Round Window Niche and Membrane Dimensions: A Systematic Review
Abstract
1. Introduction
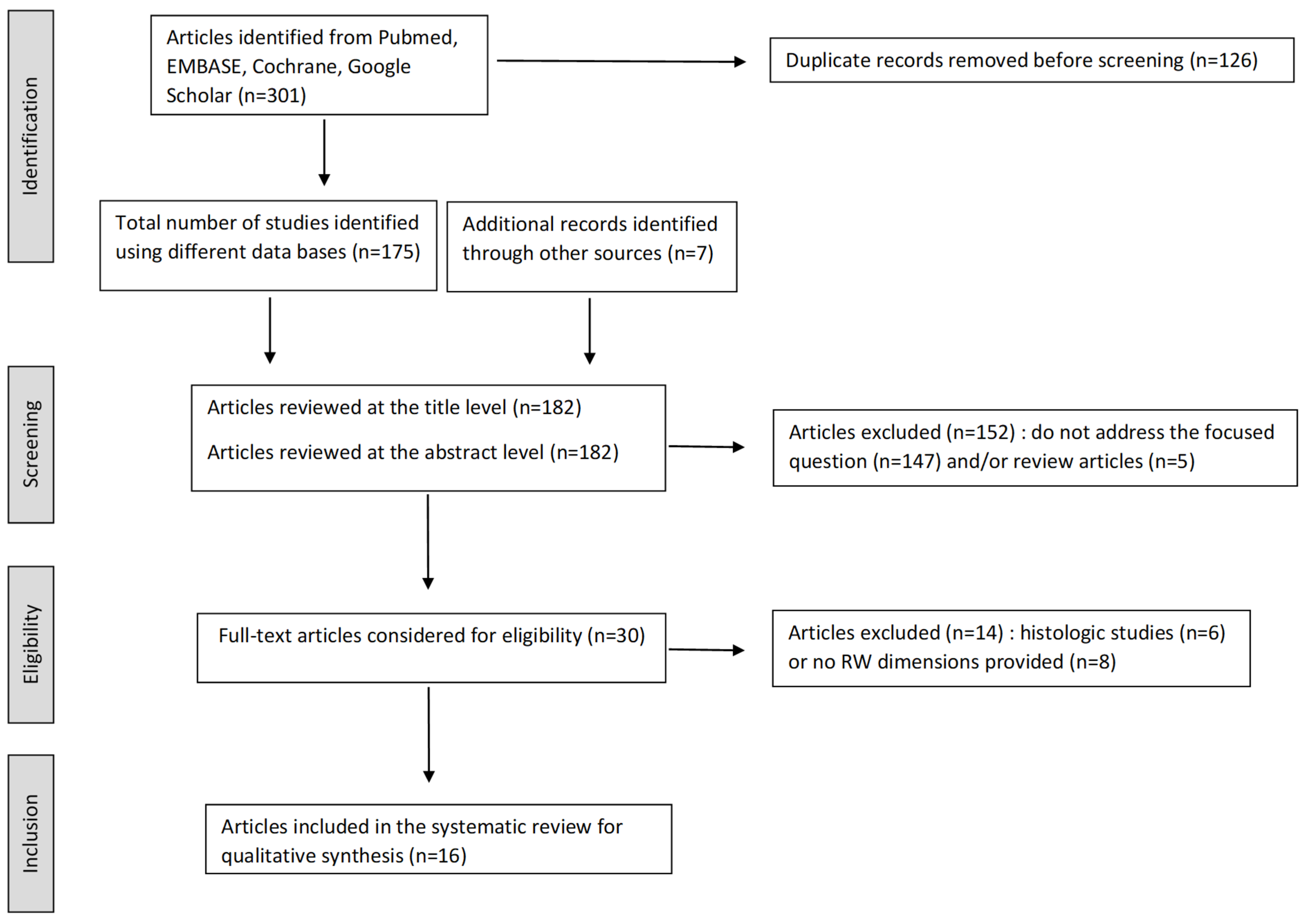
2. Materials and Methods
3. Results
| RW Membrane | RW Niche | Posterior Pillar | RW Tegmen | |
|---|---|---|---|---|
| Stewart & Belal [5]; n = 68 (cadaveric temporal bones, CTB) (risk of bias ROB: high) | Transverse diameter: 1.5 (min: 0.6; max: 2.8) Vertical diameter: 1.2 (min: 1.2; max: 1.6 | Length: 2.8 (min: 2.0; max: 4.0) | Length: 1.1 (min: 0.5; max: 1.8) | |
| Okuno & Sando [13]; n = 40 (CTB) (ROB: high) | Area: 2.29 mm2 (SD: 0.42) | |||
| Takahashi et al. [24] †; n = 5 (CTB) (ROB: high) | Maximal diameter: 2.98 (SD: 0.23) Depth: 0.66 (SD: 0.16) | Thickness: 0.66 (SD: 0.16) | ||
| Takahashi et al. [17] †; n = 5 (CTB) (ROB: high) | Area: 2.98 mm2 (min: 2.51; max: 3.72) | Maximal diameter: 2.32 mm (min: 2.13; max: 2.53) Length: 2.08 mm (min: 1.86; max: 2.43) Width: 1.76 mm (min: 1.61; max: 1.89) | ||
| Roland et al. [18]; n = 15/30 (CTB) (ROB: low) | Before drilling overhang, area: 0.32 mm2 (min: 0.04; max: 0.61) After drilling overhang, area: 0.72 mm2 (min: 0.46; max: 1.16) | |||
| Singla et al. [26]; n = 50 (CTB) (ROB: low) | Maximum height: 1.62 (SD: 0.77) Maximum width: 1.15 (SD: 0.39) | |||
| Atturo et al. [19] *; n = 30 (CTB) (ROB: low) | Long diameter: 1,9 mm (min: 1.32; max: 2.35) Small diameter 1.54 mm (min: 0.9; max: 2.1) Area: 2.08 (min: 0.99; max: 3.2) | |||
| Shakeel et al. [25]; n = 14 (CTB) (ROB: unclear) | Vertical height: 2.02 mm (min: 1.85; max: 2.15) | Thickness: 2.1 (min: 1.9; max: 2.4) | ||
| Angeli et al. [20]; n = 10 (CTB) (ROB: high) | Height: 0.77 mm (min: 0.6; max: 1.04) Width: 1.41 mm (min: 1,19; max: 1.71) Area: 0.91 mm2 (min: 0.54; max: 1.29) Area after drilling crista fenestra: 1.42 mm2 (min: 0.83; max: 2.02) | |||
| Karkas et al. [12] **; n =10 (CTB) (ROB: high) | Maximal diameter: 1.2 mm (SD: 0.2) | Thickness: 1.3 mm (SD: 0.2) | ||
| Jain et al. [23]; n = 34 (CTB) (ROB: low) | Maximum height: 0.69 (min: 0.51; max: 1.27) Maximum width: 1.16 (min: 0.51; max: 2.04) | |||
| Mehanna et al. [21] §; n = 20 (CTB) (ROB: high) | Maximum height: 1.53 mm (min: 0.9; max: 2.3) Maximum width: 1.18 (min: 0.8; max: 1.65) Area: 1.52 mm2 (min: 1.24; max: 1.52) | Length: 2.09 (min: 1.7; max: 2.37) | ||
| Liang et al. [22] *; n = 14 (CTB) (ROB: unclear) | Short diameter: 1.81 mm (min: 1.65; max: 1.97) Long diameter: 2.04 mm (min: 1.87; max: 2.20) Area: 2.89 mm2 (2.67; max: 3.16) | |||
| Cohen et al. [14]; n = 414 (CT scans) (ROB: high) | Width: 1.58 mm (min: 0.9; max: 2.7) | Width: 2.22 mm (min: 0.9; max: 3.4) Length: 1.67 mm (min: 1.0; max: 2.7) | ||
| Matin et al. [15]; n = 50 (CT scans) (ROB: high) | Area: 2.93 mm2 (min: 1.3; max: 4.39) Volume: 4.54 mm3 (min:2.28; max: 6.64) | Depth: 1.35 mm (min: 0.98; max: 1.88) | Thickness: 0.56 mm (min: 0.04; max: 1.24) | |
| Karkas et al. [12] **; n = 10 (CT scans) (ROB: high) | Maximal diameter: 1.5 mm (SD: 0.2) | Thickness: 1.1 mm (SD: 0.1) | ||
| Mehanna et al. [21] §; n = 20 (CT scans) (ROB: high) | Maximal transverse diameter: 1.27 mm (min: 1.2; max: 2.3) Height: 1.52 mm (min:1.1; max: 2.4) | |||
| Cornwall et al. [16]; n = 14 (CT scans) (ROB: high) | Maximum diameter: 1.3 mm (min: 1.07; max: 1.44) |
4. Discussion
4.1. Variability of the RW Area Anatomy
4.2. Constant Anatomical Features: Fustis and Three-Dimensional (3D) Shape of the RW Membrane
4.3. Implications for Future RW Devices
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CT | Computed Tomography |
| FMT | Floating Mass Transducer |
| RW | Round Window |
References
- Adunka, O.; Unkelbach, M.H.; Mack, M.; Hambek, M.; Gstoettner, W.; Kiefer, J. Cochlear implantation via the round window membrane minimizes trauma to cochlear structures: A histologically controlled insertion study. Acta Otolaryngol. 2004, 124, 807–812. [Google Scholar] [CrossRef]
- Briggs, R.J.S.; Tykocinski, M.; Xu, J.; Risi, F.; Svehla, M.; Cowan, R.; Stöver, T.; Erfurt, P.; Lenarz, T. Comparison of round window and cochleostomy approaches with a prototype hearing preservation electrode. Audiol. Neurootol. 2006, 11 (Suppl. S1), 42–48. [Google Scholar] [CrossRef] [PubMed]
- Colletti, V.; Soli, S.D.; Carner, M.; Colletti, L. Treatment of mixed hearing losses via implantation of a vibratory transducer on the round window. Int. J. Audiol. 2006, 45, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Beltrame, A.M.; Todt, I.; Sprinzl, G.; Profant, M.; Schwab, B. Consensus statement on round window vibroplasty. Ann. Otol. Rhinol. Laryngol. 2014, 123, 734–740. [Google Scholar] [CrossRef] [PubMed]
- Stewart, T.J.; Belal, A. Surgical anatomy and pathology of the round window. Clin. Otolaryngol. Allied Sci. 1981, 6, 45–62. [Google Scholar] [CrossRef]
- Su, W.Y.; Marion, M.S.; Hinojosa, R.; Matz, G.J. Anatomical measurements of the cochlear aqueduct, round window membrane, round window niche, and facial recess. Laryngoscope 1982, 92, 483–486. [Google Scholar] [CrossRef]
- Proctor, B.; Bollobas, B.; Niparko, J.K. Anatomy of the round window niche. Ann. Otol. Rhinol. Laryngol. 1986, 95, 444–446. [Google Scholar] [CrossRef]
- Marchioni, D.; Alicandri-Ciufelli, M.; Pothier, D.D.; Rubini, A.; Presutti, L. The round window region and contiguous areas: Endoscopic anatomy and surgical implications. Eur. Arch. Oto-Rhino-Laryngol. 2015, 272, 1103–1112. [Google Scholar] [CrossRef]
- Marchioni, D.; Soloperto, D.; Colleselli, E.; Tatti, M.F.; Patel, N.; Jufas, N. Round window chamber and fustis: Endoscopic anatomy and surgical implications. Surg. Radiol. Anat. 2016, 38, 1013–1019. [Google Scholar] [CrossRef]
- Yammine, K. Evidence-based anatomy. Clin. Anat. 2014, 27, 847–852. [Google Scholar] [CrossRef]
- Henry, B.M.; Tomaszewski, K.A.; Ramakrishnan, P.K.; Roy, J.; Vikse, J.; Loukas, M.; Tubbs, R.S.; Walocha, J.A. Development of the anatomical quality assessment (AQUA) tool for the quality assessment of anatomical studies included in meta-analyses and systematic reviews. Clin. Anat. 2017, 30, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Karkas, A.; Champfleur NMde Uziel, A.; Mondain, M.; Puel, J.-L.; Venail, F. Benefit of Preoperative Temporal Bone CT for Atraumatic Cochlear Implantation. Otol. Neurotol. 2018, 39, e186–e194. [Google Scholar] [CrossRef] [PubMed]
- Okuno, H.; Sando, I. Anatomy of the round window. A histopathological study with a graphic reconstruction method. Acta Otolaryngol. 1988, 106, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.; Blinder, G.; Perez, R.; Raveh, D. Standardized computed tomographic imaging and dimensions of the round-window niche. Int. Tinnitus J. 2005, 11, 158–162. [Google Scholar] [PubMed]
- Matin, F.; Gao, Z.; Repp, F.; John, S.; Lenarz, T.; Scheper, V. Determination of the Round Window Niche Anatomy Using Cone Beam Computed Tomography Imaging as Preparatory Work for Individualized Drug-Releasing Implants. J. Imaging 2021, 7, 79. [Google Scholar] [CrossRef]
- Cornwall, H.L.; Marway, P.S.; Bance, M. A Micro-Computed Tomography Study of Round Window Anatomy and Implications for Atraumatic Cochlear Implant Insertion. Otol. Neurotol. 2021, 42, 327–334. [Google Scholar] [CrossRef]
- Takahashi, H.; Takagi, A.; Sando, I. Computer-aided three-dimensional reconstruction and measurement of the round window and its membrane. Otolaryngol. Head Neck Surg. 1989, 101, 517–521. [Google Scholar] [CrossRef]
- Roland, P.S.; Wright, C.G.; Isaacson, B. Cochlear implant electrode insertion: The round window revisited. Laryngoscope 2007, 117, 1397–1402. [Google Scholar] [CrossRef]
- Atturo, F.; Barbara, M.; Rask-Andersen, H. Is the human round window really round? An anatomic study with surgical implications. Otol. Neurotol. 2014, 35, 1354–1360. [Google Scholar] [CrossRef]
- Angeli, R.D.; Lavinsky, J.; Setogutti, E.T.; Lavinsky, L. The Crista Fenestra and Its Impact on the Surgical Approach to the Scala Tympani during Cochlear Implantation. Audiol. Neurootol. 2017, 22, 50–55. [Google Scholar] [CrossRef]
- Mehanna, A.M.; Abdelnaby, M.M.; Eid, M. The Anatomy and Anatomical Variations of the Round Window Prechamber and Their Implications on Cochlear Implantation: An Anatomical, Imaging, and Surgical Study. Int. Arch. Otorhinolaryngol. 2020, 24, e288–e298. [Google Scholar] [CrossRef]
- Liang, J.; Nakmali, D.; Gan, R.Z.; Lu, H.; Dai, C. Investigating the Geometry and Mechanical Properties of Human Round Window Membranes Using Micro-Fringe Projection. Otol. Neurotol. 2021, 42, 319–326. [Google Scholar] [CrossRef]
- Jain, S.; Gaurkar, S.; Deshmukh, P.T.; Khatri, M.; Kalambe, S.; Lakhotia, P.; Chandravanshi, D.; Disawal, A. Applied anatomy of round window and adjacent structures of tympanum related to cochlear implantation. Braz. J. Otorhinolaryngol. 2019, 85, 435–446. [Google Scholar] [CrossRef]
- Takahashi, H.; Sando, I.; Takagi, A. Computer-aided three-dimensional reconstruction and measurement of the round window niche. Laryngoscope 1989, 99, 505–509. [Google Scholar] [CrossRef]
- Shakeel, M.; Spielmann, P.M.; Jones, S.E.; Hussain, S.S.M. Direct measurement of the round window niche dimensions using a 3-dimensional moulding technique—A human cadaveric temporal bone study. Clin. Otolaryngol. 2015, 40, 657–661. [Google Scholar] [CrossRef]
- Singla, A.; Sahni, D.; Gupta, A.K.; Loukas, M.; Aggarwal, A. Surgical anatomy of round window and its implications for cochlear implantation. Clin. Anat. 2014, 27, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Tóth, M.; Alpár, A.; Patonay, L.; Oláh, I. Development and surgical anatomy of the round window niche. Ann. Anat. 2006, 188, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Anschuetz, L.; Alicandri-Ciufelli, M.; Wimmer, W.; Bonali, M.; Caversaccio, M.; Presutti, L. The endoscopic anatomy of the cochlear hook region and fustis: Surgical implications. Acta Otorhinolaryngol. Ital. 2019, 39, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Goycoolea, M.V.; Lundman, L. Round window membrane. Structure function and permeability: A review. Microsc. Res. Tech. 1997, 36, 201–211. [Google Scholar] [CrossRef]
- Carpenter, A.M.; Muchow, D.; Goycoolea, M.V. Ultrastructural studies of the human round window membrane. Arch. Otolaryngol. Head Neck Surg. 1989, 115, 585–590. [Google Scholar] [CrossRef]
- Salt, A.N.; Plontke, S.K. Principles of local drug delivery to the inner ear. Audiol. Neurootol. 2009, 14, 350–360. [Google Scholar] [CrossRef]
- Garcia-Ibanez, L. Sonoinversion: A new audiosurgical system. Arch. Otolaryngol. 1961, 73, 268–272. [Google Scholar] [CrossRef] [PubMed]
- Alzamil, K.S.; Linthicum, F.H. Extraneous round window membranes and plugs: Possible effect on intratympanic therapy. Ann. Otol. Rhinol. Laryngol. 2000, 109, 30–32. [Google Scholar] [CrossRef] [PubMed]
- Plontke, S.K.R.; Plinkert, P.K.; Plinkert, B.; Koitschev, A.; Zenner, H.-P.; Löwenheim, H. Transtympanic endoscopy for drug delivery to the inner ear using a new microendoscope. Adv. Otorhinolaryngol. 2002, 59, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Crane, B.T.; Minor, L.B.; Della Santina, C.C.; Carey, J.P. Middle ear exploration in patients with Ménière’s disease who have failed outpatient intratympanic gentamicin therapy. Otol. Neurotol. 2009, 30, 619–624. [Google Scholar] [CrossRef]
- Si, Y.; Jiang, H.L.; Chen, Y.B.; Chu, Y.G.; Chen, S.J.; Chen, X.M.; He, W.H.; Zheng, Y.Q.; Zhang, Z.G. Round Window Niche Drilling with Intratympanic Steroid Is a Salvage Therapy of Sudden Hearing Loss. Audiol. Neurootol. 2018, 23, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Plontke, S.K.; Glien, A.; Rahne, T.; Mäder, K.; Salt, A.N. Controlled release dexamethasone implants in the round window niche for salvage treatment of idiopathic sudden sensorineural hearing loss. Otol. Neurotol. 2014, 35, 1168–1171. [Google Scholar] [CrossRef]
- Chiang, H.; Yu, M.; Aksit, A.; Wang, W.; Stern-Shavit, S.; Kysar, J.W.; Lalwani, A.K. 3D-Printed Microneedles Create Precise Perforations in Human Round Window Membrane in Situ. Otol. Neurotol. 2020, 41, 277–284. [Google Scholar] [CrossRef]
- Gehrke, M.; Verin, J.; Gnansia, D.; Tourrel, G.; Risoud, M.; Vincent, C.; Siepmann, F.; Siepmann, J. Hybrid Ear Cubes for local controlled dexamethasone delivery to the inner ear. Eur. J. Pharm. Sci. 2019, 126, 23–32. [Google Scholar] [CrossRef]
- Arnold, A.; Kompis, M.; Candreia, C.; Pfiffner, F.; Häusler, R.; Stieger, C. The floating mass transducer at the round window: Direct transmission or bone conduction? Hear Res. 2010, 263, 120–127. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marx, M.; Nieto, P.; Sagot, O.; de Bonnecaze, G.; Gallois, Y. Round Window Niche and Membrane Dimensions: A Systematic Review. Audiol. Res. 2025, 15, 90. https://doi.org/10.3390/audiolres15040090
Marx M, Nieto P, Sagot O, de Bonnecaze G, Gallois Y. Round Window Niche and Membrane Dimensions: A Systematic Review. Audiology Research. 2025; 15(4):90. https://doi.org/10.3390/audiolres15040090
Chicago/Turabian StyleMarx, Mathieu, Pauline Nieto, Olivier Sagot, Guillaume de Bonnecaze, and Yohan Gallois. 2025. "Round Window Niche and Membrane Dimensions: A Systematic Review" Audiology Research 15, no. 4: 90. https://doi.org/10.3390/audiolres15040090
APA StyleMarx, M., Nieto, P., Sagot, O., de Bonnecaze, G., & Gallois, Y. (2025). Round Window Niche and Membrane Dimensions: A Systematic Review. Audiology Research, 15(4), 90. https://doi.org/10.3390/audiolres15040090






