Abstract
Purpose: Although open reduction and internal fixation (ORIF) by plating are the treatment of choice for diaphyseal fractures of the forearm, delayed union and non-union remain as existing complications. This study aimed to analyze predictive factors for the union time in diaphyseal fractures of the forearm. Methods: A retrospective study was conducted on all adult patients with diaphyseal forearm fractures who underwent surgical treatment with plate fixation between 2007 and 2016 at a tertiary care referral center. The patients were divided into two groups based on their union times: ≤3 months or >3 months. They were then compared for demographics, fracture pattern and characteristics, associated injuries, type of fixation, and quality of postoperative reduction. Results: Eighty-six diaphyseal forearm bone fractures (radius, ulna, or both) were observed in 55 adults. Out of these fractures, 55 (65.1%) achieved union within ≤3 months, 26 (30.3%) took more than 3 months to achieve union, and 4 (4.6%) resulted in nonunion. The use of a locking plate in open reduction and internal fixation of diaphyseal forearm fractures significantly increased the likelihood of union within ≤3 months (p = 0.043). The parameter of gap width at the fracture site, as observed on postoperative X-rays, showed a qualitative and quantitative correlation with union time (p = 0.028). Conclusion: The use of a locking plate, combined with reducing the gap width at the fracture site after reduction during open reduction and internal fixation (ORIF) of diaphyseal forearm fractures, is significantly correlated with an increased likelihood of achieving bone union within 3 months.
1. Introduction
Forearm fractures can occur due to various traumatic forces, ranging from low energy incidents to high-energy trauma. The most common mechanism of injury for these fractures is axial loading applied to the forearm, typically resulting from a fall onto an outstretched hand. Forearm fractures encompass a spectrum of severity, ranging from simple, single-bone fractures to complex comminuted fractures or fracture dislocations. In adults, forearm fractures can also be caused by motor vehicle accidents and falls from heights. These injuries can manifest as either direct or indirect trauma, while less frequently seen mechanisms include gunshot injuries and nightstick injuries [1,2]. The interosseous membrane, situated between the radius and ulna, plays a crucial role in providing stability to the distal radioulnar joint, maintaining longitudinal stability in the forearm, and serving as an attachment site for forearm muscles [3]. The radius and ulna, along with secondary soft tissue stabilizers, function as a joint that facilitates pronation and supination movements. The Biceps brachii, Supinator, and Pronator teres can exert significant deforming forces in forearm fractures [4]. An accurate diagnosis of forearm fractures relies on a comprehensive assessment, including a detailed history, clinical examination, and relevant radiological investigations. It is important to conduct a thorough clinical examination to rule out open fractures and associated soft tissue injuries [5]. Diagnostic imaging, such as plain radiographs comprising anteroposterior and lateral views of the forearm, is routinely employed to confirm forearm fractures. Forearm fractures pose a high risk of concomitant injuries to the distal radioulnar joint (DRUJ), proximal radioulnar joint, and elbow dislocation.
Consequently, it is crucial to effectively manage such fractures to restore optimal forearm functionality. Successful fracture management aims to achieve anatomic (or near-anatomic) reduction, stable fixation, bony healing, an early return to daily activities, and minimize complications [6,7].
Although alternative approaches such as closed reduction and casting, external fixation, intramedullary nailing, and percutaneous pinning have been proven effective for the treatment of diaphyseal fractures of the radius and ulna [8,9,10], open reduction and internal fixation (ORIF) with compression plates remains the gold standard in adult patients [11]. Its reliability in terms of biomechanics and functional outcomes has been widely demonstrated [12,13,14,15], especially with the increasing use of locking plates [16,17]. Delayed unions and nonunions are still sometimes encountered, with incidence rates ranging from 2% to 10% in different studies. [4,14,18,19,20,21] and those complications can significantly complicate the recovery from these injuries. Nonunion of these fractures often requires revision surgery, which includes bone grafting in the case of established nonunion. Numerous risk factors influence the occurrence of nonunion in fractures of the upper and lower limbs [5,22,23,24].
This study’s primary objective was to address this knowledge gap and determine predictive factors influencing union time in adult patients with diaphyseal forearm fractures treated by plating. By discerning these factors, our aim is to advance our comprehension of the healing process in such fractures and potentially develop strategies to optimize treatment outcomes. The investigation of a diverse range of forearm fractures and their associated factors is intended to contribute to the existing body of knowledge, ultimately enhancing patient care and treatment outcomes in managing these injuries.
2. Materials and Methods
After obtaining approval from the institutional review board, a retrospective review was conducted on the medical charts, operative notes, and radiographic records of adult patients who underwent surgical treatment with plate fixation for diaphyseal forearm fractures. The study encompassed the period from 2007 to 2016 and focused on patients treated at a tertiary care referral center. To minimize potential bias, the study excluded certain patient groups, specifically individuals under the age of 18, smokers, patients with diabetes, those with open fractures, periprosthetic fractures, and patients with multiple traumas, from the analysis. The collected data included information on demographics, fracture characteristics, and the immediate postoperative status of the patients.
All radiographs underwent independent evaluation by two hand surgeons with specialized training in the field, who were unaware of the study’s objectives. This evaluation was performed using PACS (Picture Archiving and Communication System). In instances where discrepancies arose between the observers, a third surgeon conducted an assessment to facilitate the attainment of a unanimous decision whenever possible. Fractures were considered minimally displaced when the translation was less than one-third of the bone width and the angulation was less than 10 degrees in all planes. Moderate displacement was defined by the translation being between one- and two-thirds of the bone width or the angulation being more than 10 degrees. Very displaced fractures were those with the translation being greater than two-thirds of the bone width or the angulation being greater than 30 degrees in at least one plane. The gap at the fracture site was measured as well.
All the patients were operated on by senior orthopedic surgeons using a classic volar Henry approach for the radius and a medial longitudinal approach for the ulna. From 2007 to 2011, internal fixation was performed by means of non-locking compression plates with 3.5 mm cortical screws, ensuring a minimum of three screws on each side of the fracture, and a postoperative above-elbow cast was worn for 6 weeks. However, starting in 2011, our approach shifted to the utilization of locking compression plates while still adhering to the AO Foundation’s recommendation of employing a minimum of three screws on each side of the fracture. This newer technique enabled the initiation of an early postoperative therapy program without the need for prolonged postoperative immobilization.
Immediate postoperative X-rays were utilized to measure the width of any gaps present and determine the percentage of cortical contact for each fracture. Subsequently, the patients were scheduled for follow-up visits at 2, 6, and 12 weeks after the surgery. During these visits, X-rays were taken to evaluate the advancement of fracture healing.
Radiographic healing was defined as the interval in days between the occurrence of the fracture and the time when bridging in three of the four cortices is seen on X-ray images [25]. Based on the timing of union, the patients were categorized into two groups: those who achieved union within 3 months and those who experienced union either after more than 3 months or not at all, referred to as nonunion. This division allowed for the differentiation and analysis of the healing progress between the two groups, enabling a comprehensive understanding of the outcomes.
3. Statistical Analysis
Anonymous data were entered into an Excel sheet, and a meticulous manual check and descriptive data analysis were performed to ensure the accuracy of the data and assess its normality. Each parameter was individually subjected to a Fisher’s exact test to determine its association with the time to union. A chi-square test and logistic regression were performed to assess the association between the use of locking plates and the likelihood of achieving union. Additionally, a correlation analysis was carried out to examine the correlation between the gap width observed on immediate postoperative X-rays after reduction and the probability of requiring more than 3 months to achieve union. The chi-square test was used to test the initial association between these variables, whereas logistic regression was applied to control for potential confounding factors. The dependent variable in the logistic regression model was time to union. The independent variables were plate type (locking or non-locking), width of gap, and fracture location (mid 1/3, distal 1/3, and proximal 1/3). For statistical analysis, a 95% confidence interval was employed, and significance was defined as p < 0.05.
4. Results
Fifty-five adult patients with 86 diaphyseal forearm fractures were surgically treated with plate fixation during the study period. Of which, 49 fractures of the radius and 37 fractures of the ulna occurred. Thirty-one of the 55 study patients had fractures of both the radius and ulna. Forty-five patients (82%) were males and ten were females (representing a ratio of 9 to 2). The mean age at the time of surgery was 41 years (range 18–86, SD 20.7). Six radial fractures were associated with a distal radial ulnar joint dislocation (Galeazzi fracture-dislocation), and one ulnar fracture was associated with a proximal radial head dislocation (Monteggia fracture-dislocation). (Table 1) An additional oblique bi-cortical compression screw was used in eight cases. Overall, out of these fractures, 55 (65.1%) achieved union within ≤3 months, 26 (30.3%) took more than 3 months to achieve union, and 4 (4.6%) resulted in nonunion.

Table 1.
Demographic table.
In the mid 1/3 section of the radius, there were 28 fractures observed, while in the distal 1/3 section, there were 18 fractures. The proximal 1/3 section of the radius had the fewest fractures, with only 3 cases reported. Similarly, in the ulna bone, the highest number of fractures occurred in the mid 1/3 section (24 cases), followed by the distal 1/3 section (12 cases), and finally, only 1 fracture was reported in the proximal 1/3 section. Overall, the data indicates that the mid 1/3 section of both the radius and ulna bones had the highest number of fractures, with a total of 52 cases reported. The distal 1/3 section had 30 fractures, while the proximal 1/3 section had the fewest fractures, with only 4 cases observed across both bones.
The most common fracture type in the radius was transversal, with 36 cases reported. Following that, there were 10 cases of oblique fractures, 2 cases of bifocal fractures, and only 1 case of a spiral fracture. In the ulna bone, the highest number of fractures observed were of the transversal type, with 22 cases. This was followed by 10 cases of oblique fractures, 4 cases of bifocal fractures, and 1 case of a spiral fracture. Overall, across both bones, the transversal fracture type was the most prevalent, with a total of 58 cases reported. Oblique fractures accounted for 20 cases, bifocal fractures for 6 cases, and spiral fractures for 2 cases.
Among the fractures in the radius, a two-part fracture (i.e., a neat pattern) was the most common, with 34 cases reported. The butterfly pattern followed with 12 cases, and there were 3 cases of comminuted fractures. In the ulna bone, the highest number of fractures were neat, with 28 cases. This was followed by eight cases of butterfly fractures and one case of a comminuted fracture. Overall, considering both bones, neat fractures were the most prevalent, with a total of 62 cases reported. Butterfly fractures accounted for 20 cases, and there were 4 cases of comminuted fractures.
In the radius bone, there were 3 cases of non-displaced fractures, 12 cases of minimally displaced fractures, 1 case of moderately displaced fractures, and the highest number of fractures, with 33 cases, were very displaced. Regarding the ulna bone, there were 13 cases of non-displaced fractures, 5 cases of minimally displaced fractures, 3 cases of moderately displaced fractures, and 16 cases of very displaced fractures. Considering both bones, non-displaced fractures were observed in 16 cases, minimally displaced fractures in 17 cases, moderately displaced fractures in 4 cases, and the highest number of fractures, with 49 cases, were classified as very displaced.
Regarding the distribution of fractures based on the width gap in both the radius and ulna bones. In the radius bone, there were 22 cases where the width gap was 0 mm, indicating no gap between the fractured parts. For a 1 mm width gap, there were 17 cases, followed by 6 cases with a 2 mm width gap, 3 cases with a 3 mm width gap, and only 1 case with a 4 mm width gap. In the ulna bone, the highest number of fractures occurred with no width gap (0 mm), totaling 18 cases. There were 14 cases with a 1 mm width gap, 3 cases with a 2 mm width gap, 2 cases with a 3 mm width gap, and no fractures were reported with a 4 mm width gap. Overall, across both bones, the most common width gap was 0 mm, with a total of 40 cases. A 1 mm width gap was observed in 31 cases, followed by 9 cases with a 2 mm width gap, 5 cases with a 3 mm width gap, and only 1 case with a 4 mm width gap (Table 2). The width gap and percentage of cortical contact after reduction are presented in Table 3.

Table 2.
Description of the fractures and number.

Table 3.
Width gap and percentage of cortical contact after reduction, number.
Overall, 41 non-locking plates (Dynamic Compression Plates with Limited Bone Contact (LC-DCP), (Depuy Synthes, Oberdorf, Switzerland) and 45 locking plates were used, of which 28 were anatomic midshaft forearm plating systems (Acumed, Hislboro, OR, USA) and 17 were locking compression plates (Depuy Synthes, Oberdorf, Switzerland). No disparities in fracture patterns were observed between the groups. Based on the results of the logistic regression analysis, we found that the type of plate fixation used for the surgical treatment of diaphyseal forearm fractures had a significant association with the outcomes. Specifically, the group of patients who achieved union within 3 months had a higher proportion of individuals who received locking plate fixation compared to the nonunion group (p = 0.043). This indicates a statistically significant relationship, suggesting that the choice of locking plate fixation may have a positive impact on the early bone union process in these patients. (Figure 1) There was no difference between the two types of locking plates. The gap width after reduction as seen on immediate postoperative X-rays was correlated with the probability of requiring more than 3 months to achieve union, i.e., the wider the gap, the higher the probability (p = 0.028). There was no significant difference in the gap width after reduction between the locking and the non-locking groups.
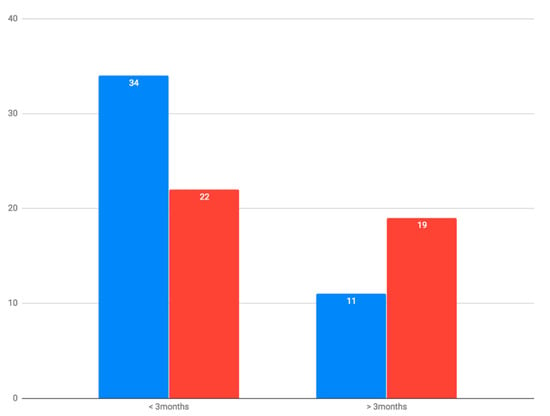
Figure 1.
Union time according to the type of plate (number of cases). Blue = locking; Red = non-locking.
At the final follow-up, four cases of nonunion were observed, with two involving the radius and two involving the ulna. Among these cases, one patient experienced nonunion in both bones, while the remaining nonunion cases were associated with segmental fractures. In terms of the initial treatment, three out of the four nonunion cases were managed with a locking plate. The patient with nonunion in both the radius and ulna eventually underwent revision surgery, which involved a massive iliac crest bone graft and fixation with new locking plates. Consequently, both bones achieved union within three months. The two other patients with nonunion remained asymptomatic during the final follow-up and did not undergo further surgical intervention. Notably, none of the other assessed parameters, including age, sex, fracture location, involvement of single or both forearm bones, fracture type, or preoperative displacement, demonstrated a significant correlation with the time required for union.
5. Discussion
The identification of predictive factors for the time to union in diaphyseal forearm fractures treated with plating has not been clearly defined. Mechanical elements, such as inadequate immobilization, nonoperative treatment, suboptimal internal or external fixation, excessive motion at the fracture site, and improper reduction or osteosynthesis systems, play a significant role. Additionally, biological factors, encompassing local elements such as bone defects, open fractures, infections, soft tissue injuries, segmental and comminuted fractures, as well as inter-fragmentary gaps, contribute to this phenomenon. Moreover, systemic factors, including neuropathy, diabetes, chronic smoking, chronic alcoholism, certain medications, and radiation therapy, can increase the risk of nonunion. Identifying and considering these risk factors is paramount in fracture management to minimize nonunion occurrence and promote favorable healing outcomes. Currently, there is a lack of comprehensive understanding regarding the specific factors that influence the duration of union in these types of fractures. However, the findings from our study shed light on this matter. We aimed to develop a classification system that could account for a wide range of fracture characteristics relevant to our study population and purpose. By considering factors such as translation relative to bone width and angulation in all planes, we aimed to provide a more nuanced understanding of fracture displacement. This detailed assessment allowed us to evaluate the impact of different degrees of displacement on the outcomes of plate fixation in these fractures. While the AO/OTA classification system is widely accepted and utilized, it primarily focuses on fracture pattern and location rather than specific displacement measurements.
We observed that the utilization of a locking plate, in comparison to a non-locking plate combined with a postoperative cast, significantly increased the likelihood of achieving union within 3 months among adult patients.
The superiority of locking plates can be attributed to their ability to provide a more rigid fixation, facilitating early active mobilization [16,17]. Our results strongly support the notion that postoperative immobilization is not obligatory when employing locking plates for ORIF in diaphyseal forearm fractures. This approach offers potential benefits in terms of reducing the duration of immobilization and enabling earlier initiation of rehabilitation protocols, thereby improving patient outcomes and promoting faster recovery.
Several reports have documented alternative treatment options to ORIF using plate fixation for adult diaphyseal forearm fractures [8,9,10]. One such alternative is the utilization of an intramedullary nail, which presents the theoretical advantage of a closed reduction and internal fixation achieved through a percutaneous technique. This approach respects the integrity of the soft tissue envelope while minimizing the need for extensive muscular and periosteal elevation [26]. However, it is important to note that, despite the existence of alternative techniques, ORIF with compression plates remains the gold standard for forearm fracture fixation [11]. This is primarily attributed to its ability to achieve a satisfactory fracture reduction and establish a stable structure. The reliability and effectiveness of ORIF with compression plates have been well established, making it the preferred approach in most cases of diaphyseal forearm fractures. Nonetheless, the consideration of alternative methods and their potential benefits is crucial for informed decision-making in individual patient cases, taking into account factors such as fracture type, patient characteristics, and surgical expertise [27].
Our study achieved an overall union rate of 95.4%, which aligns with the reported percentages found in the literature for various fixation devices [15,26,28,29]. Notably, our findings emphasized the qualitative and quantitative correlation between the fracture gap after reduction and the risk of nonunion within a 3-month timeframe. While the association between union time and reduction gap has been described in relation to lower limb fractures [30,31], this correlation has not been previously demonstrated in diaphyseal forearm fractures. The significance of this correlation is particularly relevant in cases of ORIF with plating, as the fracture hematoma is disrupted, necessitating an optimal amount of compression for successful bone healing. It is important to note that the biomechanical forces acting on the forearm differ significantly from those in the lower extremities, emphasizing the need for caution when extrapolating conclusions from lower to upper limb fractures. Interestingly, our study did not find a comparable correlation between union time and the other evaluated parameters.
Previous studies on lower limb diaphyseal fractures have reported a correlation between union time and the surface of cortical contact after reduction [30,31]. However, in our series of diaphyseal forearm fractures, this correlation did not reach a level of statistical significance. Caution should be exercised when extrapolating conclusions from lower limb fractures to upper limb fractures, as there are significant biomechanical differences between the two regions. The distinct loading forces and mechanical constraints in the forearm necessitate a separate consideration when evaluating the factors influencing union time.
Locking plates have shown superiority over non-locking plates in achieving union within the first three months following surgery, although the gap width after reduction was comparable between the two groups. While previous studies have demonstrated the biomechanical advantage of locking plates in terms of construct strength [12,16], the observation of faster bone healing compared to non-locking plates has not been consistently observed [17]. In the case of lower extremity fractures, where load-bearing perpendicular to the fracture line promotes bone healing, the radius and ulna are subjected to significant torque constraints during prono-supination. Unlike compressive loading forces, this motion within the fracture site is unlikely to enhance bone healing. Therefore, a more rigid construct that restricts such movements creates better conditions for faster bone union. Further biomechanical studies are required to support this hypothesis.
Although open fractures are typically associated with a higher risk of delayed union or nonunion within a three-month period, this study excluded patients with open fractures. This exclusion was made in order to maintain a more precise and concentrated analysis, thus enabling a clearer interpretation of the results. By doing so, the study aimed to minimize potential confounding factors and enhance the validity of its findings. Yi et al. compared injury patterns and outcomes of open versus closed fractures of the proximal ulna and found no significant differences in bone union rates or union delay [32]. They concluded that most of those fractures were open due to superficial and immediately subcutaneous skin lacerations from sharp bone edges, therefore leading to a wound that is less contaminated and with fewer soft tissue damages than seen in a penetrating injury such as from ballistic trauma or a mangled extremity. However, these considerations do not necessarily apply to diaphyseal fractures, and further investigations with larger numbers of open fracture cases will be required.
Contrary to the findings of Martin et al. [27], the use of a bi-cortical screw perpendicular to the fracture line, which was expected to provide stability and compression at the fracture site, did not show a significant correlation with a shorter time to union. However, it is important to note that in this study, only eight cases involved the use of bi-cortical screws, limiting the statistical power and preventing firm conclusions from being drawn. The same limitation applies to fractures complicated by a proximal or distal radio ulnar joint dislocation (Monteggia or Galeazzi fracture-dislocation).
In the case of a single fracture of the radius, ulna, or both, the bone union ratio within three months was not affected. However, due to the small sample size and unequal distribution within these three groups, drawing definitive conclusions is difficult.
This study has several limitations that should be acknowledged. Firstly, the retrospective nature of the study introduces potential bias, as the data collection relies on past records. Secondly, the relatively small number of patients within our subgroups limits the generalizability of the findings. Furthermore, we did not utilize the AO/OTA classification system, potentially impacting the generalizability and comparability of our findings with other studies. Additionally, the broader definitions of ‘delayed union’ and ‘nonunion’ used in this study may limit direct comparison with studies employing strict clinical criteria. Finally, it is important to note that the distribution between non-locking and locking plating was purely chronological, as the surgical technique was modified and the use of locking plates was implemented in 2011. This may introduce confounding factors that could impact the interpretation of the results.
6. Conclusions
The findings of this study indicate that several preoperative parameters, including age, sex, fracture location (radius, ulna, or both; proximal, mid, or distal third), fracture type, and preoperative displacement, showed no significant correlation with the time required for union. However, two perioperative parameters, namely the utilization of a locking plate and the gap width after reduction, demonstrated a significant correlation with the likelihood of achieving union within three months. These factors could be considered predictive indicators for the time to union in adult diaphyseal forearm fractures.
Author Contributions
Conceptualization, F.A. and T.P.; methodology, R.G.; formal analysis, G.E.; investigation, D.T., Y.R. and T.P.; data curation, R.G. and G.E.; writing—original draft preparation, S.F. and F.A.; writing—review and editing, S.F., Y.R. and F.A.; supervision, F.A.; project administration, S.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Tel Aviv Medical Center (protocol code TLV-0206-18. date of approval: 1 May 2018) for studies involving humans.
Informed Consent Statement
Patient consent was waived due to the retrospective nature of this study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding authors. The data are not publicly available due to the restrictions imposed by the local Helsinki committee.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Schulte, L.M.; Meals, C.G.; Neviaser, R.J. Management of adult diaphyseal both-bone forearm fractures. J. Am. Acad. Orthop. Surg. 2014, 22, 437–446. [Google Scholar] [CrossRef]
- Bot, A.G.J.; Doornberg, J.N.; Lindenhovius, A.L.C.; Ring, D.; Goslings, J.C.; Van Dijk, C.N. Long-term outcomes of fractures of both bones of the forearm. J. Bone Jt. Surg. 2011, 93, 527–532. [Google Scholar] [CrossRef]
- Adams, J.E. Forearm Instability: Anatomy, Biomechanics, and Treatment Options. J. Hand Surg. Am. 2017, 42, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Richard, M.J.; Ruch, D.S.; Aldridge, J.M. Malunions and Nonunions of the Forearm. Hand Clin. 2007, 23, 235–243. [Google Scholar] [CrossRef]
- Dimartino, S.; Pavone, V.; Carnazza, M.; Cuffaro, E.R.; Sergi, F.; Testa, G. Forearm Fracture Nonunion with and without Bone Loss: An Overview of Adult and Child Populations. J. Clin. Med. 2022, 11, 4106. [Google Scholar] [CrossRef]
- Delpont, M.; Louahem, D.; Cottalorda, J. Monteggia injuries. Orthop. Traumatol. Surg. Res. 2018, 104, S113–S120. [Google Scholar] [CrossRef]
- Zhang, X.F.; Huang, J.W.; Mao, H.X.; Chen, W.B.; Luo, Y. Adult diaphyseal both-bone forearm fractures: A clinical and biomechanical comparison of four different fixations. Orthop. Traumatol. Surg. Res. 2016, 102, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.B.; Kakar, S. Adult diaphyseal forearm fractures: Intramedullary nail versus plate fixation. J. Hand Surg. Am. 2011, 36, 1216–1219. [Google Scholar] [CrossRef]
- Dhariwal, Q.; Inamdar, P.; Arora, P.; Shyam, A. Stacked Flexible Nailing for Radius Ulna Fractures: Revival of a lost Technique. J. Orthop. Case Rep. 2017, 7, 106–108. [Google Scholar] [PubMed]
- Hong, G.; Cong-Feng, L.; Hui-Peng, S.; Cun-Yi, F.; Bing-Fang, Z. Treatment of diaphyseal forearm nonunions with interlocking intramedullary nails. Clin. Orthop. Relat. Res. 2006, 450, 186–192. [Google Scholar] [CrossRef]
- Al-Sadek, T.A.; Niklev, D.; Al-Sadek, A. Diaphyseal fractures of the forearm in adults, plating or intramedullary nailing is a better option for the treatment? Maced. J. Med. Sci. 2016, 4, 670–673. [Google Scholar] [CrossRef]
- Roberts, J.W.; Grindel, S.I.; Rebholz, B.; Wang, M. Biomechanical Evaluation of Locking Plate Radial Shaft Fixation: Unicortical Locking Fixation Versus Mixed Bicortical and Unicortical Fixation in a Sawbone Model. J. Hand Surg. Am. 2007, 32, 971–975. [Google Scholar] [CrossRef]
- Knight, R.A.; Purvis, G.D. Fractures of both bones of the forearm in adults. J. Bone Jt. Surg. Am. 1949, 31, 755–764. [Google Scholar] [CrossRef]
- Droll, K.P.; Perna, P.; Potter, J.; Harniman, E.; Schemitsch, E.H.; McKee, M.D. Outcomes following plate fixation of fractures of both bones of the forearm in adults. J. Bone Jt. Surg. Ser. A 2007, 89, 2619–2624. [Google Scholar] [CrossRef]
- Kim, S.B.; Heo, Y.M.; Yi, J.W.; Lee, J.B.; Lim, B.G. Shaft fractures of both forearm bones: The outcomes of surgical treatment with plating only and combined plating and intramedullary nailing. Clin. Orthop. Surg. 2015, 7, 282–290. [Google Scholar] [CrossRef]
- Zhang, X.; Hu, C.; Yu, K.; Bai, J.; Tian, D.; Xu, Y.; Zhang, B. Volar locking plate (VLP) versus non-locking plate (NLP) in the treatment of die-punch fractures of the distal radius, an observational study. Int. J. Surg. 2016, 34, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Pérez, M.; Gutiérrez-Morales, M.J.; Guerra-Ferraz, A.; Pais-Brito, J.L.; Boluda-Mengod, J.; Garcés, G.L. Locking versus non-locking one-third tubular plates for treating osteoporotic distal fibula fractures: A comparative study. Injury 2017, 6, S60–S65. [Google Scholar] [CrossRef]
- Marcheix, P.S.; Delclaux, S.; Ehlinger, M.; Scheibling, B.; Dalmay, F.; Hardy, J.; Lebaron, M.; Bonnevialle, P. Pre- and postoperative complications of adult forearm fractures treated with plate fixation. Orthop. Traumatol. Surg. Res. 2016, 102, 781–784. [Google Scholar] [CrossRef]
- Jayakumar, P.; Jupiter, J.B. Non-union in forearm fractures. Acta Chir. Orthop. Traumatol. Cech. 2014, 81, 22–32. [Google Scholar]
- Dodge, H.S.; Cady, G.W. Treatment of fractures of the radius and ulna with compression plates. J. Bone Jt. Surg. Am. 1972, 54, 1167–1176. [Google Scholar] [CrossRef]
- Hadden, W.A.; Reschauer, R.; Seggl, W. Results of AO plate fixation of forearm shaft fractures in adults. Injury 1983, 15, 44–52. [Google Scholar] [CrossRef]
- Boussakri, H.; Elibrahimi, A.; Bachiri, M.; Elidrissi, M.; Shimi, M.; Elmrini, A. Nonunion of fractures of the ulna and radius diaphyses: Clinical and radiological results of surgical treatment. Malays. Orthop. J. 2016, 10, 27–34. [Google Scholar] [CrossRef]
- Kloen, P.; Buijze, G.A.; Ring, D. Management of forearm nonunions: Current concepts. Strateg. Trauma Limb Reconstr. 2012, 7, 1–11. [Google Scholar] [CrossRef]
- Perisano, C.; Cianni, L.; Polichetti, C.; Cannella, A.; Mosca, M.; Caravelli, S.; Maccauro, G.; Greco, T. Plate Augmentation in Aseptic Femoral Shaft Nonunion after Intramedullary Nailing: A Literature Review. Bioengineering 2022, 9, 560. [Google Scholar] [CrossRef]
- Patel, S.P.; Anthony, S.G.; Zurakowski, D.; Didolkar, M.M.; Kim, P.S.; Wu, J.S.; Kung, J.W.; Dolan, M.; Rozental, T.D. Radiographic scoring system to evaluate union of distal radius fractures. J. Hand Surg. Am. 2014, 39, 1471–1479. [Google Scholar] [CrossRef]
- Young, H.L.; Sang, K.L.; Moon, S.C.; Goo, H.B.; Hyun, S.G.; Kyung, H.K. Interlocking contoured intramedullary nail fixation for selected diaphyseal fractures of the forearm in adults. J. Bone Jt. Surg. Ser. A 2008, 90, 1891–1898. [Google Scholar] [CrossRef]
- Mehdi Nasab, S.A.; Sarrafan, N.; Sabahi, S. Four-screw plate fixation vs conventional fixation for diaphyseal fractures of the forearm. Trauma. Mon. 2012, 17, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.D.; Sisk, T.D.; Tooms, R.E.; Park, W.I. Compression plate fixation in acute diaphyseal fractures of the radius and ulna. J. Bone Jt. Surg. Ser. A 1975, 57, 287–297. [Google Scholar] [CrossRef]
- Chapman, M.W.; Gordon, E.; Zissimos, A.G. Compression-plate fixation of acute fractures of the diaphyses of the radius and ulna. J. Bone Jt. Surg. Ser. A 1989, 71, 159–169. [Google Scholar] [CrossRef]
- Lim, H.S.; Kim, C.K.; Park, Y.S.; Moon, Y.W.; Lim, S.J.; Kim, S.M. Factors associated with increased healing time in complete femoral fractures after long-term bisphosphonate therapy. J. Bone Jt. Surg. Am. 2016, 98, 1978–1987. [Google Scholar] [CrossRef]
- Fong, K.; Truong, V.; Foote, C.J.; Petrisor, B.; Williams, D.; Ristevski, B.; Sprague, S.; Bhandari, M. Predictors of nonunion and reoperation in patients with fractures of the tibia: An observational study. BMC Musculoskelet. Disord. 2013, 14, 103. [Google Scholar] [CrossRef] [PubMed]
- Yi, P.H.; Weening, A.A.; Shin, S.R.; Hussein, K.I.; Tornetta, P.; Jawa, A. Injury patterns and outcomes of open fractures of the proximal ulna do not differ from closed fractures. Clin. Orthop. Relat. Res. 2014, 472, 2100–2104. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).