83–90. [Google Scholar]
- Astedt-Kurki, P.; Friedemann, M.; Paavilainen, E.; Tammentie, T.; Paunonen-Ilmonen, M. Assessment of strategies in families tested by Finnish families. Neurol. Psychiatry Brain Res. 2001, 38, 17–24. [Google Scholar] [CrossRef]
- Barroilhet, S.; Cano-Prous, A.; Cervera-Enguix, S.; Forjaz, M.; Guillen-Grima, F. A Spanish version of the family assesment device. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 1051–1065. [Google Scholar] [CrossRef] [PubMed]
- Speranza, M.; Guenole, F.; Revah-Levy, A.; Egler, P.; Negadi, F.; Falissard, B.; Baleyte, J. The French Version of the Family Assessment Device. Can. J. Psychiatry 2012, 57, 570–577. [Google Scholar] [CrossRef] [PubMed]
- Beierlein, V.; Bultmann, J.C.; Möller, B.; Von Klitzing, K.; Flechtner, H.-H.; Resch, F.; Herzog, W.; Brähler, E.; Führer, D.; Romer, G.; et al. Measuring family functioning in families with parental cancer: Reliability and validity of the German adaptation of the Family Assessment Device (FAD). J. Psychosom. Res. 2017, 93, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Epstein, N.B.; Baldwin, L.M.; Bishop, D.S. The Mcmaster Family Assessment Device. J. Marital Fam. Ther. 1983, 9, 171–180. [Google Scholar] [CrossRef]
- Smilkstein, G.; Ashworth, C.; Montano, D. Validity and reliability of the family APGAR as a test of family function. J. Fam. Pract. 1982, 15, 303–311. [Google Scholar] [PubMed]
- Åstedt-Kurki, P.; Tarkka, M.-T.; Paavilainen, E.; Lehti, K. Development and Testing of a Family Nursing Scale. West J. Nurs. Res. 2002, 24, 567–579. [Google Scholar] [CrossRef]
- Hoge, R.D.; Andrews, D.A.; Faulkner, P.; Robinson, D. The family relationship index: Validity data. J. Clin. Psychol. 1989, 45, 897–903. [Google Scholar] [CrossRef]
- Sveinbjarnardottir, E.K.; Svavarsdottir, E.K.; Hrafnkelsson, B. Psychometric Development of the Iceland-Expressive Family Functioning Questionnaire (ICE-EFFQ). J. Fam. Nurs. 2012, 18, 353–377. [Google Scholar] [CrossRef]
- Friedemann, M.L. Assessment of Strategies in Families: Testing. United States. 2020. Available online: https://friedemm.info/index.php/assessment-of-strategies-in-nursing/testing (accessed on 26 May 2020).
- Olson, D. FACES IV and the Circumplex Model: Validation Study. J. Marital Fam. Ther. 2011, 37, 64–80. [Google Scholar] [CrossRef]
- Gómez-Clavelina, F.; Irigoyen-Coria, A.; Ponce-Rosas, R. Selección y análisis de instrumentos para la evaluación de la estructura y funcionalidad familiar. Arch. Med. Fam. 1999, 1, 45–57. [Google Scholar]
- Grandi, S.; Fabbri, S.; Scortichini, S.; Bolzani, R. Validazione italiana del Family Assessment Device (FAD). Riv. Psichiatr. 2007, 42, 114–122. [Google Scholar]
- Traebert, E.; Cremona, O.; Traebert, J. Internal construct validity of a brazilian version of the McMaster family assessment device. J. Bras. Psiquiatr. 2016, 65, 309–313. [Google Scholar] [CrossRef]
- Hamilton, E.; Carr, A. Systematic Review of Self-Report Family Assessment Measures. Fam. Process. 2016, 55, 16–30. [Google Scholar] [CrossRef] [PubMed]
- Mayorga-Muñoz, C.; Gallardo-Peralta, L.; Galvez-Nieto, J.L. Propiedades psicométricas de la escala APGAR-familiar en personas mayores residentes en zonas rurales multiétnicas chilenas. Rev. Méd. Chile 2019, 147, 1283–1290. [Google Scholar] [CrossRef] [PubMed]
- Suárez, M.; Alcalá, M. Apgar Familiar: Una herramienta para detectar disfunción familiar. Rev. Méd. La Paz 2014, 20, 53–57. [Google Scholar]
- Wright, L.M.; Leahey, M. Nurses and Families: A Guide to Family Assessment and Intervention, 5th ed.; F.A. Davis: Philadelphia, PA, USA, 2009. [Google Scholar]
- Takenaka, H.; Ban, N. The most important question in family approach: The potential of the resolve item of the family APGAR in family medicine. Asia Pac. Fam. Med. 2016, 15, 3. [Google Scholar] [CrossRef]
- Staccini, L.; Tomba, E.; Grandi, S.; Keitner, G.I. The Evaluation of Family Functioning by the Family Assessment Device: A Systematic Review of Studies in Adult Clinical Populations. Fam. Process. 2014, 54, 94–115. [Google Scholar] [CrossRef]
- Teston, E.F.; Santos, A.D.L.; Cecilio, H.P.M.; Manoel, M.F.; Marcon, S.S. A vivência de doentes crônicos e familiares frente a necessidade de cuidado. Ciênc. Cuidad. Saúde 2013, 12, 131–138. [Google Scholar] [CrossRef]
- Barbosa, D.C.; De Sousa, F.G.M.; Silva, A.C.O.; Silva, Í.R.; Da Silva, D.C.M.; Da Silva, T.P. Funcionalidade de famílias de mães cuidadoras de filhos com condição crônica. Ciênc. Cuidad. Saúde 2011, 10, 731–738. [Google Scholar] [CrossRef]
- Rintala, T.-M.; Jaatinen, P.; Paavilainen, E.; Åstedt-Kurki, P. Interrelation Between Adult Persons with Diabetes and Their Family. J. Fam. Nurs. 2013, 19, 3–28. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.M.; Crofford, L.J.; Mease, P.J.; Burgess, S.M.; Palmer, S.C.; Abetz, L.; Martin, S.A. Patient perspectives on the impact of fibromyalgia. Patient Educ. Couns. 2008, 73, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Montejo, C.; Zapata-Vazquez, R.; Lopez-Ramon, C.; Zurita-Zarracino, E. Adherencia terapéutica y funcionalidad familiar en pacientes con enfermedades hematológicas. Horiz. Sanit. 2018, 17, 235–240. [Google Scholar] [CrossRef]
| Instrument | Instruments’ Author/s | Description | Cronbach’s Alpha | Validation Studies in Health Science Context |
|---|---|---|---|---|
| Family Assessment Device (FAD) | Epstein et al., 1983 | Self-administered questionnaire Items: 60 Dimensions (6): Problem solving, Communication, Affective responsiveness, Affective involvement, Behavior control, and Overall general functioning | 0.92 | Barroilhet et al., 2009 [40] Speranza et al., 2012 [41] Beierlein et al., 2017 [42] Epstein, Baldwin, and Bishop, 1983 [43] |
| Family APGAR | Smilkstein, 1978 | Self-administered questionnaire Items: 5 score, 2 no score Dimensions (5): Adaptation, Partnership, Growth, Affection, and Resolve | 0.80 | Smilkstein, Ashworth, and Montano, 1982 [44] |
| Family Functioning Health and Social Support (FAFHES) | Astedt-Kurki et al., 1998 | Self-administered questionnaire Items: 63 Dimensions (3): Family functioning, Family health, and Social support | 0.80–0.92 | Astedt-Kurki et al., 2009 [34] Astedt-Kurki, Tarkka, Paavilainen, Rikala, and Lehti, 2002 [45] |
| Family Relationship Index (FRI) | Moos and Holahan, 1989 | Self-administered questionnaire Items: 27 Dimensions (3): Cohesion, Expressiveness, and Conflict | 0.78 | Hoge, Andrews, Faulkner, and Robinson, 1989 [46] |
| Iceland Expressive Family Functioning (ICE-EFFQ) | Sveinbjarnardottir et al., 2009 | Self-administered questionnaire Items: 17 Dimensions (4): Expressive emotions, Collaboration and problem solving, Communication, and Behavior | 0.91 | Sveinbjarnardottir et al., 2012 [47] Konradsen et al., 2018 [30] |
| Brief Family Assessment Measure (Brief FAM-III) | Skinner et al., 2000 | Self-administered questionnaire Items: 14 Dimensions (7): Task accomplishment, Role performance, Communication, Affective expression, Involvement, Control, and Values and norms | 0.94 | Shamali et al., 2018 [19] |
| Assessment of Strategies in Families Effectiveness (ASF) | Friedemann, 1995 | Self-administered questionnaire Items: 20 Dimensions (4): Coherence, Individuation, System change, and System maintenance Targets (4): Stability, Growth, Control, and Spirituality | 0.84 | Astedt-Kurki et al., 2001 [39] Friedemann, 2020 [48] |
| Family Adaptability and Cohesion Evaluation Scales (FACES IV) | Olson, 1980 | Self-administered questionnaire Items: 42 Dimensions (4): Cohesion, Flexibility, Family satisfaction, and Communication | 0.77–0.89 | Olson, 2011 [49] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galán-González, E.; Martínez-Pérez, G.; Gascón-Catalán, A. Family Functioning Assessment Instruments in Adults with a Non-Psychiatric Chronic Disease: A Systematic Review. Nurs. Rep. 2021, 11, 341-355. https://doi.org/10.3390/nursrep11020033
Galán-González E, Martínez-Pérez G, Gascón-Catalán A. Family Functioning Assessment Instruments in Adults with a Non-Psychiatric Chronic Disease: A Systematic Review. Nursing Reports. 2021; 11(2):341-355. https://doi.org/10.3390/nursrep11020033
Chicago/Turabian StyleGalán-González, Edna, Guillermo Martínez-Pérez, and Ana Gascón-Catalán. 2021. "Family Functioning Assessment Instruments in Adults with a Non-Psychiatric Chronic Disease: A Systematic Review" Nursing Reports 11, no. 2: 341-355. https://doi.org/10.3390/nursrep11020033
APA StyleGalán-González, E., Martínez-Pérez, G., & Gascón-Catalán, A. (2021). Family Functioning Assessment Instruments in Adults with a Non-Psychiatric Chronic Disease: A Systematic Review. Nursing Reports, 11(2), 341-355. https://doi.org/10.3390/nursrep11020033







