Postoperative Osteopathic Manipulative Treatment in Children with Esophageal Atresia: Potential Benefits on the Anthropometric Parameters
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Clinical Findings and Diagnostic Assessment
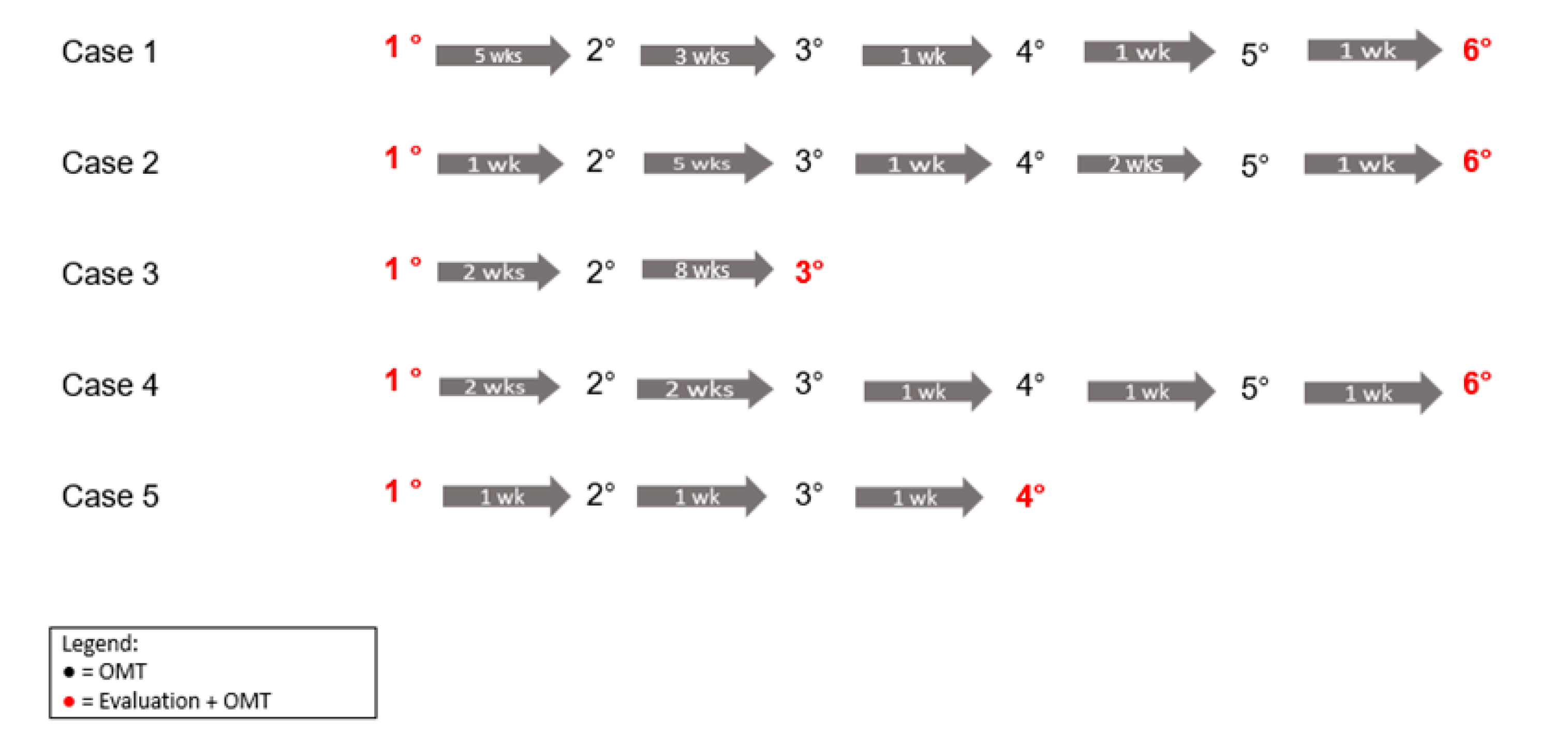
2.3. Therapeutic Intervention
3. Results
3.1. Patient Data
3.1.1. Case 1
3.1.2. Case 2
3.1.3. Case 3
3.1.4. Case 4
3.1.5. Case 5
Technique
Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smith, N. Oesophageal Atresia and Tracheo-Oesophageal Fistula. Early Hum. Dev. 2014, 90, 947–950. [Google Scholar] [CrossRef] [PubMed]
- van Lennep, M.; Singendonk, M.M.J.; Dall’Oglio, L.; Gottrand, F.; Krishnan, U.; Terheggen-Lagro, S.W.J.; Omari, T.I.; Benninga, M.A.; van Wijk, M.P. Oesophageal Atresia. Nat. Rev. Dis. Primer 2019, 5, 26. [Google Scholar] [CrossRef] [PubMed]
- Askarpour, S.; Peyvasteh, M.; Ashrafi, A.; Dehdashtian, M.; Malekian, A.; Aramesh, M.-R. Muscle-Sparing Versus Standard Posterolateral Thoracotomy in Neonates with Esophageal Atresia. ABCD Arq. Bras. Cir. Dig. 2018, 31, e1365. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, A.; Sowande, O.; Alizai, N.K.; Rampersad, B. Aesthetics and Lateral Thoracotomy in the Neonate. J. Pediatr. Surg. 1998, 33, 1798–1800. [Google Scholar] [CrossRef]
- Zhang, J.; Wu, Q.; Chen, L.; Wang, Y.; Cui, X.; Huang, W.; Zhou, C. Clinical Analysis of Surgery for Type III Esophageal Atresia via Thoracoscopy: A Study of a Chinese Single-Center Experience. J. Cardiothorac. Surg. 2020, 15, 55. [Google Scholar] [CrossRef] [PubMed]
- Parravicini, G.; Bergna, A. Biological Effects of Direct and Indirect Manipulation of the Fascial System. Narrative Review. J. Bodyw. Mov. Ther. 2017, 21, 435–445. [Google Scholar] [CrossRef] [PubMed]
- Pavan, P.G.; Stecco, A.; Stern, R.; Stecco, C. Painful Connections: Densification versus Fibrosis of Fascia. Curr. Pain Headache Rep. 2014, 18, 441. [Google Scholar] [CrossRef]
- Manzotti, A.; Cerritelli, F.; Chiera, M.; Lombardi, E.; La Rocca, S.; Biasi, P.; Galli, M.; Esteves, J.; Lista, G. Neonatal Assessment Manual Score: Is There a Role of a Novel, Structured Touch-Based Evaluation in Neonatal Intensive Care Unit? Front. Pediatr. 2020, 8, 432. [Google Scholar] [CrossRef]
- McGlone, F.; Cerritelli, F.; Walker, S.; Esteves, J. The Role of Gentle Touch in Perinatal Osteopathic Manual Therapy. Neurosci. Biobehav. Rev. 2017, 72, 1–9. [Google Scholar] [CrossRef]
- WHO. Benchmarks for Training in Traditional/Compementary and Alternative Medicine: Benchmarks for Training in Osteopathy; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Degenhardt, B.F.; Johnson, J.C.; Fossum, C.; Andicochea, C.T.; Stuart, M.K. Changes in Cytokines, Sensory Tests, and Self-Reported Pain Levels After Manual Treatment of Low Back Pain. Clin. Spine Surg. Spine Publ. 2017, 30, E690–E701. [Google Scholar] [CrossRef]
- Licciardone, J.C.; Kearns, C.M.; Hodge, L.M.; Bergamini, M.V.W. Associations of Cytokine Concentrations With Key Osteopathic Lesions and Clinical Outcomes in Patients With Nonspecific Chronic Low Back Pain: Results From the OSTEOPATHIC Trial. J. Am. Osteopath. Assoc. 2012, 112, 596. [Google Scholar] [CrossRef] [PubMed]
- Tozzi, P. Selected Fascial Aspects of Osteopathic Practice. J. Bodyw. Mov. Ther. 2012, 16, 503–519. [Google Scholar] [CrossRef] [PubMed]
- Chaitow, L. What’s in a Name: Myofascial Release or Myofascial Induction? J. Bodyw. Mov. Ther. 2017, 21, 749–751. [Google Scholar] [CrossRef]
- Serra-Añó, P.; Inglés, M.; Bou-Catalá, C.; Iraola-Lliso, A.; Espí-López, G.V. Effectiveness of Myofascial Release after Breast Cancer Surgery in Women Undergoing Conservative Surgery and Radiotherapy: A Randomized Controlled Trial. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2019, 27, 2633–2641. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, G.; Cerritelli, F.; Cortelli, P. Sensitization and Interoception as Key Neurological Concepts in Osteopathy and Other Manual Medicines. Front. Neurosci. 2016, 10, 100. [Google Scholar] [CrossRef]
- Manzotti, A.; Cerritelli, F.; Lombardi, E.; La Rocca, S.; Chiera, M.; Galli, M.; Lista, G. Effects of Osteopathic Treatment versus Static Touch on Heart Rate and Oxygen Saturation in Premature Babies: A Randomized Controlled Trial. Complement. Ther. Clin. Pract. 2020, 39, 101116. [Google Scholar] [CrossRef] [PubMed]
- Cerritelli, F.; Chiacchiaretta, P.; Gambi, F.; Perrucci, M.G.; Barassi, G.; Visciano, C.; Bellomo, R.G.; Saggini, R.; Ferretti, A. Effect of Manual Approaches with Osteopathic Modality on Brain Correlates of Interoception: An FMRI Study. Sci. Rep. 2020, 10, 3214. [Google Scholar] [CrossRef] [PubMed]
- Cerritelli, F.; Chiacchiaretta, P.; Gambi, F.; Saggini, R.; Perrucci, M.G.; Ferretti, A. Osteopathy Modulates Brain–Heart Interaction in Chronic Pain Patients: An ASL Study. Sci. Rep. 2021, 11, 4556. [Google Scholar] [CrossRef] [PubMed]
- Grunau, R.E.; Holsti, L.; Peters, J.W.B. Long-Term Consequences of Pain in Human Neonates. Semin. Fetal. Neonatal Med. 2006, 11, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Tezza, G.; Paiola, G.; Zoccante, L.; Gandolfi, M.; Smania, N.; Ciceri, M.L.; Boner, A.; Piacentini, G.; Banzato, C. Gut-Brain Axis Exploration: Stabilometric Platform Performances in Children Affected by Functional Gastrointestinal Disorders. J. Pediatr. Gastroenterol. Nutr. 2021, 72, 347–353. [Google Scholar] [CrossRef]
- Walker, K.; Holland, A.J.; Winlaw, D.; Sherwood, M.; Badawi, N. Neurodevelopmental Outcomes and Surgery in Neonates. J. Paediatr. Child Health 2006, 42, 749–751. [Google Scholar] [CrossRef] [PubMed]
- Barni, A.; Zecchillo, D.; Uberti, S.; Ratti, S. Osteopathic Manipulative Treatment in a Paediatric Patient with Oesophageal Atresia and Tracheo-Oesophageal Fistula. Case Rep. Gastroenterol. 2019, 13, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Posadzki, P.; Lee, M.S.; Ernst, E. Osteopathic Manipulative Treatment for Pediatric Conditions: A Systematic Review. Pediatrics 2013, 132, 140–152. [Google Scholar] [CrossRef] [PubMed]
- Bergna, A.; Vismara, L.; Parravicini, G.; Dal Farra, F. A New Perspective for Somatic Dysfunction in Osteopathy: The Variability Model. J. Bodyw. Mov. Ther. 2020, 24, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Licciardone, J.C.; Kearns, C.M.; Hodge, L.M.; Minotti, D.E. Osteopathic Manual Treatment in Patients with Diabetes Mellitus and Comorbid Chronic Low Back Pain: Subgroup Results from the OSTEOPATHIC Trial. J. Am. Osteopath. Assoc. 2013, 113, 468–478. [Google Scholar]
- American Association of Colleges of Osteopathic Medicine (AACOM). Glossary of Osteopathic Terminology; AACOM: Chevy Chase, MD, USA, 2017. [Google Scholar]
- Cerritelli, F.; Martelli, M.; Renzetti, C.; Pizzolorusso, G.; Cozzolino, V.; Barlafante, G. Introducing an Osteopathic Approach into Neonatology Ward: The NE-O Model. Chiropr. Man. Ther. 2014, 22, 18. [Google Scholar] [CrossRef][Green Version]
- Pizzolorusso, G.; Cerritelli, F.; D’Orazio, M.; Cozzolino, V.; Turi, P.; Renzetti, C.; Barlafante, G.; D’Incecco, C. Osteopathic Evaluation of Somatic Dysfunction and Craniosacral Strain Pattern among Preterm and Term Newborns. J. Am. Osteopath. Assoc. 2013, 113, 462–467. [Google Scholar]
- Cerritelli, F.; Cardone, D.; Pirino, A.; Merla, A.; Scoppa, F. Does Osteopathic Manipulative Treatment Induce Autonomic Changes in Healthy Participants? A Thermal Imaging Study. Front. Neurosci. 2020, 14, 887. [Google Scholar] [CrossRef]
- Ben Ari, A.; Margalit, D.; Udassin, R.; Benarroch, F. Traumatic Stress among School-Aged Pediatric Surgery Patients and Their Parents. Eur. J. Pediatr. Surg. Off. J. Austrian Assoc. Pediatr. Surg. Al Z. Kinderchir. 2019, 29, 437–442. [Google Scholar] [CrossRef]
- Bastard, F.; Bonnard, A.; Rousseau, V.; Gelas, T.; Michaud, L.; Irtan, S.; Piolat, C.; Ranke-Chrétien, A.; Becmeur, F.; Dariel, A.; et al. Thoracic Skeletal Anomalies Following Surgical Treatment of Esophageal Atresia. Lessons from a National Cohort. J. Pediatr. Surg. 2018, 53, 605–609. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, H.; Tazuke, Y.; Uenoa, T.; Yamanaka, H.; Takama, Y.; Saka, R.; Nara, K.; Usui, N. Long-Term Morbidity in Adolescents and Young Adults with Surgically Treated Esophageal Atresia. Surg. Today 2017, 47, 872–876. [Google Scholar] [CrossRef] [PubMed]
- Sposato, N.S.; Bjerså, K. Osteopathic Manipulative Treatment in Surgical Care: Short Review of Research Publications in Osteopathic Journals During the Period 1990 to 2017. J. Evid.-Based Integr. Med. 2018, 23, 2515690X18767671. [Google Scholar] [CrossRef] [PubMed]
- Birketvedt, K.; Mikkelsen, A.; Klingen, L.L.; Henriksen, C.; Helland, I.B.; Emblem, R. Nutritional Status in Adolescents with Esophageal Atresia. J. Pediatr. 2020, 218, 130–137. [Google Scholar] [CrossRef]
- Frongillo, E.A.; Leroy, J.L.; Lapping, K. Appropriate Use of Linear Growth Measures to Assess Impact of Interventions on Child Development and Catch-Up Growth. Adv. Nutr. 2019, 10, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Weber, D.R.; Moore, R.H.; Leonard, M.B.; Zemel, B.S. Fat and Lean BMI Reference Curves in Children and Adolescents and Their Utility in Identifying Excess Adiposity Compared with BMI and Percentage Body Fat. Am. J. Clin. Nutr. 2013, 98, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Pervanidou, P.; Makris, G.; Chrousos, G.; Agorastos, A. Early Life Stress and Pediatric Posttraumatic Stress Disorder. Brain Sci. 2020, 10, 169. [Google Scholar] [CrossRef]
- Henley, C.E.; Ivins, D.; Mills, M.; Wen, F.K.; Benjamin, B.A. Osteopathic Manipulative Treatment and Its Relationship to Autonomic Nervous System Activity as Demonstrated by Heart Rate Variability: A Repeated Measures Study. Osteopath. Med. Prim. Care 2008, 2, 7. [Google Scholar] [CrossRef]
- Ruffini, N.; D’Alessandro, G.; Mariani, N.; Pollastrelli, A.; Cardinali, L.; Cerritelli, F. Variations of High Frequency Parameter of Heart Rate Variability Following Osteopathic Manipulative Treatment in Healthy Subjects Compared to Control Group and Sham Therapy: Randomized Controlled Trial. Front. Neurosci. 2015, 9, 272. [Google Scholar] [CrossRef]
- Nuño, V.; Siu, A.; Deol, N.; Juster, R.-P. Osteopathic Manipulative Treatment for Allostatic Load Lowering. J. Am. Osteopath. Assoc. 2019, 119, 646–654. [Google Scholar] [CrossRef]
- Midwood, K.S.; Williams, L.V.; Schwarzbauer, J.E. Tissue Repair and the Dynamics of the Extracellular Matrix. Int. J. Biochem. Cell Biol. 2004, 36, 1031–1037. [Google Scholar] [CrossRef]
- Lunghi, C.; Consorti, G.; Tramontano, M.; Esteves, J.E.; Cerritelli, F. Perspectives on Tissue Adaptation Related to Allostatic Load: Scoping Review and Integrative Hypothesis with a Focus on Osteopathic Palpation. J. Bodyw. Mov. Ther. 2020, 24, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Abu-Zidan, F.M.; Abbas, A.K.; Hefny, A.F. Clinical “case series”: A concept analysis. Afr. Health Sci. 2012, 12, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Storm, J.M.; Wolman, R.; Bakker, E.; Wyon, M.A. The Relationship Between Range of Motion and Injuries in Adolescent Dancers and Sportspersons: A Systematic Review. Front. Psychol. 2018, 9, 287. [Google Scholar] [CrossRef] [PubMed]
- Ballaz, L.; Plamondon, S.; Lemay, M. Ankle range of motion is key to gait efficiency in adolescents with cerebral palsy. Clin. Biomech. Bristol. Avon. 2010, 25, 944–948. [Google Scholar] [CrossRef] [PubMed]
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age (yrs) | 5 | 5 | 3 | 3 | 7 | |||||
| Parameter | ||||||||||
| Pre and post treatment | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post |
| Height (cm) | 106 | 109.5 | 99 | 102 | 86 | 86 | 90 | 93 | 115.5 | 117.5 |
| Weight (kg) | 18 | 17 | 14.5 | 14.7 | 10.5 | 10 | 12 | 12.8 | 22.2 | 22 |
| BMI | 16.02 | 14.31 | 14.75 | 13.46 | 13.52 | 13.52 | 14.81 | 13.87 | 16.64 | 16.07 |
| Right shoulder elevation ROM (°) | 165° | 171° | 158° | 158° | 137° | 158° | 164° | 167° | 150° | 160° |
| Linear measure of growth (height, percentile) | 10th | 25th | −2 SD to st. pop. | 10th | 5th | 5th | 5th | 5th | 10th | 25th |
| Z-score BMI | 0.48 | −1.21 | −0.29 | −0.92 | −1.73 | −2.55 | −1.06 | −1.07 | 0.65 | 0.25 |
| Percentile BMI | 68th | 11th | 39th | 18th | 4th | 1st | 14th | 14th | 74th | 60th |
| Z-score Height for age | −0.68 | 0.07 | −1.96 | −1.28 | −2.58 | −2.58 | −1.42 | −0.60 | −1.21 | −0.84 |
| Percentile Height for Age | 25th | 53rd | 2.5th | 10th | 0.5th | 0.5th | 8th | 27th | 11th | 20th |
| Z-score Weight for Age | −0.21 | −0.67 | −1.78 | −1.65 | −3.12 | −3.66 | −1.73 | −1.09 | −0.30 | −0.36 |
| Percentile Weight for Age | 42nd | 25th | 4th | 5th | 0.1st | 0.1st | 4th | 14th | 38th | 36th |
| Case 1 |
|
| Case 2 |
|
| Case 3 |
|
| Case 4 |
|
| Case 5 |
|
| Region Restricted Pre-Treatment Period | Region Restricted Post Treatment Period | |
|---|---|---|
| Case 1 |
|
|
| Case 2 |
|
|
| Case 3 |
|
|
| Case 4 |
|
|
| Case 5 |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manzotti, A.; Alati, A.; Galli, M.; Cerritelli, F.; Leva, C.; Alberti, A.; Stizzoli, A.; Costanzo, S.; Canonica, C.P.M.; Destro, F.; et al. Postoperative Osteopathic Manipulative Treatment in Children with Esophageal Atresia: Potential Benefits on the Anthropometric Parameters. Pediatr. Rep. 2022, 14, 434-443. https://doi.org/10.3390/pediatric14040051
Manzotti A, Alati A, Galli M, Cerritelli F, Leva C, Alberti A, Stizzoli A, Costanzo S, Canonica CPM, Destro F, et al. Postoperative Osteopathic Manipulative Treatment in Children with Esophageal Atresia: Potential Benefits on the Anthropometric Parameters. Pediatric Reports. 2022; 14(4):434-443. https://doi.org/10.3390/pediatric14040051
Chicago/Turabian StyleManzotti, Andrea, Alessia Alati, Matteo Galli, Francesco Cerritelli, Chiara Leva, Adele Alberti, Alessandro Stizzoli, Sara Costanzo, Carlotta Paola Maria Canonica, Francesca Destro, and et al. 2022. "Postoperative Osteopathic Manipulative Treatment in Children with Esophageal Atresia: Potential Benefits on the Anthropometric Parameters" Pediatric Reports 14, no. 4: 434-443. https://doi.org/10.3390/pediatric14040051
APA StyleManzotti, A., Alati, A., Galli, M., Cerritelli, F., Leva, C., Alberti, A., Stizzoli, A., Costanzo, S., Canonica, C. P. M., Destro, F., Zuccotti, G., Calcaterra, V., & Pelizzo, G. (2022). Postoperative Osteopathic Manipulative Treatment in Children with Esophageal Atresia: Potential Benefits on the Anthropometric Parameters. Pediatric Reports, 14(4), 434-443. https://doi.org/10.3390/pediatric14040051










