Large Congenital Pericardial Cyst Presented by Palpitation and Left Ventricle Posterior Wall Compression: A Rare Case Report
Abstract
1. Introduction
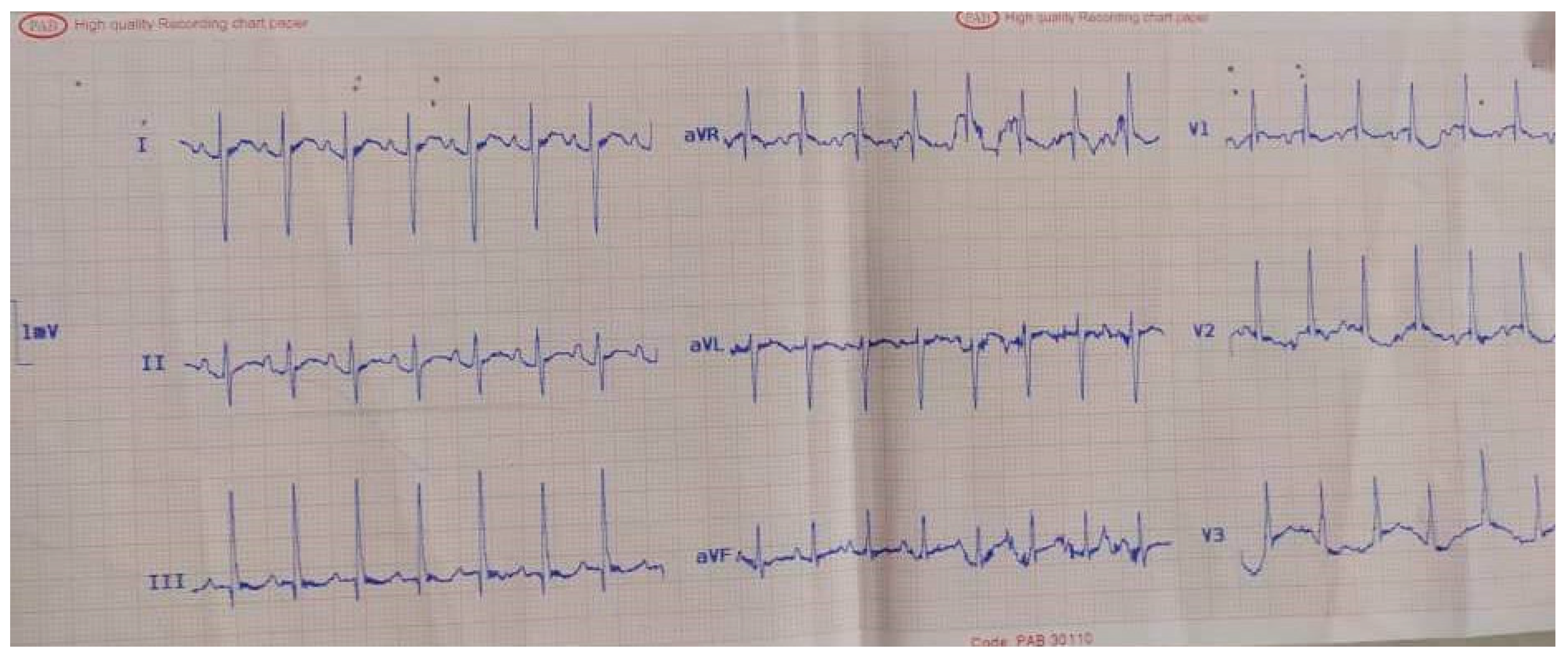
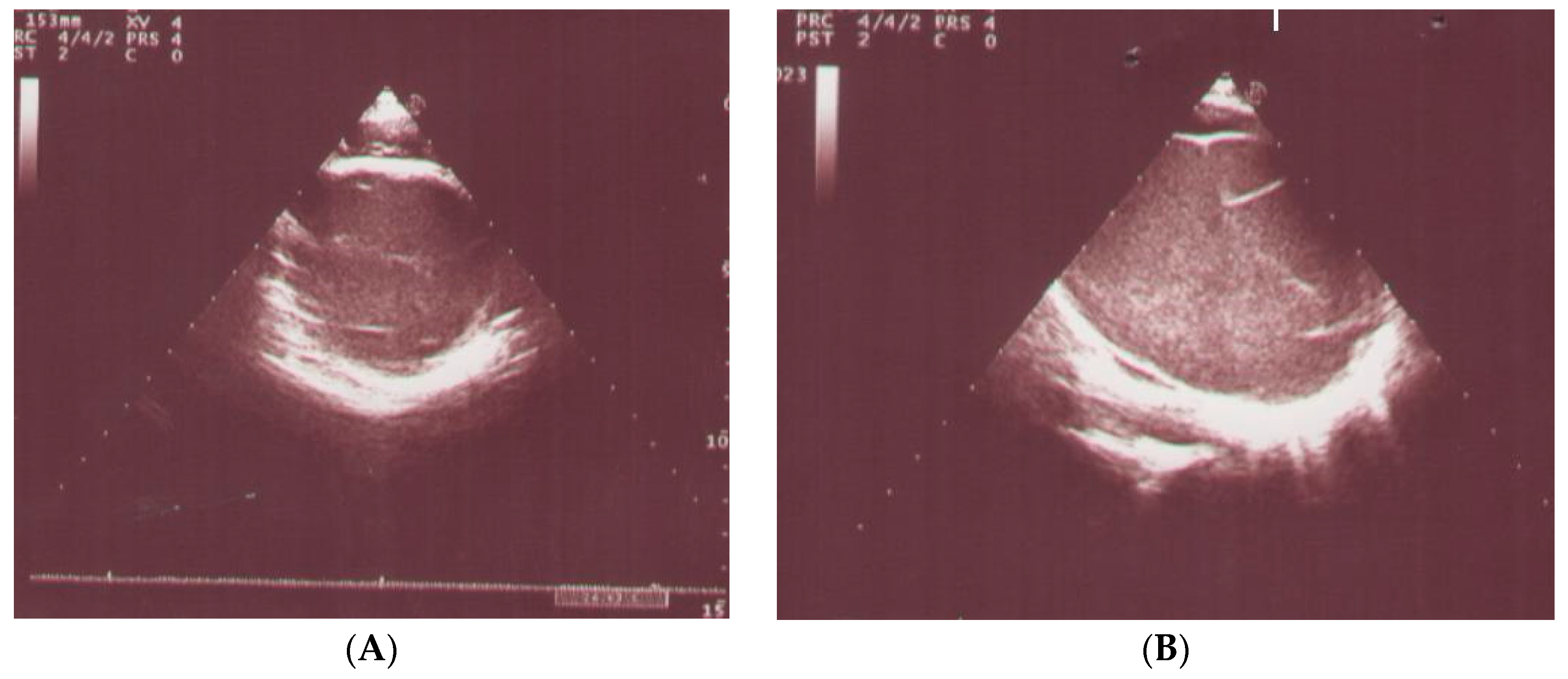
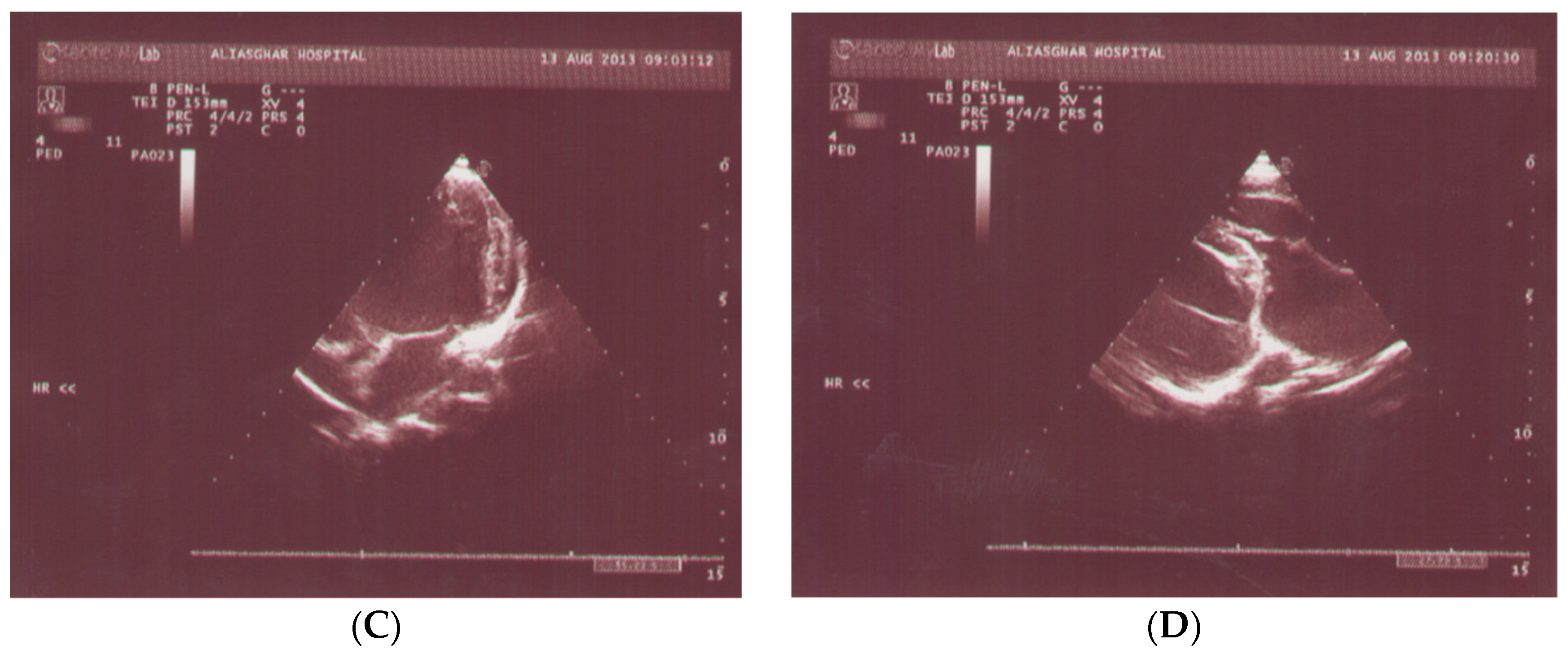
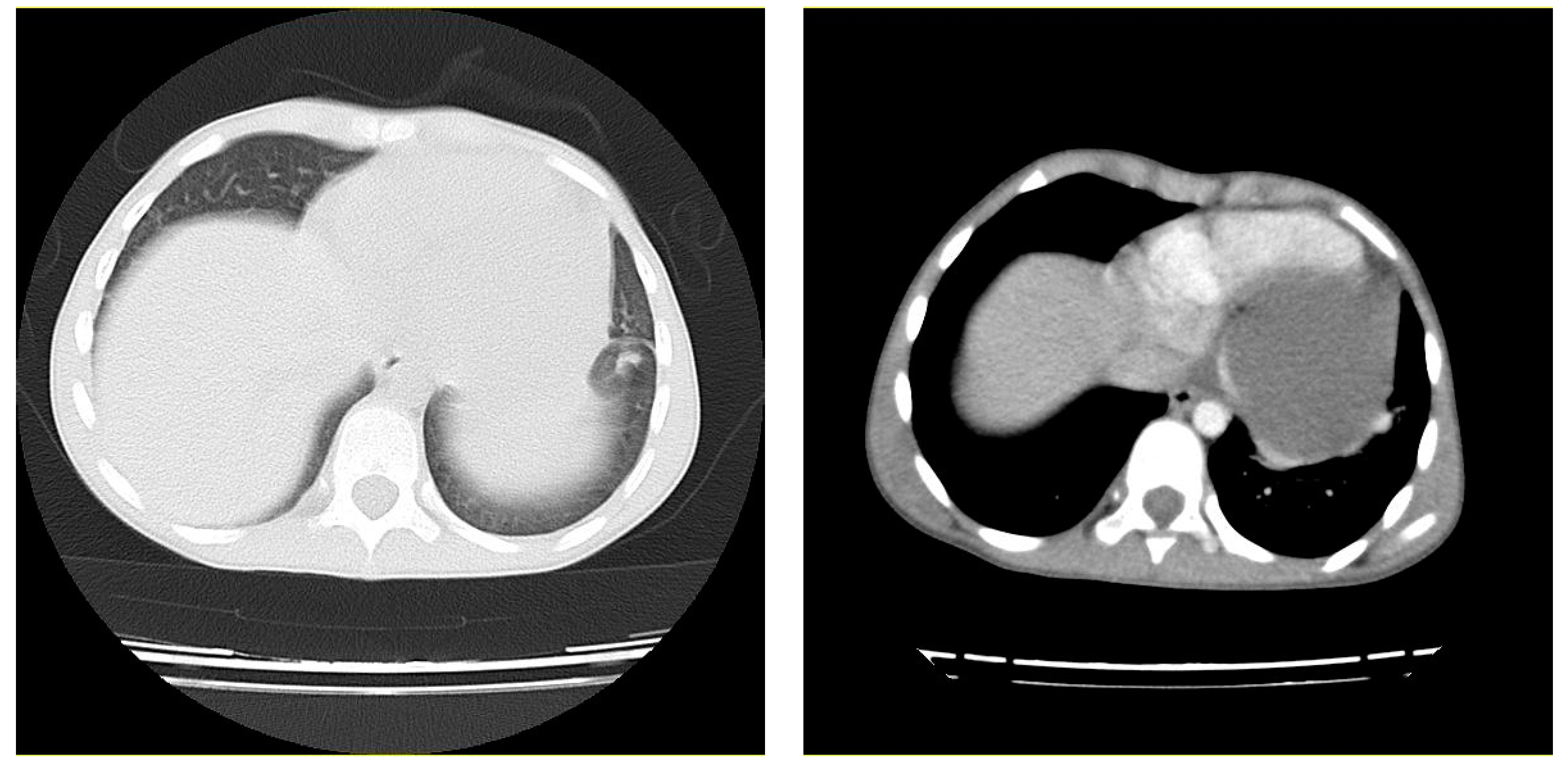
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jabr, F.I.; Skeik, N. Pericardial Cyst. Intern. Med. 2010, 49, 805–806. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mwita, J.C.; Chipeta, P.; Mutagaywa, R.; Rugwizangoga, B.; Ussiri, E. Pericardial cyst with right ventricular compression. Pan Afr. Med. J. 2012, 12, 60. [Google Scholar] [PubMed]
- Matono, R.; Shoji, F.; Yano, T.; Maehara, Y. Case report—Thoracic non-oncologic, surgical resection of a giant pericardial cyst showing a rapidly growing feature. Interact. Cardiovasc. Thorac. Surg. 2010, 10, 1056–1058. [Google Scholar] [CrossRef] [PubMed]
- Elamin, W.F.; Hannan, K. Pericardial cyst: An unusual cause of pneumonia. Cases J. 2008, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Tanoue, Y.; Fujita, S.; Kanaya, Y.; Tominaga, R. Acute Cardiac Tamponade Due to a Bleeding Pericardial Cyst in a 3-Year-Old Child. Ann. Thorac. Surg. 2007, 84, 282–284. [Google Scholar] [CrossRef] [PubMed]
- Schweigert, M.; Dubecz, A.; Beron, M.; Ofner, D.; Stein, H.J. The Tale of Spring Water Cysts; A Historical Outline of Surgery for Congenital Pericardial Diverticula and Cysts. Tex. Heart Inst. J. 2012, 39, 330–334. [Google Scholar] [PubMed]
- Antonini-Canterin, F.; Piazza, R.; Ascione, L.; Pavan, D.; Nicolosi, G.L. Value of Transesophageal Echocardiography in the Diagnosis of Compressive, Atypically Located Pericardial Cysts. J. Am. Soc. Echocardiogr. 2002, 15, 192–194. [Google Scholar] [CrossRef]
- Patel, J.; Park, C.; Michaels, J.; Rosen, S.; Kort, S. Pericardial Cyst: Case Reports and a Literature Review. Echocardiography 2004, 21, 269–272. [Google Scholar] [CrossRef]
- Najib, M.Q.; Chaliki, H.P.; Raizada, A.; Ganji, J.L.; Panse, P.M.; Click, R.L. Symptomatic pericardial cyst: A case series. Eur. J. Echocardiogr. 2011, 12, E43. [Google Scholar] [CrossRef]
- Kaul, P.; Javangula, K.; Farook, S.A. Massive benign pericardial cyst presenting with simultaneous superior vena cava and middle lobe syndromes. J. Cardiothorac. Surg. 2008, 3, 32. [Google Scholar] [CrossRef]
- Beroukhim, R.S.; Prakash, A.; Buechel, E.R.V.; Cava, J.R.; Dorfman, A.L.; Festa, P.; Hlavacek, A.M.; Johnson, T.R.; Keller, M.S.; Misra, N. Characterization of Cardiac Tumors in Children by Cardiovascular Magnetic Resonance Imaging. J. Am. Coll. Cardiol. 2011, 58, 1044–1054. [Google Scholar] [CrossRef] [PubMed]
- Noyes, B.E.; Weber, T.; Vogler, C. Pericardial Cysts in Children: Surgical or Conservative Approach? J. Pediatr. Surg. 2003, 38, 1263–1265. [Google Scholar] [CrossRef]
- Takeda, S.; Miyoshi, S.; Minami, M.; Ohta, M.; Masaoka, A.; Matsuda, H. Clinical Spectrum of Mediastinal Cysts. Chest 2003, 124, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Lambert, A.V.S. Etiology of thin-walled thoracic cysts. J. Thorac. Surg. 1940, 10, 1–7. [Google Scholar] [CrossRef]
- Mazer, M.L. True pericardial diverticulum; reportof a case, with safe operative removal. Am. J. Roentgenol. Radium Ther. 1946, 55, 27–29. [Google Scholar] [PubMed]
- Lillie, W.I.; McDonald, J.R.; Clagett, O.T. Pericardial celomic cysts and pericardial diverticula; a concept of etiology and report of cases. J. Thorac. Surg. 1950, 20, 494–504. [Google Scholar] [CrossRef]
- Lewis, K.M.; Sherer, D.M.; Gonçalves, L.F.; Fromberg, R.A.; Eglinton, G.S. Mid-trimester prenatal sonographic diagnosis of a pericardial cyst. Prenat. Diagn. 1996, 16, 549–553. [Google Scholar] [CrossRef]
- Kumar, S.; Jain, P.; Sen, R.; Rattan, K.N.; Agarwal, R.; Garg, S. Giant pericardial cyst in a 5-year-old child: A rare anomaly. Ann. Pediatr. Cardiol. 2011, 4, 68–70. [Google Scholar] [CrossRef]
- Omaygenc, M.O.; Karaca, I.O.; Cakal, B.; Gunes, H.M.; Kizilirmak, F.; Boztosun, B. Huge Pericardial Cyst with Compressing Effects on the Right-Heart Chambers. Arch. Cardiovasc. Imaging 2016, 4. [Google Scholar] [CrossRef]
- Alkharabsheh, S.; Ayache, A.; Al Halabi, S.; Kumar, A.; Mahar, J.; Gupta, N.; Gentry, J.; Klein, A. Pericardial Cysts: Do They Grow Over Time? J. Am. Coll. Cardiol. 2016, 67, 1752. [Google Scholar] [CrossRef]
- Hekmat, M.; Ghaderi, H.; Tatari, H.; Shabestari, A.A.; Mirjafari, S.A. Giant Pericardial Cyst: A Case Report and Review of Literature. Iran. J. Radiol. 2016, 13. [Google Scholar] [CrossRef] [PubMed]
- Kar, S.K.; Ganguly, T. Current concepts of diagnosis and management of pericardial cysts. Indian Heart J. 2017, 69, 364–370. [Google Scholar] [CrossRef] [PubMed]
| Etiology of Pericardial Cyst [18] |
|---|
|
|
|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noori, N.M.; Shafighi Shahri, E.; Soleimanzadeh Mousavi, S.H. Large Congenital Pericardial Cyst Presented by Palpitation and Left Ventricle Posterior Wall Compression: A Rare Case Report. Pediatr. Rep. 2021, 13, 57-64. https://doi.org/10.3390/pediatric13010007
Noori NM, Shafighi Shahri E, Soleimanzadeh Mousavi SH. Large Congenital Pericardial Cyst Presented by Palpitation and Left Ventricle Posterior Wall Compression: A Rare Case Report. Pediatric Reports. 2021; 13(1):57-64. https://doi.org/10.3390/pediatric13010007
Chicago/Turabian StyleNoori, Noor Mohamad, Elham Shafighi Shahri, and Seyed Hosein Soleimanzadeh Mousavi. 2021. "Large Congenital Pericardial Cyst Presented by Palpitation and Left Ventricle Posterior Wall Compression: A Rare Case Report" Pediatric Reports 13, no. 1: 57-64. https://doi.org/10.3390/pediatric13010007
APA StyleNoori, N. M., Shafighi Shahri, E., & Soleimanzadeh Mousavi, S. H. (2021). Large Congenital Pericardial Cyst Presented by Palpitation and Left Ventricle Posterior Wall Compression: A Rare Case Report. Pediatric Reports, 13(1), 57-64. https://doi.org/10.3390/pediatric13010007





