Accuracy of Death Certificates for Children: A Population-Based Retrospective Analysis
Abstract
1. Introduction
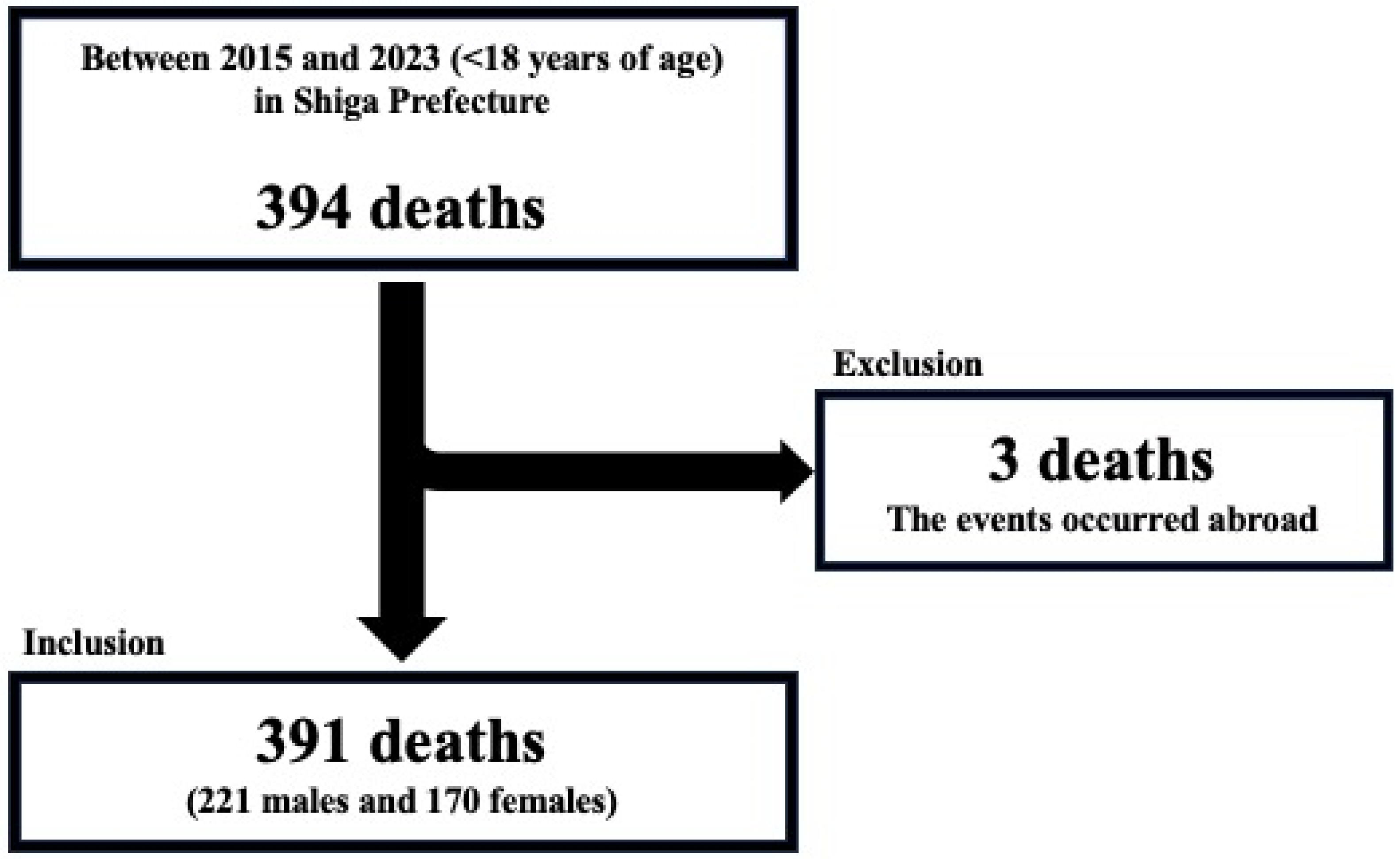
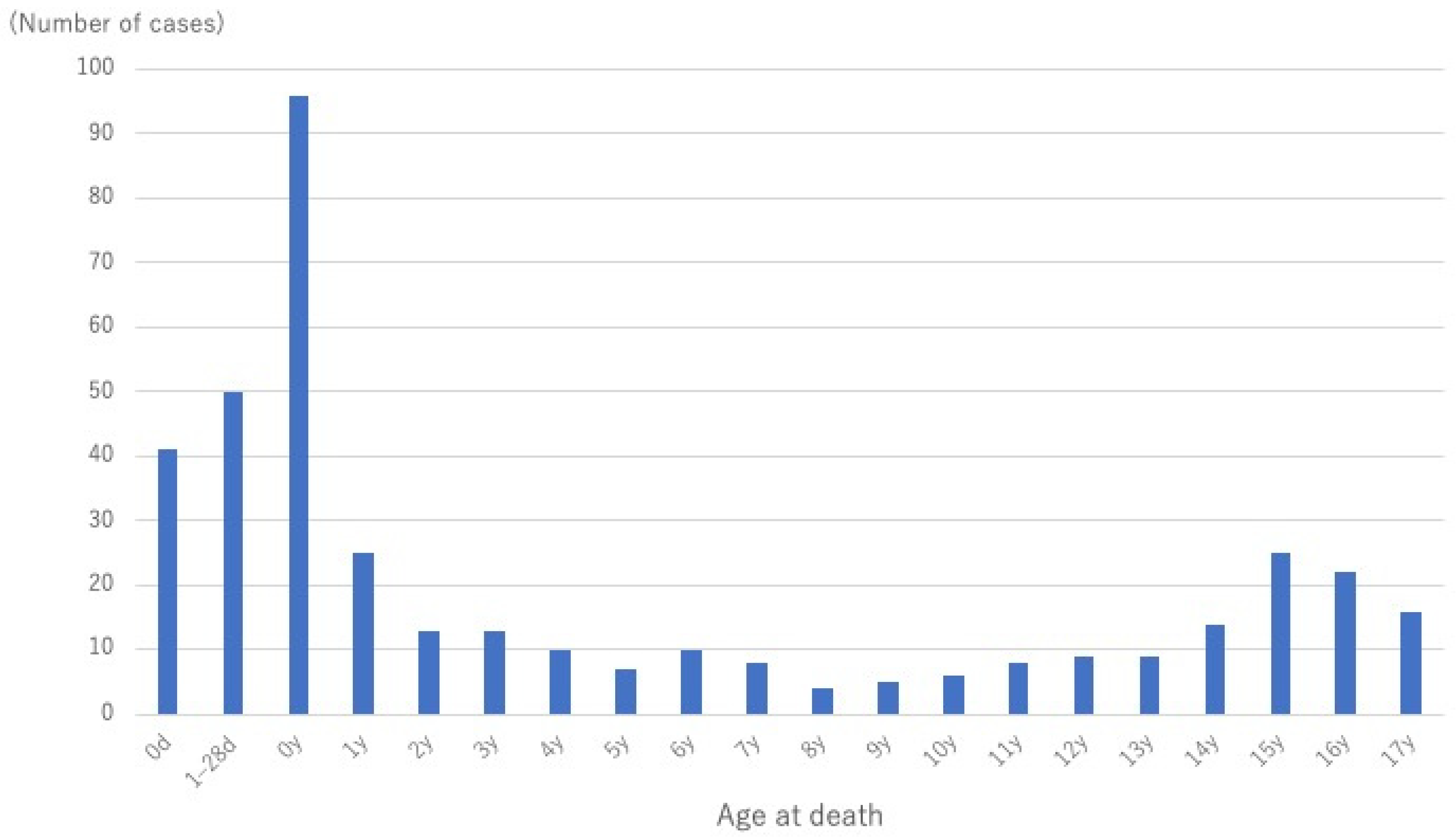
2. Materials and Methods
3. Results
3.1. General Background
3.2. Prevalence of Errors
3.3. Comparison of Distribution of Underlying Causes of Death
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DC | Death certificate |
| ICD | International Classification of Diseases |
| SIDS | Sudden infant death syndrome |
| EZR | Easy R (graphical user interface for R) |
| COVID-19 | Coronavirus disease 2019 |
| RD | Risk difference |
| CI | Confidence interval |
| BH | Benjamini–Hochberg |
References
- Global Burden of Disease Study 2021 Fertility and Forecasting Collaborators. Global fertility in 204 countries and territories, 1950–2021, with forecasts to 2100: A comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2057–2099. [Google Scholar] [CrossRef]
- World Health Organization. Newborns: Improving Survival and Well-Being. Available online: https://www.who.int/en/news-room/fact-sheets/detail/newborns-reducing-mortality (accessed on 8 July 2025).
- Lucero, M.; Riley, I.D.; Hazard, R.H.; Sanvictores, D.; Tallo, V.; Dumaluan, D.G.M.; Ugpo, J.M.; Lopez, A.D. Assessing the quality of medical death certification: A case study of concordance between national statistics and results from a medical record review in a regional hospital in the Philippines. Popul. Health Metr. 2018, 16, 23. [Google Scholar] [CrossRef] [PubMed]
- Dadzie, D.; Boadu, R.O.; Engmann, C.M.; Twum-Danso, N.A.Y. Evaluation of neonatal mortality data completeness and accuracy in Ghana. PLoS ONE 2021, 16, e0239049. [Google Scholar] [CrossRef] [PubMed]
- Khelil, M.B.; Kamel, M.; Lahmar, S.; Mrabet, A.; Falfoul, N.B.; Hamdoun, M. Death certificate accuracy in a Tunisian Emergency Department. Tunis. Med. 2017, 95, 422–428. [Google Scholar] [PubMed]
- Lu, T.H.; Shau, W.Y.; Shih, T.P.; Lee, M.C.; Chou, M.C.; Lin, C.K. Factors associated with errors in death certificate completion. A national study in Taiwan. J. Clin. Epidemiol. 2001, 54, 232–238. [Google Scholar] [CrossRef]
- El-Nour, A.E.; Mohammed, A.; Yousif, I.; Ali, A.H.; Makki, M. Evaluation of death certificates in the pediatric hospitals in Khartoum state during 2004. Sudan. J. Public Health 2007, 2, 29–37. [Google Scholar]
- Hazard, R.H.; Chowdhury, H.R.; Adair, T.; Ansar, A.; Rahman, A.M.Q.; Alam, S.; Alam, N.; Rampatige, R.; Streatfield, P.K.; Riley, I.D.; et al. The quality of medical death certification of cause of death in hospitals in rural Bangladesh: Impact of introducing the International Form of Medical Certificate of Cause of Death. BMC Health Serv. Res. 2017, 17, 688. [Google Scholar] [CrossRef] [PubMed]
- Dash, S.K.; Behera, B.K.; Patro, S. Accuracy in certification of cause of death in a tertiary care hospital—A retrospective analysis. J. Forensic Leg. Med. 2014, 24, 33–36. [Google Scholar] [CrossRef]
- Hernández, B.; Ramírez-Villalobos, D.; Romero, M.; Gómez, S.; Atkinson, C.; Lozano, R. Assessing quality of medical death certification: Concordance between gold standard diagnosis and underlying cause of death in selected Mexican hospitals. Popul. Health Metr. 2011, 9, 38. [Google Scholar] [CrossRef]
- Katsakiori, P.F.; Panagiotopoulou, E.C.; Sakellaropoulos, G.C.; Papazafiropoulou, A.; Kardara, M. Errors in death certificates in a rural area of Greece. Rural. Remote Health 2007, 7, 822. [Google Scholar] [CrossRef]
- Urabe, S.; Ishihara, K.; Chiba, F.; Yamaguchi, R.; Shiko, Y.; Kawasaki, Y.; Iwase, H. Children’s death survey using death certificates in the Chiba prefecture Forensic. Sci. Int. Rep. 2021, 4, 100246. [Google Scholar] [CrossRef]
- Ito, E.; Hitosugi, M.; Maruo, Y.; Nakamura, M.; Takaso, M.; Masumitsu, A.; Baba, M. Availability of death review of children using death certificates and forensic autopsy results. Leg. Med. 2023, 60, 102156. [Google Scholar] [CrossRef]
- National Center for Health Statistics. Physician’s Handbook on Medical Certification of Death; National Center for Health Statistics: Hyattsville, MD, USA, 2023. [CrossRef]
- Pearson, G.A.; Ward-Platt, K. How children die: Classifying child deaths. Arch. Dis. Child. 2011, 296, 922–926. [Google Scholar] [CrossRef]
- Global Burden of Disease Study 2015 Child Mortality Collaborators. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1725–1774. [Google Scholar] [CrossRef]
- Pitt, M.J.; Morris, J.K. European trends in mortality in children with congenital anomalies: 2000–2015. Birth Defects Res. 2021, 113, 958–967. [Google Scholar] [CrossRef] [PubMed]
- Takashima, K.; Hitosugi, M. Underestimation of Trisomy 18 and 13 Syndromes in Vital Statistics from Inadequate Death Certificates. Neonatology 2022, 119, 133–134. [Google Scholar] [CrossRef] [PubMed]
- Rissmann, A.; Tan, J.; Glinianaia, S.V.; Rankin, J.; Pierini, A.; Santoro, M.; Coi, A.; Garne, E.; Loane, M.; Given, J.; et al. Causes of death in children with congenital anomalies up to age 10 in eight European countries. BMJ Paediatr. Open 2023, 7, e001617. [Google Scholar] [CrossRef]
- Gupta, N.; Bharti, B.; Singhi, S.; Kumar, P.; Thakur, J.S. Errors in filling WHO death certificate in children: Lessons from 1251 death certificates. J. Trop. Pediatr. 2014, 60, 74–78. [Google Scholar] [CrossRef]
- Shantibala, K.; Akoijam, B.S.; Usharani, L.; Singh, H.N.; Laishram, J.; Singh, T.A. Death certification in a teaching hospital—A one year review. Indian J. Public Health 2009, 53, 31–33. [Google Scholar] [PubMed]
- Niska, R.; Bhuiya, F.; Xu, J. National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl. Health Stat. Rep. 2010, 26, 1–31. [Google Scholar]
- United States Burden of Disease Collaborators. The state of US health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA 2013, 310, 591–608. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Pérez-Méndez, L. Evaluating an educational intervention to improve the accuracy of death certification among trainees from various specialties. BMC Health Serv. Res. 2007, 7, 183. [Google Scholar] [CrossRef] [PubMed]
- Lakkireddy, D.R.; Basarakodu, K.R.; Vacek, J.L.; Kondur, A.K.; Ramachandruni, S.K.; Esterbrooks, D.J.; Markert, R.J.; Gowda, M.S. Improving death certificate completion: A trial of two training interventions. J. Gen. Intern. Med. 2007, 22, 544–548. [Google Scholar] [CrossRef]
| Group | Error Description |
|---|---|
| A | Inappropriate cause of death |
| A1 | Heart failure or respiratory failure as end-stage condition listed under immediate cause of death |
| A2 | The order of cause of death is wrong |
| A3 | Inappropriate injury or disease name |
| A4 | Cause of death listed as unknown without an autopsy |
| B | Inappropriate type for manner of death |
| C | Underlying cause of death was not listed or was listed under other significant conditions contributing death |
| D | Minor mistakes |
| Specialty | Prevalence | Fisher’s p-Value (vs. Other Professionals) |
|---|---|---|
| Pediatrician | 34.1% (77/226) | 0.07 |
| Physician and Surgeon | 32.8% (20/61) | 0.65 |
| Forensic physician | 8.4% (7/83) | <0.01 |
| Obstetrician | 92.9% (13/14) | <0.01 |
| Total | 30.9% (121/391) | − |
| Type of Error | Pediatrician | Physician and Surgeon | Forensic Physician | Obstetrician | Total |
|---|---|---|---|---|---|
| A | 63.6% | 80.0% | 57.1% | 92.3% | 67.8% |
| A1 | 23.4% | 25.0% | 0.0% | 61.5% | 25.6% |
| A2 | 5.0% | 10.0% | 0.0% | 7.7% | 5.0% |
| A3 | 39.7% | 60.0% | 42.9% | 23.1% | 39.7% |
| A4 | 3.3% | 0.0% | 14.3% | 7.7% | 3.3% |
| B | 4.1% | 5.0% | 0.0% | 0.0% | 4.1% |
| C | 28.9% | 15.0% | 0.0% | 23.1% | 28.9% |
| D | 17.4% | 10.0% | 42.9% | 38.5% | 17.4% |
| Manner of Death | Cause of Death | Period | RD (Post − Pre), pp | 95% CI, pp | Fisher’s p-Value | BH q-Value | |
|---|---|---|---|---|---|---|---|
| 2015–2019 (Pre) | 2020–2023 (Post) | ||||||
| Homicide | 2 (0.9%) | 0 (0%) | −0.90% | (−3.3%, 1.9%) | 0.50 | 0.58 | |
| Suicide | 13 (6.1%) | 20 (11.3%) | 5.20% | (−2.7%, 13.2%) | 0.07 | 0.23 | |
| Accidental death | 37 (17.3%) | 34 (19.2%) | 1.90% | (−8.8%, 12.8%) | 0.69 | 0.69 | |
| Disease | Malignant Diseases | 28 (13.1%) | 14 (7.9%) | −5.20% | (−13.5%, 3.6%) | 0.10 | 0.26 |
| Acute Diseases | 36 (16.8%) | 7 (4.0%) | −12.90% | (−20.5%, −4.5%) | <0.01 | <0.01 | |
| Chronic Diseases | 9 (4.2%) | 3 (1.7%) | −2.50% | (−7.2%, 2.6%) | 0.24 | 0.40 | |
| Congenital Diseases | 27 (12.6%) | 43 (24.3%) | 11.70% | (0.8%, 22.3%) | <0.01 | 0.02 | |
| Perinatal Diseases | 40 (18.7%) | 38 (21.5%) | 2.80% | (−8.4%, 14.1%) | 0.53 | 0.58 | |
| Infectious Diseases | 11 (5.1%) | 14 (7.9%) | 2.80% | (−4.2%, 9.9%) | 0.30 | 0.43 | |
| Unknown/SIDS | 11 (5.1%) | 4 (2.3%) | −2.90% | (−8.1%, 2.8%) | 0.19 | 0.38 | |
| Total | 214 (100%) | 177 (100%) | − | − | − | − | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, M.; Hitosugi, M.; Ito, E.; Takashima, K.; Nakamura, M.; Narumiya, S.; Maruo, Y. Accuracy of Death Certificates for Children: A Population-Based Retrospective Analysis. Pediatr. Rep. 2025, 17, 115. https://doi.org/10.3390/pediatric17060115
Yamamoto M, Hitosugi M, Ito E, Takashima K, Nakamura M, Narumiya S, Maruo Y. Accuracy of Death Certificates for Children: A Population-Based Retrospective Analysis. Pediatric Reports. 2025; 17(6):115. https://doi.org/10.3390/pediatric17060115
Chicago/Turabian StyleYamamoto, Masahito, Masahito Hitosugi, Eisuke Ito, Kohei Takashima, Mami Nakamura, Seiro Narumiya, and Yoshihiro Maruo. 2025. "Accuracy of Death Certificates for Children: A Population-Based Retrospective Analysis" Pediatric Reports 17, no. 6: 115. https://doi.org/10.3390/pediatric17060115
APA StyleYamamoto, M., Hitosugi, M., Ito, E., Takashima, K., Nakamura, M., Narumiya, S., & Maruo, Y. (2025). Accuracy of Death Certificates for Children: A Population-Based Retrospective Analysis. Pediatric Reports, 17(6), 115. https://doi.org/10.3390/pediatric17060115







