An Evaluation of Whether Routine QTc Interval Screening Is Necessary Prior to Starting ADHD Medications: Experience from a Large Retrospective Study
Abstract
1. Introduction
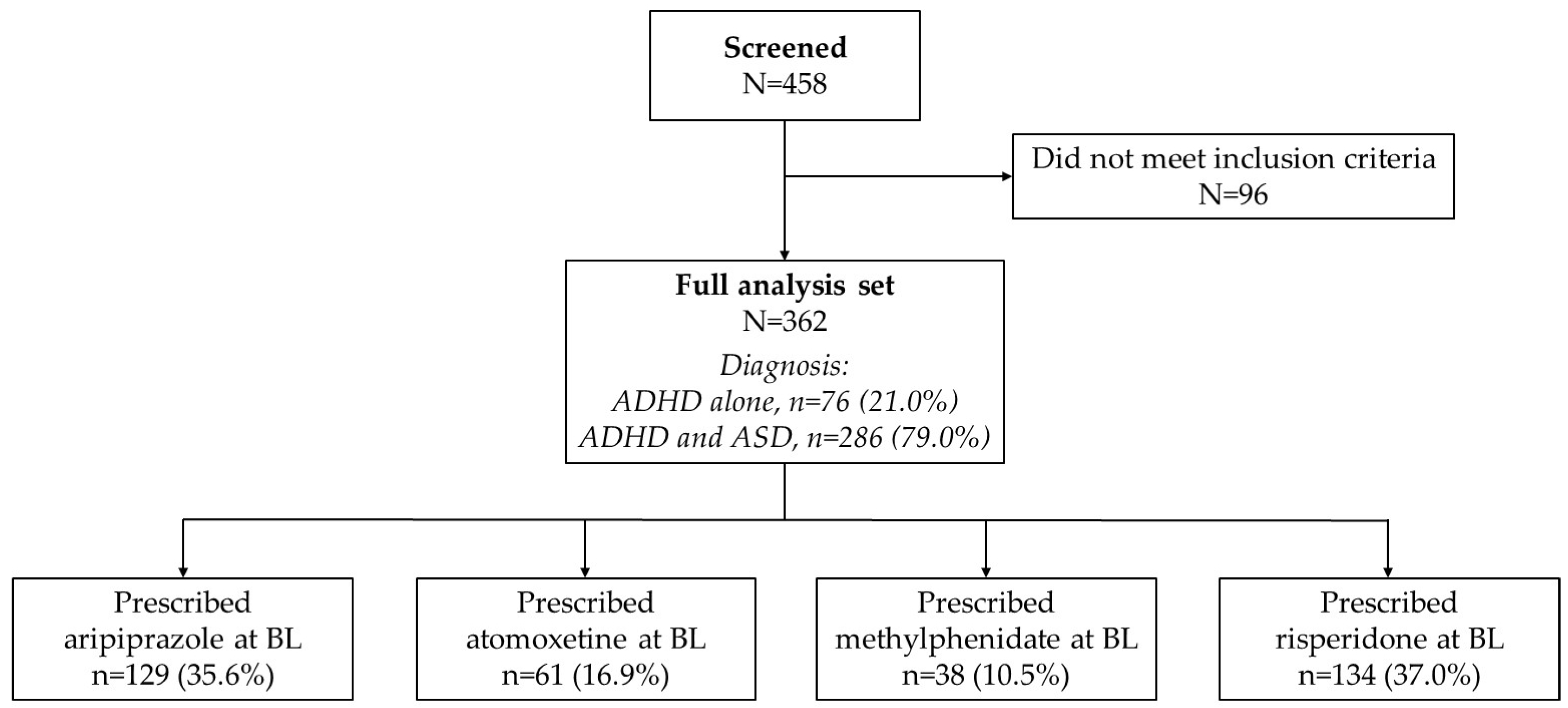
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Salari, N.; Ghasemi, H.; Abdoli, N.; Rahmani, A.; Shiri, M.H.; Hashemian, A.H.; Akbari, H.; Mohammadi, M. The global prevalence of ADHD in children and adolescents: A systematic review and meta-analysis. Ital. J. Pediatr. 2023, 49, 48. [Google Scholar] [CrossRef] [PubMed]
- Abdelnour, E.; Jansen, M.O.; Gold, J.A. ADHD diagnostic trends: Increased recognition or overdiagnosis? Mo. Med. 2022, 119, 467–473. [Google Scholar] [PubMed]
- Kazda, L.; Bell, K.; Thomas, R.; McGeechan, K.; Sims, R.; Barratt, A. Overdiagnosis of attention-deficit/hyperactivity disorder in children and adolescents: A systematic scoping review. JAMA Netw. Open 2021, 4, e215335. [Google Scholar] [CrossRef] [PubMed]
- Morrato, E.H.; Ling, S.B. The Drug Safety and Risk Management Advisory Committee: A case study of meeting frequency, content, and outcomes before and after FDAAA. Med. Care 2012, 50, 970–986. [Google Scholar] [CrossRef] [PubMed]
- Perrin, J.M.; Friedman, R.A.; Knilans, T.K.; Black Box Working Group; Section on Cardiology and Cardiac Surgery. Cardiovascular monitoring and stimulant drugs for attention-deficit/hyperactivity disorder. Pediatrics 2008, 122, 451–453. [Google Scholar] [CrossRef]
- Vetter, V.L.; Elia, J.; Erickson, C.; Berger, S.; Blum, N.; Uzark, K.; Webb, C.L.; American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee; American Heart Association Council on Cardiovascular Nursing. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder [corrected]: A scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation 2008, 117, 2407–2423, Erratum in: Circulation 2009, 120, e55–e59. [Google Scholar] [CrossRef]
- Berger, S. Attention deficit hyperactivity disorder medications in children with heart disease. Curr. Opin. Pediatr. 2016, 28, 607–612. [Google Scholar] [CrossRef]
- Zhang, L.; Yao, H.; Li, L.; Du Rietz, E.; Andell, P.; Garcia-Argibay, M.; D’Onofrio, B.M.; Cortese, S.; Larsson, H.; Chang, Z. Risk of cardiovascular diseases associated with medications used in attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. JAMA Netw. Open 2022, 5, e2243597. [Google Scholar] [CrossRef]
- Hammerness, P.; Berger, A.; Angelini, M.C.; Wilens, T.E. Cardiovascular considerations for stimulant class medications. Child Adolesc. Psychiatr. Clin. N. Am. 2022, 31, 437–448. [Google Scholar] [CrossRef]
- Warren, A.E.; Hamilton, R.M.; Bélanger, S.A.; Gray, C.; Gow, R.M.; Sanatani, S.; Côté, J.M.; Lougheed, J.; LeBlanc, J.; Martin, S.; et al. Cardiac risk assessment before the use of stimulant medications in children and youth: A joint position statement by the Canadian Paediatric Society, the Canadian Cardiovascular Society, and the Canadian Academy of Child and Adolescent Psychiatry. Can. J. Cardiol. 2009, 25, 625–630. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Bazett, H.C. An analysis of the time-relations of electrocardiograms. Heart 1920, 7, 353–370. [Google Scholar] [CrossRef]
- Goldenberg, I.; Moss, A.J.; Zareba, W. QT interval: How to measure it and what is “normal”. J. Cardiovasc. Electrophysiol. 2006, 17, 333–336. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Kutyifa, V.; Moss, A.J.; McNitt, S.; Zareba, W.; Kaufman, E.S. Long-QT syndrome and therapy for attention deficit/hyperactivity disorder. J. Cardiovasc. Electrophysiol. 2015, 26, 1039–1044. [Google Scholar] [CrossRef] [PubMed]
- Seethala, S.; Shusterman, V.; Saba, S.; Mularski, S.; Němec, J. Effect of β-adrenergic stimulation on QT interval accommodation. Heart Rhythm. 2011, 8, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Houghton, R.; de Vries, F.; Loss, G. Psychostimulants/atomoxetine and serious cardiovascular events in children with ADHD or autism spectrum disorder. CNS Drugs 2020, 34, 93–101. [Google Scholar] [CrossRef]
- Hennissen, L.; Bakker, M.J.; Banaschewski, T.; Carucci, S.; Coghill, D.; Danckaerts, M.; Dittmann, R.W.; Hollis, C.; Kovshoff, H.; McCarthy, S.; et al. Cardiovascular effects of stimulant and non-stimulant medication for children and adolescents with ADHD: A systematic review and meta-analysis of trials of methylphenidate, amphetamines and atomoxetine. CNS Drugs 2017, 31, 199–215. [Google Scholar] [CrossRef]
- Hammerness, P.G.; Perrin, J.M.; Shelley-Abrahamson, R.; Wilens, T.E. Cardiovascular risk of stimulant treatment in pediatric attention-deficit/hyperactivity disorder: Update and clinical recommendations. J. Am. Acad. Child Adolesc. Psychiatry 2011, 50, 978–990. [Google Scholar] [CrossRef]
- Winterstein, A.G.; Gerhard, T.; Shuster, J.; Johnson, M.; Zito, J.M.; Saidi, A. Cardiac safety of central nervous system stimulants in children and adolescents with attention-deficit/hyperactivity disorder. Pediatrics 2007, 120, e1494–e1501. [Google Scholar] [CrossRef]
- Winterstein, A.G.; Gerhard, T.; Kubilis, P.; Saidi, A.; Linden, S.; Crystal, S.; Zito, J.; Shuster, J.J.; Olfson, M. Cardiovascular safety of central nervous system stimulants in children and adolescents: Population based cohort study. BMJ 2012, 345, e4627. [Google Scholar] [CrossRef]
- Faraone, S.V. Stimulant therapy in the management of ADHD: Mixed amphetamine salts (extended release). Expert. Opin. Pharmacother. 2007, 8, 2127–2134. [Google Scholar] [CrossRef]
- Reed, V.A.; Buitelaar, J.K.; Anand, E.; Day, K.A.; Treuer, T.; Upadhyaya, H.P.; Coghill, D.R.; Kryzhanovskaya, L.A.; Savill, N.C. The safety of atomoxetine for the treatment of children and adolescents with attention-deficit/hyperactivity disorder: A comprehensive review of over a decade of research. CNS Drugs 2016, 30, 603–628. [Google Scholar] [CrossRef] [PubMed]
- Savill, N.C.; Buitelaar, J.K.; Anand, E.; Day, K.A.; Treuer, T.; Upadhyaya, H.P.; Coghill, D. The efficacy of atomoxetine for the treatment of children and adolescents with attention-deficit/hyperactivity disorder: A comprehensive review of over a decade of clinical research. CNS Drugs 2015, 29, 131–151. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, K.R.; Leikauf, J.E.; Tsang, T.W.; Clarke, S.; Hermens, D.F.; Efron, D.; Williams, L.M.; Kohn, M.R. Response inhibition and emotional cognition improved by atomoxetine in children and adolescents with ADHD: The ACTION randomized controlled trial. J. Psychiatr. Res. 2018, 102, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Pozzi, M.; Carnovale, C.; Mazhar, F.; Peeters, G.G.A.M.; Gentili, M.; Nobile, M.; Radice, S.; Clementi, E. Adverse drug reactions related to mood and emotion in pediatric patients treated for attention deficit/hyperactivity disorder: A comparative analysis of the US Food and Drug Administration Adverse Event Reporting System Database. J. Clin. Psychopharmacol. 2019, 39, 386–392. [Google Scholar] [CrossRef]
- Chen, Q.; Sjölander, A.; Runeson, B.; D’Onofrio, B.M.; Lichtenstein, P.; Larsson, H. Drug treatment for attention-deficit/hyperactivity disorder and suicidal behaviour: Register based study. BMJ (Clin. Res. Ed.) 2014, 348, g3769. [Google Scholar] [CrossRef]
- Linden, S.; Bussing, R.; Kubilis, P.; Gerhard, T.; Segal, R.; Shuster, J.J.; Winterstein, A.G. Risk of suicidal events with atomoxetine compared to stimulant treatment: A cohort study. Pediatrics 2016, 137, e20153199. [Google Scholar] [CrossRef]
- Shoval, G.; Visoki, E.; Moore, T.M.; DiDomenico, G.E.; Argabright, S.T.; Huffnagle, N.J.; Alexander-Bloch, A.F.; Waller, R.; Keele, L.; Benton, T.D.; et al. Evaluation of attention-deficit/hyperactivity disorder medications, externalizing symptoms, and suicidality in children. JAMA Netw. Open. 2021, 4, e2111342. [Google Scholar] [CrossRef]
- Huang, K.L.; Wei, H.T.; Hsu, J.W.; Bai, Y.M.; Su, T.P.; Li, C.T.; Lin, W.C.; Tsai, S.J.; Chang, W.H.; Chen, T.J.; et al. Risk of suicide attempts in adolescents and young adults with attention-deficit hyperactivity disorder: A nationwide longitudinal study. Br. J. Psychiatry 2018, 212, 234–238. [Google Scholar] [CrossRef]
- Dodd, M.L.; Dolenc, T.J.; Karpyak, V.M.; Rasmussen, K.G. QTc dispersion in patients referred for electroconvulsive therapy. J. ECT 2008, 24, 131–133. [Google Scholar] [CrossRef]
- Germanò, E.; Italiano, D.; Lamberti, M.; Guerriero, L.; Privitera, C.; D’Amico, G.; Siracusano, R.; Ingrassia, M.; Spina, E.; Calabrò, M.P.; et al. ECG parameters in children and adolescents treated with aripiprazole and risperidone. Prog. Neuropsychopharmacol. Biol. Psychiatry 2014, 51, 23–27. [Google Scholar] [CrossRef]
- Palanca-Maresca, I.; Ruiz-Antorán, B.; Centeno-Soto, G.A.; Forti-Buratti, M.A.; Siles, A.; Usano, A.; Avendaño-Solá, C. Prevalence and risk factors of prolonged corrected QT interval among children and adolescents treated with antipsychotic medications: A long-term follow-up in a real-world population. J. Clin. Psychopharmacol. 2017, 37, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Hommers, L.; Scherf-Clavel, M.; Stempel, R.; Roth, J.; Falter, M.; Deckert, J.; Mattheisen, M.; Unterecker, S.; Gawlik, M. Antipsychotics in routine treatment are minor contributors to QT prolongation compared to genetics and age. J. Psychopharmacol. 2021, 35, 1127–1133. [Google Scholar] [CrossRef] [PubMed]
- Leslie, L.K.; Alexander, M.E.; Trikalinos, T.A.; Cohen, J.T.; Parsons, S.K.; Newburger, J.W. Reexamining the emperor’s new clothes: Ambiguities in current cardiac screening recommendations for youth with attention deficit hyperactivity disorder. Circ. Cardiovasc. Qual. Outcomes 2008, 1, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Mahle, W.T.; Hebson, C.; Strieper, M.J. Electrocardiographic screening in children with attention-deficit hyperactivity disorder. Am. J. Cardiol. 2009, 104, 1296–1299. [Google Scholar] [CrossRef] [PubMed]
- Leslie, L.K.; Rodday, A.M.; Saunders, T.S.; Cohen, J.T.; Wong, J.B.; Parsons, S.K. Cardiac screening prior to stimulant treatment of ADHD: A survey of US-based pediatricians. Pediatrics 2012, 129, 222–230. [Google Scholar] [CrossRef]
- Brown, J.J.; Gray, J.M.; Roback, M.G.; Sethuraman, U.; Farooqi, A.; Kannikeswaran, N. Procedural sedation in children with autism spectrum disorders in the emergency department. Am. J. Emerg. Med. 2019, 37, 1404–1408. [Google Scholar] [CrossRef]
- Davico, C.; Marcotulli, D.; Succi, E.; Canavese, C.; Bodea, A.F.; Pellegrino, M.; Cuffari, E.; Cudia, V.F.; Svevi, B.; Amianto, F.; et al. Working with children with autism undergoing health-care assessments in a day hospital setting: A perspective from the health-care professionals. Children 2023, 10, 476. [Google Scholar] [CrossRef]
| Baseline Demographic and Disease Characteristics | Full Analysis Set (N = 362) |
|---|---|
| Sex, n (%) | |
| Male | 268 (74.0) |
| Female | 94 (26.0) |
| Age, years | |
| Mean ± SD | 6.4 ± 3.5 |
| Median | 6.0 |
| QTc interval, ms | |
| Mean ± SD | 400 ± 22 |
| Median | 400 |
| Min, max | 341, 465 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsayouf, H.A.; Dyab, L.M.; Al-Ghawanmeh, R.; Alhawawsha, L.S.; Alsarhan, O.; Al-Smadi, H.; Al-Taani, G.M.; Daoud, A.; Elsadek, H.E.; Khreisat, W.H. An Evaluation of Whether Routine QTc Interval Screening Is Necessary Prior to Starting ADHD Medications: Experience from a Large Retrospective Study. Pediatr. Rep. 2024, 16, 1161-1168. https://doi.org/10.3390/pediatric16040098
Alsayouf HA, Dyab LM, Al-Ghawanmeh R, Alhawawsha LS, Alsarhan O, Al-Smadi H, Al-Taani GM, Daoud A, Elsadek HE, Khreisat WH. An Evaluation of Whether Routine QTc Interval Screening Is Necessary Prior to Starting ADHD Medications: Experience from a Large Retrospective Study. Pediatric Reports. 2024; 16(4):1161-1168. https://doi.org/10.3390/pediatric16040098
Chicago/Turabian StyleAlsayouf, Hamza A., Lima M. Dyab, Redab Al-Ghawanmeh, Luay S. Alhawawsha, Osama Alsarhan, Hadeel Al-Smadi, Ghaith M. Al-Taani, Azhar Daoud, Haitham E. Elsadek, and Wael H. Khreisat. 2024. "An Evaluation of Whether Routine QTc Interval Screening Is Necessary Prior to Starting ADHD Medications: Experience from a Large Retrospective Study" Pediatric Reports 16, no. 4: 1161-1168. https://doi.org/10.3390/pediatric16040098
APA StyleAlsayouf, H. A., Dyab, L. M., Al-Ghawanmeh, R., Alhawawsha, L. S., Alsarhan, O., Al-Smadi, H., Al-Taani, G. M., Daoud, A., Elsadek, H. E., & Khreisat, W. H. (2024). An Evaluation of Whether Routine QTc Interval Screening Is Necessary Prior to Starting ADHD Medications: Experience from a Large Retrospective Study. Pediatric Reports, 16(4), 1161-1168. https://doi.org/10.3390/pediatric16040098






