Communication Outcomes of Children with Hearing Loss: A Comparison of Two Early Intervention Approaches
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Objectives and Corresponding Variables
- Describe communication functioning prior to and upon discharge from early intervention (EI) for both the LSL-SA and TSLT groups.
- ○
- Variables:
- ▪
- Communication Functioning: speech intelligibility, expressive vocabulary, receptive language, expressive language, audition, cognitive–linguistic skills (all ordinal variables: delayed, age-appropriate).
- 2.
- Compare communication outcomes between the LSL-SA and TSLT groups.
- ○
- Variables:
- ▪
- Type of Communication Intervention: TSLT OR LSL-SA (nominal).
- ▪
- Outcome Measures: proportion of children with age-appropriate communication skills at discharge (ordinal).
- 3.
- Determine associations between selected study variables and communication outcomes within each intervention approach.
- ○
- Variables:
- ▪
- Age at Identification of Hearing Loss (ratio, years).
- ▪
- Age at Diagnosis of Hearing Loss (ratio, years).
- ▪
- Age at Amplification (ratio, years).
- ▪
- Type of Amplification Device (hearing aid or cochlear implant, nominal).
- ▪
- Age at Start of EI (ratio, years).
- ▪
- Duration of EI (ratio, years).
- ▪
- Degree of Aided Audiogram (ordinal: normal, mild, moderate, severe).
- ▪
- Home Language vs. Language Used in Therapy (nominal: matched or not matched).
- 4.
- Identify the type of school recommended after EI based on communication outcomes.
- ○
- Variables:
- ▪
- Type of School Recommended (nominal: mainstream or specialized).
2.3. Study Sample and Demographics
2.4. Inclusion and Exclusion Criteria
2.5. Procedures
2.6. Data Collection Tool
2.7. Standardized Assessment Tools
2.8. Data Analysis
- Objectives 1 and 2: Comparing Communication Functioning and Outcomes:
- Objective 3: Associations Between Study Variables and Communication Outcomes:
- Objective 4: School Placement After EI:
2.9. Ethical Considerations
2.10. Validity and Reliability
2.11. Data Management
3. Results
3.1. Demographic Profile of Participants
3.2. Communication Functioning Prior to the Commencement of EI and upon Discharge from Therapy in the TSLT and LSL-SA Groups
3.2.1. The Description of Communication Functioning Prior to the Commencement of EI to the Communication Outcomes upon Discharge from Therapy in the TSLT Group (n = 64) Is Depicted in Table 2
3.2.2. The Description of Communication Functioning Prior to the Commencement of EI to the Communication Outcomes upon Discharge from Therapy in the LSL-SA Group (n = 62) Is Depicted in Table 2
3.3. Comparing the Communication Outcomes Between the Two Groups
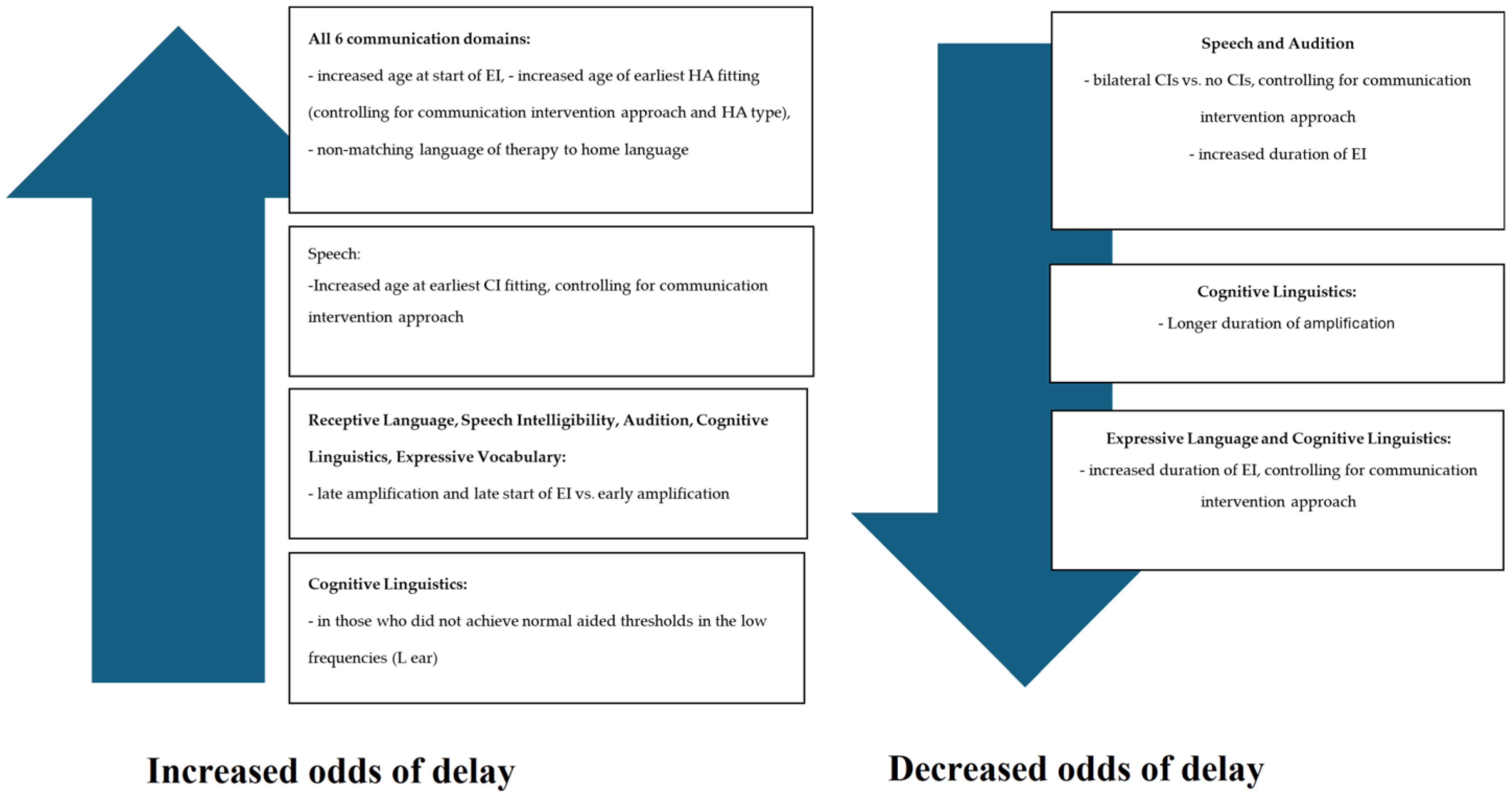
3.4. Determining If Any Associations Exist Between Selected Study Variables and Communication Outcomes Within Each Communication Intervention Approach
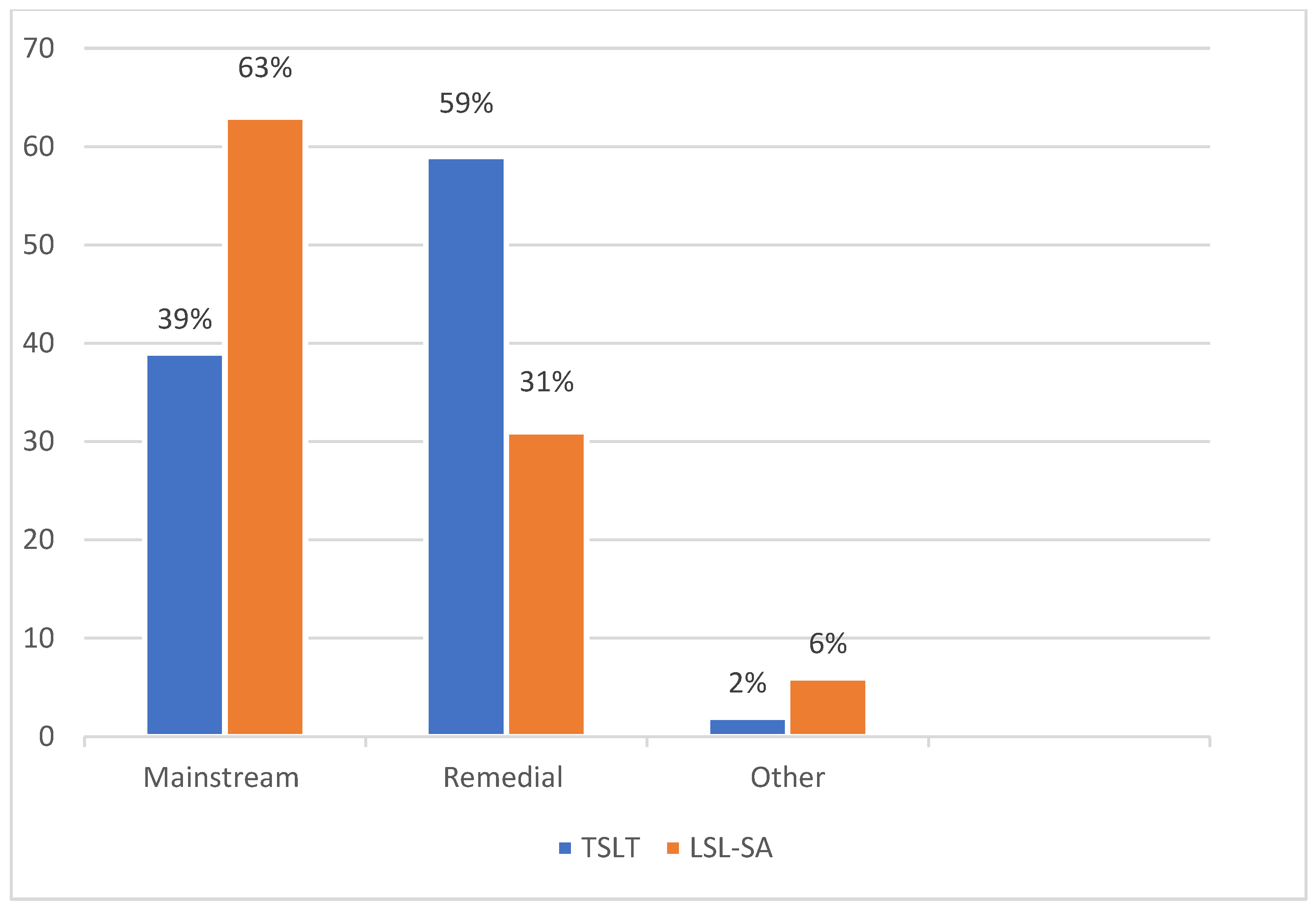
3.5. Identifying the Type of School Recommended After EI Based on Communication Outcomes
4. Discussion
5. Conclusions
6. Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LSL-SA | Listening and Spoken Language-South Africa |
| TSLT | Traditional Speech-Language Therapy |
| EHDI | Early Hearing Detection and Intervention |
| NHS | Newborn Hearing Screening |
| EI | Early Intervention |
| AVT | Auditory Verbal Therapy |
| LMIC | Low-middle-income country |
| ECD | Early Childhood Development |
| SASL | South African Sign Language |
| NDP | National Development Plan |
| HPCSA | Health Professions Council of South Africa |
| CI | Cochlear Implant |
| DALYs | Disability-Adjusted Life Years |
References
- Aanondsen, C.M.; Jozefiak, T.; Lydersen, S.; Heiling, K.; Rimehaug, T. Deaf and hard-of-hearing Children and Adolescents’ Mental health, Quality of Life and Communication. BMC Psychiatry 2023, 23, 297. [Google Scholar] [CrossRef]
- Wong, C.L.; Ching, T.Y.; Leigh, G.; Cupples, L.; Button, L.; Marnane, V.; Whitfield, J.; Gunnourie, M.; Martin, L. Psychosocial development of 5-year-old children with hearing loss: Risks and protective factors. Int. J. Audiol. 2016, 57 (Suppl. 2), S81–S92. [Google Scholar] [CrossRef] [PubMed]
- Casoojee, A.; Khoza-Shangase, K.; Kanji, A. Exploration of parental perspectives and involvement in therapeutic communication approaches for Deaf and/or hard-of-hearing children at special schools in South Africa. Med. Humanit. 2025. [Google Scholar] [CrossRef]
- Joint Committe on Infant Hearing. Year 2000 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. J. Early Hear. Detect. Interv. 2019, 4, 1–44. [Google Scholar]
- Dehorter, N.; Del Pino, I. Shifting Developmental Trajectories During Critical Periods of Brain Formation. Front. Cell. Neurosci. 2020, 14, 283. [Google Scholar] [CrossRef] [PubMed]
- Ashori, M. Impact of Auditory-Verbal Therapy on Executive Functions in Children with Cochlear Implants. J. Otol. 2022, 17, 130–135. [Google Scholar] [CrossRef]
- Auditory Verbal UK. Auditory Verbal Therapy Position Paper. Auditory Verbal. 2023. Available online: https://www.avuk.org/auditory-verbal-therapy-position-paper#B (accessed on 20 December 2024).
- Davidson, L.; Osman, A.; Geers, A. The Effects of Early Intervention on Language Growth after Age 3 for Children with Permanent Hearing Loss. J. Early Hear. Detect. Interv. 2021, 6, 1–11. [Google Scholar]
- Jeong, J.; Franchett, E.E.; Ramos de Oliveira, C.V.; Rehmani, K.; Yousafzai, A.K. Parenting interventions to promote early child development in the first three years of life: A global systematic review and meta-analysis. PLoS Med. 2021, 18, e1003602. [Google Scholar] [CrossRef]
- Moore, D.R.; Zobay, O.; Ferguson, M.A. Minimal and Mild Hearing Loss in Children. Ear Hear. 2019, 41, 1. [Google Scholar] [CrossRef]
- Shojaei, E.; Jafari, Z.; Gholami, M. Effect of Early Intervention on Language Development in Hearing-Impaired Children. Iran. J. Otorhinolaryngol. 2016, 28, 13–21. [Google Scholar]
- Ching, T.Y.C. Is Early Intervention Effective in Improving Spoken Language Outcomes of Children with Congenital Hearing Loss? Am. J. Audiol. 2015, 24, 345–348. [Google Scholar] [CrossRef]
- Ching, T.Y.C.; Dillon, H.; Leigh, G.; Cupples, L. Learning from the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study: Summary of 5-year findings and implications. Int. J. Audiol. 2017, 57 (Suppl. 2), S105–S111. [Google Scholar] [CrossRef] [PubMed]
- Dettman, S.J.; Dowell, R.C.; Choo, D.; Arnott, W.; Abrahams, Y.; Davis, A.; Dornan, D.; Leigh, J.; Constantinescu, G.; Cowan, R.; et al. Long-term Communication Outcomes for Children Receiving Cochlear Implants Younger Than 12 Months. Otol. Neurotol. 2016, 37, e82–e95. [Google Scholar] [CrossRef] [PubMed]
- Fulcher, A.N.; Purcell, A.; Baker, E.; Munro, N. Factors influencing speech and language outcomes of children with early identified severe/profound hearing loss: Clinician-identified facilitators and barriers. Int. J. Speech-Lang. Pathol. 2015, 17, 325–333. [Google Scholar] [CrossRef]
- Tomblin, J.B.; Oleson, J.J.; Ambrose, S.E.; Walker, E.; Moeller, M.P. The Influence of Hearing Aids on the Speech and Language Development of Children With Hearing Loss. JAMA Otolaryngol.–Head Neck Surg. 2014, 140, 403. [Google Scholar] [CrossRef]
- Lew, J.; Purcell, A.A.; Doble, M.; Lim, L.H. Hear here: Children with hearing loss learn words by listening. Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 1716–1725. [Google Scholar] [CrossRef] [PubMed]
- Meinzen-Derr, J.; Wiley, S.; Choo, D.I. Impact of Early Intervention on Expressive and Receptive Language Development Among Young Children with Permanent Hearing Loss. Am. Ann. Deaf 2011, 155, 580–591. [Google Scholar] [CrossRef]
- Vohr, B.; Pierre, L.S.; Topol, D.; Jodoin-Krauzyk, J.; Bloome, J.; Tucker, R. Association of maternal communicative behavior with child vocabulary at 18–24months for children with congenital hearing loss. Early Hum. Dev. 2010, 86, 255–260. [Google Scholar] [CrossRef]
- Korver, A.M.H.; Konings, S.; Dekker, F.W.; Beers, M.; Wever, C.C.; Frijns, J.H.M.; Oudesluys-Murphy, A.M.; for the DECIBEL Collaborative Study Group. Newborn Hearing Screening vs Later Hearing Screening and Developmental Outcomes in Children With Permanent Childhood Hearing Impairment. JAMA 2010, 304, 1701. [Google Scholar] [CrossRef]
- Kennedy, C.R.; McCann, D.C.; Campbell, M.J.; Law, C.M.; Mullee, M.; Petrou, S.; Watkin, P.; Worsfold, S.; Yuen, H.M.; Stevenson, J. Language Ability after Early Detection of Permanent Childhood Hearing Impairment. N. Engl. J. Med. 2006, 354, 2131–2141. [Google Scholar] [CrossRef]
- Naidoo, N.; Khan, N.B. Analysis of barriers and facilitators to early hearing detection and intervention in KwaZulu-Natal, South Africa. S. Afr. J. Commun. Disord. 2022, 69, 839. [Google Scholar] [CrossRef] [PubMed]
- Maluleke, N. A call for linguistic and culturally congruent family-centred early hearing detection and intervention programmes in South Africa. S. Afr. J. Commun. Disord. 2024, 71, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Casoojee, A. Communication Intervention in South Africa: Advocating for the Listening and Spoken Language Approach. S. Afr. J. Commun. Disord. 2024, 71, 6. [Google Scholar] [CrossRef]
- Störbeck, C.; Young, A. The HI HOPES data set of deaf children under the age of 6 in South Africa: Maternal suspicion, age of identification and newborn hearing screening. BMC Pediatr. 2016, 16, 45. [Google Scholar] [CrossRef] [PubMed]
- Department of Women, Youth and Persons with Disabilities. White Paper on the Rights of Persons with Disabilities. Republic of South Africa. 2015. Available online: https://www.gov.za/sites/default/files/gcis_documents/WPRDP%20Booklet.pdf (accessed on 20 December 2024).
- Llywodraeth Cymru Welsh Government. EU Structural Funds 2014 to 2020: Social Model of Disability. GOV.WALES. 2021. Available online: https://www.gov.wales/eu-structural-funds-2014-2020-social-model-disability (accessed on 21 December 2024).
- Roberts, M.Y. Parent-Implemented Communication Treatment for Infants and Toddlers With Hearing Loss: A Randomized Pilot Trial. J. Speech Lang. Hear. Res. 2019, 62, 143–152. [Google Scholar] [CrossRef]
- Jackson, C.W.; Schatschneider, C. Rate of Language Growth in Children with Hearing Loss in an Auditory-Verbal Early Intervention Program. Am. Ann. Deaf 2014, 158, 539–554. [Google Scholar] [CrossRef]
- Sacks, C.; Shay, S.; Repplinger, L.; Leffel, K.R.; Sapolich, S.G.; Suskind, E.; Tannenbaum, S.; Suskind, D. Pilot testing of a parent-directed intervention (Project ASPIRE) for underserved children who are deaf or hard of hearing. Child Lang. Teach. Ther. 2013, 30, 91–102. [Google Scholar] [CrossRef]
- Percy-Smith, L.; Tønning, T.L.; Josvassen, J.L.; Mikkelsen, J.H.; Nissen, L.; Dieleman, E.; Hallstrøm, M.; Cayé-Thomasen, P. Auditory verbal habilitation is associated with improved outcome for children with cochlear implant. Cochlear Implant. Int. 2017, 19, 38–45. [Google Scholar] [CrossRef]
- Henner, J.; Robinson, O. Unsettling Languages, Unruly Bodyminds: A Crip Linguistics Manifesto. J. Crit. Study Commun. Disabil. 2023, 1, 7–37. [Google Scholar] [CrossRef]
- Department of Social Development. The National Development Plan 2030 Persons with Disabilities as Equal Citizens Pilot Study on the Experiences of Persons with Disabilities in Learnerships, Higher Education Institutions and Public Entities Building a Caring Society. Together. 2015. Available online: https://www.un.org/development/desa/disabilities/wp-content/uploads/sites/15/2016/02/Disability-Analysis-of-the-National-Development-Plan-2030.pdf (accessed on 20 December 2024).
- South African Early Childhood Review. Knowledge Information & Data Solutions. 2016. Available online: https://ilifalabantwana.co.za/project/south-african-early-childhood-review-2016/ (accessed on 16 December 2024).
- LeClair, K.L.; Saunders, J.E. Meeting the educational needs of children with hearing loss. Bull. World Health Organ. 2019, 97, 722–724. [Google Scholar] [CrossRef]
- Sawula, N. The Accessibility of Further Education and Training Colleges to South African Sign Language Users in KwaZulu-Natal. Ph.D. Thesis, Durban University of Technology, Durban, South Africa, 2018. [Google Scholar]
- Jacobson, L. Is South Africa Listening? The Writer Studio. 2015. Available online: http://www.writerstudio.co.za/lana-jacobson-portfolio/health-writing/70-deaf-people-is-south-africa-listening.html (accessed on 16 December 2024).
- Deaf Federation of South Africa (DeafSA). Policy on the Provision and Regulation of South African Sign Language Interpreters. 2009. Available online: http://deafsa.co.za/resources/SASLI_policy.pdf (accessed on 20 December 2024).
- World Health Organization. Childhood Hearing Loss Act Now, Here’s How! 2016. Available online: https://iris.who.int/bitstream/handle/10665/204507/WHO_NMH_NVI_16.1_eng.pdf?sequence=1 (accessed on 20 December 2024).
- SAS Institute Inc. SAS Software, Version 9.4 for Windows; SAS Institute Inc.: Cary, NC, USA, 2010. [Google Scholar]
- Posel, D. Race as Common Sense: Racial Classification in Twentieth-Century South Africa. Afr. Stud. Rev. 2001, 44, 87. [Google Scholar] [CrossRef]
- South African Cochlear Implant Group. Quality Standards. Cochlear Implant Services for Adults and Children in South Africa. South African Cochlear Implant Group. 2022. Available online: https://www.sacig.org.za/wp-content/uploads/2024/03/SACIG-Quality-Standards-2022.pdf (accessed on 21 December 2024).
- Health Professions Council of South Africa. Professional Boards—HPCSA. Speech, Language and Hearing. 2024. Available online: https://www.hpcsa.co.za/?contentId=0&menuSubId=54&actionName=Professional%20Boards (accessed on 16 December 2024).
- Houston, K.; Bradham, T. Cochlear Implants for Children Who Are Deaf or Hard of Hearing. In The NCHAM Book. A Resource Guide for Early Hearing Detection and Intervention; Schmeltz, L., Ed.; Chapter 15; NCHAM National Center for Hearing Assessment and Management, Utah State University: Logan, UT, USA, 2022; pp. 15-1–15-30. Available online: https://www.infanthearing.org/ehdi-ebook/ (accessed on 16 December 2024).
- Kleijbergen, W.J.; Sparreboom, M.; Mylanus, E.A.M.; de Koning, G.; Helleman, H.W.; Boermans, P.P.B.M.; Frijns, J.H.M.; Vroegop, J.L.; van der Schroeff, M.P.; Gelders, E.E.J.; et al. Benefit of sequential bilateral cochlear implantation in children between 5 to 18 years old: A prospective cohort study. PLoS ONE 2022, 17, e0271497. [Google Scholar] [CrossRef] [PubMed]
- Bhamjee, A.; Mahomed-Asmail, F.; Perold, J.; Loock, J.W.; le Roux, T. Cochlear implantation in South Africa (part 2). S. Afr. Med. J. 2022, 112, 71–75. [Google Scholar] [CrossRef]
- Moodley, S.; Storbeck, C. Narrative review of EHDI in South Africa. S. Afr. J. Commun. Disord. 2015, 62, E1–E10. [Google Scholar] [CrossRef] [PubMed]
- Shearer, A.E. Hearing Loss in the 21st Century and beyond: A New Era of Precision Diagnosis and Treatment Using Genomics. Volta Rev. 2023, 123, 35. [Google Scholar] [CrossRef]
- Korver, A.M.H.; Smith, R.J.H.; Van Camp, G.; Schleiss, M.R.; Bitner-Glindzicz MA, K.; Lustig, L.R.; Usami, S.; Boudewyns, A.N. Congenital hearing loss. Nat. Rev. Dis. Primers 2017, 3, 16094. [Google Scholar] [CrossRef]
- Mulwafu, W.; Kuper, H.; Ensink, R.J.H. Prevalence and causes of hearing impairment in Africa. Trop. Med. Int. Health 2015, 21, 158–165. [Google Scholar] [CrossRef]
- Casoojee, A.; Khoza-Shangase, K.; Kanji, A. A comparative study of learning outcomes for hearing-impaired foundation phase learners. S. Afr. J. Child. Educ. 2024, 14, 11. [Google Scholar] [CrossRef]
- Bergeron, F.; Berland, A.; Demers, D.; Gobeil, S. Contemporary Speech and Oral Language Care for Deaf and Hard-of-Hearing Children Using Hearing Devices. J. Clin. Med. 2020, 9, 378. [Google Scholar] [CrossRef]
- Lieu, J.E.C.; Kenna, M.; Anne, S.; Davidson, L. Hearing Loss in Children. JAMA 2020, 324, 2195. [Google Scholar] [CrossRef]
- Banda, F.M.; Powis, K.M.; Mokoka, A.B.; Mmapetla, M.; Westmoreland, K.D.; David, T.; Steenhoff, A.P. Hearing Impairment Among Children Referred to a Public Audiology Clinic in Gaborone, Botswana. Global Pediatric Health 2018, 5, 2333794X1877007. [Google Scholar] [CrossRef]
- Schwartz, R.G. (Ed.) Handbook of Child Language Disorders; Psychology Press: New York, NY, USA, 2017; Available online: http://books.google.com (accessed on 2 December 2024).
- Lederberg, A.R.; Schick, B.; Spencer, P.E. Language and Literacy Development of Deaf and Hard-of-Hearing Children: Successes and Challenges. Dev. Psychol. 2013, 49, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.; Terlektsi, E.; Kyle, F.E. Literacy outcomes for Deaf and Hard of Hearing primary school children: A cohort comparison study. J. Speech Lang. Hear. Res. 2017, 60, 701–711. [Google Scholar] [CrossRef]
- Yanbay, E.; Hickson, L.; Scarinci, N.; Constantinescu, G.; Dettman, S.J. Language outcomes for children with cochlear implants enrolled in different communication programs. Cochlear Implant. Int. 2014, 15, 121–135. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Deafness and Hearing Loss; Who.int; World Health Organization (WHO): Geneva, Switzerland, 2024; Available online: https://www.who.int/health-topics/hearing-loss#tab=tab_1 (accessed on 21 December 2024).
- Swanepoel, D.W.; Johl, L.; Pienaar, D. Childhood hearing loss and risk profile in a South African population. Int. J. Pediatr. Otorhinolaryngol. 2013, 77, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.E.; Swanepoel, D.W.; Le Roux, T. National survey of paediatric audiological services for diagnosis and intervention in the South African private health care sector. S. Afr. J. Commun. Disord. 2014, 61, 8. [Google Scholar] [CrossRef]
- Baltussen, R.; Smith, A. Cost effectiveness of strategies to combat vision and hearing loss in sub-Saharan Africa and South East Asia: Mathematical modelling study. BMJ 2012, 344, e615. [Google Scholar] [CrossRef]
- Mdladlo, T.; Flack, P.; Joubert, R. Are South African Speech-Language Therapists adequately equipped to assess English Additional Language (EAL) speakers who are from an indigenous linguistic and cultural background? A profile and exploration of the current situation. S. Afr. J. Commun. Disord. 2016, 63, 2225–4765. [Google Scholar] [CrossRef]
- Health Professions Council of South Africa. Guidelines for Practice in a Culturally and Linguistically Diverse South Africa 2019 1 Professional Board for Speech, Language and Hearing Professions Guidelines for Practice in a Culturally and Linguistically Diverse South Africa. 2019. Available online: https://www.hpcsa.co.za/Uploads/SLH/Guidelines%20for%20practice%20in%20a%20culturally%20and%20linguistically%20divers---.pdf (accessed on 2 December 2024).
- Fulcher, A.; Purcell, A.A.; Baker, E.; Munro, N. Listen up: Children with early identified hearing loss achieve age-appropriate speech/language outcomes by 3years-of-age. Int. J. Pediatr. Otorhinolaryngol. 2012, 76, 1785–1794. [Google Scholar] [CrossRef]
- Goldblat, E.; Pinto, O.Y. Academic outcomes of adolescents and young adults with hearing loss who received auditory-verbal therapy. Deaf. Educ. Int. 2017, 19, 126–133. [Google Scholar] [CrossRef]
- Hoffman, M.F.; Quittner, A.L.; Cejas, I. Comparisons of Social Competence in Young Children With and Without Hearing Loss: A Dynamic Systems Framework. J. Deaf Stud. Deaf Educ. 2014, 20, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Kaczmarek, L. Assessment of Social-Communicative Competence: An Interdisciplinary Model. In Promoting Social Communication: Children with Developmental Disabilities from Birth to Adolescence; Goldstein, H., Kaczmarek, L., English, K., Eds.; Paul H. Brookes Publishing Company: Baltimore, MD, USA, 2002; pp. 55–115. [Google Scholar]
- Statistics South Africa. General Household Survey. [Online]. 2016. Available online: www.statssa.gov.za (accessed on 25 December 2024).
| Characteristic | Category | Overall | TSLT | LSL-SA | p-Value for Between-Group Comparison | |||
|---|---|---|---|---|---|---|---|---|
| n | % | N | % | N | % | |||
| N | 126 | 64 | 62 | |||||
| Age | Median (IQR); range | 8.3 (6.0–10.1); 1.7–16.7 | 8.7 (6.5–10.2); 1.7–16.7 | 6.8 (5.6–10.0); 1.7–11.7 | 0.092 | |||
| Gender | Male | 54 | 43 | 29 | 45 | 25 | 40 | 0.59 |
| Female | 72 | 57 | 35 | 55 | 37 | 60 | ||
| Race Group | Colored | 53 | 42 | 29 | 45 | 23 | 37 | 0.61 |
| White | 41 | 33 | 19 | 30 | 22 | 35 | ||
| Black | 23 | 18 | 13 | 20 | 10 | 16 | ||
| Indian | 7 | 6 | 2 | 3 | 5 | 8 | ||
| Other | 3 | 2 | 1 | 2 | 2 | 3 | ||
| Home Language | English | 58 | 46 | 27 | 42 | 31 | 50 | 0.84 |
| Afrikaans | 39 | 31 | 21 | 33 | 18 | 29 | ||
| Xhosa | 17 | 13 | 4 | 6 | 10 | 16 | ||
| English and Afrikaans | 5 | 4 | 10 | 16 | 7 | 11 | ||
| Zulu | 4 | 3 | 2 | 3 | 3 | 5 | ||
| Southern Sotho | 1 | 1 | 0 | 0 | 1 | 2 | ||
| Other | 2 | 2 | 1 | 2 | 1 | 2 | ||
| Type of Amplification | Hearing Aid | 37 | 29 | 23 | 36 | 14 | 23 | 0.12 |
| Cochlear Implant | 89 | 71 | 41 | 64 | 48 | 77 | ||
| Number of Cochlear Implants | 0 | 36 | 29 | 22 | 34 | 14 | 23 | 0.26 |
| 1 | 39 | 31 | 20 | 31 | 19 | 31 | ||
| 2 | 51 | 40 | 22 | 34 | 29 | 47 | ||
| Communication Domains | TSLT | LSL-SA | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Communication Functioning at the Onset of Therapy | Communication Functioning at Discharge of Therapy | Communication Functioning at the Onset of Therapy | Communication Functioning at Discharge of Therapy | |||||||||
| % Delayed | % Age Appropriate | % Unknown | % Delayed n | % Age Appropriate | % Unknown | % Delayed | % Age Appropriate | % Unknown | % Delayed | % Age Appropriate | % Unknown | |
| Speech intelligibility | 97% (n = 62) | 2% (n = 1) | 1% (n = 1) | 55% (n = 35) | 45% (n = 29) | 1% (n = 1) | 97% (n = 60) | 3% (n = 2) | 32% (n = 20) | 66% (n = 41) | ||
| Vocabulary | 98% (n = 63) | 2% (n = 1) | 61% (n = 39) | 39% (n = 25) | 97% (n = 60) | 3% (n = 2) | 39% (n = 24) | 61% (n = 38) | ||||
| Receptive Language | 98% (n = 63) | 2% (n = 1) | 61% (n = 39) | 39% (n = 25) | 97% (n = 60) | 3% (n = 2) | 37% (n = 23) | 61% (n = 38) | ||||
| Expressive Language | 98% (n = 63) | 2% (n = 1) | 61% (n = 39) | 39% (n = 25) | 97% (n = 60) | 3% (n = 2) | 44% (n = 27) | 56% (n = 35) | ||||
| Audition | 98% (n = 63) | 2% (n = 1) | 56% (n = 36) | 44% (n = 28) | 98% (n = 63) | 2% (n = 1) | 32% (n = 20) | 68% (n = 42) | ||||
| Cognitive Linguistics | 98% (n = 63) | 2% (n = 1) | 52% (n = 33) | 48% (n = 31) | 90% (n = 56) | 8% n = 5) | 1% (n = 1) | 27% (n = 17) | 73% (n = 45) | |||
| N | 126 | 64 | 62 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall | TSLT | LSL-SA | Unadjusted | Adjusted | |||||
| Communication Outcomes Trajectory (Onset to Discharge): | N | % | n | % | n | % | Odds Ratio (OR) for LSL vs. TSLT (95% CI) | ||
| Speech | Delayed—Delayed | 54 | 43 | 34 | 53 | 20 | 32 | 0.42 (0.20–0.86) | 0.46 (0.21–1.02) |
| Delayed—Age-Appropriate | 67 | 53 | 28 | 44 | 39 | 63 | reference | ||
| Age Appropriate—Age Appropriate | 3 | 2 | 1 | 2 | 2 | 3 | |||
| Unknown | 2 | 2 | |||||||
| Vocabulary | Delayed—Delayed | 62 | 49 | 38 | 59 | 24 | 39 | 0.41 (0.20–0.83) | 0.48 (0.21–1.07) |
| Age Appropriate—Delayed | 1 | 1 | 1 | 2 | |||||
| Delayed—Age-Appropriate | 61 | 48 | 25 | 39 | 36 | 58 | reference | ||
| Age Appropriate—Age Appropriate | 2 | 2 | 2 | 3 | |||||
| Receptive Language | Delayed—Delayed | 61 | 48 | 38 | 59 | 23 | 37 | 0.38 (0.18–0.78) | 0.43 (0.19–0.99) |
| Age Appropriate—Delayed | 1 | 1 | 1 | 2 | |||||
| Delayed—Age-Appropriate | 62 | 49 | 25 | 39 | 37 | 60 | reference | ||
| Age Appropriate—Age Appropriate | 2 | 2 | 2 | 3 | |||||
| Expressive Language | Delayed—Delayed | 65 | 52 | 38 | 59 | 27 | 44 | 0.50 (0.24–1.01) | 0.61 (0.28–1.33) |
| Age Appropriate—Delayed | 1 | 1 | 1 | 2 | |||||
| Delayed—Age-Appropriate | 58 | 46 | 25 | 39 | 33 | 53 | reference | ||
| Age Appropriate—Age Appropriate | 2 | 2 | 2 | 3 | |||||
| Audition | Delayed—Delayed | 55 | 44 | 35 | 55 | 20 | 32 | 0.37 (0.18–0.77) | 0.42 (0.19–0.92) |
| Age Appropriate—Delayed | 1 | 1 | 1 | 2 | |||||
| Delayed—Age-Appropriate | 69 | 55 | 28 | 44 | 41 | 66 | reference | ||
| Age Appropriate—Age Appropriate | 1 | 1 | 1 | 2 | |||||
| Cognitive Linguistics | Delayed—Delayed | 49 | 39 | 33 | 52 | 16 | 26 | 0.33 (0.16–0.71) | 0.39 (0.17–0.88) |
| Delayed—Age-Appropriate | 70 | 56 | 30 | 47 | 40 | 65 | reference | ||
| Age Appropriate—Age Appropriate | 6 | 5 | 1 | 2 | 5 | 8 | |||
| Unknown | 1 | 1 | |||||||
| Characteristic | Category | Overall | TSLT | LSL-SA | p-Value for Between-Group Comparison | |||
|---|---|---|---|---|---|---|---|---|
| N | % | n | % | n | % | |||
| N | 126 | 64 | 62 | |||||
| Identification and Diagnosis of Hearing Loss | ||||||||
| Age of identification of hearing loss (years) | median (IQR); range | 1.5 (0.5–2.5); 0.0–8.1 | 1.7 (0.7–2.5); 0.0–7.7 | 1.0 (0.3–2.3); 0.0–8.1 | 0.047 | |||
| Duration from identification to diagnosis (months) | median (IQR); range | 0.0 (0.0–7.0); 0.0–58.0 | 0.0 (0.0–6.5); 0.0–37.0 | 0.5 (0.0–7.0); 0.0–58.0 | 0.19 | |||
| Age at diagnosis of hearing loss (years) | median (IQR); range | 1.8 (0.8–3.0); 0.0–8.1 | 2.1 (1.2–3.0); 0.1–7.7 | 1.5 (0.5–3.0); 0.0–8.1 | 0.095 | |||
| Hearing Amplification | ||||||||
| Duration from diagnosis to amplification (months) | median (IQR); range | 1.0 (0.0–3.0); 0.0–61.0 | 1.0 (0.0–4.0); 0.0–61.0 | 0.0 (0.0–2.0); 0.0–13.9 | 0.075 | |||
| Earliest age of amplification (years) | median (IQR); range | 2.1 (1.0–3.1); 0.1–8.2 | 2.3 (1.7–3.3); 0.1–8.2 | 1.8 (0.6–3.0); 0.2–8.2 | 0.037 | |||
| Age of amplification with CI (years) | (n) median (IQR); range | (n = 90) 3.1 (1.9–4.9); 0.2–11.8 | (n = 42) 3.5 (2.3–5.0); 0.2–11.8 | (n = 48) 2.7 (1.8–4.9); 0.5–8.7 | 0.16 | |||
| Age at the start of Communication Intervention (years) | median (IQR); range | 2.5 (1.5–3.6); 0.2–8.3 | 2.5 (1.6–3.5); 0.3–8.3 | 2.5 (1.4–3.9); 0.2–8.2 | 0.86 | |||
| Type of hearing amplification device | Hearing Aid | 37 | 29 | 23 | 36 | 14 | 23 | 0.12 |
| Cochlear Implant | 89 | 71 | 41 | 64 | 48 | 77 | ||
| Communication Intervention | ||||||||
| Duration from diagnosis to Communication Intervention (months) | median (IQR); range | 2.7 (1.0–7.0); 0.0–67.2 | 2.7 (0.7–6.3); 0.0–53.6 | 2.9 (1.2–11.9); 0.0–67.2 | 0.40 | |||
| Duration of Communication Intervention (years) | median (IQR); range | 4.6 (3.0–6.8); 0.5–13.6 | 5.5 (3.4–7.3); 0.5–13.6 | 4.2 (2.9–6.3); 1.0–10.9 | 0.071 | |||
| Hearing Age until discharge from Communication Intervention | median (IQR); range | 4.1 (2.6–6.0); 0.1–24.0 | 4.4 (2.4–6.5); 0.7–24.0 | 4.0 (2.7–5.4); 0.1–10.7 | 0.61 | |||
| Language of Communication Intervention | ||||||||
| The language used in sessions | English | 89 | 71 | 43 | 67 | 46 | 74 | 0.44 |
| Afrikaans | 37 | 29 | 21 | 33 | 16 | 26 | ||
| Language used during communication intervention sessions | Same | 100 | 79 | 50 | 78 | 50 | 81 | 0.83 |
| Different | 26 | 21 | 14 | 22 | 12 | 19 | ||
| Characteristic | Overall | TSLT | LSL-SA | p-Value for Between-Group Comparisons | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | N | % | n | % | |||
| Aided Audiogram Results Available | No | 60 | 48 | 20 | 31 | 40 | 65 | 0.0003 |
| Yes | 66 | 52 | 44 | 69 | 22 | 35 | ||
| % fail (25dB cutoff): Ear R | 250 Hz (n = 54) | 28 | 29 | 26 | >0.99 | |||
| 500 Hz (n = 58) | 40 | 40 | 40 | >0.99 | ||||
| 1000 Hz (n = 58) | 43 | 42 | 45 | >0.99 | ||||
| 2000 Hz (n = 56) | 55 | 58 | 50 | 0.77 | ||||
| 4000 Hz (n = 49) | 63 | 71 | 43 | 0.10 | ||||
| 8000 Hz (n = 7) | ||||||||
| Low frequencies (250–1000 Hz) (n = 58) | 48 | 45 | 55 | 0.58 | ||||
| High frequencies (2000–4000 Hz) (n = 56) | 68 | 74 | 56 | 0.23 | ||||
| % fail (25dB cutoff): Ear L | 250 Hz (n = 54) | 30 | 31 | 28 | >0.99 | |||
| 500 Hz (n = 56) | 43 | 46 | 37 | 0.58 | ||||
| 1000 Hz (n = 56) | 41 | 38 | 47 | 0.57 | ||||
| 2000 Hz (n = 55) | 45 | 49 | 39 | 0.57 | ||||
| 4000 Hz (n = 49) | 49 | 56 | 33 | 0.22 | ||||
| 8000 Hz (n = 5) | ||||||||
| Low frequencies (250–1000 Hz) (n = 56) | 50 | 51 | 47 | >0.99 | ||||
| High frequencies (2000–4000 Hz) (n = 55) | 60 | 65 | 50 | 0.38 | ||||
| Odds Ratios are for Delay vs. Age Appropriate | Speech | Vocabulary | Receptive Language | Expressive Language | Audition | Cognitive Linguistics | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Delayed | Age Appropriate | OR (95% CI) | Delayed | Age Appropriate | OR (95% CI) | Delayed | Age Appropriate | OR (95% CI) | Delayed | Age Appropriate | OR (95% CI) | Delayed | Age Appropriate | OR (95% CI) | Delayed | Age Appropriate | OR (95% CI) | ||
| Duration from ID to diagnosis (m) | median (IQR) | 0.0 (0.0–11.0) | 0.0 (0.0–3.0) | 1.04 (1.01–1.08) | 0.0 (0.0–9.0) | 0.0 (0.0–3.0) | 1.03 (0.99–1.07) | 0.0 (0.0–9.0) | 0.0 (0.0–3.0) | 1.04 (0.99–1.08) | 0.0 (0.0–8.0) | 0.0 (0.0–3.0) | 1.03 (0.99–1.07) | 0.0 (0.0–8.0) | 0.0 (0.0–6.0) | 1.01 (0.98–1.05) | 0.0 (0.0–8.0) | 0.0 (0.0–6.0) | 1.01 (0.98–1.05) |
| Duration from ID to EI (m) | median (IQR) | 8.2 (2.6–22.7) | 6.0 (2.6–19.2) | 1.02 (0.99–1.04) | 7.4 (2.7–18.3) | 6.9 (2.5–26.3) | 1.00 (0.98–1.03) | 7.2 (2.7–16.9) | 7.2 (2.5–26.9) | 1.00 (0.97–1.02) | 7.8 (2.8–18.3) | 6.5 (2.4–23.8) | 1.00 (0.98–1.03) | 6.9 (2.6–14.4) | 7.5 (2.6–27.6) | 0.99 (0.96–1.02) | 7.8 (2.6–18.3) | 6.6 (2.7–23.8) | 1.00 (0.97–1.03) |
| Duration from identification to amplification (m) | median (IQR); range | 6.0 (1.0–15.0) | 2.0 (0.0–8.5) | 1.03 (0.99–1.07) | 6.0 (1.0–18.0) | 2.0 (0.0–8.0) | 1.04 (0.99–1.07) | 6.0 (1.0–18.0) | 2.0 (0.0–7.6) | 1.04 (0.99–1.07) | 6.0 (1.0–15.0) | 2.0 (0.0–8.3) | 1.03 (0.98–1.07) | 6.0 (1.1–12.5) | 2.0 (0.0–9.0) | 1.01 (0.98–1.05) | 6.0 (1.1–12.0) | 3.0 (0.0–9.0) | 1.01 (0.98–1.05) |
| Duration of Amplification (y) | median (IQR); range | 3.4 (1.8–5.4) | 4.9 (3.5–6.4) | 0.73 (0.59–0.89) | 3.9 (2.3–5.7) | 4.7 (3.4–6.3) | 0.86 (0.72–1.01) | 3.9 (2.3–5.7) | 4.7 (3.3–6.2) | 0.88 (0.74–1.04) | 3.9 (2.3–5.7) | 4.8 (3.4–6.3) | 0.86 (0.72–1.02) | 3.8 (2.3–5.5) | 4.7 (3.2–6.3) | 0.85 (0.71–1.02) | 3.4 (1.8–5.4) | 4.8 (3.4–6.3) | 0.76 (0.62–0.93) |
| Audiogram (% fail) | Ear A—low frequencies (n = 58) | 63 | 38 | 3.03 (0.96–9.53) | 63 | 38 | 3.10 (0.96–10.0) | 61 | 40 | 2.79 (0.84–9.22) | 63 | 38 | 3.10 (0.96–10.0) | 60 | 42 | 2.50 (0.71–8.85) | 72 | 38 | 6.14 (1.48–25.4) |
| Ear A—high frequencies (n = 56) | 83 | 58 | 2.67 (0.71–10.1) | 87 | 55 | 4.11 (0.97–17.5) | 86 | 56 | 3.49 (0.81–15.1) | 87 | 55 | 4.11 (0.97–17.5) | 90 | 56 | 5.08 (0.95–27.1) | 94 | 55 | 10.3 (1.19–89) | |
| Ear B—low frequencies (n = 56) | 67 | 38 | 3.31 (1.06–10.4) | 67 | 38 | 3.49 (1.05–11.6) | 65 | 39 | 3.08 (0.90–10.5) | 67 | 38 | 3.49 (1.05–11.6) | 63 | 43 | 2.52 (0.68–9.38) | 71 | 41 | 3.83 (1.01–14.6) | |
| Ear B—high frequencies (n = 56) | 75 | 48 | 2.69 (0.78–9.32) | 78 | 47 | 2.57 (0.69–9.52) | 77 | 48 | 2.07 (0.54–7.92) | 78 | 47 | 2.57 (0.69–9.52) | 79 | 50 | 2.09 (0.50–8.71) | 88 | 47 | 6.22 (1.16–33) | |
| Number of cochlear implants (column %) | 0 | 34 | 23 | reference | 41 | 16 | reference | 42 | 16 | reference | 41 | 15 | reference | 46 | 14 | reference | 46 | 17 | reference |
| 1 | 31 | 31 | 0.73 (0.28–1.92) | 37 | 25 | 0.58 (0.22–1.58) | 35 | 27 | 0.53 (0.20–1.42) | 35 | 27 | 0.50 (0.19–1.36) | 36 | 27 | 0.43 (0.16–1.14) | 42 | 24 | 0.71 (0.27–1.45) | |
| 2 | 34 | 47 | 0.14 (0.05–0.38) | 22 | 59 | 0.16 (0.06–0.41) | 23 | 58 | 0.16 (0.06–0.42) | 24 | 58 | 0.16 (0.06–0.42) | 18 | 59 | 0.10 (0.04–0.28) | 12 | 59 | 0.37 (0.16–0.86) | |
| Age at start of EI (y) | median (IQR); range | 3.0 (2.1–4.3) | 2.3 (1.0–3.3) | 1.49 (1.15–1.92) | 2.9 (2.1–4.2) | 2.1 (0.9–3.1) | 1.52 (1.16–1.99) | 2.9 (2.1–4.2) | 2.2 (0.9–3.1) | 1.52 (1.16–1.99) | 2.8 (2.1–4.1) | 2.1 (0.9–3.2) | 1.47 (1.13–1.90) | 2.9 (1.9–4.3) | 2.3 (1.0–3.3) | 1.38 (1.07–1.78) | 3.0 (2.1–4.5) | 2.3 (1.0–3.2) | 1.50 (1.16–1.96) |
| Earliest age of amplification (y) | median (IQR); range | 2.8 (1.8–4.0) | 1.8 (0.6–2.6) | 1.65 (1.24–2.21) | 2.8 (2.0–4.0) | 1.4 (0.4–2.4) | 2.07 (1.47–2.92) | 2.8 (2.0–4.0) | 1.4 (0.5–2.4) | 2.18 (1.53–3.11) | 2.6 (1.8–4.0) | 1.5 (0.4–2.5) | 1.88 (1.35–2.60) | 2.8 (2.0–4.0) | 1.6 (0.6–2.6) | 1.75 (1.27–2.39) | 2.9 (2.0–4.2) | 1.8 (0.6–2.6) | 1.74 (1.28–2.37) |
| Earliest age of amplification with CI (y) (n = 90) | median (IQR); range | 4.0 (3.0–5.7) | 2.5 (1.6–4.2) | 1.34 (1.07–1.68) | 3.6 (2.5–5.2) | 2.7 (1.6–4.3) | 1.19 (0.97–1.46) | 3.6 (2.5–5.1) | 2.8 (1.6–4.5) | 1.17 (0.95–1.43) | 3.6 (2.3–5.2) | 2.8 (1.6–4.5) | 1.15 (0.95–1.40) | 3.6 (2.5–5.3) | 2.8 (1.7–4.7) | 1.15 (0.94–1.41) | 4.3 (3.0–5.3) | 2.7 (1.7–4.3) | 1.23 (0.99–1.52) |
| Earliest age of amplification vs. Age at start of EI(cutoffs 2.1y and 2.5y respectively | Early / Early | 36 | 59 | reference | 41 | 57 | reference | 42 | 56 | reference | 42 | 57 | reference | 41 | 56 | reference | 36 | 58 | reference |
| Early / Late | 5 | 16 | 0.83 (0.20–3.47) | 3 | 19 | 0.33 (0.07–1.70) | 2 | 20 | 0.16 (0.02–1.3) | 5 | 18 | 0.46 (0.11–1.90) | 2 | 19 | 0.20 (0.02–1.75) | 4 | 16 | 0.68 (0.13–3.59) | |
| Late / Late | 58 | 26 | 3.38 (1.49–7.66) | 56 | 24 | 2.97 (1.30–6.75) | 56 | 23 | 2.97 (1.30–6.78) | 53 | 25 | 2.55 (1.13–5.78) | 57 | 26 | 2.75 (1.20–6.62) | 60 | 26 | 3.42 (1.48–7.94) | |
| Duration of EI (y) | median (IQR); range | 4.1 (2.4–6.8) | 5.4 (3.8–7.3) | 0.81 (0.68–0.95) | 4.1 (2.9–6.8) | 5.4 (3.6–7.4) | 0.80 (0.68–0.94) | 4.2 (2.9–6.8) | 5.4 (3.6–7.3) | 0.81 (0.68–0.95) | 4.1 (2.9–6.6) | 5.5 (3.8–7.4) | 0.79 (0.67–0.93) | 4.1 (2.8–6.7) | 5.4 (3.7–7.3) | 0.77 (0.65–0.91) | 3.7 (2.8–6.1) | 5.5 (3.8–7.3) | 0.72 (0.60–0.87) |
| SLT Language match to home language | Same | 67 | 89 | reference | 67 | 92 | reference | 66 | 92 | reference | 67 | 93 | reference | 61 | 94 | reference | 62 | 91 | reference |
| Different | 33 | 11 | 3.55 (1.34–9.41) | 33 | 8 | 5.69 (1.88–17.2) | 34 | 8 | 6.06 (1.98–18.5) | 33 | 7 | 6.74 (2.08–21.9) | 39 | 6 | 12.3 (3.57–42.6) | 38 | 9 | 6.28 (2.20–17.9) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casoojee, A.; Khoza-Shangase, K.; Kanji, A. Communication Outcomes of Children with Hearing Loss: A Comparison of Two Early Intervention Approaches. Audiol. Res. 2025, 15, 27. https://doi.org/10.3390/audiolres15020027
Casoojee A, Khoza-Shangase K, Kanji A. Communication Outcomes of Children with Hearing Loss: A Comparison of Two Early Intervention Approaches. Audiology Research. 2025; 15(2):27. https://doi.org/10.3390/audiolres15020027
Chicago/Turabian StyleCasoojee, Aisha, Katijah Khoza-Shangase, and Amisha Kanji. 2025. "Communication Outcomes of Children with Hearing Loss: A Comparison of Two Early Intervention Approaches" Audiology Research 15, no. 2: 27. https://doi.org/10.3390/audiolres15020027
APA StyleCasoojee, A., Khoza-Shangase, K., & Kanji, A. (2025). Communication Outcomes of Children with Hearing Loss: A Comparison of Two Early Intervention Approaches. Audiology Research, 15(2), 27. https://doi.org/10.3390/audiolres15020027






