Abstract
Sri Lanka, a country with 22 million people, has nearly 2000 thalassemia patients with severe thalassemia, two-thirds of whom have beta thalassemia major (TM). The current prevention program based on promoting “safe marriages”, which has been in existence for over 15 years, has failed to reduce thalassemia major births. We set about to examine the cost-effectiveness of novel policy options for thalassemia prevention in Sri Lanka. Methods: The current cost for treatment of a thalassemia major patient (USD 2602/yr) was compared against the cost per reduction of single birth with three novel strategies, namely intensifying the screening in the current five districts combined with an education program (policy option 1), a nationwide screening program (policy option 2), and antenatal screening combined with the termination of pregnancy (policy option 3). The incremental cost-effectiveness ratio (ICER) of the different strategies was calculated. Results: The status quo was considered to reduce one TM birth whilst the new policy options were able to reduce births by 14, 35, and 48, respectively. The costs incurred for the program for a year for status quo and the three novel programs were USD 104,788, 173,884, 781,372, and 904,186 respectively. Cost per prevention of a thalassemia major birth was USD 87,324, 12,420, 22,324, and 20,084, respectively. The lifetime cost per treatment of a thalassemia major patient was USD 34,653. Conclusions: Given the current legal restriction on termination of pregnancy for fetal indications, policy option 2, an island-wide screening with mass education, is the most cost-effective and will be expected to deliver a substantial reduction in new births.
1. Introduction
Thalassemia and other hemoglobinopathies are the commonest monogenic diseases to affect humankind, and it is estimated that there are over 300,000 new births globally every year [1]. Beta thalassemia major is a particular problem in the Indian subcontinent, which has the highest burden of disease [2]. In Sri Lanka, though α3.7 thalassemia deletion is the commonest hemoglobinopathy, among clinically significant thalassemia syndromes β thalassemia major (TM) and hemoglobin E β thalassemia account for the bulk of patients [3]. In a hospital survey conducted in 2015, there were approximately 1800 patients seeking treatment in 25 different hospitals across the 25 districts in Sri Lanka [4]. The cost of treatment of thalassemia patients has been assessed twice in Sri Lanka. Health costs in Sri Lanka are almost exclusively borne by the state among patients who patronize the state-sponsored hospital system. Though private health care is available in the country, very few thalassemia patients receive treatment in the private sector. In 1997, it was estimated that approximately 5% of the annual health budget is spent on the treatment of these 1800 patients [5]. A more recent estimate suggested that the cost per patient is USD 2601 per year [6]. This included direct hospital costs for blood transfusion, iron chelation, investigations, clinic attendance, staff cost, and indirect hospital costs for overhead and buildings. In a nation of 22 million people, a small number of patients with thalassemia consuming a huge portion of the health budget could be seen as a travesty. Thus, clearly, the way forward is to implement an effective prevention program.
In 2006/7 the Ministry of Health laid out the first steps towards a national prevention program with the concept of propagation of a “safe marriage”, i.e., discouraging marriage between two carriers [7]. Prenatal diagnosis and termination of pregnancy of affected pregnancies were not considered as a possible means for thalassemia control because of the rigid laws governing the termination of pregnancy in Sri Lanka. TOP could legally be carried out only in the case of safeguarding maternal health or in cases of incest or rape.
The prevention program was based on using low red cell indices of the full blood count for screening, treating those who had such with iron for three months and repeating the test. If the red cell indices/Hb continued to be low, HPLC or CE was performed. Kurunegala, Ragama, Anuradhapura, Badulla, and Kandy were the five centers that started the process initially. Aside from Ragama, the other three centers are located in areas in Sri Lanka where thalassemia has a high prevalence. Funds were allocated by the Ministry of Health for the screening program, and the consultants in charge of the individual units took their own initiative to start their programs. There was minimal, if any, central regulation or data assessment of the success of the program. There was no central allocation policy of staff or resources to these units, and the efficiency of the screening program depended on the motivation of each unit.
The target population for each district or center was the same: school children around the ages of 15–19 years, young employees of factories and other establishments, and students at technical colleges, nursing schools, and universities. Health education of the target population was carried out using lectures followed by screening and appropriate genetic counseling.
There were clear drawbacks to this strategy. Among them were probable technical failures due to people not returning for a repeat full blood count (FBC) after a course of iron therapy, missing Hb S and Hb S traits, and inadequate counseling of carriers detected during the program. In addition, there was a lack of data-keeping to provide evidence of marriage outcomes.
The biggest drawback of this was highlighted in a survey completed in 2015, in which the number of thalassemia major births did not reduce over a period of 10 years. The number of births has remained at around 45–60 per year [4]. A recent telephone survey of new births at a few major centers in Sri Lanka verified that approximately 58 new diagnoses of beta thalassemia major were reported in 2021.
Against this backdrop, an attempt was made with the guidance of the Non-Communicable Diseases Bureau of the Ministry of Health to revisit and design new policy options with the aim of reducing thalassemia major births in Sri Lanka. The final objective of the exercise was to decide on a suitable policy option that is cost-effective and both politically and practically feasible.
2. Materials and Methods
The existing prevention program (status quo) was considered the baseline against which several policy options were to be compared prior to deciding on the most suitable option. Three new policy options were developed.
Policy option 1: Screening would be limited to the same five centers (regions) of the country as it is currently carried out. School children aged 16 years old will be screened and the program will be intensified to cover 85% of the target population. Resources will be allocated for disease-specific health education of the masses and healthcare workers. The education would cover include usage of social media, as well as making inroads into the school curriculum and using mass media whenever possible.
Policy option 2: Widening the screening program to cover all 25 districts of Sri Lanka (from the current five) and also to continue the intensified health education program as mentioned in option 1. Screening of school children aged 16 years old with 95% coverage will be expected.
Policy option 3: Antenatal (ANC) screening for thalassemia of all mothers at the booking visit in all 25 districts, proceeding to partner screening in those identified with beta thalassemia traits. This will be augmented by offering services of prenatal diagnosis and /or termination of pregnancy if the fetus is found to have thalassemia major.
The cost of treatment for patients was obtained using previous publications [5,6]. The current cost for bone marrow transplantation at the leading Sri Lankan transplantation center was considered for the calculation (personal communication).
As there are no survival data for thalassemia major patients in Sri Lanka, the mean age of the current thalassemia major population obtained from a recent national survey of thalassemia patients (13.5 years) was used as the average life expectancy of a thalassemia major patient [4].
Reduction in thalassemia births was considered the desired outcome. Analysis was from the Ministry of Health perspective, and the time frame for implementation was considered as 5–8 years. The analytical horizon was after 10 years.
Screening data for the year 2018 from the five centers were used for calculations of the “status quo”. These data suggested an overall beta thalassemia carrier rate of 5% which was used for further calculations too. (Unpublished data from the Non-Communicable Diseases Bureau of the Ministry of Health Sri Lanka).
The cost of prevention was calculated using the data from the Ministry of Health, Sri Lanka.
Expenditures incurred for screening programs included transport, consumables, staff salaries, reagent costs, machinery costs, the cost for reporting, and educational materials.
As the number of births per year was known, the cost per prevention was calculated accordingly [8].
In policy option number 2, the assumption was of a more intensified program, and as such data were not available from Sri Lanka, a decision was made to use data from a similar regional program from Iran [9]. Based on this, the success of effective prevention was assumed to be a 50% reduction in births [9]. Using this assumption and using other relevant data such as fertility rates of Sri Lankan women, the cost per prevention of one birth was calculated [8].
Expenditures were calculated to cover all 25 districts. The estimated cost of public awareness using island-wide mass media coverage was included.
Calculation of the number of births averted by status quo and policy options 1 and 2 was performed as below.
We calculated the probabilities of thalassemia major (TM) births in each of the above options for the “screened” and “not screened” groups separately, using the decision tree model. The probability of TM births in the “screened” group in each option was multiplied by the number of the corresponding screened population to obtain the number of TM births in the screened group. The number of TM births in the “not screened” group was calculated in the same way. The number of TM births averted by screening was calculated by subtracting the number of TM births in the “screened group” from the number of TM births in the “unscreened group”, i.e., (Number of TM births averted by screening = Number of TM births in the “not screened” group − Number of TM births in the “screened” group).
The estimated number of TM births averted by option 3 (prenatal diagnosis and termination of the affected fetuses) was calculated using the published data, statistics, and best guess. The calculation was based on the number of females becoming pregnant in 2019 [10,11,12] (Figure 1).
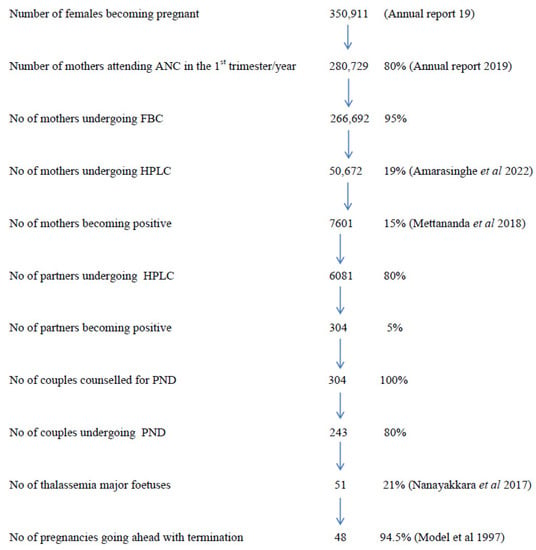
Figure 1.
Calculation of the estimated number of TM births averted by policy option 3 prenatal diagnosis. Within parenthesis the references relating the data sources are given.
For option 3, the cost for fetal sampling for amniocentesis and prenatal diagnosis using ARMS PCR for common mutations and the cost for medical termination as used in the private sector facilities were used for calculation.
In the absence of local statistics on prenatal genetic diagnosis and termination, respective data from a UK-based study was used [13].
The cost per thalassemia major birth averted by each option was calculated by dividing the annual program cost by the number of thalassemia major births averted per year.
The incremental cost effectiveness ratio (ICER) for each policy option, which indicated the additional cost for preventing a thalassemia major birth compared to the status quo, was calculated using the following formula.
ICER = Cost of each option-cost of the status quo.
The desired outcome of each option-desired outcome of the status quo.
The desired outcome in our case was the number of thalassemia major births averted per year.
To calculate the benefit-cost ratio, the following calculation was used [14].
Benefit-cost ratio = Benefits of program/costs of program.
Where benefits of program = Average lifetime costs of treatment of Thalassemia major patient x Number of Thalassemia major births averted.
Costs of program = Costs of educational program + costs of screening.
Data analysis was performed using Microsoft Excel.
USD was considered to be equivalent to LKR 202 (the trading rate at the time the article was drafted).
3. Results
Table 1 shows the summary of the data analysis.

Table 1.
Summary of data analysis: Benefit-cost ratios from the Ministry of Health perspective is shown for the status quo and the three novel policy options.
The total cost for the prevention of one thalassemia major birth in the status quo was LKR 17,640,288 (USD 87,324).
Total cost per prevention of one birth in options 1, 2, and 3 were LKR 2,509,033 (USD 12,420), LKR 4,509,859 (USD 22,324) and LKR 4,057,202 (USD 20,084), respectively. Assuming the average life expectancy of a thalassemia major patient is 13.5 years and the cost of treatment for a patient per year is USD 2601 per year, the total cost for treatment of a thalassemia patient would be from USD 35,113 to USD 33,750.
The number of thalassemia births averted by status quo was 1 while options 1, 2 and 3 averted 14, 35, and 45 births, respectively.
ICER of options 1, 2, and 3 compared to status quo were LKR 1,073,701 (USD 5315), LKR 4,019,904 (USD 19,899) and LKR 3,668,488 (USD 18,159), respectively.
Option 1 had the highest benefit-cost ratio of 3/1, at a program cost of LKR 2,509,033 (USD 12,420) with the aversion of 14 thalassemia major births and a lifetime treatment cost of LKR 7,093,278 (USD 35,113). This was followed by options 2 and 3 with benefit-cost ratios of 2/1 and 1.74/1, respectively. Status quo had the lowest ratio of 0.33/1.
4. Discussion
The cost of treatment of a thalassemia major patient for a lifetime was LKR 7,093,278 (USD 35,113) and the cost for bone marrow transplantation was LKR 5,000,000 (USD 24,751) to LKR 8,000,000 (USD 39,601).
The current screening program (status quo) has the lowest number of desired outcomes with the aversion of only 1 thalassemia major birth and the lowest benefit-cost ratio of 0.33/1.
The data suggest that the current method of thalassemia prevention is not effective.
Out of the three novel policy options, intensifying the current thalassemia screening program (option 1) has the lowest program implementation cost (USD 173,884), the lowest cost for a thalassemia major birth averted (USD 12,420), and the lowest ICER compared to status quo (USD 5315). Among the new options, it had the lowest success in reducing the number of thalassemia major births though it had the highest benefit-cost ratio of 3.
Implementation of an island-wide screening program with public and staff awareness (Option 2) in comparison to the prenatal diagnosis and termination of affected fetuses (option 3) has a lower program implementation cost (USD 781,372 vs. USD 904,186). However, with the lower success in reducing thalassemia major births (35 vs. 45), it has a higher cost for thalassemia major birth averted (USD 22,324 vs. USD 20,084).
With the higher program implementation cost, the benefit-cost ratio of option 3 is higher than option 2 (2/1 vs. 1.74/1).
In the current study, we observe that option 2 (implementation of an island-wide screening program with public and staff awareness) would be the most appropriate policy option to reduce the number of thalassemia major births in Sri Lanka. The reasons include that the ICER over status quo (USD 19,899) is still lower than the lifetime treatment cost of a thalassemia major patient (USD 35,113), political and operational feasibility, and reduction in a considerable number of thalassemia major births (35).
Given the legal barriers, option 3 (prenatal diagnosis and termination of affected fetuses) would not be feasible at present. The lowest benefit-cost ratio of this option could be partly due to the higher costs incurred for outsourcing the genetic tests, given the scarcity of state-driven genetic diagnostic facilities.
Our data is comparable to other studies which have found that the cost of prevention of one TM birth is less than the lifetime cost of treatment of a patient [15]. This was shown in all three policy options. (USD 35,113 vs. USD 124,202,232,420,084 ). The disproportionate amounts seen in studies from Israel and Iran and our studies, where the former show at least a fourfold superiority of prevention over treatment is due to the low mean survival of TM patients we have used for our calculation (13.2 years) [14,16,17].
The data we have generated are based on several assumptions. The success of a prevention program based on screening school children would clearly depend on the success of the health education messages imparted to them and the potential it has in changing their partner selection/marriage many years later. The Maldives has managed to substantially reduce thalassemia births initially by screening and educating young people, but the number of thalassemia births started to increase after an initial dip [18,19]. There is also evidence that the best age to screen for thalassemia may not be school children as they are likely to lose the message by the time they marry [20]. Contradictory results have been cited from studies from the West and East (Canada/France and India), where in the former two countries the children remembered and used the information much later in partner selection whilst disappointing results were seen in the Indian cohort [20]. Screening coupled with education alone was effective in changing the marital behavior in premarital couples in Iran, but there too, this approach was used as a stepping stone for a subsequent prenatal diagnosis and termination of pregnancy-based program [9]. In Sri Lanka, termination of pregnancy remains illegal except for a few restricted indications, and fetal and infant health is not one of them. Though there have been several unsuccessful attempts to change the law relating to the termination of pregnancy, thalassemia had never even been a reason that was discussed by any panel regarding these issues. Until such time, the new policy option 2 would remain the best and most cost-effective option for Sri Lanka if used in a sustainable way.
Author Contributions
Conceptualization, F.M. and A.P.; methodology, P.W., M.A. and F.M., formal analysis, A.T., M.A., N.A., P.W. and A.A.; resources, M.A., P.W. and F.M.; writing—original draft preparation, A.P.; writing—A.P., N.A. and M.A., supervision, C.W. project administration, C.W. All authors have read and agreed to the published version of the manuscript.
Funding
The research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data used for this analyses can be provided on request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- De Sanctis, V. β-thalassemia distribution in the old world: A historical standpoint of an ancient disease. Mediterr. J. Hematol. Infect. Dis. 2017, 9, e2017018. [Google Scholar] [CrossRef] [PubMed]
- Colah, R.; Gorakshakar, A.; Nadkarni, A. Global burden, distribution and prevention of β-thalassemias and hemoglobin E disorders. Expert Rev. Hematol. 2010, 3, 103–117. [Google Scholar] [CrossRef] [PubMed]
- Premawardhena, A.; Allen, A.; Piel, F.B.; Fisher, C.; Perera, L.; Rodrigo, R.; Goonathilaka, G.; Ramees, L.; Peto, T.; Olivieri, N.; et al. The evolutionary and clinical implications of the uneven distribution of the frequency of the inherited haemoglobin variants over short geographical distances. Br. J. Haematol. 2017, 176, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Premawardhana, A.P.; Mudiyanse, R.; De Silva, S.T.; Jiffry, N.; Nelumdeniya, U.; de Silva, U.; Lamabadusuriya, S.P.; Pushpakumara, K.; Dissanayaka, R.; Jansz, M.; et al. A nationwide survey of hospital-based thalassemia patients and standards of care and a preliminary assessment of the national prevention program in Sri Lanka. PLoS ONE 2019, 14, e0220852. [Google Scholar] [CrossRef]
- de Silva, S.; Fisher, C.; Premawardhena, A.; Lamabadusuriya, S.; Peto, T.; Perera, G.; Old, J.; Clegg, J.; Olivieri, N.F.; Weatherall, D. Thalassaemia in Sri Lanka: Implications for the future health burden of Asian populations. Lancet 2000, 355, 786–791. [Google Scholar] [CrossRef]
- Reed-Embleton, H.; Arambepola, S.; Dixon, S.; Maldonado, B.N.; Premawardhena, A.; Arambepola, M.; Khan, J.A.M.; Allen, S. A cost-of-illness analysis of β-Thalassaemia major in children in Sri Lanka—Experience from a tertiary level teaching hospital. BMC Pediatr. 2020, 20, 257. [Google Scholar] [CrossRef] [PubMed]
- Mudiyanse, R.M. Thalassemia Treatment and Prevention in Uva Province, Sri Lanka: A Public Opinion Survey. Hemoglobin 2006, 30, 275–289. [Google Scholar] [CrossRef] [PubMed]
- Annual Report 2019, Family Health Bureau. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjXnpXW9Or3AhXVjOYKHfHqCnQQFnoECAgQAQ&url=https%3A%2F%2Ffhb.health.gov.lk%2Findex.php%2Fen%2Fresources%2Fannual-report&usg=AOvVaw21KeoABrD8h888odYVv84J (accessed on 12 September 2022).
- Samavat, A.; Modell, B. Iranian national thalassaemia screening programme. BMJ 2004, 329, 1134–1137. [Google Scholar] [CrossRef]
- Amarasinghe, G.S.; Agampodi, T.C.; Mendis, V.; Malawanage, K.; Kappagoda, C.; Agampodi, S.B. Prevalence and aetiologies of anaemia among first trimester pregnant women in Sri Lanka; the need for revisiting the current control strategies. BMC Pregnancy Childbirth 2022, 22, 16. [Google Scholar] [CrossRef]
- Mettananda, S.; Suranjan, M.; Fernando, R.; Dias, T.; Mettananda, C.; Rodrigo, R.; Perera, L.; Gibbons, R.; Premawardhena, A.; Higgs, D. Anaemia among females in child-bearing age: Relative contributions, effects and interactions of α- and β-thalassaemia. PLoS ONE 2018, 13, e0206928. [Google Scholar] [CrossRef]
- Nanayakkara, K.K.; Rodrigo, U.G.; Perera, K.L.N.; Nanayakkara, C.D. Pre-natal diagnosis of thalassaemia in Sri Lanka: A ten year review. J. Obstet. Gynaecol. 2017, 37, 861–863. [Google Scholar] [CrossRef]
- Model, B. Delivering genetic screening to the community. Ann. Med. 1997, 29, 591–599. [Google Scholar] [CrossRef]
- Ginsberg, G.; Tulchinsky, T.; Filon, D.; Goldfarb, A.; Abramov, L.; A Rachmilevitz, E. Cost-benefit analysis of a national thalassaemia prevention programme in Israel. J. Med. Screen. 1998, 5, 120–126. [Google Scholar] [CrossRef]
- Ostrowsky, J.T.; Lippman, A.; Scriver, C.R. Cost-benefit analysis of a thalassemia disease prevention program. Am. J. Public Health 1985, 75, 732–736. [Google Scholar] [CrossRef][Green Version]
- Koren, A.; Profeta, L.; Zalman, L.; Palmor, H.; Levin, C.; Zamir, R.B.; Shalev, S.; Blondheim, O. Prevention of β thalassemia in Northern Israel—A cost-benefit analysis. Mediterr. J. Hematol. Infect. Dis. 2014, 6, e2014012. [Google Scholar] [CrossRef]
- Esmaeilzadeh, F.; Ahmadi, B.; Vahedi, S.; Barzegari, S.; Rajabi, A. Major Thalassemia, Screening or Treatment: An Economic Evaluation Study in Iran. Int. J. Health Policy Manag. 2022, 11, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Waheed, F. Thalassaemia Prevention in Maldives: Effectiveness of Primary, Secondary and Tertiary Prevention Interventions. Doctoral Thesis, The University of Western Australia, Crawley, WA, Australia, 2015. [Google Scholar]
- Saeed, F. Status of thalassaemia in the Maldves. Abdulla Waheed’s Blog. Available online: http://abdullahwaheedsblog.blogspot.com/ (accessed on 12 September 2022).
- Colah, R.; Thomas, M.; Mayekar, P. Assessing the impact of screening and counselling high school children for β-thalassaemia in India. J. Med. Screen. 2007, 14, 158. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).