Acute Abdominal Pain with Obstructing Trichobezoar: A Pediatric Case of Rapunzel Syndrome Diagnosed in a Pediatric Emergency Department
Abstract
1. Introduction
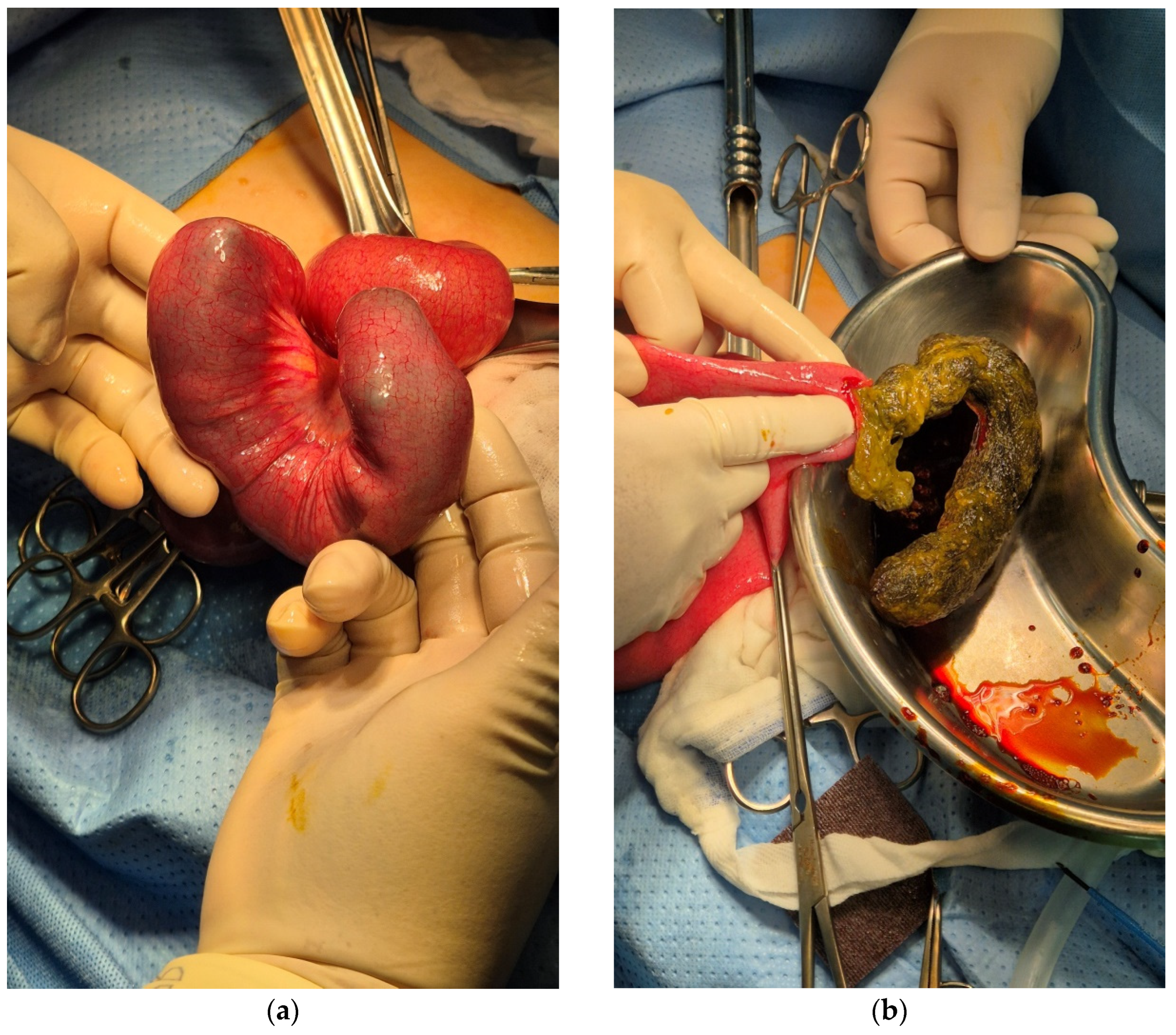
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ED | Emergency department |
| CT | Computed tomography |
References
- Leung, A.K.; Sigalet, D.L. Acute abdominal pain in children. Am. Fam. Physician 2003, 67, 2321–2326. [Google Scholar] [PubMed]
- Scholer, S.J.; Pituch, K.; Orr, D.P.; Dittus, R.S. Clinical outcomes of children with acute abdominal pain. Pediatrics 1996, 98, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Eng, K.; Kay, M. Gastrointestinal bezoars: History and current treatment paradigms. Gastroenterol. Hepatol. 2012, 8, 776–778. [Google Scholar]
- Naik, S.; Gupta, V.; Naik, S.; Rangole, A.; Chaudhary, A.K.; Jain, P.; Sharma, A.K. Rapunzel syndrome reviewed and redefined. Dig. Surg. 2007, 24, 157–161. [Google Scholar] [CrossRef]
- Kwok, A.M.F. Trichobezoar as a cause of pediatric acute small bowel obstruction. Clin. Case Rep. 2020, 8, 166–170. [Google Scholar] [CrossRef]
- Kim, J.S. Acute abdominal pain in children. Pediatr. Gastroenterol. Hepatol. Nutr. 2013, 16, 219–224. [Google Scholar] [CrossRef]
- Lin, K.C.; Wu, H.P.; Huang, C.Y.; Lin, C.Y.; Chang, C.F. Discriminant analysis of serum inflammatory biomarkers which differentiate pediatric appendicitis from other acute abdominal diseases. Acta Paediatr. Taiwan. 2007, 48, 125–130. [Google Scholar]
- Tseng, Y.C.; Lee, M.S.; Chang, Y.J.; Wu, H.P. Acute abdomen in pediatric patients admitted to the pediatric emergency department. Pediatr. Neonatol. 2008, 49, 126–134. [Google Scholar] [CrossRef]
- Jackson, P.; Vigiola Cruz, M. Intestinal Obstruction: Evaluation and Management. Am. Fam. Physician 2018, 98, 362–367. [Google Scholar]
- Sayed, A.O.; Zeidan, N.S.; Fahmy, D.M.; Ibrahim, H.A. Diagnostic reliability of pediatric appendicitis score, ultrasound and low-dose computed tomography scan in children with suspected acute appendicitis. Ther. Clin. Risk Manag. 2017, 13, 847–854. [Google Scholar] [CrossRef]
- Cison, H.; Kus, A.; Popowicz, E.; Szyca, M.; Reich, A. Trichotillomania and Trichophagia: Modern Diagnostic and Therapeutic Methods. Dermatol. Ther. 2018, 8, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Daoud, R.; Tlili, A.; Fendri, S.; Akrout, A.; Trigui, A.; Boujelbene, S. Gastric trichobezoar: An uncommon cause of epigastric pain: A case report. Clin. Case Rep. 2022, 10, e05653. [Google Scholar] [CrossRef] [PubMed]
- Shetty, S.; Janarathanan, K.; Arunachalam, P. Trichotillomania with gastric trichobezoar. Ann. Gastroenterol. 2013, 26, 255. [Google Scholar] [PubMed]
- Czerwinska, K.; Bekiesinska-Figatowska, M.; Brzewski, M.; Gogolewski, M.; Wolski, M. Trichobezoar, rapunzel syndrome, tricho-plaster bezoar—A report of three cases. Pol. J. Radiol. 2015, 80, 241–246. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, M.J.; McGreal, G.; Walsh, J.G.; Redmond, H.P. Trichobezoar. J. R. Soc. Med. 2001, 94, 68–70. [Google Scholar] [CrossRef]
- Verma, A.; Sharma, S.; Tyagi, G.; Singh, S. Huge trichobezoar causing obstructive jaundice. BMJ Case Rep. 2014, 2014, bcr2013201667. [Google Scholar] [CrossRef]
- Vaughan, E.D., Jr.; Sawyers, J.L.; Scott, H.W., Jr. The Rapunzel syndrome. An unusual complication of intestinal bezoar. Surgery 1968, 63, 339–343. [Google Scholar]
- Mirza, M.B.; Talat, N.; Saleem, M. Gastrointestinal trichobezoar: An experience with 17 cases. J. Pediatr. Surg. 2020, 55, 2504–2509. [Google Scholar] [CrossRef]
- Habib, M.; Amjad, M.B.; Abbas, M.; Chaudhary, M.A. Gastric Trichobezoars in paediatric population—A series of six cases and literature review. Ann. Med. Surg. 2022, 84, 104906. [Google Scholar] [CrossRef]
- Kaba, M.; Karadag, C.A.; Sever, N.; Ser, I.; Demir, M.; Yildiz, A.; Usta, A.M. A rare cause of intestinal obstruction in children trichobezoar: How to diagnose? Ulus. Travma Acil Cerrahi Derg. 2023, 29, 1288–1295. [Google Scholar] [CrossRef]
- Pogorelic, Z.; Juric, I.; Zitko, V.; Britvic-Pavlov, S.; Biocic, M. Unusual cause of palpable mass in upper abdomen--giant gastric trichobezoar: Report of a case. Acta Chir. Belg. 2012, 112, 160–163. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Ramirez, B.E.; Nuno-Guzman, C.M.; Zaragoza-Carrillo, R.E.; Salado-Renteria, H.; Gomez-Abarca, A.; Corona, J.L. Small-Bowel Obstruction Secondary to Ileal Trichobezoar in a Patient with Rapunzel Syndrome. Case Rep. Gastroenterol. 2018, 12, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Chun, S.W.; Lee, K.; Park, Y.J.; Shin, H.D. [Rapunzel Syndrome Removed with Enteroscopy in a Child]. Korean J. Gastroenterol. 2019, 74, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.C.; Andrade, T.C.; Brito, F.F.; Silva, G.V.; Cavalcante, M.L.; Martelli, A.C. Trichotillomania: A case report with clinical and dermatoscopic differential diagnosis with alopecia areata. An. Bras. Dermatol. 2017, 92, 118–120. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-H.; Lee, J.-I.; Park, S.; Paek, S.-H. Acute Abdominal Pain with Obstructing Trichobezoar: A Pediatric Case of Rapunzel Syndrome Diagnosed in a Pediatric Emergency Department. Pediatr. Rep. 2025, 17, 53. https://doi.org/10.3390/pediatric17030053
Kim S-H, Lee J-I, Park S, Paek S-H. Acute Abdominal Pain with Obstructing Trichobezoar: A Pediatric Case of Rapunzel Syndrome Diagnosed in a Pediatric Emergency Department. Pediatric Reports. 2025; 17(3):53. https://doi.org/10.3390/pediatric17030053
Chicago/Turabian StyleKim, Sung-Ha, Jong-In Lee, Soohyun Park, and So-Hyun Paek. 2025. "Acute Abdominal Pain with Obstructing Trichobezoar: A Pediatric Case of Rapunzel Syndrome Diagnosed in a Pediatric Emergency Department" Pediatric Reports 17, no. 3: 53. https://doi.org/10.3390/pediatric17030053
APA StyleKim, S.-H., Lee, J.-I., Park, S., & Paek, S.-H. (2025). Acute Abdominal Pain with Obstructing Trichobezoar: A Pediatric Case of Rapunzel Syndrome Diagnosed in a Pediatric Emergency Department. Pediatric Reports, 17(3), 53. https://doi.org/10.3390/pediatric17030053






