Neonatal and Pediatric Emergency Room Visits in a Tertiary Center during the COVID-19 Pandemic in Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
3.1. Characteristics of PED Visits in the Two Study Periods
3.2. Distribution of Visits According to Age Group and Disease Category
3.3. Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 28 June 2020).
- Parri, N.; Lenge, M.; Buonsenso, D. Children with Covid-19 in Pediatric Emergency Departments in Italy. N. Engl. J. Med. 2020, 383, 187–190. [Google Scholar] [CrossRef]
- Verdoni, L.; Mazza, A.; Gervasoni, A.; Martelli, L.; Ruggeri, M.; Ciuffreda, M. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: An observational cohort study. Lancet 2020, 395, 1771–1778. [Google Scholar] [CrossRef]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Lynn, R.M.; Avis, J.L.; Lenton, S.; Amin-Chowdhury, Z.; Ladhani, S.N. Delayed access to care and late presentations in children during the COVID-19 pandemic: A snapshot survey of 4075 paediatricians in the UK and Ireland. Arch. Dis. Child. 2021, 106, e8. [Google Scholar] [CrossRef] [PubMed]
- Nourazari, S.; Davis, S.R.; Granovsky, R.; Austin, R.; Straff, D.J.; Joseph, J.W.; Sanchez, L.D. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am. J. Emerg. Med. 2020. [Google Scholar] [CrossRef]
- Scaramuzza, A.; Tagliaferri, F.; Bonetti, L.; Soliani, M.; Morotti, F.; Bellone, S.; Cavalli, C.; Rabbone, I. Changing admission patterns in paediatric emer-gency departments during the COVID-19 pandemic. Arch. Dis. Child. 2020, 105, 704–706. [Google Scholar] [CrossRef]
- Isba, R.; Edge, R.; Jenner, R.; Broughton, E.; Francis, N.; Butler, J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch. Dis. Child. 2020, 105, 704. [Google Scholar] [CrossRef]
- Dann, L.; Fitzsimons, J.; Gorman, K.M.; Hourihane, J.; Okafor, I. Disappearing act: COVID-19 and paediatric emergency department attendances. Arch. Dis. Child. 2020, 105, 810–811. [Google Scholar] [CrossRef] [PubMed]
- Hon, K.L.; Leung, A.K. Childhood accidents: Injuries and poisoning. Adv. Pediatr. 2010, 57, 33–62. [Google Scholar] [CrossRef] [PubMed]
- Pines, J.M.; Zocchi, M.S.; Black, B.S.; Carlson, J.N.; Celedon, P.; Moghtaderi, A.; Venkat, A.; US Acute Care Solutions Research Group. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am. J. Emerg. Med. 2020, 41, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Chong, S.-L.; Soo, J.S.L.; Allen, J.C., Jr.; Ganapathy, S.; Lee, K.P.; Tyebally, A.; Yung, C.F.; Thoon, K.C.; Ng, Y.H.; Oh, J.Y.; et al. Impact of COVID-19 on pediatric emergencies and hospitalizations in Singapore. BMC Pediatr. 2020, 20, 562. [Google Scholar] [CrossRef] [PubMed]
- Angoulvant, F.; Ouldali, N.; Yang, D.D.; Filser, M.; Gajdos, V.; Rybak, A.; Guedj, R.; Soussan-Banini, V.; Basmaci, R.; Lefevre-Utile, A.; et al. Coronavirus Disease 2019 Pandemic: Impact Caused by School Closure and National Lockdown on Pediatric Visits and Admissions for Viral and Nonviral Infections—A Time Series Analysis. Clin. Infect. Dis. 2021, 72, 319–322. [Google Scholar] [CrossRef] [PubMed]
- Auger, K.A.; Shah, S.S.; Richardson, T.; Hartley, D.; Hall, M.; Warniment, A.; Timmons, K.; Bosse, D.; Ferris, S.A.; Brady, P.W.; et al. Association Between Statewide School Closure and COVID-19 Incidence and Mortality in the US. JAMA 2020, 324, 859. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; Principi, N. School Closure during the Coronavirus Disease 2019 (COVID-19) Pandemic. JAMA Pediatr. 2020, 174, 921. [Google Scholar] [CrossRef]
- McDermott, K.W.; Stocks, C.; Freeman, W.J. Overview of Pediatric Emergency Department Visits, 2015, Statistical Brief #242. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2006. [Google Scholar]
- Poropat, F.; Heinz, P.; Barbi, E.; Ventura, A. Comparison of two European paediatric emergency departments: Does primary care organisation influence emergency attendance? Ital. J. Pediatr. 2017, 43, 29. [Google Scholar] [CrossRef][Green Version]
- Armon, K.; Stephenson, T.; Gabriel, V.; MacFaul, R.; Eccleston, P.; Werneke, U.; Smith, S. Determining the common medical presenting problems to an accident and emergency department. Arch. Dis. Child. 2001, 84, 390–392. [Google Scholar] [CrossRef]
- Garazzino, S.; Montagnani, C.; Donà, D.; Meini, A.; Felici, E.; Vergine, G.; Bernardi, S.; Giacchero, R.; Vecchio, A.L.; Marchisio, P.; et al. Multicentre Italian study of SARS-CoV-2 infection in children and adolescents, preliminary data as at 10 April 2020. Eurosurveillance 2020, 25, 2000600. [Google Scholar] [CrossRef]
- De Luca, D.; Rava, L.; Nadel, S.; Tissieres, P.; Gawronski, O.; Perkins, E.; Chidini, G.; Tingay, D.G. The EPICENTRE (ESPNIC Covid pEdiatric Neonatal Registry) initiative: Background and protocol for the international SARS-CoV-2 infections registry. Eur. J. Pediatr. 2020, 179, 1271–1278. [Google Scholar] [CrossRef]
- Castagnoli, R.; Votto, M.; Licari, A.; Brambilla, I.; Raffaele, B.; Perlini, S.; Rovida, F.; Baldanti, F.; Marseglia, G.L. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Children and Adolescents: A Systematic Review. JAMA Pediatr. 2020, 174, 882–889. [Google Scholar] [CrossRef]
- Parri, N.; Magistà, A.M.; Marchetti, F.; Cantoni, B.; Arrighini, A.; Romanengo, M.; Felici, E.; Urbino, A.; Da Dalt, L.; Verdoni, L.; et al. Characteristic of COVID-19 infection in pediatric patients: Early findings from two Italian Pediatric Research Networks. Eur. J. Pediatr. 2020, 179, 1315–1323. [Google Scholar] [CrossRef] [PubMed]
- Cozzi, G.; Minute, M.; Skabar, A.; Pirrone, A.; Jaber, M.; Neri, E.; Montico, M.; Ventura, A.; Barbi, E. Somatic symptom disorder was common in children and ado-lescents attending an emergency department complaining of pain. Acta Paediatr. Int. J. Paediatr. 2017, 106, 586–593. [Google Scholar] [CrossRef]
- Manivannan, M.; Jogalekar, M.P.; Kavitha, M.S.; Maran, B.A.V.; Gangadaran, P. A mini-review on the effects of COVID-19 on younger individuals. Exp. Biol. Med. 2021, 246, 293–297. [Google Scholar] [CrossRef]
- Graciano, A.L.; Bhutta, A.T.; Custer, J.W. Reduction in paediatric intensive care admissions during COVID-19 lockdown in Mar-yland, USA. BMJ Paediatr. Open 2020, 4, e000876. [Google Scholar] [CrossRef]
- De Araujo, O.R.; De Almeida, C.G.; Lima-Setta, F.; Prata-Barbosa, A.; Junior, J.C. The Impact of the Novel Coronavirus on Brazilian PICUs. Pediatr. Crit. Care Med. 2020, 21, 1059–1063. [Google Scholar] [CrossRef]

| 2019 | 2020 | p-Value | |
|---|---|---|---|
| Number of visits, n | 3159 | 1039 | |
| Visits per day, n (SD) | 51.62 (10.4) | 17.03 (6.8) | <0.001 |
| Sex (n, %) | |||
| Female | 1418 (44.9) | 437 (42.1) | 0.11 |
| Male | 1741 (55.1) | 602 (57.9) | 0.11 |
| Age group (n, %) | |||
| <28 d | 78 (2.5) | 59 (5.7) | <0.001 |
| 28 d–1 y | 544 (17.2) | 203 (19.5) | 0.09 |
| 1–3 y | 583 (18.5) | 241 (23.2) | 0.001 |
| 3–6 y | 860 (27.2) | 194 (18.7) | <0.001 |
| 6–10 y | 436 (13.8) | 162 (15.6) | 0.15 |
| 10–14 y | 402 (12.7) | 136 (13.1) | 0.76 |
| ≥14 y | 256 (8.1) | 44 (4.2) | <0.001 |
| Priority tags at triage | |||
| White (n, %) | 1447 (45.8) | 364 (35.0) | <0.001 |
| Green (n, %) | 1450 (45.9) | 574 (55.3) | <0.001 |
| Yellow (n, %) | 261 (8.27) | 100 (9.6) | 0.17 |
| Red (n, %) | 1 (0.03) | 1 (0.1) | 0.41 |
| 2019 | 2020 | p-Value | |
|---|---|---|---|
| Total visits, n | 78 | 59 | |
| Newborns with pathological conditions, n (%) | 34 (43.6) | 11 (18.6) | <0.001 |
| Respiratory infections | 17 (50) | 0 (0) | 0.016 |
| Urinary infections | 2 (5.9) | 0 (0) | 0.71 |
| Aspecific fever | 3 (8.8) | 1 (9.1) | 0.99 |
| Other infections | 7 (20.6) | 3 (27.3) | 0.64 |
| Neurological conditions | 2 (5.9) | 3 (27.3) | 0.08 |
| Others | 3 (8.8) | 4 (36.4) | 0.03 |
| Newborns with minor clinical conditions, n (%) | 44 (56.4) | 48 (81.4) | <0.001 |
| Aspecific crying | 3 (6.8) | 0 (0) | 0.26 |
| Umbilical cord care | 13 (29.5) | 9 (18.8) | 0.22 |
| Feeding issues | 10 (22.7) | 25 (52.1) | 0.007 |
| Constipation | 12 (27.3) | 7 (14.6) | 0.13 |
| Others | 6 (13.6) | 7 (14.6) | 0.9 |
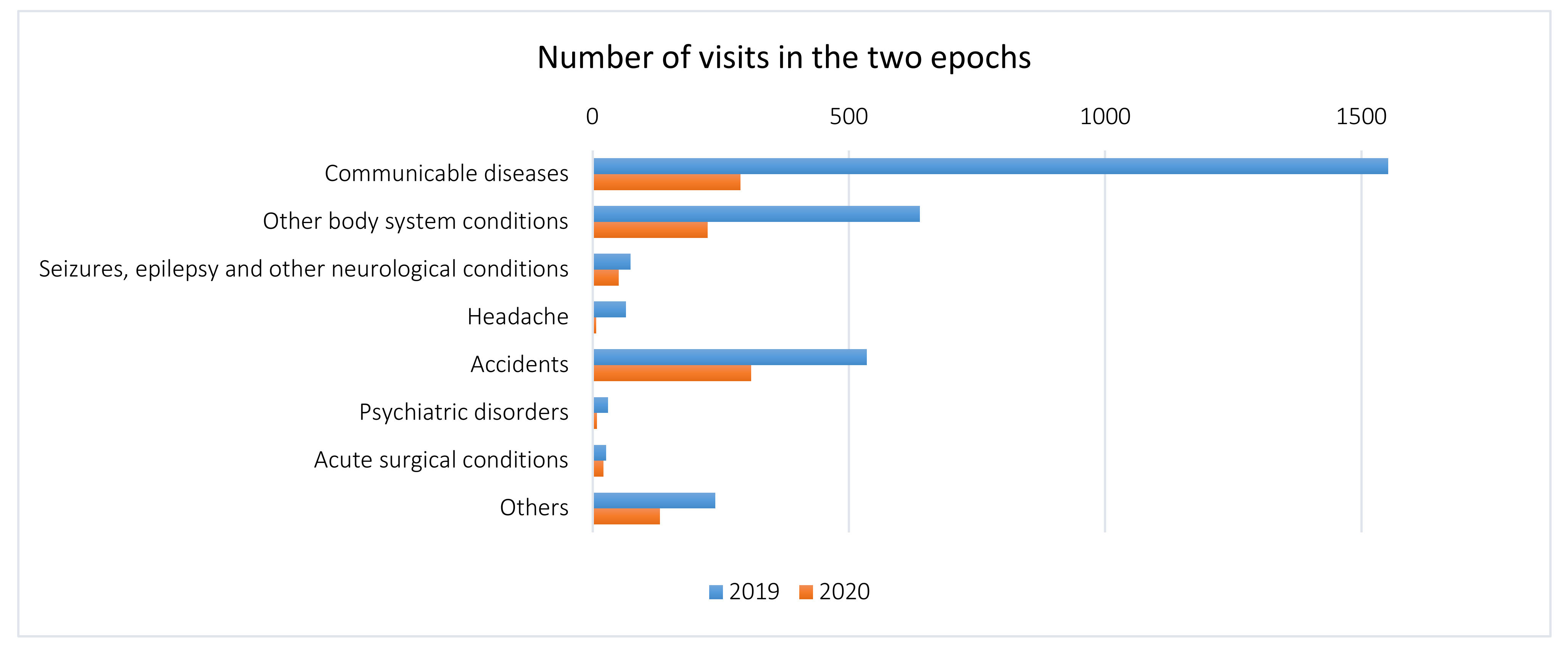
| Diagnosis at Discharge, n (%) | 2019 | 2020 | p |
|---|---|---|---|
| Communicable diseases | 1552 (49.1) | 288 (27.7) | <0.001 |
| Lower airways infections | 255 (16.4) | 54 (18.7) | 0.33 |
| Upper airways infections | 796 (51.3) | 160 (55.6) | 0.18 |
| Gastroenteritis | 378 (24.4) | 42 (14.6) | <0.001 |
| Aspecific fever | 123 (7.9) | 32 (11.1) | 0.07 |
| Other body system conditions | 638 (20.2) | 224 (21.6) | 0.34 |
| Gastrointestinal and genitourinary diseases | 371 (58.2) | 159 (70.99) | 0.01 |
| Dermatological pathologies | 247 (41.8) | 65 (29.01) | 0.01 |
| Seizures, epilepsy and other neurological conditions | 74 (2.3) | 51 (4.9) | <0.001 |
| Headache | 65 (2.1) | 7 (0.7) | 0.003 |
| Accidents | 535 (16.9) | 309 (29.7) | <0.001 |
| Head injury | 132 (24.7) | 71 (22.98) | 0.58 |
| Other traumas—burns—wounds | 237 (44.3) | 183 (59.22) | <0.001 |
| Foreign body ingestion/inhalation | 53 (9.9) | 30 (9.7) | 0.92 |
| Musculoskeletal pain | 113 (21.1) | 25 (8.1) | <0.001 |
| Psychiatric disorders | 30 (0.9) | 8 (0.8) | 0.59 |
| Acute surgical conditions | 26 (0.8) | 21 (2.0) | 0.001 |
| Others | 239 (7.6) | 131 (12.6) | <0.001 |
| Total | 3159 | 1039 |
| Outcome, n (%) | 2019 | 2020 | p |
|---|---|---|---|
| Discharge | 2893 (91.6) | 930 (89.5) | 0.04 |
| Admissions | 266 (8.4) | 109 (10.5) | 0.04 |
| PICU admissions | 27 (10.2) | 11 (10.1) | 0.99 |
| Respiratory conditions | 13 (48.1) | 0 (0) | 0.02 |
| Prolonged seizures | 1 (3.7) | 2 (18.2) | 0.13 |
| Sepsis | 3 (11.1) | 2 (18.2) | 0.29 |
| Major trauma | 2 (7.4) | 3 (27.3) | 0.1 |
| Diabetic ketoacidosis | 0 (0) | 1 (9.1) | 0.5 |
| Surgical urgencies | 4 (14.8) | 0 (0) | 0.37 |
| Others | 4 (14.8) | 3 (27.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silvagni, D.; Baggio, L.; Lo Tartaro Meragliotta, P.; Soloni, P.; La Fauci, G.; Bovo, C.; Ielo, S.; Biban, P. Neonatal and Pediatric Emergency Room Visits in a Tertiary Center during the COVID-19 Pandemic in Italy. Pediatr. Rep. 2021, 13, 168-176. https://doi.org/10.3390/pediatric13020023
Silvagni D, Baggio L, Lo Tartaro Meragliotta P, Soloni P, La Fauci G, Bovo C, Ielo S, Biban P. Neonatal and Pediatric Emergency Room Visits in a Tertiary Center during the COVID-19 Pandemic in Italy. Pediatric Reports. 2021; 13(2):168-176. https://doi.org/10.3390/pediatric13020023
Chicago/Turabian StyleSilvagni, Davide, Laura Baggio, Patrizia Lo Tartaro Meragliotta, Pietro Soloni, Giovanna La Fauci, Chiara Bovo, Stefania Ielo, and Paolo Biban. 2021. "Neonatal and Pediatric Emergency Room Visits in a Tertiary Center during the COVID-19 Pandemic in Italy" Pediatric Reports 13, no. 2: 168-176. https://doi.org/10.3390/pediatric13020023
APA StyleSilvagni, D., Baggio, L., Lo Tartaro Meragliotta, P., Soloni, P., La Fauci, G., Bovo, C., Ielo, S., & Biban, P. (2021). Neonatal and Pediatric Emergency Room Visits in a Tertiary Center during the COVID-19 Pandemic in Italy. Pediatric Reports, 13(2), 168-176. https://doi.org/10.3390/pediatric13020023






