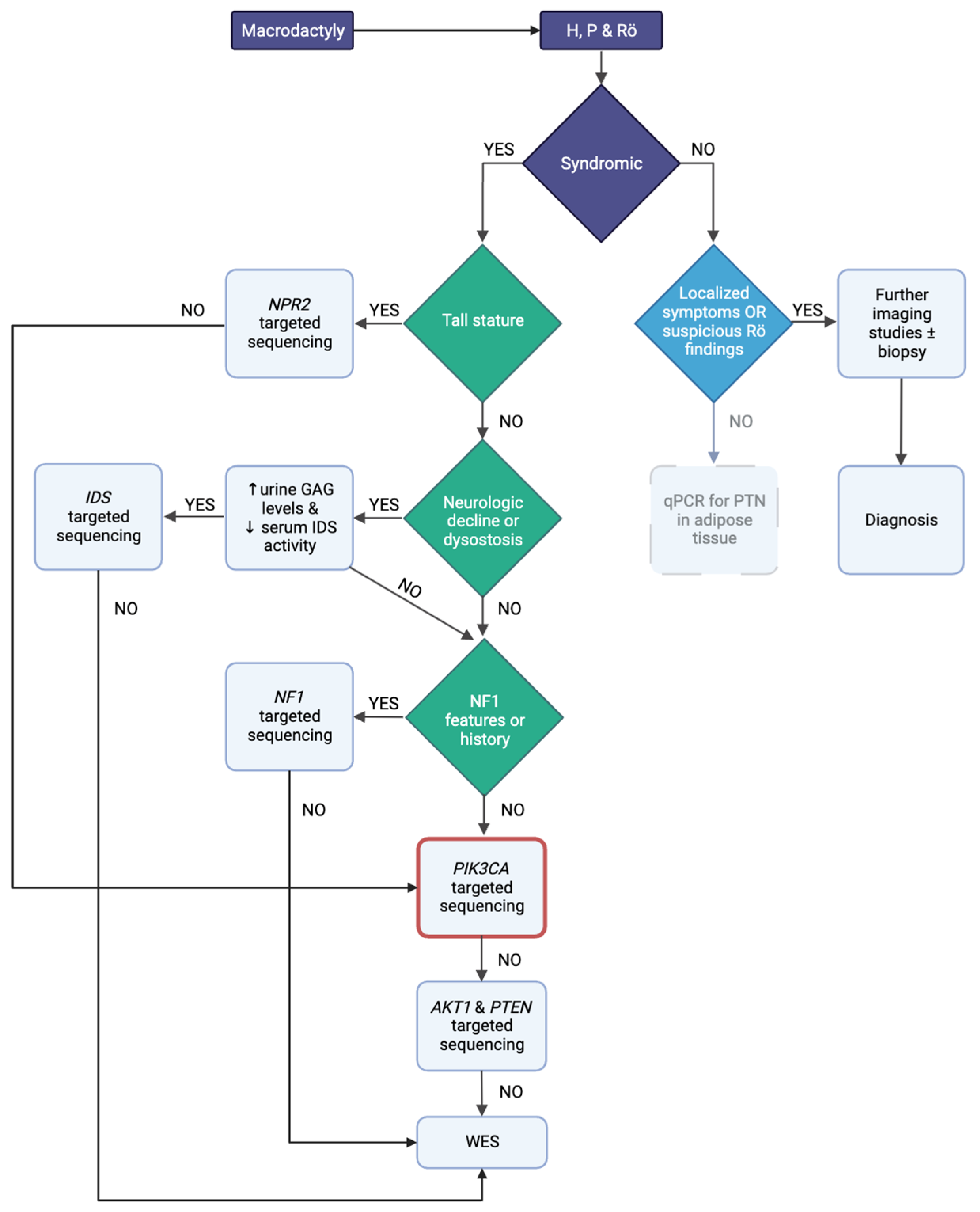
Approach to Macrodactyly: A Case Report and Diagnostic Algorithm for Syndromic and Isolated Forms
Abstract
1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, J.-F.; Tian, G.-L.; Pan, H.; Zhang, W.-T.; Li, D.-C.; Liu, J.-D.; Zhao, L.; Li, H.-L. An Analysis of the Pathogenic Genes and Mutation Sites of Macrodactyly. Pharmgenomics Pers. Med. 2022, 15, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Giżewska-Kacprzak, K.; Śliwiński, M.; Nicieja, K.; Babiak-Choroszczak, L.; Walaszek, I. Macrodactyly. Children 2024, 11, 753. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.F.; Gasteratos, K.; Spyropoulou, G.-A.; Yin, F.; Rui, Y.J. Congenital Difference of the Hand and Foot: Pediatric Macrodactyly. J. Plast. Reconstr. Aesthet. Surg. 2022, 75, 4054–4062. [Google Scholar] [CrossRef] [PubMed]
- Ezaki, M.; Beckwith, T.; Oishi, S.N. Macrodactyly: Decision-Making and Surgery Timing. J. Hand Surg. Eur. Vol. 2019, 44, 32–42. [Google Scholar] [CrossRef]
- Méneret, A.; Grabli, D.; Depienne, C.; Gaudebout, C.; Picard, F.; Dürr, A.; Lagroua, I.; Bouteiller, D.; Mignot, C.; Doummar, D.; et al. PRRT2 Mutations: A Major Cause of Paroxysmal Kinesigenic Dyskinesia in the European Population. Neurology 2012, 79, 170–174. [Google Scholar] [CrossRef]
- Groffen, A.J.A.; Klapwijk, T.; van Rootselaar, A.-F.; Groen, J.L.; Tijssen, M.A.J. Genetic and Phenotypic Heterogeneity in Sporadic and Familial Forms of Paroxysmal Dyskinesia. J. Neurol. 2013, 260, 93–99. [Google Scholar] [CrossRef]
- Lee, Y.-C.; Lee, M.-J.; Yu, H.-Y.; Chen, C.; Hsu, C.-H.; Lin, K.-P.; Liao, K.-K.; Chang, M.-H.; Liao, Y.-C.; Soong, B.-W. PRRT2 Mutations in Paroxysmal Kinesigenic Dyskinesia with Infantile Convulsions in a Taiwanese Cohort. PLoS ONE 2012, 7, e38543. [Google Scholar] [CrossRef]
- Barber, J.C.K.; Hall, V.; Maloney, V.K.; Huang, S.; Roberts, A.M.; Brady, A.F.; Foulds, N.; Bewes, B.; Volleth, M.; Liehr, T.; et al. 16p11.2–P12.2 Duplication Syndrome; a Genomic Condition Differentiated from Euchromatic Variation of 16p11.2. Eur. J. Hum. Genet. 2013, 21, 182–189. [Google Scholar] [CrossRef][Green Version]
- Firouzabadi, S.G.; Kariminejad, R.; Vameghi, R.; Darvish, H.; Ghaedi, H.; Banihashemi, S.; Firouzkouhi Moghaddam, M.; Jamali, P.; Mofidi Tehrani, H.F.; Dehghani, H.; et al. Copy Number Variants in Patients with Autism and Additional Clinical Features: Report of VIPR2 Duplication and a Novel Microduplication Syndrome. Mol. Neurobiol. 2017, 54, 7019–7027. [Google Scholar] [CrossRef]
- Shinawi, M.; Liu, P.; Kang, S.-H.L.; Shen, J.; Belmont, J.W.; Scott, D.A.; Probst, F.J.; Craigen, W.J.; Graham, B.H.; Pursley, A.; et al. Recurrent Reciprocal 16p11.2 Rearrangements Associated with Global Developmental Delay, Behavioural Problems, Dysmorphism, Epilepsy, and Abnormal Head Size. J. Med. Genet. 2010, 47, 332–341. [Google Scholar] [CrossRef]
- Keppler-Noreuil, K.M.; Rios, J.J.; Parker, V.E.R.; Semple, R.K.; Lindhurst, M.J.; Sapp, J.C.; Alomari, A.; Ezaki, M.; Dobyns, W.; Biesecker, L.G. PIK3CA-Related Overgrowth Spectrum (PROS): Diagnostic and Testing Eligibility Criteria, Differential Diagnosis, and Evaluation. Am. J. Med. Genet. A 2015, 167A, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.L. Smith’s Recognizable Patterns of Human Malformation, 7th ed.; Elsevier/Saunders: Philadelphia, PA, USA, 2013; ISBN 978-1-4557-3811-3. [Google Scholar]
- Kliegman, R. Nelson Textbook of Pediatrics, 21st ed.; Elsevier: Philadelphia, PA, USA, 2020; ISBN 978-0-323-52950-1. [Google Scholar]
- Lau, F.H.; Xia, F.; Kaplan, A.; Cerrato, F.; Greene, A.K.; Taghinia, A.; Cowan, C.A.; Labow, B.I. Expression Analysis of Macrodactyly Identifies Pleiotrophin Upregulation. PLoS ONE 2012, 7, e40423. [Google Scholar] [CrossRef] [PubMed]
- Chen, H. Atlas of Genetic Diagnosis and Counseling, 3rd ed.; Springer: New York, NY, USA, 2017; ISBN 978-1-4939-2400-4. [Google Scholar]
- Lauffer, P.; Boudin, E.; van der Kaay, D.C.M.; Koene, S.; van Haeringen, A.; van Tellingen, V.; Van Hul, W.; Prickett, T.C.R.; Mortier, G.; Espiner, E.A.; et al. Broadening the Spectrum of Loss-of-Function Variants in NPR-C-Related Extreme Tall Stature. J. Endocr. Soc. 2022, 6, bvac019. [Google Scholar] [CrossRef]
- Mohamed, S.; He, Q.Q.; Singh, A.A.; Ferro, V. Mucopolysaccharidosis Type II (Hunter Syndrome): Clinical and Biochemical Aspects of the Disease and Approaches to Its Diagnosis and Treatment. Adv. Carbohydr. Chem. Biochem. 2020, 77, 71–117. [Google Scholar] [CrossRef]
- Bendon, C.L.; Giele, H.P. Macrodactyly in the Setting of a Plexiform Schwannoma in Neurofibromatosis Type 2: Case Report. J. Hand Surg. Am. 2013, 38, 740–744. [Google Scholar] [CrossRef]
- Tian, W.; Huang, Y.; Sun, L.; Guo, Y.; Zhao, S.; Lin, M.; Dong, X.; Zhong, W.; Yin, Y.; Chen, Z.; et al. Phenotypic and Genetic Spectrum of Isolated Macrodactyly: Somatic Mosaicism of PIK3CA and AKT1 Oncogenic Variants. Orphanet J. Rare Dis. 2020, 15, 288. [Google Scholar] [CrossRef]
- Kim, Y.-M.; Lee, Y.; Choi, Y.; Choi, I.H.; Heo, S.H.; Choi, J.M.; Do, H.-S.; Jang, J.-H.; Yum, M.-S.; Yoo, H.-W.; et al. Clinical and Genetic Analyses of Patients with Lateralized Overgrowth. BMC Med. Genom. 2022, 15, 206. [Google Scholar] [CrossRef]
- Rodríguez-Laguna, L.; Davis, K.; Finger, M.; Aubel, D.; Vlamis, R.; Johnson, C. Mapping the PIK3CA-Related Overgrowth Spectrum (PROS) Patient and Caregiver Journey Using a Patient-Centered Approach. Orphanet J. Rare Dis. 2022, 17, 189. [Google Scholar] [CrossRef]
- Biesecker, L.G.; Sapp, J.C. Proteus Syndrome. 2012 Aug 9 [Updated 2023 May 25]. In GeneReviews®; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Amemiya, A., Eds.; University of Washington, Seattle: Seattle, WA, USA, 1993. [Google Scholar]
- Alotibi, R.S.; Sannan, N.S.; AlEissa, M.; Aldriwesh, M.G.; Tuwaijri, A.A.; Akiel, M.A.; Almutairi, M.; Alsamer, A.; Altharawi, N.; Aljawfan, G.; et al. The Diagnostic Yield of CGH and WES in Neurodevelopmental Disorders. Front. Pediatr. 2023, 11, 1133789. [Google Scholar] [CrossRef]
- Manor, J.; Lalani, S.R. Overgrowth Syndromes—Evaluation, Diagnosis, and Management. Front. Pediatr. 2020, 8, 574857. [Google Scholar] [CrossRef]
- Reimann, E.; Kõks, S.; Ho, X.D.; Maasalu, K.; Märtson, A. Whole Exome Sequencing of a Single Osteosarcoma Case--Integrative Analysis with Whole Transcriptome RNA-Seq Data. Hum. Genom. 2014, 8, 20. [Google Scholar] [CrossRef]
- Douzgou, S.; Rawson, M.; Baselga, E.; Danielpour, M.; Faivre, L.; Kashanian, A.; Keppler-Noreuil, K.M.; Kuentz, P.; Mancini, G.M.S.; Maniere, M.-C.; et al. A Standard of Care for Individuals with PIK3CA-Related Disorders: An International Expert Consensus Statement. Clin. Genet. 2022, 101, 32–47. [Google Scholar] [CrossRef] [PubMed]
- Keppler-Noreuil, K.M.; Sapp, J.C.; Lindhurst, M.J.; Parker, V.E.R.; Blumhorst, C.; Darling, T.; Tosi, L.L.; Huson, S.M.; Whitehouse, R.W.; Jakkula, E.; et al. Clinical Delineation and Natural History of the PIK3CA-Related Overgrowth Spectrum. Am. J. Med. Genet. A 2014, 164A, 1713–1733. [Google Scholar] [CrossRef]
- Madsen, R.R.; Vanhaesebroeck, B.; Semple, R.K. Cancer-Associated PIK3CA Mutations in Overgrowth Disorders. Trends Mol. Med. 2018, 24, 856–870. [Google Scholar] [CrossRef] [PubMed]
- Canaud, G.; Lopez Gutierrez, J.C.; Irvine, A.D.; Vabres, P.; Hansford, J.R.; Ankrah, N.; Branle, F.; Papadimitriou, A.; Ridolfi, A.; O’Connell, P.; et al. Alpelisib for Treatment of Patients with PIK3CA-Related Overgrowth Spectrum (PROS). Genet. Med. 2023, 25, 100969. [Google Scholar] [CrossRef]
- Mirzaa, G.; Graham, J.M.; Keppler-Noreuil, K. PIK3CA-Related Overgrowth Spectrum. 2013 Aug 15 [Updated 2023 Apr 6]. In GeneReviews®; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Amemiya, A., Eds.; University of Washington, Seattle: Seattle, WA, USA, 1993. [Google Scholar]

| Phenotype | Gene (Location) | Other Features |
|---|---|---|
| PIK3CA-related overgrowth syndrome (PROS) | PIK3CA (3q26.32) | Including (i) macrodactydy including fibroadipose overgrowth; (ii) CLOVE syndrome; (iii) CLAPO syndrome; (iv) epidermal nevus; (v) seborrheic or benign lichenoid keratosis; (vi) cerebral cavernous malformations 4; (vii) Cowden syndrome 5; (viii) MCAP; (ix) HHML; (x) muscle hemihypertrophy; (xi) facial-infiltrating lipomatosis; and (xii) specific cancers: breast, colorectal, gastric, hepatocellular, non-small-cell lung, and ovarian types. |
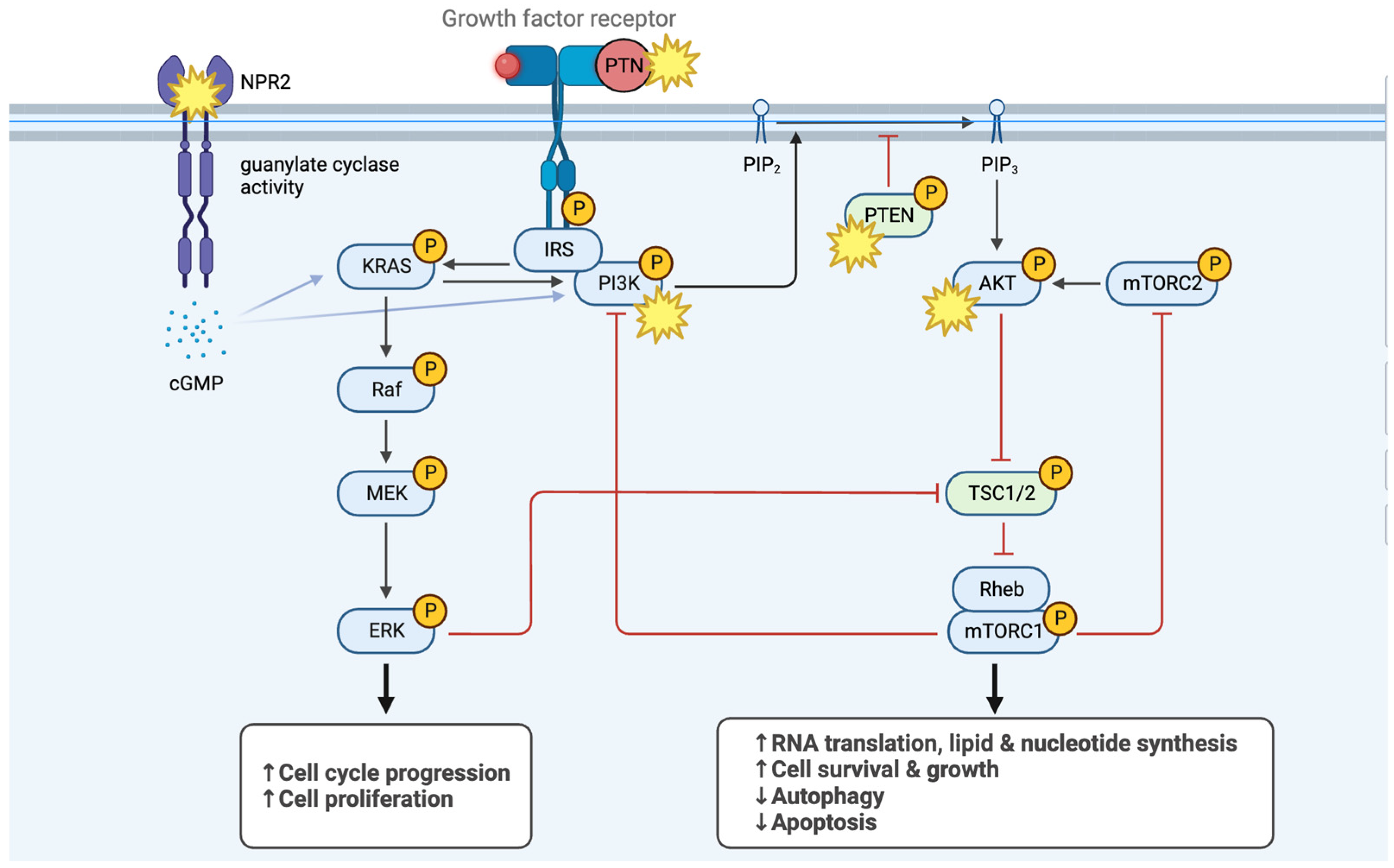
| Non-syndromic macrodactyly | PTN (7q33) | Pleiotrophin upregulation. PTN seems to activate PI3K signaling. |
| Klippel–Trenaunay–Weber syndrome | Diversity in its genetic landscape. Many cases display somatic mosaicism for a missense mutation in PIK3CA | Large cutaneous hemangiomata with hypertrophy of the related bones and soft tissues, venous varicosities, and half of patients with Kasabach–Merritt syndrome |
| Tuberous sclerosis complex (TSC) | TSC1 (9q34.13) or TSC2 (16p13.3) | Autosomal dominant. Cystic areas of bone rarefaction–especially for phalanges |
| Natriuretic Peptide Receptor 2 mutations | NPR2 (9p13.3) | Including epiphyseal chondrodysplasia, Miura type. Macrodactyly is also seen with NPR3 (Boudin–Mortier syndrome) and NPPC (alias CNP) variants. |
| PTEN hamartoma syndromes (with variable expression and age-related penetrance) | PTEN (10q23.31) | Including (i) Cowden syndrome 1: a hamartomatous disorder characterized by macrocephaly, facial trichilemmomas, acral keratoses, papillomatous papules, and an increased risk for the development of breast, thyroid, and endometrial carcinoma; (ii) Bannayan–Riley–Ruvalcaba syndrome: hamartomatous polyps of the gastrointestinal tract, mucocutaneous lesions, developmental delay, macrocephaly, lipomas, hemangiomas, and pigmented speckled macules of the glans penis in males, and an increased risk of developing neoplasms; (iii) Lhermitte–Duclos disease with dysplastic gangliocytoma of the cerebellum; and (iv) Proteus-like syndrome |
| Proteus syndrome | AKT1 (14q32.33) | Partial gigantism of hands and feet, nevi, hemihyperthrophy, and macrocephaly; Elattoproteus syndrome and fibroadipose hyperplasia included |
| Mucopolysaccharidosis type II or Hunter syndrome | IDS region (Xq28) | X-linked recessive inheritance. Patients excrete excessive amounts of chondroitin sulfate B (dermatan sulfate) and heparitin sulfate (heparan sulfate) in the urine. Severe airway obstruction, skeletal deformities, cardiomyopathy, and neurologic decline. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kyriakidis, I.; Pelagiadis, I.; Katzilakis, N.; Stiakaki, E. Approach to Macrodactyly: A Case Report and Diagnostic Algorithm for Syndromic and Isolated Forms. Pediatr. Rep. 2025, 17, 32. https://doi.org/10.3390/pediatric17020032
Kyriakidis I, Pelagiadis I, Katzilakis N, Stiakaki E. Approach to Macrodactyly: A Case Report and Diagnostic Algorithm for Syndromic and Isolated Forms. Pediatric Reports. 2025; 17(2):32. https://doi.org/10.3390/pediatric17020032
Chicago/Turabian StyleKyriakidis, Ioannis, Iordanis Pelagiadis, Nikolaos Katzilakis, and Eftichia Stiakaki. 2025. "Approach to Macrodactyly: A Case Report and Diagnostic Algorithm for Syndromic and Isolated Forms" Pediatric Reports 17, no. 2: 32. https://doi.org/10.3390/pediatric17020032
APA StyleKyriakidis, I., Pelagiadis, I., Katzilakis, N., & Stiakaki, E. (2025). Approach to Macrodactyly: A Case Report and Diagnostic Algorithm for Syndromic and Isolated Forms. Pediatric Reports, 17(2), 32. https://doi.org/10.3390/pediatric17020032







