1. Introduction
Childhood hearing loss is a significant public health challenge that affects language acquisition, cognitive development, academic achievement, and socialization [
1]. There are more than 34 million children across the world with disabling hearing loss, mostly in low- and middle-income countries where hearing loss among children remains undiagnosed due to limited early screening and treatment services [
2]. Hearing loss in childhood remains unidentified because of parent ignorance, cultural misunderstanding, and the inaccessibility of treatment facilities. The long-term impact of hearing loss can be mitigated through early diagnosis and intervention, with the involvement of parents, especially mothers [
3].
Adequate knowledge among mothers regarding risk factors, signs, and warning signs of hearing loss, as well as accessible healthcare services, is fundamental for early detection and timely care [
4]. Childhood hearing loss is associated with preventable risk factors, including ototoxic medications, prenatal infections, noise exposure, premature births, and genetic predisposition, which are essential modifiable determinants of childhood hearing loss [
5,
6,
7]. Nevertheless, individuals from various cultural, educational, and socioeconomic backgrounds differ substantially in their awareness of these components, which influences the ability to diagnose early and take measures [
8]. There can be several reasons behind children’s hearing loss, which can broadly be grouped into genetic, prenatal, perinatal, postnatal, and environmental/lifestyle factors.
Figure 1 shows the principal categories of such risk factors.
In most developing nations, such as those in the Middle East and North Africa (MENA), inconsistent knowledge in mothers puts children at a higher likelihood of delayed diagnosis and developmental effects [
9]. Most MENA countries, including Jordan, present sociocultural and economic challenges peculiar to the global situation of childhood hearing loss. Although the field has advanced in terms of the development of hearing screening and healthcare delivery platforms in general, Jordan has also failed to properly sensitize mothers concerning risk factors and the ongoing detection of hearing loss [
10]. The understanding of risk factors for hearing loss and the importance of detecting it early varies among mothers, depending on their education, socioeconomic status (SES), and health literacy. Consanguineous marriages occur at a high rate in Jordan and increase the chances of genetic hearing disorder; thus, it is important to educate mothers on these risks [
11].
This paper discusses parental awareness of the risk factors for childhood hearing loss, with an emphasis on maternal education, socioeconomic status (SES), and health literacy. In this regard, this research will adopt a mixed-methods approach to yield both quantitative knowledge levels and qualitative insights into maternal awareness, healthcare-seeking behavior, and barriers to healthcare services. To design effective maternal health education programs and particular interventions in the early detection and prevention of childhood hearing loss in Jordan, several factors need to be understood [
12].
Hearing loss in children is a significant global public health issue affecting speech, language development, academic performance, and quality of life [
1]. Early detection and intervention can minimize adverse effects; however, parental awareness and knowledge hinder their success [
5]. This research establishes maternal understanding of the early indications of hearing loss and the need for early healthcare steps [
8,
12]. Despite this, there is very low knowledge of hearing loss risk factors in these countries, particularly in developing countries and in the Middle East [
3,
7].
Thus, there is little research on this issue in Jordan, where cultural, economic, and healthcare accessibility factors influence maternal knowledge. Studies from neighboring Arab countries, such as Egypt and Saudi Arabia, support the notion that parental knowledge is primarily based on parents’ educational level, socioeconomic status (SES), or lack of access to healthcare [
4,
8]. However, little empirical evidence has been obtained regarding how these factors affect Jordanian mothers’ knowledge and perception of hearing loss risk factors. Thus, maternal knowledge information is important in this context as Jordan has a high rate of consanguineous marriage (a genetic risk for congenital hearing loss) [
12]. Gaps in maternal awareness may result in delayed diagnosis or in early intervention being unavailable, leading to fewer educational and social opportunities for children affected by it [
2,
9]. It has also been suggested that their limited health literacy may delay healthcare-seeking behavior, which in turn impedes the long-term management of hearing loss [
13].
Despite the research on parental awareness of childhood deafness carried out in other countries, little research has been conducted regarding Jordanian mothers [
7,
9]. This results in an empirical gap in understanding how maternal education, socioeconomic status (SES), and health literacy relate to awareness of hearing loss risk factors. In most existing studies, however, descriptive assessments are provided without considering health behavior theories related to knowledge acquisition and healthcare decision-making [
3,
13]. There are several models, such as the Health Belief Model (HBM) and the Theory of Planned Behavior (TPB), that could provide much deeper insights into why some mothers are more knowledgeable than others.
Previous research relied on useful quantitative cross-sectional studies, which could not reveal why maternal awareness changes and how this happens [
5,
8]. A mixed-methods, quantitative and qualitative approach is needed to explore both statistical associations and contextual factors that shape maternal knowledge.
Regardless of regional disease awareness campaigns aimed at implementing early screening and parental education, several mothers still lack awareness of critical risk factors, including ototoxic medications, pregnancy infections, and genetic predisposition [
14]. In Jordan, there are no targeted awareness programs, and no studies have been conducted to determine whether mothers’ health literacy affects their ability to understand and utilize health information. It would be interesting to learn from the insights they provide to policymakers, healthcare providers, and educators, allowing them to address these gaps in terms of empirical, theoretical, methodological, and practical aspects. The findings will inform the development of culturally appropriate interventions to enhance maternal awareness, increase early screening uptake, and promote child health outcomes in Jordan [
11].
Although there have been attempts globally to enhance the early detection of hearing loss in children, the issue of maternal knowledge in early identification and intervention in Jordan has not been explored yet. Several researchers have studied parental awareness in different Middle Eastern and African settings [
4,
5,
8], but none systematically looked at how maternal education, financial status (socioeconomic status), and literacy regarding health affect awareness of the risk factors of hearing loss in Jordan. Considering the social and cultural context of the country, including the high frequency of consanguineous marriage, a known genetic risk factor for its most prominent genetic disease, this study contributes empirically to knowledge of an understudied population. By examining these maternal factors, the study aims to determine whether mothers can facilitate early detection and intervention for hearing loss.
This study brings more than an empirical contribution; it also presents a methodological advancement using mixed methodology (qualitative interviews and quantitative surveys). Most previous studies on maternal awareness were based on cross-sectional surveys, which cannot fully portray in-depth perceptions and contextual influences on maternal knowledge. Through the combination of statistical analysis and the deliberation of rich qualitative insights, this study offers a holistic account of the barriers and factors likely to influence mothers’ knowledge [
3]. In addition, it enriches theoretical discussions in the field by integrating models of health behavior such as the Health Belief Model (HBM) and the Theory of Planned Behavior (TPB) to understand how maternal perception, belief, and literacy levels affect health-seeking behavior. This study’s contribution is enhanced by the application of these theoretical frameworks, thereby bridging the gap between knowledge acquisition and real-world health decisions.
1.1. Accuracy and Comprehensiveness of Knowledge and Maternal Knowledge of Hearing Loss Risk Factors
The knowledge of mothers is vital in the early detection and prevention of childhood hearing loss, particularly in terms of its impact on parental decision-making and health-seeking behaviors [
12]. Mothers who are aware of the risk factors for hearing loss are more likely to identify early warning signs and seek medical help when needed [
5]. Risk factors include genetic predisposition, prenatal infections (such as rubella and cytomegalovirus), perinatal complications (such as preterm birth and neonatal hyperbilirubinemia), and exposure to ototoxic medications, as well as environmental factors (such as noise exposure) [
7]. Nevertheless, maternal misconceptions and the absence of trustworthy health info prevent early diagnosis and lead to inadequate management of children’s hearing loss [
15]. While studies have demonstrated that better maternal knowledge about health is related to better child health, enormous variation in the accuracy and coverage of maternal knowledge also exists [
9]. In settings where resources are scarce, mothers tend to have little awareness of health education programs and then rely on outdated beliefs or misinformation, which may hinder their ability to adopt proactive health measures [
5].
1.2. The Role of Mothers’ Education Level in Maternal Knowledge of Hearing Loss Risk Factors
Education is considered a significant factor in determining health awareness and healthcare practices [
13]. Research suggests that the higher a mother’s education level is, the more likely she is to have accurate knowledge about childhood diseases [
8]. Additionally, educated mothers are more capable of understanding medical information, recognizing symptoms, and determining whether intervention is needed earlier in seeking treatment [
2]. A study in South Africa demonstrated that mothers with tertiary education were more aware of the risk factors for hearing loss than mothers with lower educational levels [
3]. For instance, women with less-educated backgrounds may not be able to access scientifically right information related to their health and may put more trust in traditional beliefs or informal sources of information that lead to misconceptions about the prevention of hearing loss [
7].
1.3. The Impact of Socioeconomic Status (SES) on Maternal Knowledge of Hearing Loss Risk Factors
Socioeconomic status (SES) matters in terms of educational opportunities and access to healthcare and health information [
5], and so it plays a part in determining the level of health knowledge. Mothers with higher-socioeconomic-status (SES) backgrounds tend to have greater access to healthcare facilities and preventive health programs, as well as numerous awareness campaigns that enable them to be aware of risk factors and early intervention for hearing loss [
9]. Mothers from higher income levels are better at identifying the early signs of hearing loss and seeking medical attention earlier than those from lower income levels [
7]. On the other hand, mothers from low-SES backgrounds have barriers of access to healthcare such as financial capacity, low exposure to health education programs, and low primary healthcare-seeking behaviors [
3]. Traditionally, low-income mothers tend to rely more on traditional beliefs or knowledge from their community, which may or may not be scientifically correct [
8]. Consequently, more maternal knowledge of hearing loss risk should be observed to be associated with higher SES.
1.4. Moderating Role of Health Literacy
Health literacy refers to the knowledge encompassing one’s ability to comprehend, decode, process, and employ health-related information in health decision-making [
6]. Mothers with health literacy are able to understand health-related information and translate or critically analyze it. Additionally, their proper interaction with healthcare professionals provides more accurate and broader knowledge [
9]. For example, a Pakistani study found that mothers with better health literacy are more comfortable identifying early signs of childhood hearing loss and asking for professional assistance than those with less health literacy [
13]. However, on the other hand, low health literacy levels may lead to errors in interpreting medical advice, reliance on incorrect health beliefs, and delayed healthcare-seeking behaviors [
15]. There are gaps in mothers’ knowledge, despite exposure to health education, because they are likely to have low literacy levels and struggle to understand and apply medical terms correctly [
8].
1.5. Objective
The findings of this study have practical significance for healthcare policymakers, educators, and public health professionals in Jordan and other low- and middle-income countries facing similar challenges. The study identifies key determinants of maternal knowledge. It provides evidence-based recommendations for designing health awareness campaigns and community-based interventions to promote the early detection of childhood hearing loss. Additionally, understanding how health literacy affects maternal decision-making will enable healthcare providers to employ more effective communication strategies to disseminate and utilize critical health information [
10].
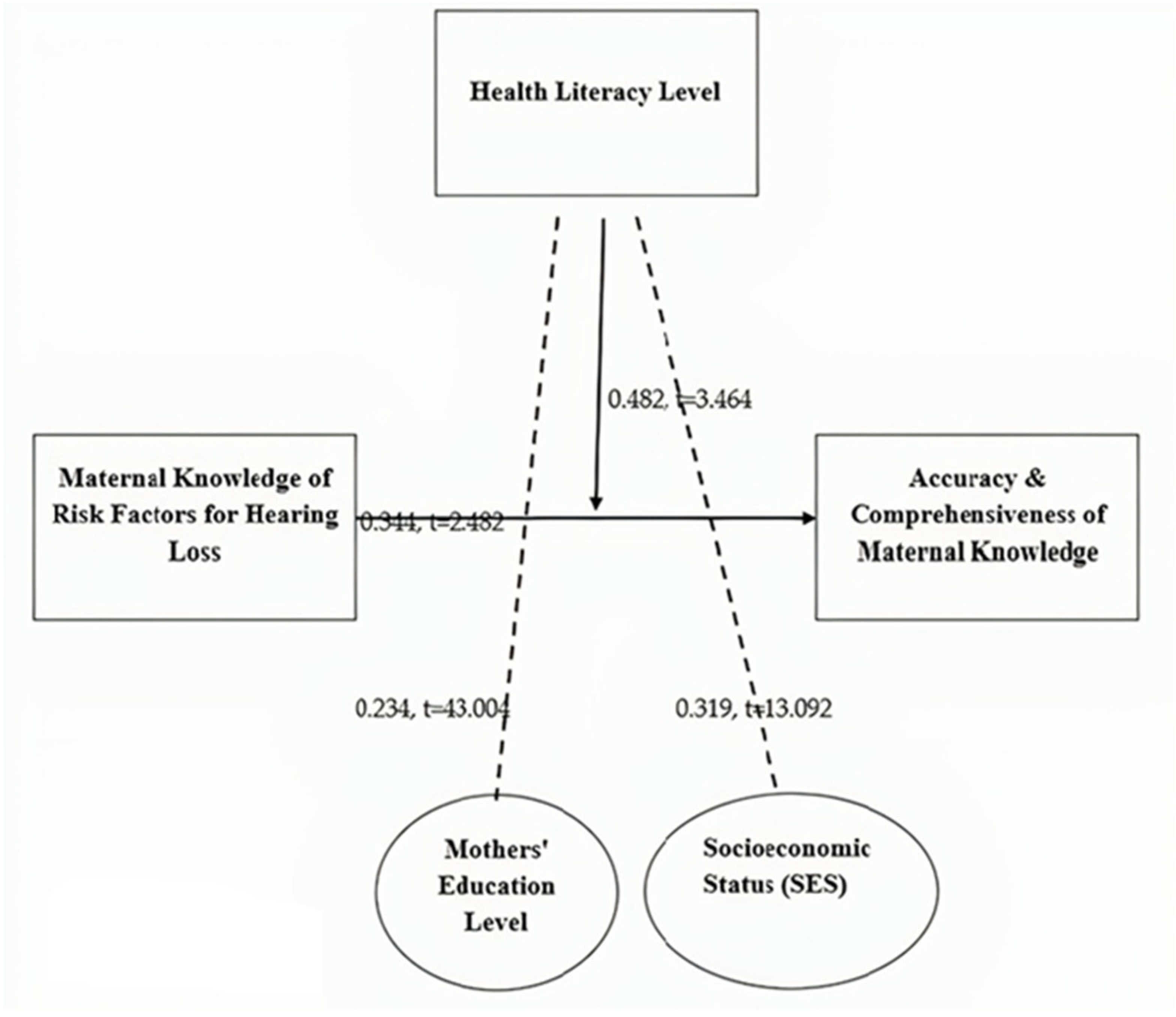
This study aims to examine Jordanian mothers’ knowledge of childhood hearing loss risk factors and investigate the impact of education level and socioeconomic status (SES) on the accuracy and comprehensiveness of this knowledge with the moderating effect of health literacy. The hypotheses of this study are as follows:
H1. Maternal knowledge of hearing loss risk factors plays a significant role in the accuracy and comprehensiveness of maternal knowledge.
H2. Maternal awareness of risk factors for hearing loss is positively associated with mothers’ education levels.
H3. There is a positive association between socioeconomic status (SES) and maternal knowledge about hearing loss risk factors.
H4. The relationship between maternal knowledge and the accuracy of maternal knowledge is moderated by maternal health literacy level.
4. Discussion of Themes
Interview thematic analysis provides important information about maternal knowledge of, challenges in, and responses to childhood hearing loss. Each section presents quotes from participants and contextual insights relevant to each of the themes discussed below.
4.1. Theme 1: Maternal Knowledge of Hearing Loss Causes
Mothers had different levels of awareness of the causes of child hearing loss. Some could correctly identify real factors, such as infections, genetics, or exposure to loud noise, while others had incorrect beliefs or did not know the details.
According to Interviewee 1, “I’ve heard that loud noises can cause hearing problems, but I don’t know how exactly that works”. In the same manner, Interviewee 3 explained “I always thought that hearing loss is mainly genetic, but I didn’t know that infections during pregnancy can also cause it”.
This theme indicates that there needs to be increased education on what causes hearing loss in children.
4.2. Theme 2: Sources of Information on Hearing Loss
The sources from which mothers heard information about childhood hearing loss were largely doctors, media, and family members. Many trusting medical professionals had doubts about the reliability of non-medical sources.
Interviewee 5 explained “Whenever I have questions, I will ask a doctor.” Sometimes, however, I also check social media for quick answers”. Another interviewee, Interviewee 8, took a different tack: “My mother told me about risks of hearing loss when I was pregnant but then later found out some of what she said was not accurate”.
This underlines the need to ensure that mothers receive accurate, accessible information from trusted sources.
4.3. Theme 3: Recognition of Early Signs
Mothers showed different levels of confidence in their children’s early symptoms of hearing loss. Some were assured that they could see signs, while others were not, especially for subtle points.
Interviewee 2 added “If a child doesn’t respond to sounds, that’s a clear sign. I’m not sure if there are further subtle signs that I should be on the lookout for”. Interviewee 7 admitted “I wouldn’t know if my baby had hearing loss unless it was something obvious. I assume they can hear fine”.
The theme points to what needs to be done to boost parental awareness of the early symptoms of hearing loss so that early intervention might be implemented.
4.4. Theme 4: Challenges in Understanding Medical Advice
Many participants had trouble with complicated medical terms and conflicting information from other healthcare providers, and obtaining comprehensive advice about hearing loss was hard.
According to Interviewee 4, “Doctors give explanations, but the medical terms are quite confusing sometimes”. According to Interviewee 9, “different doctors tell me different things, so I don’t always know what to believe”.
This theme emphasizes the importance of clear, simple, and consistent communication from healthcare professionals so that mothers can truly understand what they are listening to in terms of medical advice.
4.5. Theme 5: Influence of Education on Health Awareness
Maternal education was very effective in determining how well mothers understood the causes, symptoms, and treatment of childhood hearing loss. Comprehension was found to be better in those with higher education levels, whereas those with lower education backgrounds reported greater uncertainty.
As Interviewee 6 points out, “I studied health sciences, so I knew some of the risk factors before my child was even born”. On the other hand, Interviewee 10 stated “I never really learned about hearing loss”. I only found out about it when the doctor mentioned it during a checkup.”
This theme focuses on maternal education and its effects on health literacy, as well as the necessity to provide information for all mothers regardless of their education.
4.6. Theme 6: Impact of Socioeconomic Status
Financial constraints were very important in determining access to information and treatment of childhood hearing loss. Some mothers could afford specialist visits, whereas others could not attend them due to financial limitations.
According to Interviewee 3, “If my child would have had a hearing problem, I would have taken him immediately to a specialist.’ Since we have insurance, I’m not too much worried”. Nevertheless, Interviewee 7 experienced another story: “I can’t pay for private healthcare, so I have to use public services and it takes a long time”.
This theme shows that many families with limited finances need more affordable healthcare services.
4.7. Theme 7: Maternal Response to Diagnosis
Different responses were given by mothers to how they would respond if their children were diagnosed with hearing loss. Some were ready for medical assistance, and others resisted to the point of hesitating due to a lack of affordability and accessibility.
Interviewee 1 said “If my child has the diagnosis, I will not leave any stone unturned to get the best treatment for my child”. Interviewee 5 admitted the opposite: “I would be worried about the costs”. That must be expensive, as well as hearing aids and therapy.”
This theme reflects the necessity of adequate financial backing and public awareness of the resources involved in helping families of children with childhood hearing loss.
4.8. Theme 8: Improving Awareness and Support
Mothers provided various suggestions to improve hearing loss awareness and support systems for childhood hearing loss. Some emphasized the need for more educational programs, better access to pediatric hearing screenings, and more healthy communication from healthcare providers.
According to Interviewee 4, “More awareness campaigns should be conducted, especially for new mothers, so that they know what to watch out for”. Interviewee 9 said “I would have liked doctors to explain things more clearly and give us details of all the other support services”.
This theme reinforces the need for community education programs and more effective healthcare communication strategies to help mothers become educated about keeping tabs on hearing loss risks and remedies.
5. Discussion, Conclusions, and Implications
5.1. Discussion
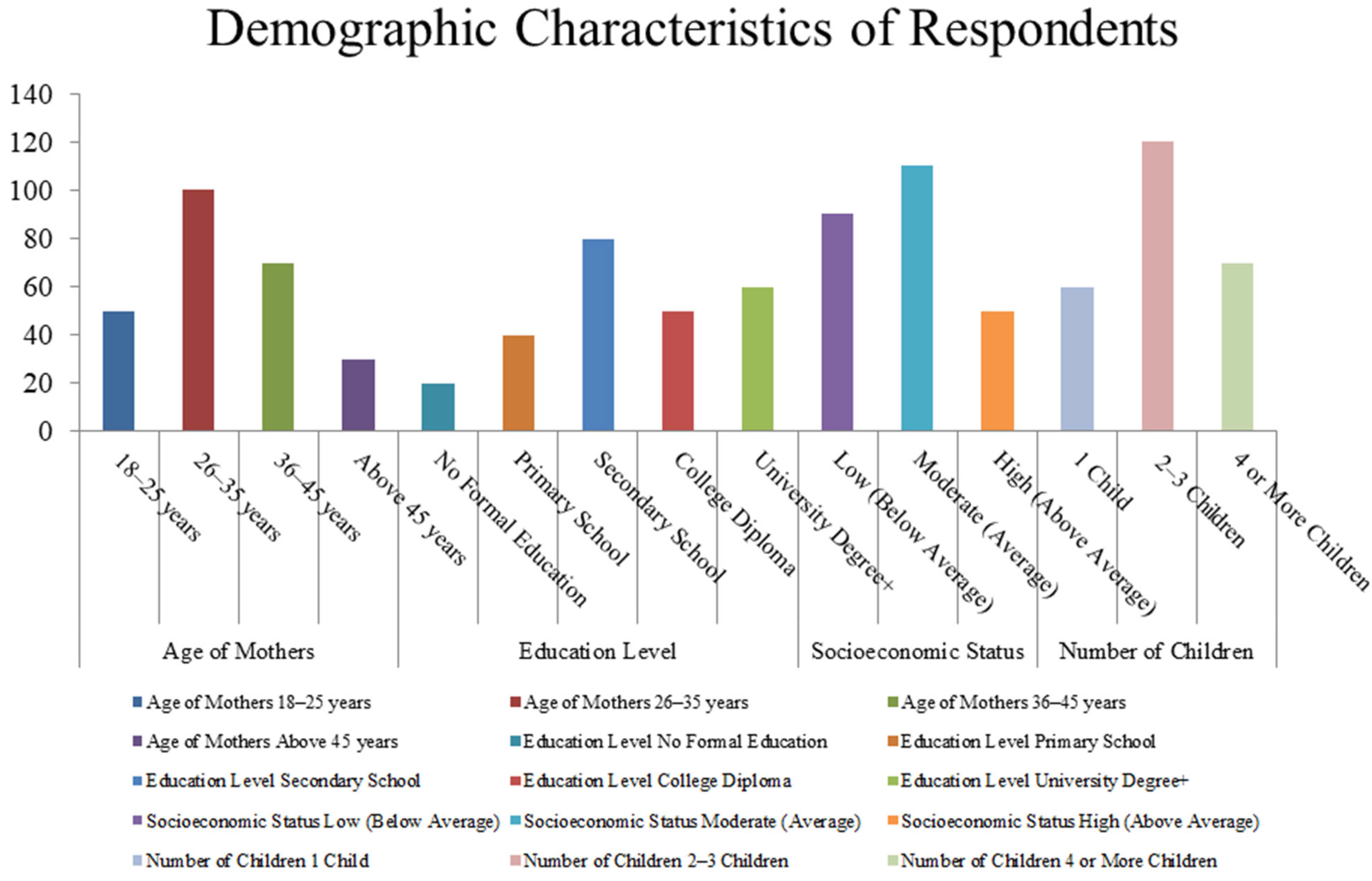
The researchers investigated the role of maternal knowledge, education level, social economic status (SES), and health literacy in the identification of risk factors of childhood hearing loss among Jordanian mothers. These findings were evaluated against the existing literature during discussions. Not only is this work novel in terms of the research focus and methodology, but it is also highly important for informing future public health initiatives targeting reducing childhood hearing loss through the education and awareness of mothers.
Hearing loss during childhood is a major global health problem that is present in about 34 million children across the world, with a major proportion of children living in low- and middle-income countries [
1]. The condition results from genetic, perinatal, and environmental factors that are, fortunately, preventable when detected early [
2]. More than 50–60 percent of cases of congenital hearing loss are thought to be due to genetic predisposition, especially in populations from the Middle East, where the rate of consanguineous marriages is high [
12]. In addition, maternal infections (such as rubella or cytomegalovirus), neonatal hyperbilirubinemia, premature birth, and low birth weight are known risk factors [
7].
Environmental factors such as ototoxic medications, recurrent ear infections, and excess noise likewise cause hearing loss in children [
9]. In developing areas, an incomplete or complete lack of parental awareness and no provision of healthcare facilities result in late diagnosis and treatment, leading to poor intervention, and this affects children’s language development, academic progress, and social isolation. To avoid long-term consequences, programs must increase parental education and expand early detection programs [
5].
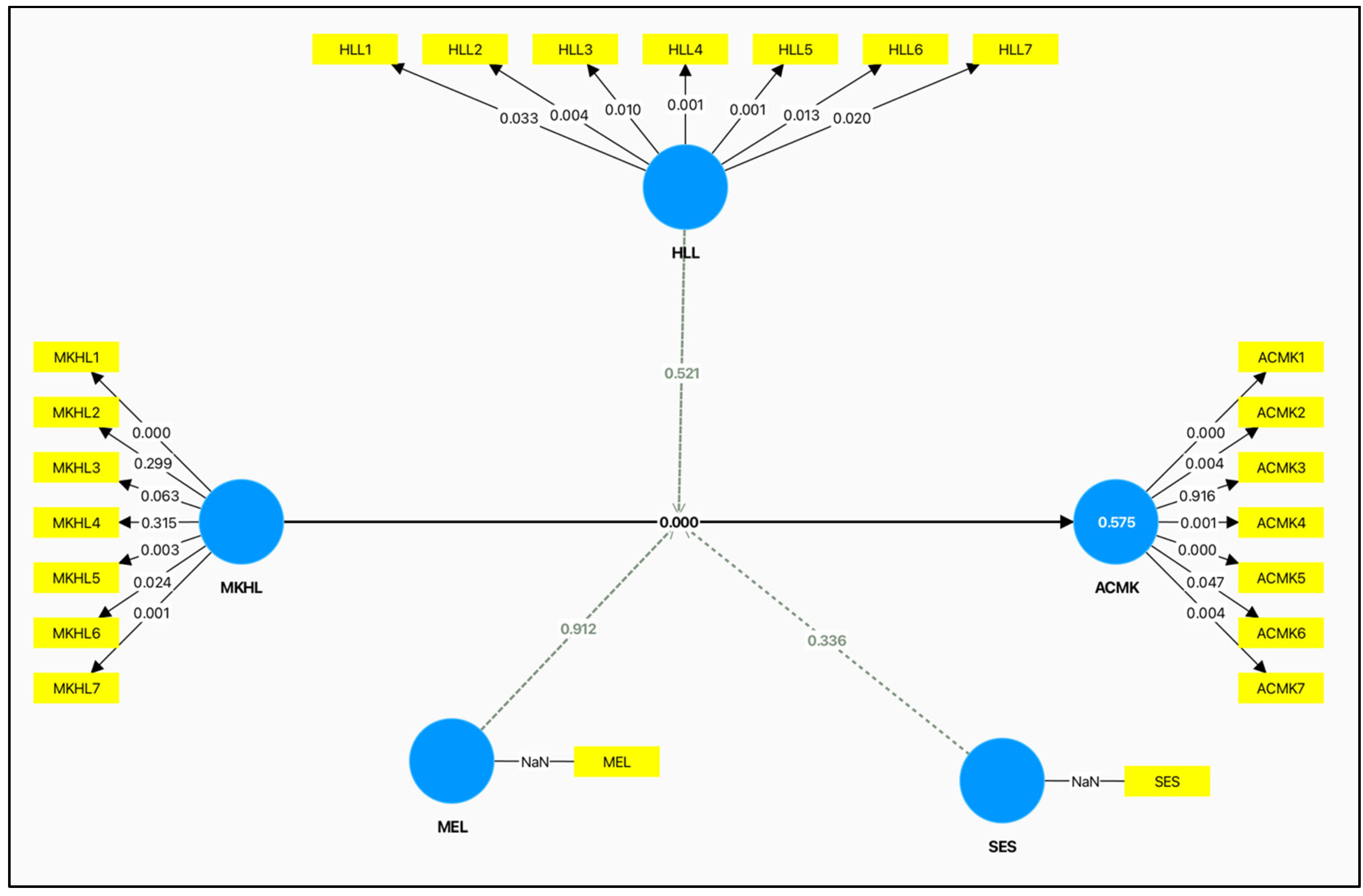
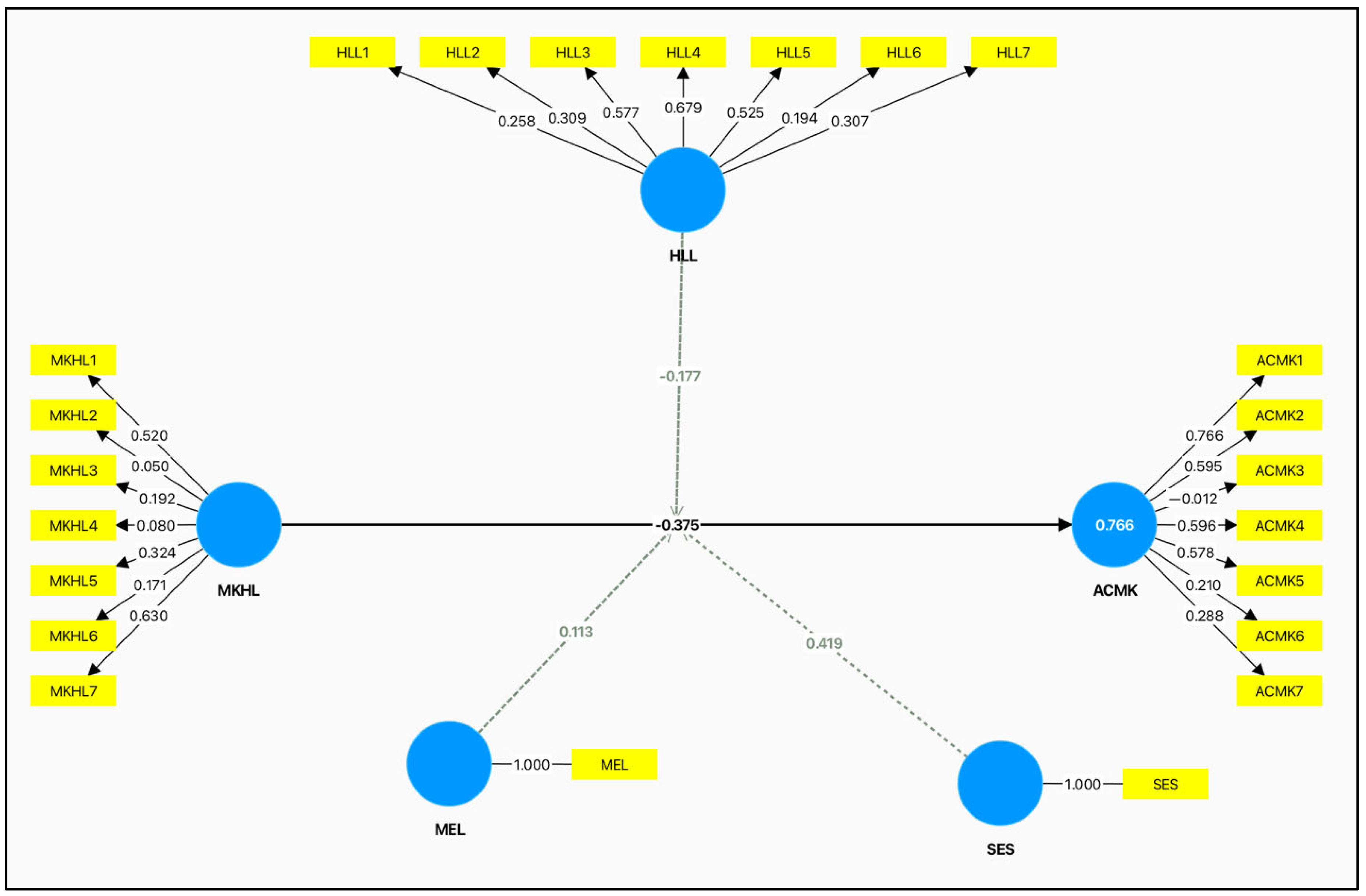
Quantitative analysis showed a significant positive relationship between maternal knowledge of hearing loss risk factors and maternal knowledge accuracy and comprehensiveness (β = 0.344; *
t = 2.482;
p = 0.000.) Therefore, it can be said that H1 is accepted, and this means that mothers who are more aware are possibly more likely to have accurate and more comprehensive knowledge. This has also been found in [
5,
12]; the more maternal knowledge there is, the better the ability to signpost early signs of congenital disabilities and recognize the need for early intervention.
The qualitative findings further supported this result; a number of respondents had stated that when provided with enough health information, they could identify risk factors. However, some mothers also had some misconceptions that hearing loss is connected to superstitions or external environmental factors not supported by science. This aligns with [
7], which states that knowledge is important, but the need for structured health education programs exists to combat misinformation.
The findings revealed a significant relationship between socioeconomic status (SES) and maternal knowledge (β = 0.243,
t = 43,004,
p = 0.000), supporting the hypothesis that higher SES improves access to education and healthcare resources. They also showed that mothers with higher socioeconomic status (SES) had a higher rate of awareness of the risk factors for hearing loss, which aligns with previous findings that financial stability is related to health literacy and healthcare utilization [
3,
9]. These findings underscore the importance of socioeconomic factors in accessing maternal health information, again highlighting the need to develop targeted interventions to address knowledge deficits, particularly among low-socioeconomic-status groups.
Nevertheless, qualitative interviews revealed that mothers from lower-SES backgrounds frequently used informal sources such as family and social media, which sometimes yielded misinformation. Disparities in healthcare access impacted a participant, who spoke about the affordability of medical consultations. The implications of these findings point to the need for free or subsidized health education programs for low-income mothers.
H3 was supported, with education level showing a significant positive association with maternal knowledge (β = 0.319,
t = 13.092,
p = 0.001). This result agrees with [
2] and [
7], which showed that education enhances health comprehension and awareness.
After the qualitative analysis, it was seen that highly educated mothers could more easily process medical information, while less-educated mothers had difficulty digesting complex medical advice. Less-educated mothers said they had merely heard the doctor and done what they said without understanding the reasoning behind it. This is corroborated by [
13], which stated that maternal education leads to health-related decisions.
H4 was confirmed by the fact that health literacy significantly moderated the relationship between maternal knowledge and the accuracy of knowledge (β = 0.482,
t = 3.464,
p = 0.001). This is consistent with [
3,
9], who suggested that health literacy enables individuals to read, interpret, and use health information as needed.
The qualitative results showed that mothers with lower health literacy had difficulty understanding medical explanations, resulting in uncertainty and a delay in seeking healthcare. A few participants reported being overwhelmed by the use of technical jargon by healthcare providers. These findings highlight the importance of developing simple, clear, and culturally appropriate communications to relay medical recommendations that mothers can fully understand. Additionally, the introduction of the Jordanian Newborn Hearing Screening Program in 2021 has made a substantial contribution to the enhancement of early hearing loss identification. The national program could be useful in reducing the pressure on parents, particularly mothers, through the early detection and treatment of childhood hearing loss [
22].
5.2. Conclusions and Implications
The results of this study highlight important gaps in Jordanian mothers’ knowledge of the risk factors for childhood hearing loss. While many mothers knew common causes, such as infections and genetic predisposition, misconceptions and a lack of understanding of environmental and perinatal risk factors remained. For quantitative results, this meant a very strong relationship between maternal knowledge and the measures of education level, SES, and health literacy. Those mothers with higher education and SES were more aware and correct in identifying risk factors. Qualitative findings also indicated that mothers sometimes received information from doctors, family, and media, but the reliability of these sources of information varied. Health literacy barriers also led to challenges that many participants faced in understanding medical advice, highlighting the need for clearer healthcare communication. The present results are consistent with previous studies on the impact of parent educational and socioeconomic status on enhancing health knowledge [
3,
5]. According to these findings, specific approaches should be given priority, including community-based workshops, mobile health campaigns, and counseling within hospitals, to ensure an increase in maternal awareness about the risk factors of hearing loss. Moreover, health communication must be made elementary to accommodate different health literacy levels. Maternal understanding may be enhanced by visual aids as well as multilingual resources.
The results of this study are important for healthcare practitioners, policymakers, and public health educators. Therefore, education and skills development should be targeted to increase maternal awareness of hearing loss risk factors, particularly among females with lower educational attainment and financial constraints. Moreover, AI technologies may be a valuable addition to audiological training, making the process of disseminating knowledge about the risks of developing hearing loss much more efficient. Advances in Artificial Intelligence-based health education platforms and individualized digital learning tools in recent years can help shape educational material to meet the needs of individuals, making it more accessible and easier to understand [
22,
23].
Community workshops, mobile health campaigns, and hospital-based counseling programs can enhance knowledge and facilitate early intervention. Second, medical communication needs to be simplified by healthcare providers so that mothers who have different health literacy levels can access the information provided [
12]. Furthermore, knowledge could be increased by incorporating visual aids and text resources in multiple languages. Financial and structural barriers to hearing healthcare services need to be addressed by increasing access to hearing screenings on a lump sum basis and pediatric audiology care. More specifically, based on this study’s results, these strategies could be implemented in national health initiatives aimed at reducing childhood hearing loss through enhanced parental education and early detection. Further research will focus on developing longitudinal measures of maternal knowledge improvement and assessing the effectiveness of educational programs designed according to the diversity of populations.
5.3. Limitations and Suggestions for Future Studies
Although it does provide some valuable insights, this study has several limitations. To start with, the cross-sectional research design is limiting in the establishment of the cause-and-effect relationships between maternal knowledge and such factors as education, SES, and health literacy. In future research, longitudinal designs are recommended to monitor maternal awareness over time and determine the effects of educational interventions. Also, it is notable that no information was collected about the presence of hearing loss in the family members of the children, particularly in participating mothers. Maternal knowledge, awareness, and health-seeking behavior may be influenced by personal experience with hearing loss, and this aspect should be considered by future studies to gain a deeper understanding of its role. Longitudinal studies of future research should examine how maternal awareness varies through time and, second, the effect of educational treatments. Second, the self-reported data used in this study suggest a risk of social desirability bias, as mothers may exaggerate their awareness of the risk factors associated with hearing loss. In further research, using objective measures, such as standardized testing, is recommended to better understand the level of maternal knowledge. Future studies would include objective measures of maternal knowledge, such as standardized tests or more objective observational methods.
The analysis was conducted within a single geographical area in Jordan, which reduces its generalizability. Future research should expand the sample to obtain a more diverse and nationally representative one, in order to investigate potential regional variations in maternal knowledge and healthcare access. The second limitation was the small sample size during the qualitative phase. Although the sample was adequate to carry out the thematic analysis, a larger sample size, comprising focus groups or ethnographic studies, would provide greater insight into the concerns and perceptions of mothers. Additionally, this study examined the roles of education, SES, and health literacy but did not explore other possible influences, such as cultural beliefs, healthcare accessibility, and paternal involvement. Further studies are required to examine other variables, including cultural beliefs, access to healthcare, and the presence of the father in the decision-making process regarding childhood hearing impairment. This would give better insights into parental knowledge and health-seeking behavior.