An Evaluation of the Caudal End Deviation of the Nasal Septum Using the Quantitative Analysis of Computed Tomography
Abstract
:1. Introduction
2. Material and Methods
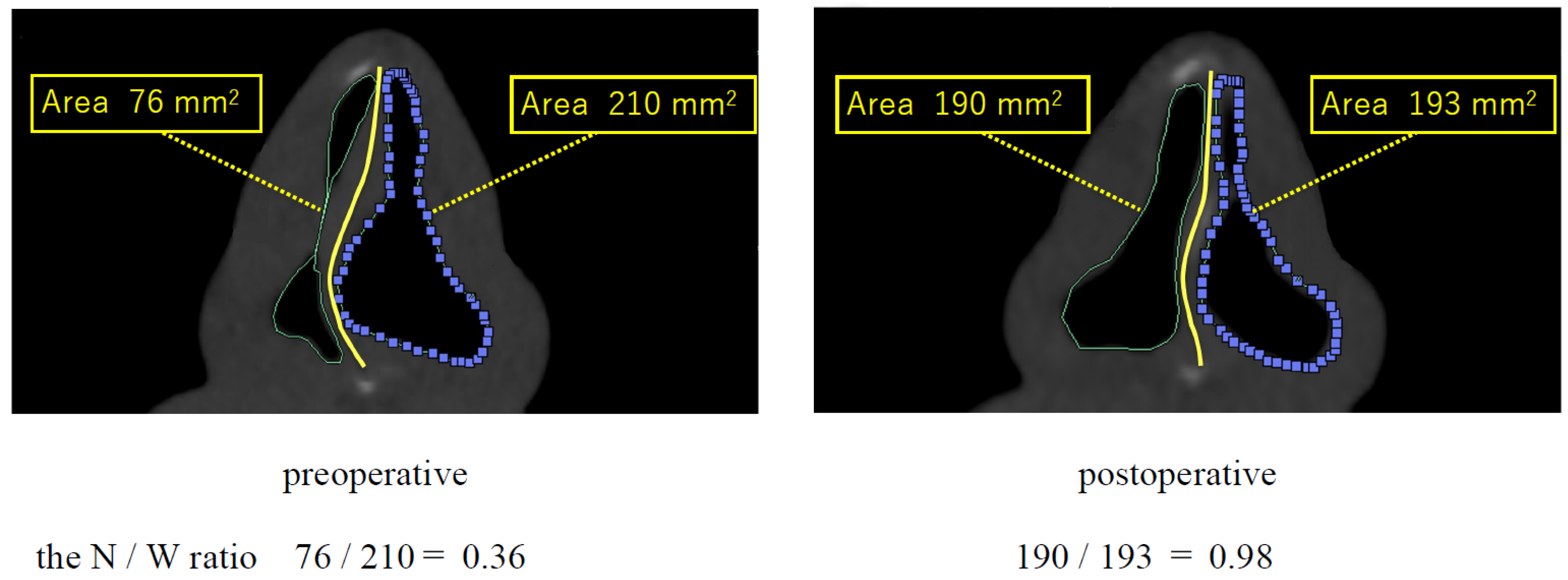
2.1. CT Analysis
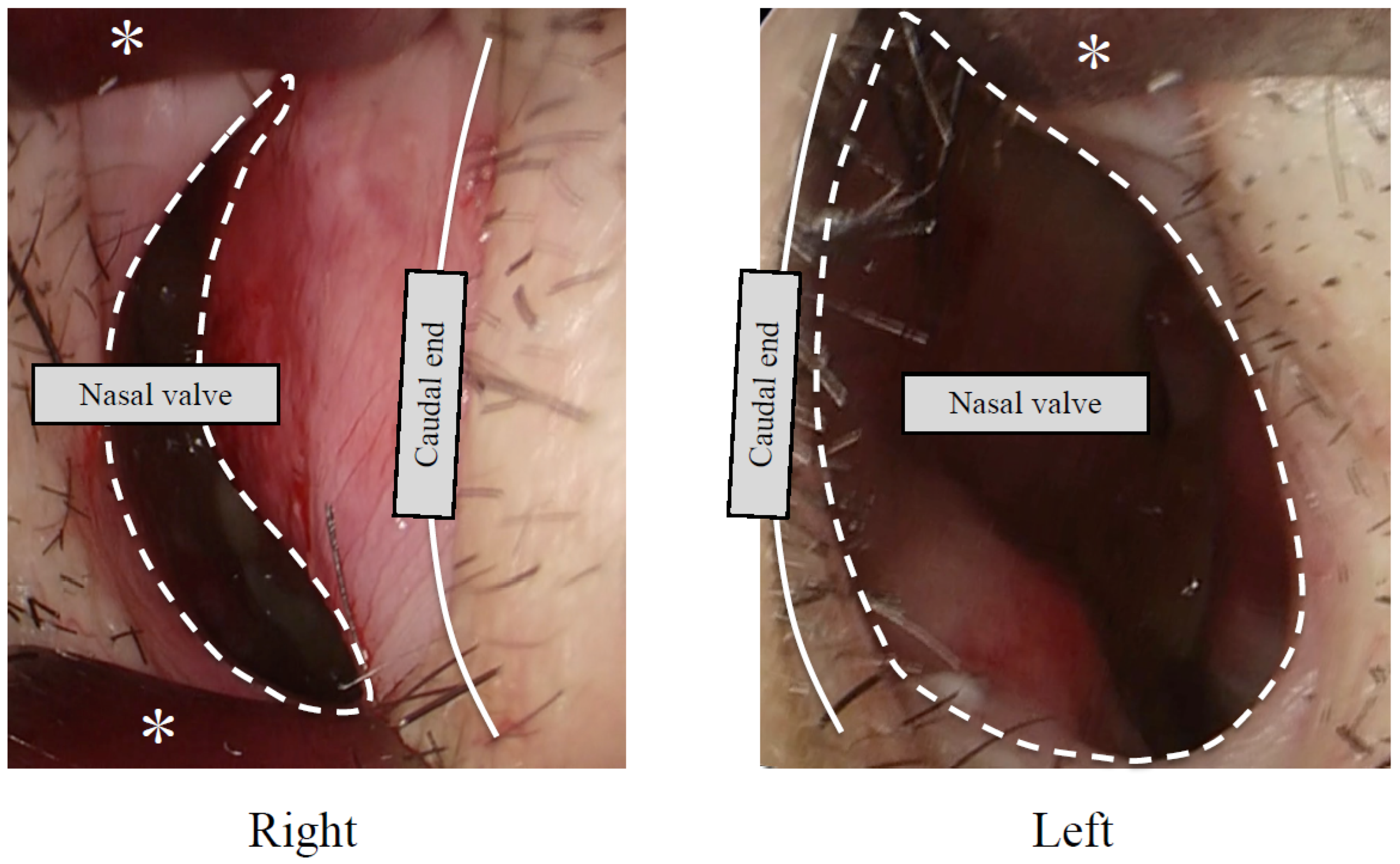
2.2. Patients
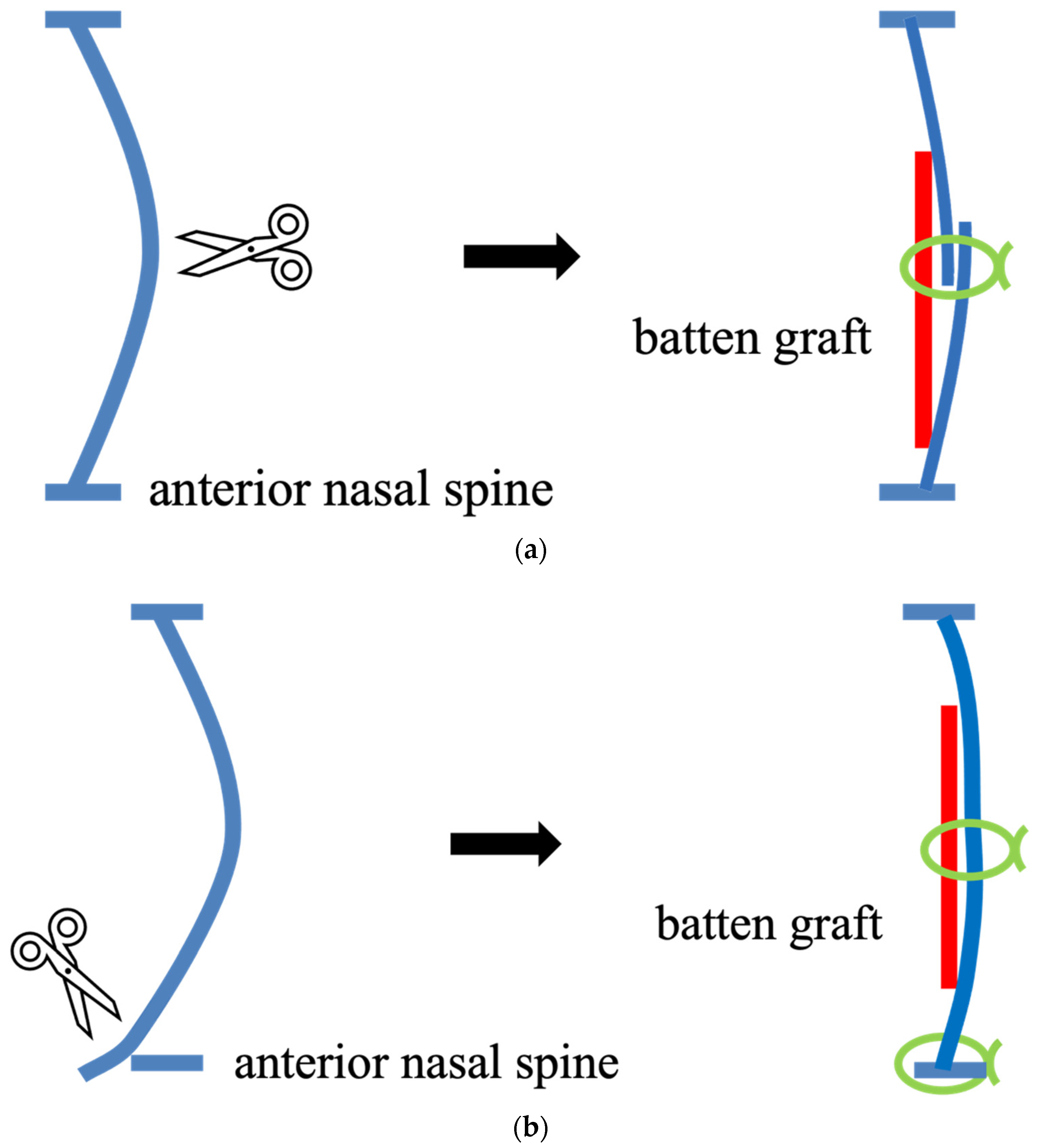
- A.
- For the cases where the inferior part of the curved caudal end was not dislocated from the anterior nasal spine, cutting and suturing techniques [6] were performed. The caudal strut was cut using scissors at the convex-most region in the caudocephalic direction. The excess portions of the upper and lower caudal strut were then overlapped, and the overlapping cartilages were sutured together. They were reinforced with a batten graft.
- B.
- For the cases where the inferior part of the caudal end was dislocated from anterior the nasal spine, the excess cartilage was resected and the lower edge of the cartilage was fixed to the anterior nasal spine. They were reinforced with a batten graft.
3. Results
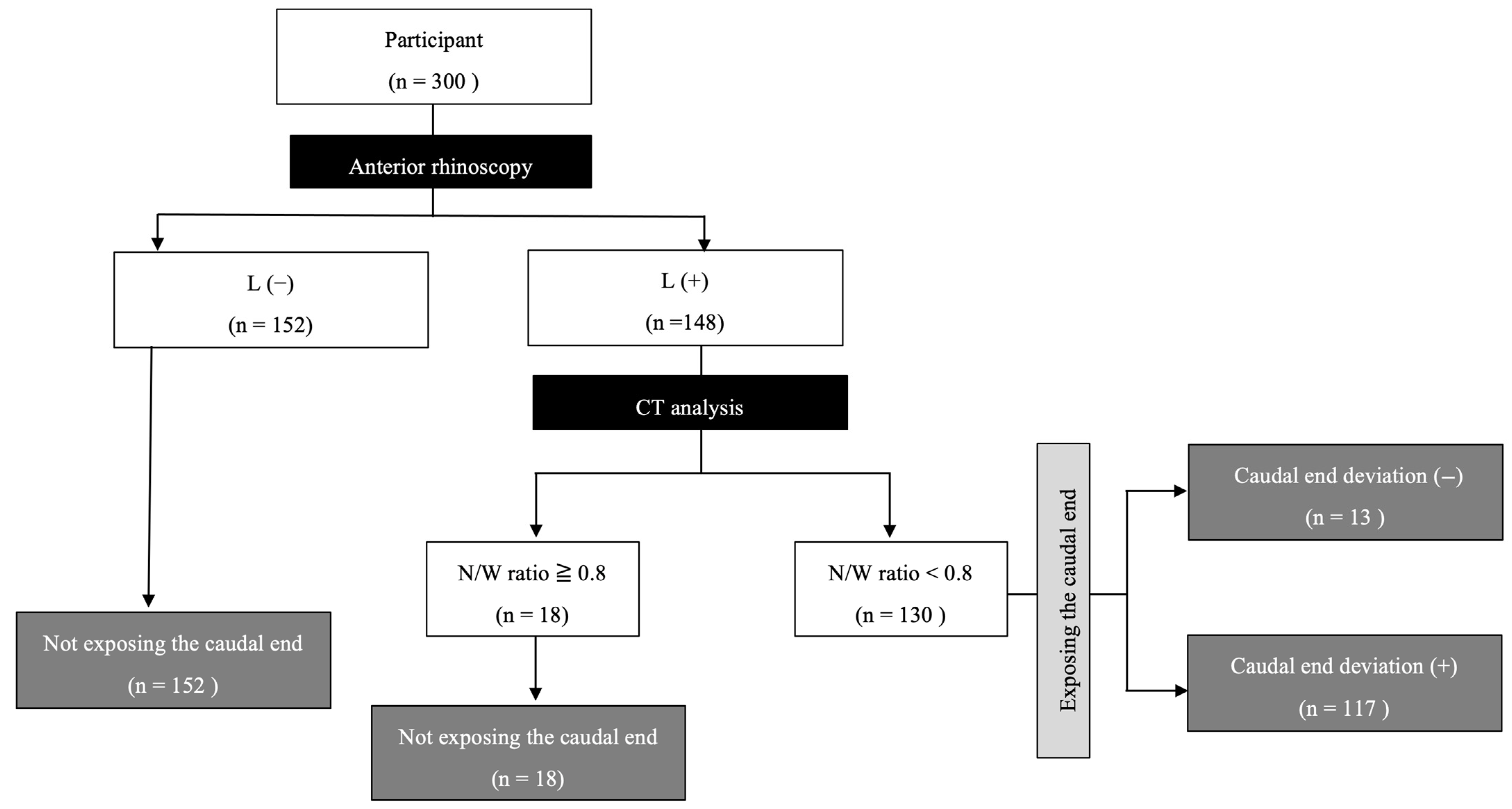
3.1. Participant Division
3.2. The Relationship between the AR Findings and the N/W Ratio
3.3. Correcting Effect
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hsu, D.W.; Suh, J.D. Anatomy and Physiology of Nasal Obstruction. Otolaryngol. Clin. N. Am. 2018, 51, 853–865. [Google Scholar] [CrossRef] [PubMed]
- Shafik, A.G.; Alkady, H.A.; Tawfik, G.M.; Mohamed, A.M.; Rabie, T.M.; Huy, N.T. Computed tomography evaluation of internal nasal valve angle and area and its correlation with NOSE scale for symptomatic improvement in rhinoplasty. Braz. J. Otorhinolaryngol. 2020, 86, 343–350. [Google Scholar] [CrossRef]
- Haight, J.S.J.; Cole, P. The site and function of the nasal valve. Laryngoscope 1983, 93, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Nigro, C.E.N.; Nigro, J.F.d.A.; Mion, O.; Mello, J.F. Nasal Valve: Anatomy and physiology. Braz. J. Otorhinolaryngol. 2009, 75, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Tasca, I.; Compadretti, C.; Sorace, F. Nasal valve surgery. Acta Otorhinolaryngol. Ital. 2013, 33, 196–201. [Google Scholar] [PubMed]
- Jang, Y.J.; Yeo, N.-K.; Wang, J.H. Cutting and Suture Technique of the Caudal Septal Cartilage for the Management of Caudal Septal Deviation. Arch. Otolaryngol. Head Neck Surg. 2009, 135, 1256–1260. [Google Scholar] [CrossRef]
- Slavit, D.H.; Bansberg, S.F.; Facer, G.W.; Kern, E.B. Reconstruction of Caudal End of Septum: A Case for Transplantation. Arch. Otolaryngol. Neck Surg. 1995, 121, 1091–1098. [Google Scholar] [CrossRef]
- Chmielik, L.P.; Mielnik-Niedzielska, G.; Kasprzyk, A.; Stankiewicz, T.; Niedzielski, A. An Evaluation of Health-Related Quality of Life in Children with Nasal Septum Deviation. Children 2022, 9, 1714. [Google Scholar] [CrossRef]
- Aziz, T.; Biron, V.L.; Ansari, K.; Flores-Mir, C. Measurement tools for the diagnosis of nasal septal deviation: A systematic review. J. Otolaryngol. Head Neck Surg. 2014, 43, 11. [Google Scholar] [CrossRef]
- Nakayama, T.; Okushi, T.; Yamakawa, S.; Kuboki, A.; Haruna, S.-I. Endoscopic single-handed septoplasty with batten graft for caudal septum deviation. Auris Nasus Larynx 2014, 41, 441–445. [Google Scholar] [CrossRef]
- Iimura, J.; Miyawaki, T.; Kikuchi, S.; Tsumiyama, S.; Mori, E.; Nakajima, T.; Kojima, H.; Otori, N. A new “J septoplasty” technique for correction of mild caudal septal deviation. Auris Nasus Larynx 2020, 47, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Elkenawy, I.; Fijany, L.; Colak, O.; Paredes, N.A.; Gargoum, A.; Abedini, S.; Cantarella, D.; Dominguez-Mompell, R.; Sfogliano, L.; Moon, W. An assessment of the magnitude, parallelism, and asymmetry of micro-implant-assisted rapid maxillary expansion in non-growing patients. Prog. Orthod. 2020, 21, 42. [Google Scholar] [CrossRef]
- Hirai, T.; Fukushima, N.; Go, K.; Takahashi, S.; Nishida, M.; Masuda, S.; Nagamine, H. Clinical Analysis of Septoplasty Performed via the Hemitransfixion Approach for Caudal End Deviation of the Nasal Septum. Nippon. Jibiinkoka Gakkai Kaiho 2018, 121, 664–672. [Google Scholar] [CrossRef]
- Huizing, E.H. Incorrect terminology in nasal anatomy and surgery, suggestions for improvement. Rhinol. J. 2003, 41, 129–133. [Google Scholar]
- Maniaci, A.; Merlino, F.; Cocuzza, S.; Iannella, G.; Vicini, C.; Cammaroto, G.; Lechien, J.R.; Calvo-Henriquez, C.; La Mantia, I. Endoscopic surgical treatment for rhinogenic contact point headache: Systematic review and meta-analysis. Eur. Arch. Oto Rhino Laryngol. 2021, 278, 1743–1753. [Google Scholar] [CrossRef] [PubMed]
- Cocuzza, S.; Maniaci, A.; Di Luca, M.; La Mantia, I.; Grillo, C.; Spinato, G.; Motta, G.; Testa, D.; Ferlito, S. Long-term results of nasal surgery: Comparison of mini-invasive turbinoplasty. J. Biol. Regul. Homeost. Agents 2020, 34, 1203–1208. [Google Scholar] [CrossRef]
- Cole, P.; Chaban, R.; Naito, K.; Oprysk, D. The Obstructive Nasal Septum: Effect of Simulated Deviations on Nasal Airflow Resistance. Arch. Otolaryngol. Neck Surg. 1988, 114, 410–412. [Google Scholar] [CrossRef]
- Mink, P.J. The nasal valves: Changes in anatomy and physiology in normal subjects. Rhinology 2000, 38, 7–12. [Google Scholar]
- Mladina, R. The role of maxillar morphology in the development of pathological septal deformities. Rhinol. J. 1987, 25, 199–205. [Google Scholar]
- Mladina, R.; Skitarelić, N.; Poje, G.; Šubarić, M. Clinical implications of nasal septal deformities. Balk. Med. J. 2015, 32, 137–146. [Google Scholar] [CrossRef]
- Mladina, R.; Čujić, E.; Šubarić, M.; Vuković, K. Nasal septal deformities in ear, nose, and throat patients: An international study. Am. J. Otolaryngol. 2008, 29, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.; Virk, J.S.; Randhawa, P.S.; Andrews, P.J. The internal nasal valve: A validated grading system and operative guide. Eur. Arch. Oto Rhino Laryngol. 2018, 275, 2739–2744. [Google Scholar] [CrossRef] [PubMed]
- Sunnychan, S.; Deshmukh, P. Association Between Anterior Rhinoscopic/Endoscopic Assessment of Internal Nasal Valve and Various Nasal Deformities in the Rural Population of Vidarbha Region of India: A Cross-Sectional Study. Cureus 2023, 15, e35682. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.C.; Swift, D.L.; Fujimoto, Y.; Huang, J.; Fukunaga, T.; Kato, R.; Higashino, M.; Shinomiya, S.; Kitadate, S.; Takahara, Y.; et al. Acoustic rhinometry: Evaluation of nasal cavity geometry by acoustic reflection. J. Appl. Physiol. 1989, 66, 295–303. [Google Scholar] [CrossRef]
- Stoksted, P.; Nielsen, J.Z. XV Rhinomanometric Measurements of the Nasal Passage. Ann. Otol. Rhinol. Laryngol. 1957, 66, 187–197. [Google Scholar] [CrossRef]
- Choi, H.; Park, I.-H.; Geun, H.; Lee, H.-M. Diagnostic Accuracy Evaluation of Nasal Sound Spectral Analysis Compared with Peak Nasal Inspiratory Flow in Nasal Septal Deviation. Am. J. Rhinol. Allergy 2011, 25, e86–e89. [Google Scholar] [CrossRef]
- Kimura, S.; Suzuki, M.; Honma, A.; Nakazono, A.; Osawa, M.; Nakamaru, Y.; Homma, A. Objective evaluation of caudal deviation of the nasal septum and selection of the appropriate septoplasty technique. Auris Nasus Larynx 2022, 49, 67–76. [Google Scholar] [CrossRef]


| The N/W Ratio | |||
|---|---|---|---|
| ≥0.8 | <0.8 | ||
| AR findings | Laterality (−) | 135 | 17 |
| Laterality (+) | 18 | 130 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirai, T.; Ueda, T.; Ishino, T.; Takeno, S. An Evaluation of the Caudal End Deviation of the Nasal Septum Using the Quantitative Analysis of Computed Tomography. Surg. Tech. Dev. 2023, 12, 145-155. https://doi.org/10.3390/std12030014
Hirai T, Ueda T, Ishino T, Takeno S. An Evaluation of the Caudal End Deviation of the Nasal Septum Using the Quantitative Analysis of Computed Tomography. Surgical Techniques Development. 2023; 12(3):145-155. https://doi.org/10.3390/std12030014
Chicago/Turabian StyleHirai, Tomohisa, Tsutomu Ueda, Takashi Ishino, and Sachio Takeno. 2023. "An Evaluation of the Caudal End Deviation of the Nasal Septum Using the Quantitative Analysis of Computed Tomography" Surgical Techniques Development 12, no. 3: 145-155. https://doi.org/10.3390/std12030014
APA StyleHirai, T., Ueda, T., Ishino, T., & Takeno, S. (2023). An Evaluation of the Caudal End Deviation of the Nasal Septum Using the Quantitative Analysis of Computed Tomography. Surgical Techniques Development, 12(3), 145-155. https://doi.org/10.3390/std12030014







