Do Patients Aged 85 Years and above Benefit from Their Cochlear Implants?
Abstract
1. Introduction
2. Materials and Methods
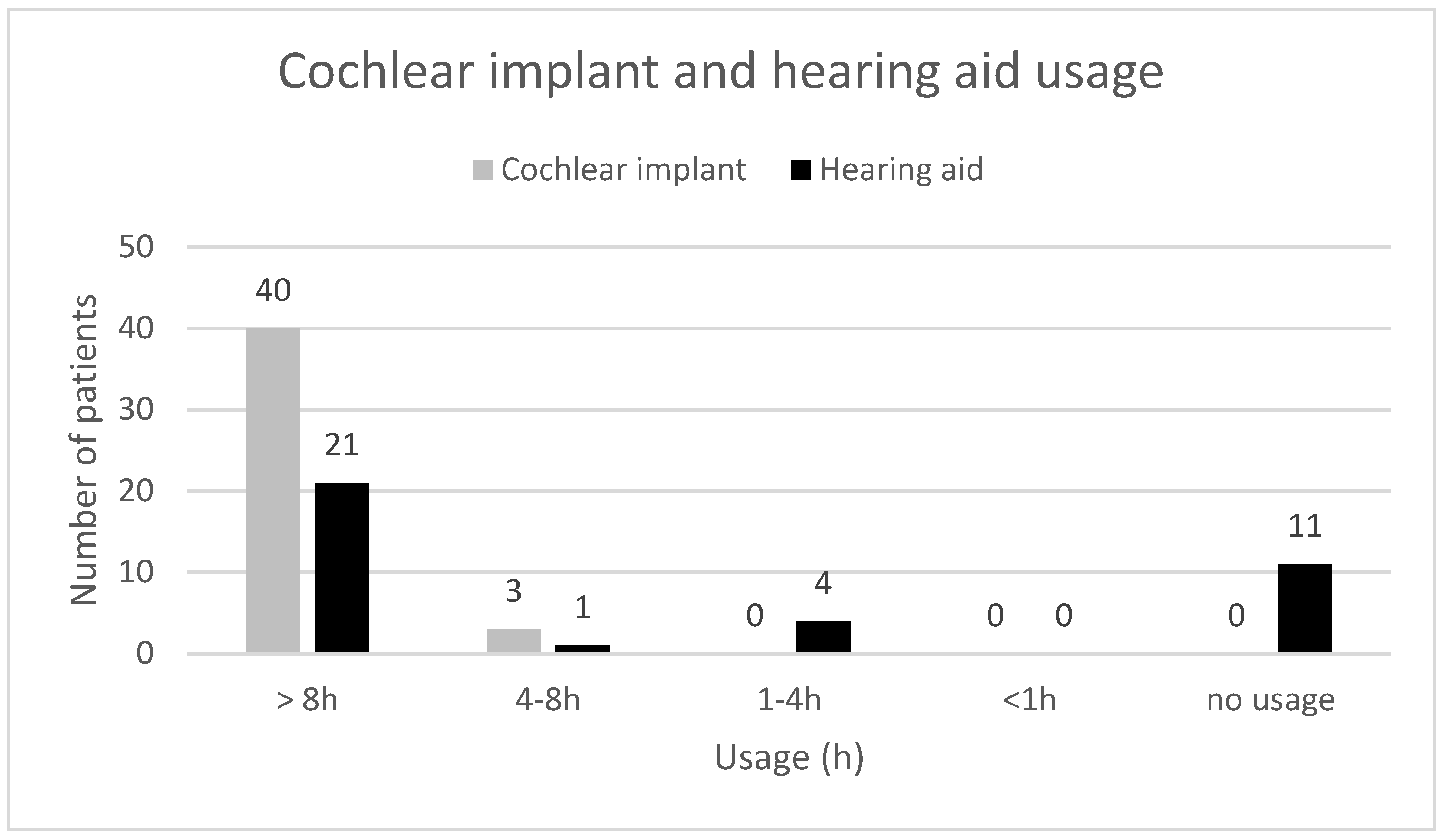
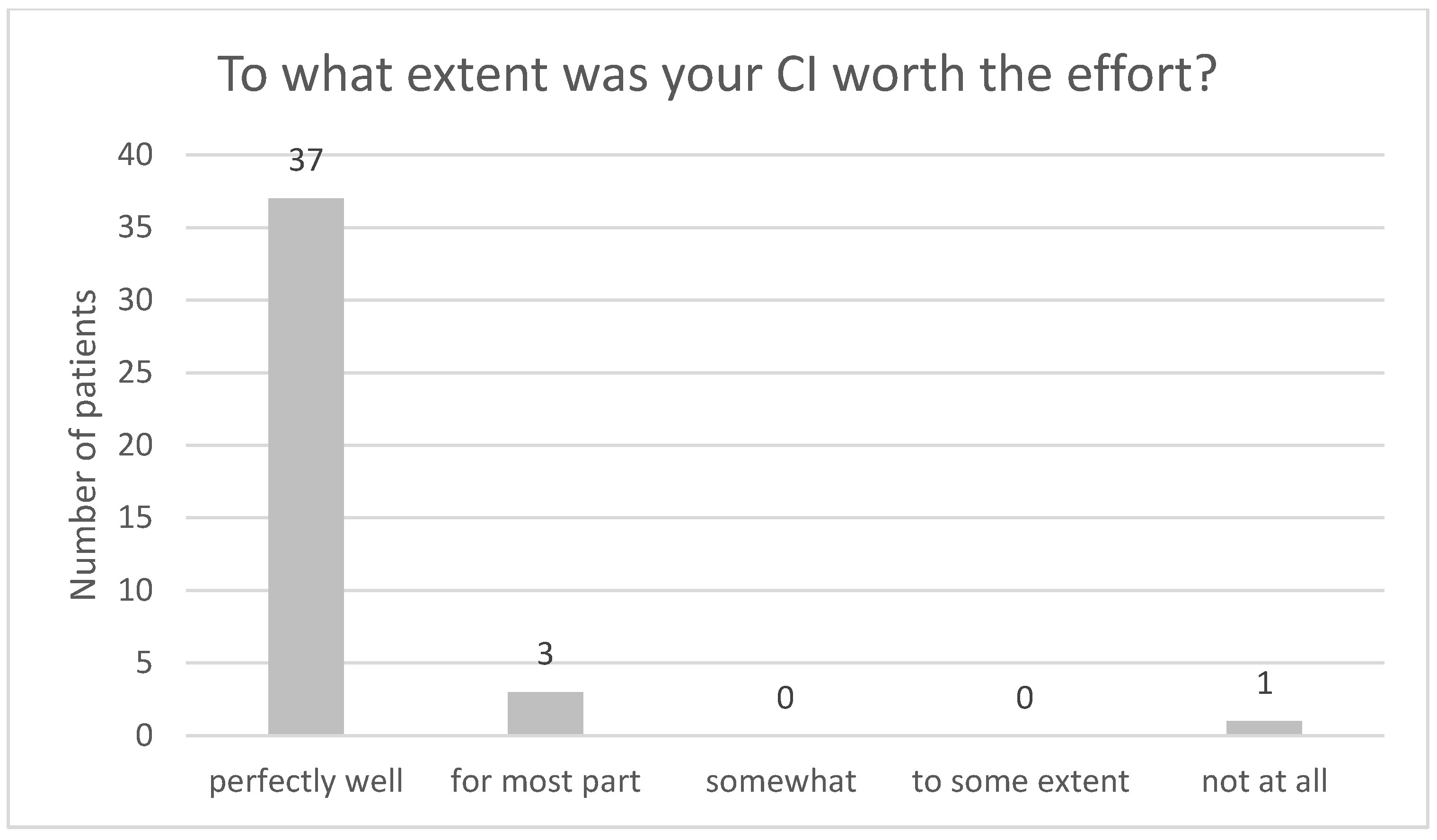
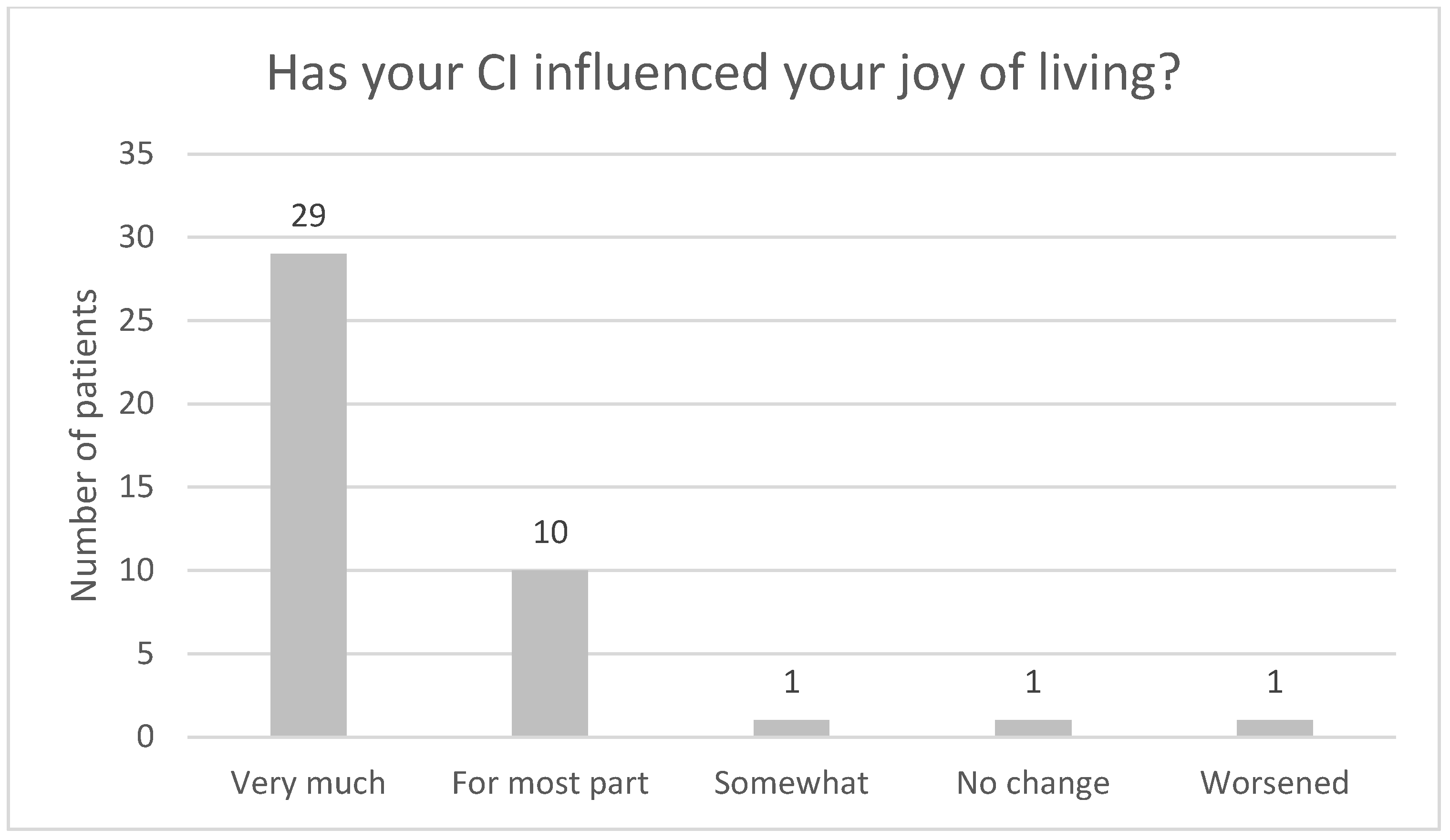
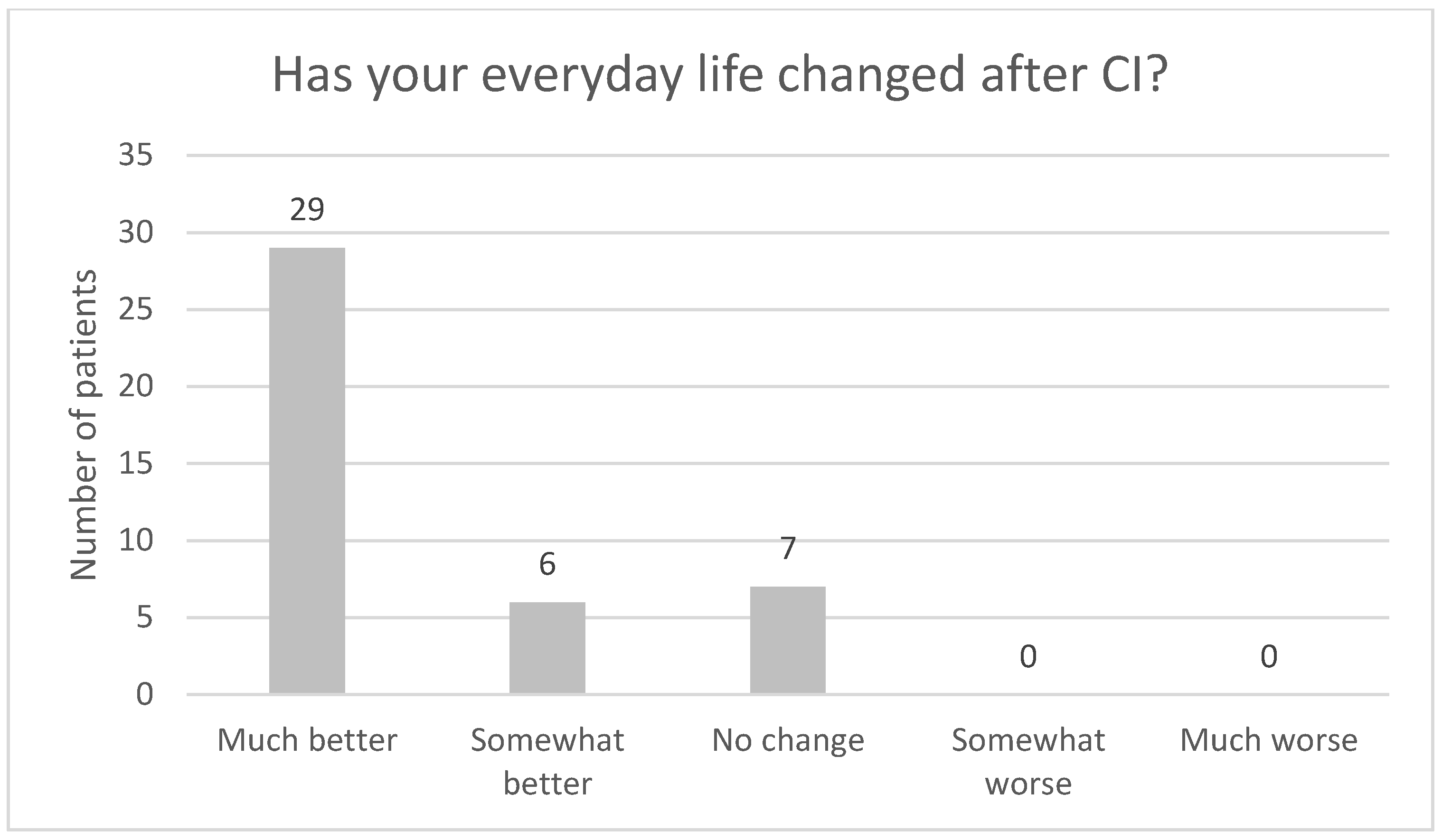
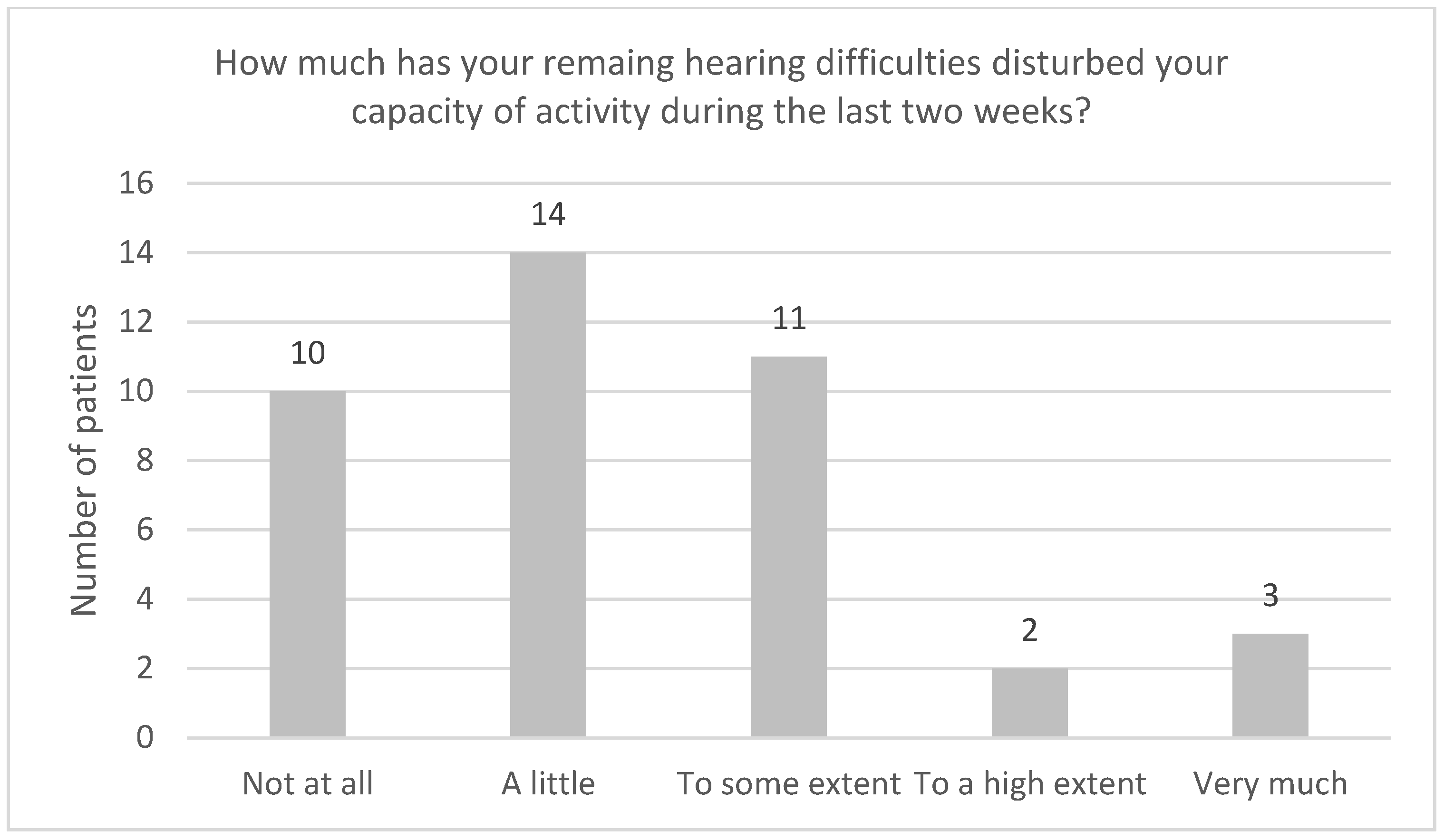
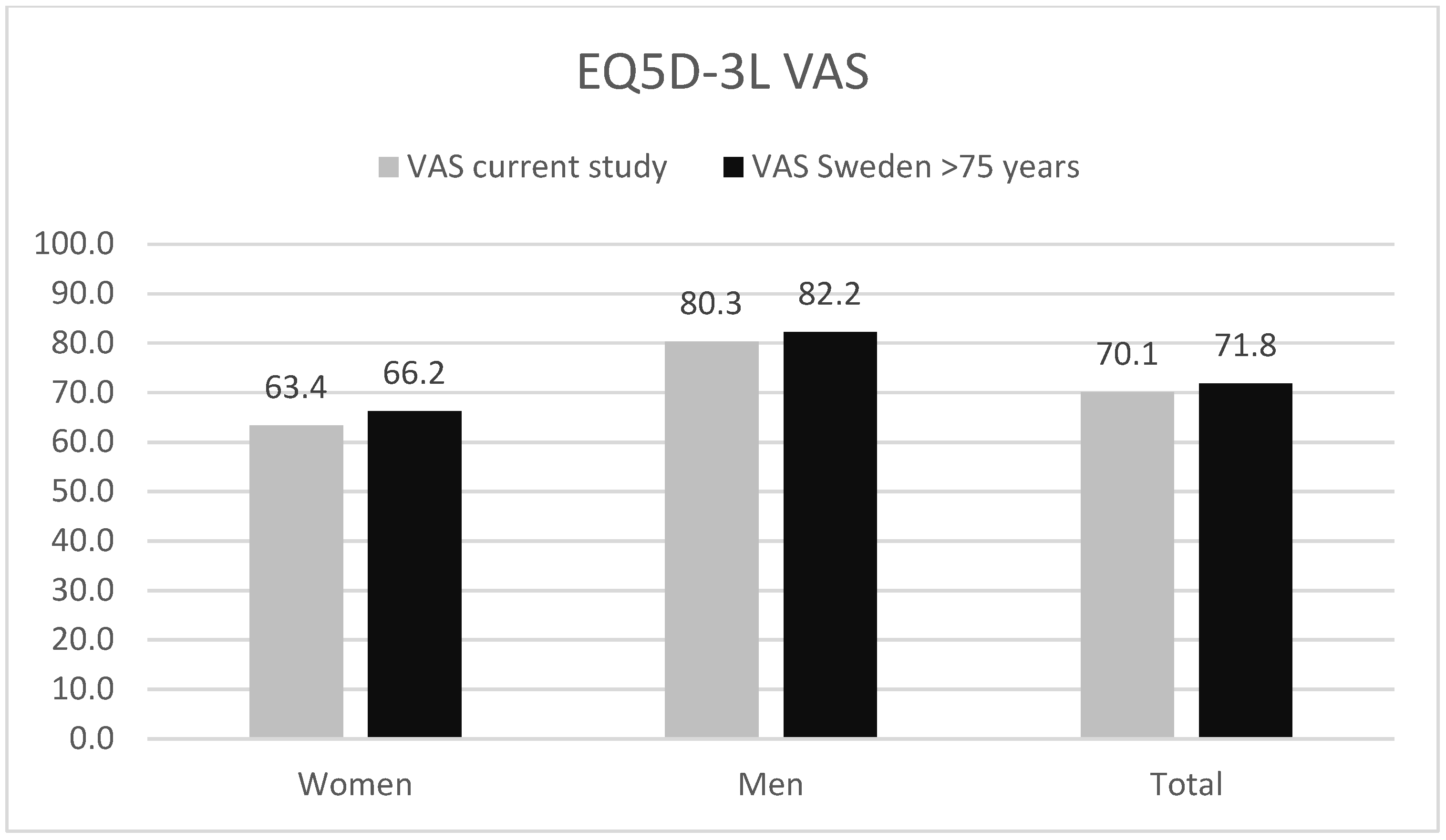
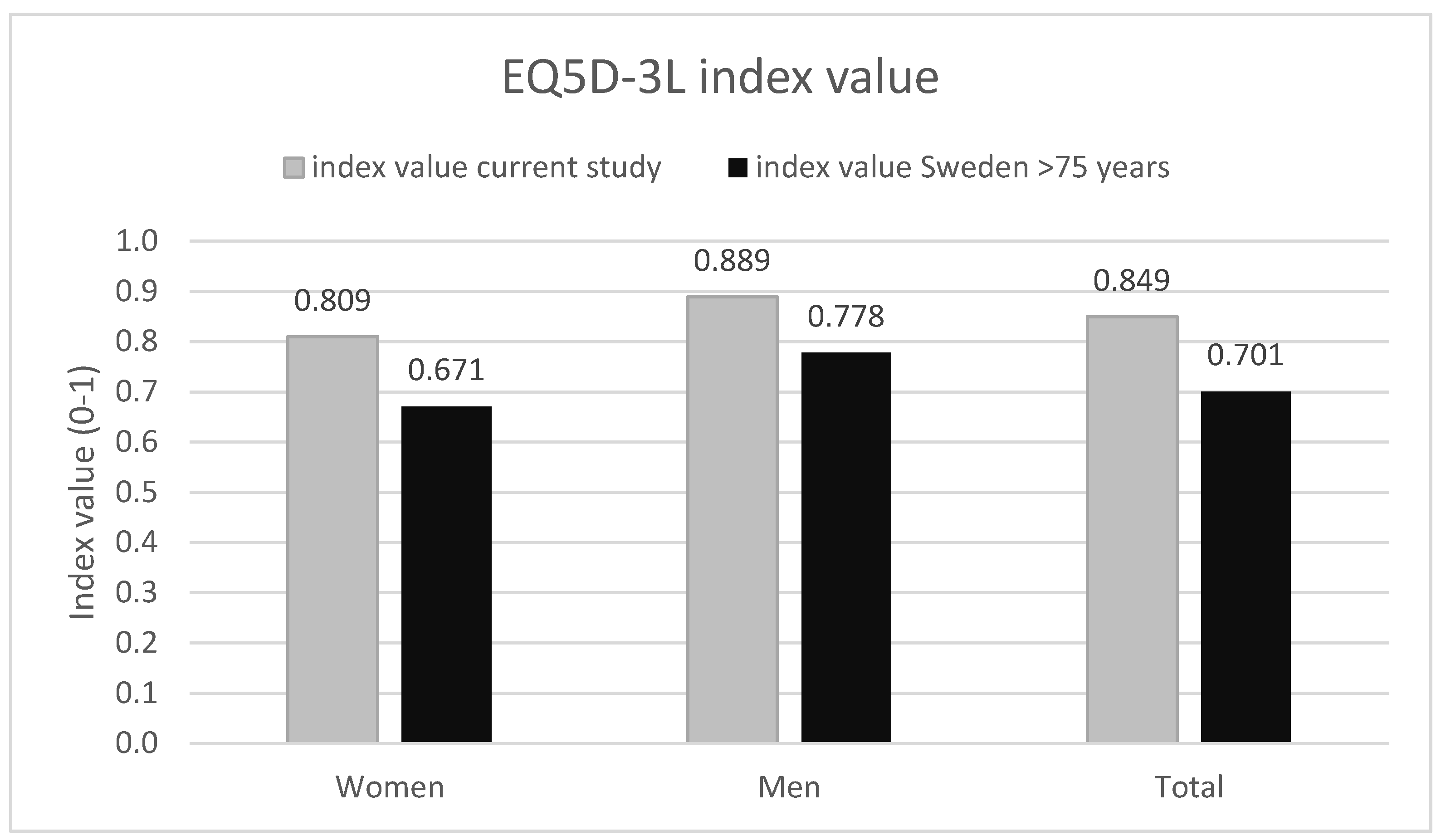
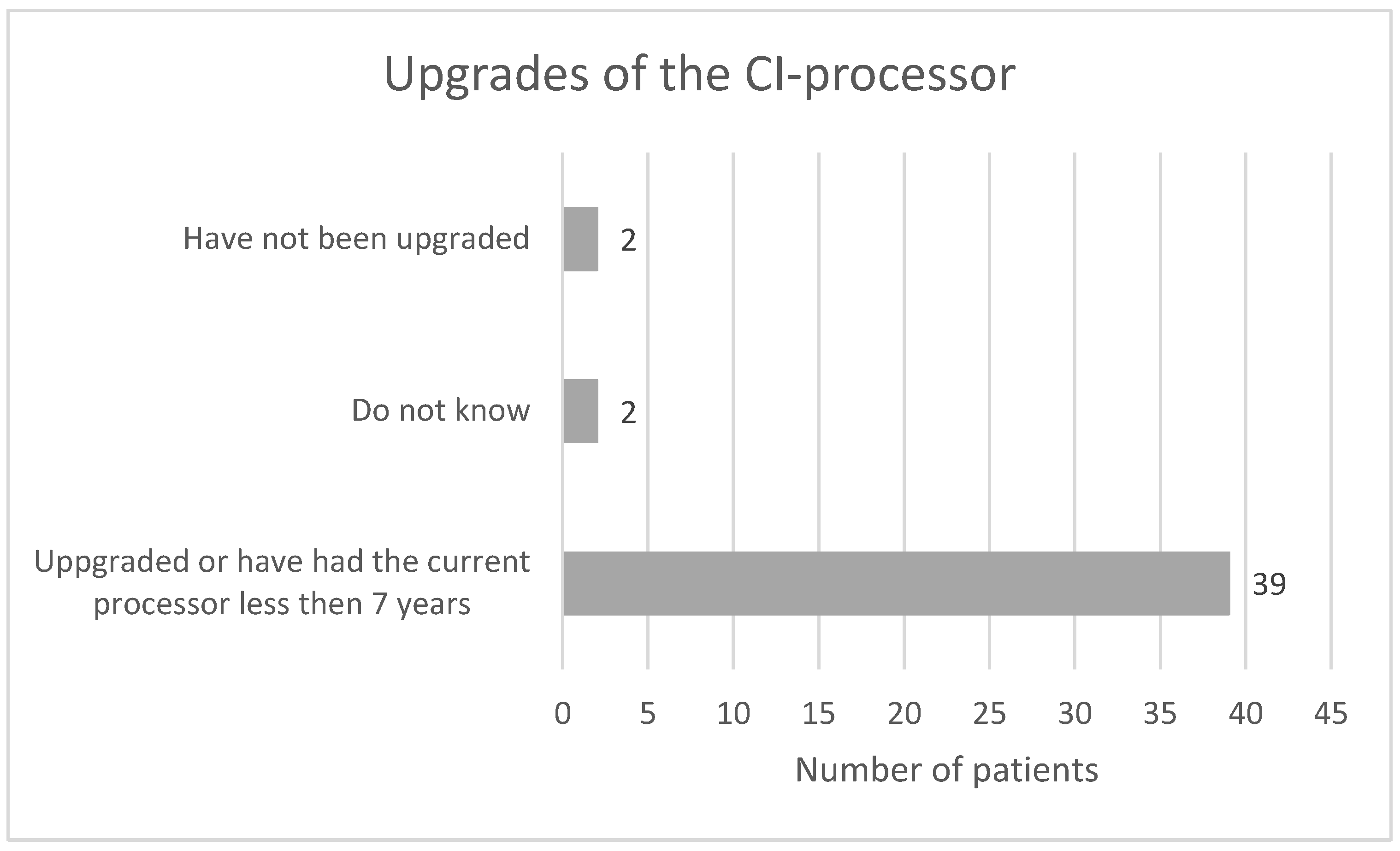
3. Results


4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Babajanian, E.E.; Patel, N.S.; Gurgel, R.K. The impact of Cochlear Implantation: Cognitive Function, Quality of Life, and Frailty in Older Adults. Semin. Hear. 2021, 42, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Löfvenberg, C.; Turunen-Taheri, S.; Carlsson, P.-I.; Skagerstrand, Å. Rehabilitation of Severe-to-Profound Hearing Loss in Adults in Sweden. Audiol. Res. 2022, 12, 443–444. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Lin, F.R.; Metter, E.J.; O’Brien, R.J.; Resnick, S.M.; Zonderman, A.B.; Ferrucci, L. Hearing loss and incident dementia. Arch Neurotol. 2011, 68, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Thomson, R.S.; Auduong, P.; Miller, A.T.; Gurgel, R.K. Hearing loss as a risk factor for dementia: A systematic review. Laryngoscope Investig. Otolaryngol. 2017, 2, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Gurgel, R.K.; Ward, P.D.; Schwartz, S.; Norton, M.; Foster, N.L.; Tschanz, J.T. Relationship of hearing loss and dementia: A prospective, population-based study. Otol. Neurotol. 2014, 35, 775–781. [Google Scholar] [CrossRef]
- Amieva, H.; Ouvrard, C.; Meillon, C.; Rullier, L.; Dartigues, J.F. Death, depression, disability, and dementia associated with self-reported hearing problems: A 25-year study. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 1383–1389. [Google Scholar] [CrossRef]
- Ray, J.; Popli, G.; Fell, G. Association of cognition and age-related hearing impairment in the English longitudinal study of ageing. JAMA Otolaryngol. Head Neck Surg. 2018, 144, 876–882. [Google Scholar] [CrossRef]
- Maharani, A.; Dawes, P.; Nazroo, J.; Tampubolon, G.; Pendleton, N. Longitudinal relationship between hearing aid use and cognitive function in older Americans. J. Am. Geriatr Soc. 2018, 66, 1130–1136. [Google Scholar] [CrossRef]
- Budenz, C.L.; Cosetti, M.K.; Coelho, D.H.; Birenbaum, B.; Babb, J.; Waltzman, S.B.; Roehm, P.C. The effects of cochlear implantation on speech perception in older adults. J. Am. Geriatr. Soc. 2011, 59, 446–453. [Google Scholar] [CrossRef]
- Lundin, K.; Näsvall, A.; Köbler, S.; Linde, G.; Rask-Andersen, H. Cochlear implantation in the elderly. Cochlear Implant. Int. 2013, 14, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Sonnet, M.-H.; Montaut-Verient, B.; Niemier, J.-Y.; Hoen, M.; Ribeyre, L.; Parietti-Winkler, C. Cognitive Abilities and Quality of Life After Cochlear Implant in the Elderly. Otol. Neurotol. 2017, 38, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Marx, M.; Mosnier, I.; Belmin, J.; Wyss, J.; Coudert-Koall, C.; Manrique Huarte, R.; Khnifes, R.; Hilly, O.; Martini, A.; Cudo, D. Healthy aging in elderly cochlear implant recipients: A multinational observational study. BMC Geriatr. 2020, 20, 252. [Google Scholar] [CrossRef] [PubMed]
- Oyanguren, V.; Goffi Gomes, M.V.; Tsuji, R.-K.; Bento, R.F.; Neto, R.B. Auditory results from cochlear implants in elderly people. Braz. J. Otorhinolaryngol. 2010, 76, 450–453. [Google Scholar] [CrossRef]
- Burström, K.; Sun, S.; Gerdtham, U.G.; Henriksson, M.; Johannesson, M.; Levin, L.Å.; Zethraeus, N. Swedish experience-based value sets for EQ-5D health states. Qual. Life Res. 2014, 23, 431–432. [Google Scholar] [CrossRef]
- EQ5D. Available online: https.euroqol.org (accessed on 14 April 2022).
- Swedish Quality Register of Otorhinolaryngology. Available online: http://www.registercentrum.se/ (accessed on 3 November 2022).
- Björk, S.; Norinder, A. The weighting exercise for the Swedish version of the EuroQol. Health Econ. 1999, 8, 117–126. [Google Scholar] [CrossRef]
- Said de Angelo, T.C.; Moret, A.L.M.; Alves da Costa, O.; Nascimento, L.T.; de Freitas Alvarenga, K. Quality of life in adult cochlear implant users. CoDAS 2016, 28, 106–112. [Google Scholar] [CrossRef]
- Hilly, O.; Ehwang, E.; Smith, L.; Shipp, D.; Nedzelski, J.M.; Chen, J.M.; Lin, V.W.Y. Cochlear implantation in elderly patients: Stability of outcome over time. J. Laryngol. Otol. 2016, 130, 706–711. [Google Scholar] [CrossRef]
- Saraça, E.T.; Batukb, M.O.; Sennaroglub, G. Evaluation of the quality of life in adults with cochlear implants: As good as the healthy adults? Am. J. Otolaryngol. 2019, 40, 720–723. [Google Scholar] [CrossRef]
- Imagawa, N.E.; Hirota, E.; Morino, T.; Kojima, H. Factors related to the satisfaction level of elderly hearing-impaired individuals with cochlear implants. Auris Nasus Larynx 2020, 47, 793–799. [Google Scholar] [CrossRef]
- Nationellt Kliniskt Kunskapsstöd. Personcentrerat Och Sammanhållet Vårdförlopp Grav Hörselnedsättning. Available online: https://nationelltklinisktkunskapsstod.se/vardprogramochvardforlopp (accessed on 17 October 2022).
- Rohloff, K.; Koopmann, M.; Weiß, D.; Rudack, C.; Savvas, E. Cochlear Implantation in the Elderly: Does Age Matter? Otol. Neurotol. 2016, 38, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Raymond, M.J.; Dong, A.; Naissir, S.B.; Vivas, E.X. Postoperative Healthcare Utilization of Elderly Adults After Cochlear Implantation. Otol. Neurotol. 2020, 41, 2008–2013. [Google Scholar] [CrossRef]
- Dietz, A.; Wüstefeld, M.; Niskanen, M.; Löppönen, H. Cochlear Implant Surgery in the Elderly: The Feasibility of a Modified Suprameatal Approach Under Local Anesthesia. Otol. Neurotol. 2016, 37, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Kecskeméti, N.; Szőnyi, M.; Küstel, M.; Gáborján, A.; Tamás, L.; Répássy, G. Cochlear implantation under local anesthesia: A possible alternative for elderly patients. Eur. Arch Otorhinolaryngol. 2019, 276, 1643–1647. [Google Scholar] [CrossRef] [PubMed]
- Luger, T.J.; Kammerlander, C.; Luger, M.F.; Kammerlander-Knauer, U.; Gosch, M.Z. Gerontol Geriatr Mode of anesthesia, mortality and outcome in geriatric patients. Z Gerontol. Geriatr. 2014, 47, 110–124. [Google Scholar] [CrossRef]
- Fakurnejad, S.; Vail, D.; Song, Y.; Alyono, J.; Blevins, N.H. Trends in Age of Cochlear Implant Recipients, and the Impact on Perioperative Complication Rates. Otol. Neurotol. 2020, 41, 438–443. [Google Scholar] [CrossRef]
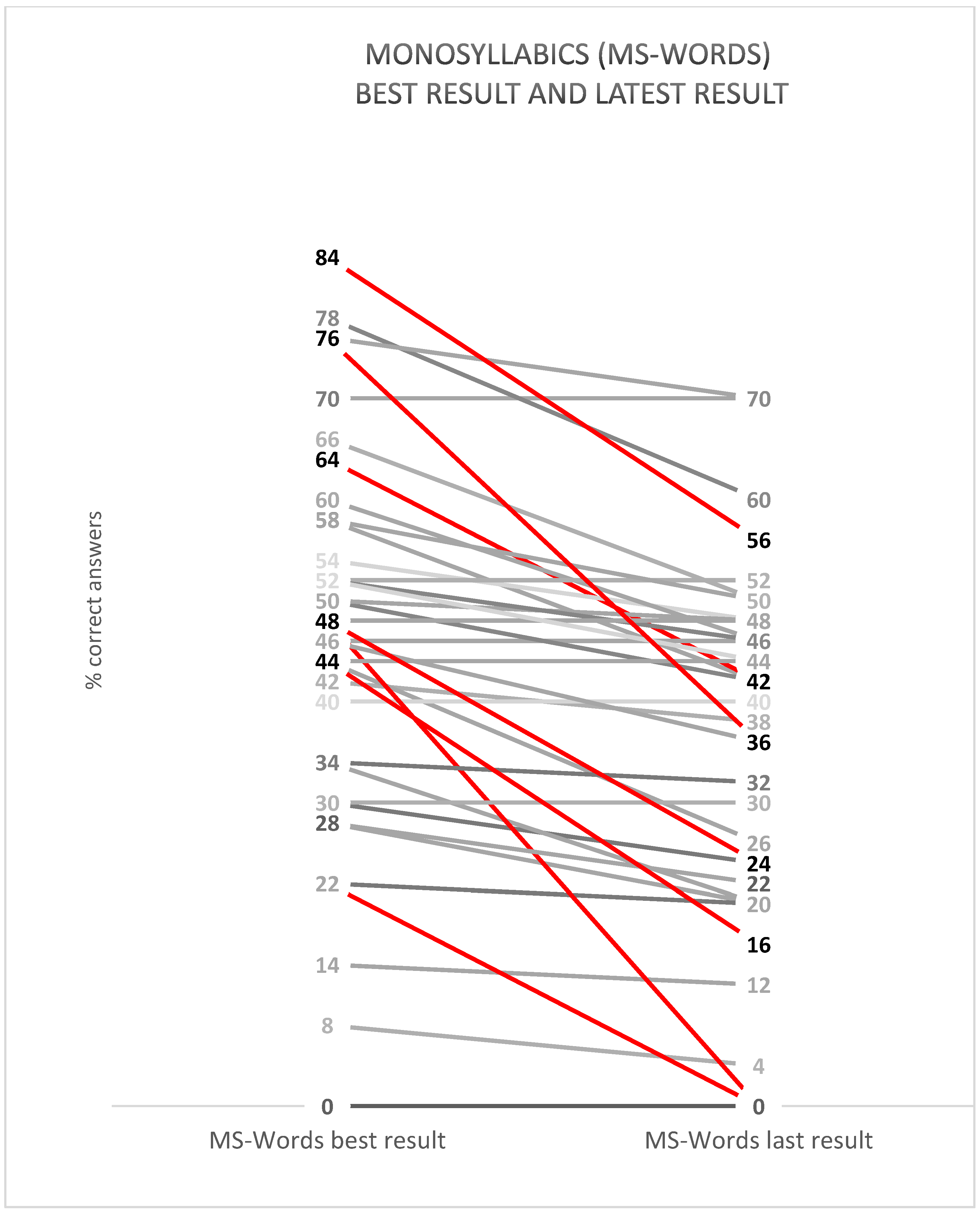
| Patient | MS Best (%) | MS Latest (%) | Change (Percentage Points) | Usage/Dag (h) | EQ5D VAS | Index Value | Age | Sex | Comment |
|---|---|---|---|---|---|---|---|---|---|
| Q3 | 64 | 42 | −22 | >8 h | 80 | 0.9349 | 85 | W | |
| Q19 | 22 | 0 | −22 | 4–8 h | 70 | 0.7139 | 88 | W | Reported “I cannot handle my usual activities” on EQ-5D. Other health-related issues than hearing difficulties. |
| Q29 | 48 | 0 | −48 | >8 h | 90 | 0.9694 | 90 | W | |
| Q38 | 84 | 56 | −28 | >8 h | 70 | 0.9694 | 97 | M | Even after a significant decline in results, these results are better than average for adults at our clinic. |
| Q40 | 48 | 24 | −24 | >8 h | 72 | NA | 88 | W | The patient has been upgraded since the last MS word test. The best MS word score is measured on a higher presentation level than the latest measure. |
| Q41 | 44 | 16 | −28 | >8 h | NA | NA | 96 | M | The patient lives at a nursing home. Vision impaired. Isolated. |
| Q42 | 76 | 36 | −40 | >8 h | 80 | 0.9349 | 85 | M |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hallin, K.; Larsson, U.; Schart-Morén, N. Do Patients Aged 85 Years and above Benefit from Their Cochlear Implants? Audiol. Res. 2023, 13, 96-106. https://doi.org/10.3390/audiolres13010010
Hallin K, Larsson U, Schart-Morén N. Do Patients Aged 85 Years and above Benefit from Their Cochlear Implants? Audiology Research. 2023; 13(1):96-106. https://doi.org/10.3390/audiolres13010010
Chicago/Turabian StyleHallin, Karin, Ulrika Larsson, and Nadine Schart-Morén. 2023. "Do Patients Aged 85 Years and above Benefit from Their Cochlear Implants?" Audiology Research 13, no. 1: 96-106. https://doi.org/10.3390/audiolres13010010
APA StyleHallin, K., Larsson, U., & Schart-Morén, N. (2023). Do Patients Aged 85 Years and above Benefit from Their Cochlear Implants? Audiology Research, 13(1), 96-106. https://doi.org/10.3390/audiolres13010010






