Clinically Mild Encephalopathy with a Reversible Splenial Lesion Caused by Influenza B Virus in an Unvaccinated Child
Abstract
:1. Introduction
2. Case Report
3. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- García-Moncó, J.C.; Cortina, I.E.; Ferreira, E.; Martínez, A.; Ruiz, L.; Cabrera, A.; Beldarrain, M.G. Reversible Splenial Lesion Syndrome (RESLES): What’s in a Name? J. Neuroimaging 2011, 21, e1–e14. [Google Scholar] [CrossRef] [PubMed]
- Takanashi, J.-I.; Tada, H.; Maeda, M.; Suzuki, M.; Terada, H.; Barkovich, A.J. Encephalopathy with a reversible splenial lesion is associated with hyponatremia. Brain Dev. 2009, 31, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Ma, Y.; Feng, J. Clinicoradiological spectrum of reversible splenial lesion syndrome (RESLES) in adults: A retrospective study of a rare entity. Medicine 2015, 94, e512. [Google Scholar] [CrossRef] [PubMed]
- Tada, H.; Takanashi, J.; Barkovich, A.J.; Oba, H.; Maeda, M.; Tsukahara, H.; Suzuki, M.; Yamamoto, T.; Shimono, T.; Ichiyama, T.; et al. Clinically mild encephalitis/encephalopathy with a reversible splenial lesion. Neurology 2004, 63, 1854–1858. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.-X.; Liu, H.; Yang, S.-D.; Zeng, S.-H.; Gao, Y.-Y.; Du, Z.-H.; Li, X.-J.; Lin, H.-S.; Liang, H.-C.; Mai, J. Reversible splenial lesion syndrome in children: Retrospective study and summary of case series. Brain Dev. 2016, 38, 915–927. [Google Scholar] [CrossRef] [PubMed]
- Fumarola, A.; Ricciardelli, P.; Guiducci, C.; Turlà, G.; Cenni, P.; Marchetti, F. Encephalitis by type B influenza: A pediatric clinical case and literature review. Recenti Prog. Med. 2019, 110, 42–46. [Google Scholar] [PubMed]
- Yıldız, A.E.; Genç, H.M.; Gürkaş, E.; Ünlü, H.A.; Öncel, I.H.; Güven, A. Mild encephalitis/encephalopathy with a reversible splenial lesion in children. Diagn. Interv. Radiol. 2018, 24, 108–112. [Google Scholar] [PubMed]
- Vanderschueren, G.; Schotsmans, K.; Maréchal, E.; Crols, R. Mild encephalitis with reversible splenial (MERS) lesion syndrome due to influenza B virus. Pract. Neurol. 2018, 18, 391–392. [Google Scholar] [CrossRef] [PubMed]
| Learning Points | |
|---|---|
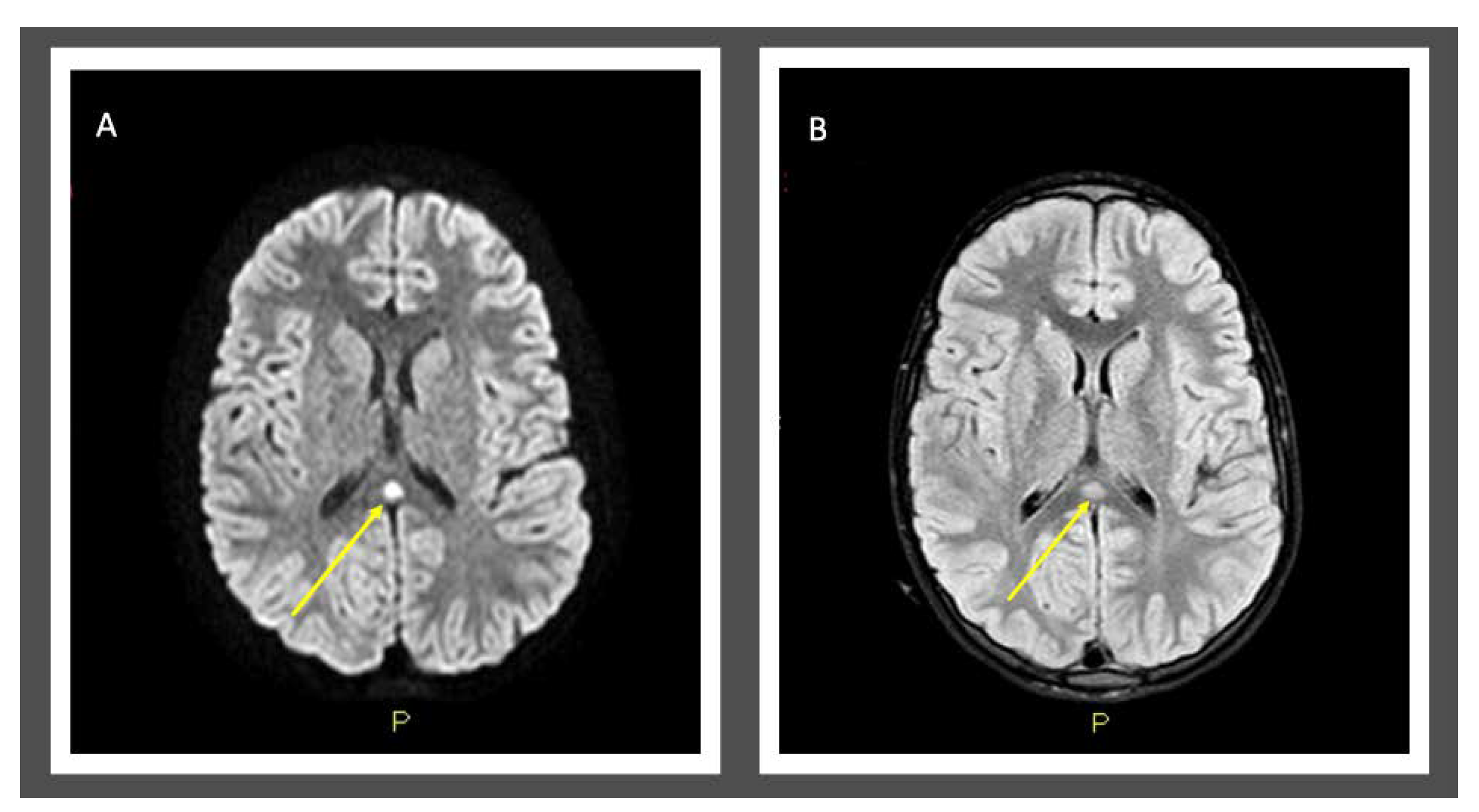
| 1 | MERS is rare clinic-radiological syndrome characterized by acute mild encephalopathy and brain MRI lesion evident in the splenium of corpus callosum (type I) that could extend into callosal radiations, frontoparietal subcortical white matter, to the rest of corpus callosum, and cerebellum (type II). |
| 2 | Viruses are most commonly related to MERS. |
| 3 | Prognosis is good if lesions are limited to splenium of corpus callosum. |
| 4 | Consider MERS in children with clinical signs of encephalopathy (neurologic symptoms or alterations of the state of consciousness) during a viral infectious event and investigate it with brain MRI exam and DWI examinations. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ventresca, S.; Guiducci, C.; Tagliani, S.; Dal Bo, S.; Ricciardelli, P.; Cenni, P.; Marchetti, F. Clinically Mild Encephalopathy with a Reversible Splenial Lesion Caused by Influenza B Virus in an Unvaccinated Child. Pediatr. Rep. 2021, 13, 72-75. https://doi.org/10.3390/pediatric13010009
Ventresca S, Guiducci C, Tagliani S, Dal Bo S, Ricciardelli P, Cenni P, Marchetti F. Clinically Mild Encephalopathy with a Reversible Splenial Lesion Caused by Influenza B Virus in an Unvaccinated Child. Pediatric Reports. 2021; 13(1):72-75. https://doi.org/10.3390/pediatric13010009
Chicago/Turabian StyleVentresca, Silvia, Claudia Guiducci, Sara Tagliani, Sara Dal Bo, Paolo Ricciardelli, Patrizia Cenni, and Federico Marchetti. 2021. "Clinically Mild Encephalopathy with a Reversible Splenial Lesion Caused by Influenza B Virus in an Unvaccinated Child" Pediatric Reports 13, no. 1: 72-75. https://doi.org/10.3390/pediatric13010009
APA StyleVentresca, S., Guiducci, C., Tagliani, S., Dal Bo, S., Ricciardelli, P., Cenni, P., & Marchetti, F. (2021). Clinically Mild Encephalopathy with a Reversible Splenial Lesion Caused by Influenza B Virus in an Unvaccinated Child. Pediatric Reports, 13(1), 72-75. https://doi.org/10.3390/pediatric13010009





