Epidemiological, Clinical and Phylogenetic Characteristics of West Nile Virus in Bulgaria, 2024
Abstract
1. Introduction
2. Materials and Methods
2.1. Human WNV Infection Cases
2.2. RT-qPCR and Serological Testing
2.3. Whole Genome Sequencing
2.4. Bioinformatic Analysis
2.5. Data Availability
3. Results
3.1. Demographics and Clinical Presentation
3.2. Fatal Outcomes
3.3. Laboratory Findings
3.4. Epidemiological Data
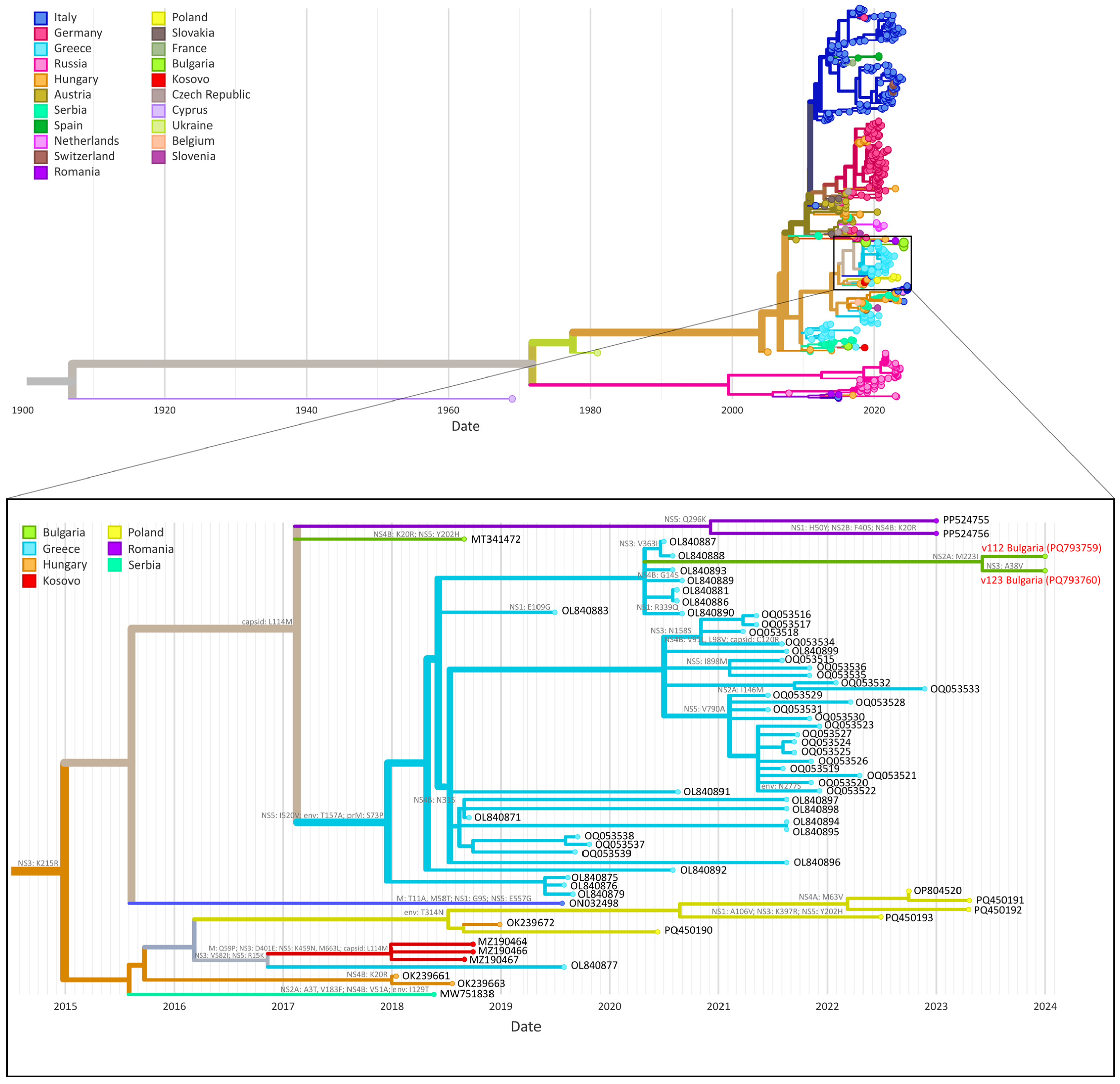
3.5. Phylogenetic and Amino Acid Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| WNV | West Nile virus |
| WGS | Whole genome sequencing |
| CSF | Cerebrospinal fluid |
| PCR | Polymerase chain reaction |
| ELISA | Enzyme-linked immunosorbent assay |
| NCIPD | National centre of infectious and parasitic diseases |
| ECDC | European Centre for Disease Prevention and Control |
References
- Rossi, S.L.; Ross, T.M.; Evans, J.D. West Nile Virus. Clin. Lab. Med. 2010, 30, 47–65. [Google Scholar] [CrossRef] [PubMed]
- Colpitts, T.M.; Conway, M.J.; Montgomery, R.R.; Fikrig, E. West Nile virus: Biology, transmission, and human infection. Clin. Microbiol. Rev. 2012, 25, 635–648. [Google Scholar] [CrossRef]
- Iwamoto, M.; Jernigan, D.B.; Guasch, A.; Trepka, M.J.; Blackmore, C.G.; Hellinger, W.C.; Pham, S.M.; Zaki, S.; Lanciotti, R.S.; Lance-Parker, S.E.; et al. West Nile Virus in Transplant Recipients Investigation Team. Transmission of West Nile Virus from an Organ Donor to Four Transplant Recipients. N. Engl. J. Med. 2003, 348, 2196–2203. [Google Scholar] [CrossRef] [PubMed]
- Pisani, G.; Cristiano, K.; Pupella, S.; Liumbruno, G.M. West Nile Virus in Europe and Safety of Blood Transfusion. Transfus. Med. Hemother. 2016, 43, 158–167. [Google Scholar] [CrossRef] [PubMed]
- David, S.; Abraham, A.M. Epidemiological and clinical aspects on West Nile virus, a globally emerging pathogen. Infect. Dis. 2016, 48, 571–586. [Google Scholar] [CrossRef]
- Pacenti, M.; Sinigaglia, A.; Franchin, E.; Pagni, S.; Lavezzo, E.; Montarsi, F.; Capelli, G.; Barzon, L. Human West Nile Virus Lineage 2 Infection: Epidemiological, Clinical, and Virological Findings. Viruses 2020, 12, 458. [Google Scholar] [CrossRef]
- Erazo, D.; Grant, L.; Ghisbain, G.; Marini, G.; Colón-González, F.J.; Wint, W.; Rizzoli, A.; Van Bortel, W.; Vogels, C.B.F.; Grubaugh, N.D.; et al. Contribution of climate change to the spatial expansion of West Nile virus in Europe. Nat. Commun. 2024, 15, 1–10. [Google Scholar] [CrossRef]
- Lu, L.; Zhang, F.; Oude Munnink, B.B.; Munger, E.; Sikkema, R.S.; Pappa, S.; Tsioka, K.; Sinigaglia, A.; Dal Molin, E.; Shih, B.B.; et al. West Nile virus spread in Europe: Phylogeographic pattern analysis and key drivers. PLoS Pathog. 2024, 20, e1011880. [Google Scholar] [CrossRef]
- Bogdanic, M.; Savic, V.; Klobucar, A.; Barbic, L.; Sabadi, D.; Tomljenovic, M.; Madic, J.; Hruskar, Z.; Curman Posavec, M.; Santini, M.; et al. The Re-Emergence of Neuroinvasive Flaviviruses in Croatia During the 2022 Transmission Season. Microorganisms 2024, 12, 2210. [Google Scholar] [CrossRef]
- Fleischmann, W.A.; Cao, L.C.; Nurjadi, D.; Velavan, T.P. Addressing the rise of autochthonous vector-borne diseases in a warming Europe. Int. J. Infect. Dis. 2024, 149, 107275. [Google Scholar] [CrossRef]
- Brandolini, M.; De Pascali, A.M.; Zaghi, I.; Dirani, G.; Zannoli, S.; Ingletto, L.; Lavazza, A.; Lelli, D.; Dottori, M.; Calzolari, M.; et al. Advancing West Nile virus monitoring through whole genome sequencing: Insights from a One Health genomic surveillance study in Romagna (Italy). One Health 2024, 19, 100937. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Epidemiological Update: West Nile Virus Transmission Season in Europe. 2018. Available online: https://www.ecdc.europa.eu/en/news-events/epidemiological-update-west-nile-virus-transmission-season-europe-2018 (accessed on 25 December 2024).
- European Food Safety Authority and European Centre for Disease Prevention and Control (EFSA and ECDC). The European Union One Health 2018 Zoonoses Report. EFSA J. 2019, 17, e05926. [Google Scholar] [CrossRef]
- European Food Safety Authority and European Centre for Disease Prevention and Control (EFSA and ECDC). The European Union Summary Report on Trends and Sources of Zoonoses, Zoonotic Agents and Food-Borne Outbreaks in 2016. EFSA J. 2017, 15, e05077. [Google Scholar] [CrossRef]
- National Center of Infectious and Parasitic Diseases. Остри заразни бoлести в България през 2023 г. [Acute Infectious Diseases in Bulgaria in 2023]. Available online: https://www.ncipd.org/images/UserFiles/File/Analizi/Analysis_ZB%20_2023%20FINAL.pdf (accessed on 25 December 2024).
- National Center of Infectious and Parasitic Diseases. Епидемиoлoгичен бюлетин [Epidemiological bulletin]. Available online: https://www.ncipd.org/index.php?option=com_biuletin&view=view&year=2024&month=49&lang=bg (accessed on 25 December 2024).
- European Commission. Commission Implementing Decision (EU) 2018/945 of 22 June 2018 on the communicable diseases and related special health issues to be covered by epidemiological surveillance as well as relevant case definitions. OJEU 2018, L 170, 1–74. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32018D0945&from=EN#page=50 (accessed on 29 March 2025).
- Linke, S.; Ellerbrok, H.; Niedrig, M.; Nitsche, A.; Pauli, G. Detection of West Nile virus lineages 1 and 2 by real-time PCR. J. Virol. Methods 2007, 146, 355–358. [Google Scholar] [CrossRef]
- Babraham Bioinformatics. FastQC A Quality Control tool for High Throughput Sequence Data. Available online: https://www.bioinformatics.babraham.ac.uk/projects/fastqc/ (accessed on 25 December 2024).
- Chen, S. Ultrafast one-pass FASTQ data preprocessing, quality control, and deduplication using fastp. iMeta 2023, 2, e107. [Google Scholar] [CrossRef]
- Geneious. Bioinformatics Software for Sequence Data Analysis. Available online: https://www.geneious.com/ (accessed on 25 December 2024).
- Wang, S.; Sundaram, J.P.; Spiro, D. VIGOR, an annotation program for small viral genomes. BMC Bioinform. 2010, 11, 451. [Google Scholar] [CrossRef]
- Hadfield, J.; Megill, C.; Bell, S.M.; Huddleston, J.; Potter, B.; Callender, C.; Sagulenko, P.; Bedford, T.; Neher, R.A. Nextstrain: Real-time tracking of pathogen evolution. Bioinformatics 2018, 34, 4121–4123. [Google Scholar] [CrossRef]
- Mencattelli, G.; Ndione, M.H.D.; Silverj, A.; Diagne, M.M.; Curini, V.; Teodori, L.; Di Domenico, M.; Mbaye, R.; Leone, A.; Marcacci, M.; et al. Spatial and temporal dynamics of West Nile virus between Africa and Europe. Nat. Commun. 2023, 14, 6440. [Google Scholar] [CrossRef]
- Huddleston, J.; Hadfield, J.; Sibley, T.R.; Lee, J.; Fay, K.; Ilcisin, M.; Harkins, E.; Bedford, T.; Neher, R.A.; Hodcroft, E.B. Augur: A bioinformatics toolkit for phylogenetic analyses of human pathogens. J. Open Source Softw. 2021, 6, 2906. [Google Scholar] [CrossRef]
- Tsioka, K.; Gewehr, S.; Pappa, S.; Kalaitzopoulou, S.; Stoikou, K.; Mourelatos, S.; Papa, A. West Nile Virus in Culex Mosquitoes in Central Macedonia, Greece, 2022. Viruses 2023, 15, 224. [Google Scholar] [CrossRef] [PubMed]
- Bode, A.V.; Sejvar, J.J.; Pape, W.J.; Campbell, G.L.; Marfin, A.A. West Nile virus disease: A descriptive study of 228 patients hospitalized in a 4-county region of Colorado in 2003. Clin. Infect. Dis. 2006, 42, 1234–1240. [Google Scholar] [CrossRef] [PubMed]
- Jean, C.M.; Honarmand, S.; Louie, J.K.; Glaser, C.A. Risk Factors for West Nile Virus Neuroinvasive Disease, California, 2005. Emerg. Infect. Dis. 2007, 13, 1918. [Google Scholar] [CrossRef] [PubMed]
- Murray, K.O.; Koers, E.; Baraniuk, S.; Herrington, E.; Carter, H.; Sierra, M.; Kilborn, C.; Arafat, R. Risk factors for encephalitis from West Nile Virus: A matched case-control study using hospitalized controls. Zoonoses Public Health 2009, 56, 370–375. [Google Scholar] [CrossRef]
- Christova, I.; Panayotova, E.; Trifonova, I.; Taseva, E.; Gladnishka, T. Unexpectedly high number of West Nile neuroinvasive diseases in Bulgaria in 2018. Probl. Infect. Parasit. Dis. 2018, 46, 16–19. [Google Scholar] [CrossRef]
- Baymakova, M.; Trifonova, I.; Panayotova, E.; Dakova, S.; Pacenti, M.; Barzon, L.; Lavezzo, E.; Hristov, Y.; Ramshev, K.; Plochev, K.; et al. Fatal Case of West Nile Neuroinvasive Disease in Bulgaria. Emerg. Infect. Dis. 2016, 22, 2203. [Google Scholar] [CrossRef]
- Argirova, P.; Kalchev, Y.; Vasilev, P.; Christova, I.; Stoycheva, M.; Murdjeva, M. West Nile virus meningoencephalitis and cytokines analysis: Review and case report. Biotechnol. Biotechnol. Equip. 2024, 38, 2358991. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Surveillance of West Nile Virus Infections in Humans, Weekly Report. Available online: https://www.ecdc.europa.eu/en/west-nile-fever/surveillance-and-disease-data/disease-data-ecdc (accessed on 25 December 2024).
- Sejvar, J.J. Clinical Manifestations and Outcomes of West Nile Virus Infection. Viruses 2014, 6, 606–623. [Google Scholar] [CrossRef]
- Mazurek, J.M.; Winpisinger, K.; Mattson, B.J.; Duffy, R.; Moolenaar, R.L. The epidemiology and early clinical features of West Nile virus infection. Am. J. Emerg. Med. 2005, 23, 536–543. [Google Scholar] [CrossRef]
- Sambri, V.; Capobianchi, M.R.; Cavrini, F.; Charrel, R.; Donoso-Mantke, O.; Escadafal, C.; Franco, L.; Gaibani, P.; Gould, E.A.; Niedrig, M.; et al. Diagnosis of West Nile Virus Human Infections: Overview and Proposal of Diagnostic Protocols Considering the Results of External Quality Assessment Studies. Viruses 2013, 5, 2329. [Google Scholar] [CrossRef]
- Lustig, Y.; Mannasse, B.; Koren, R.; Katz-Likvornik, S.; Hindiyeh, M.; Mandelboim, M.; Dovrat, S.; Sofer, D.; Mendelson, E. Superiority of West Nile Virus RNA Detection in Whole Blood for Diagnosis of Acute Infection. J. Clin. Microbiol. 2016, 54, 2294. [Google Scholar] [CrossRef] [PubMed]
- Tardei, G.; Ruta, S.; Chitu, V.; Rossi, C.; Tsai, T.F.; Cernescu, C. Evaluation of Immunoglobulin M (IgM) and IgG Enzyme Immunoassays in Serologic Diagnosis of West Nile Virus Infection. J. Clin. Microbiol. 2000, 38, 2232. [Google Scholar] [CrossRef] [PubMed]
- Busch, M.P.; Kleinman, S.H.; Tobler, L.H.; Kamel, H.T.; Norris, P.J.; Walsh, I.; Matud, J.L.; Prince, H.E.; Lanciotti, R.S.; Wright, D.J.; et al. Virus and antibody dynamics in acute west nile virus infection. J. Infect. Dis. 2008, 198, 984–993. [Google Scholar] [CrossRef] [PubMed]
- De Filette, M.; Ulbert, S.; Diamond, M.; Sanders, N.N. Recent progress in West Nile virus diagnosis and vaccination. Vet. Res. 2012, 43, 1–15. [Google Scholar] [CrossRef]
- Christova, I.; Panayotova, E.; Tchakarova, S.; Taseva, E.; Trifonova, I.; Gladnishka, T. A nationwide seroprevalence screening for West Nile virus and Tick-borne encephalitis virus in the population of Bulgaria. J. Med. Virol. 2017, 89, 1875–1878. [Google Scholar] [CrossRef]
- Panayotova, E.; Christova, I.; Trifonova, I.; Taseva, E.; Gladnishka, T.; Ivanova, V. Seroprevalence of West Nile virus in Bulgaria, 2018. Probl. Infect. Parasit. Dis. 2019, 47, 15–17. [Google Scholar] [CrossRef]
- Christova, I.; Papa, A.; Trifonova, I.; Panayotova, E.; Pappa, S.; Mikov, O. West Nile virus lineage 2 in humans and mosquitoes in Bulgaria, 2018–2019. J. Clin. Virol. 2020, 127, 104365. [Google Scholar] [CrossRef]
- Rusenova, N.; Rusenov, A.; Chervenkov, M.; Sirakov, I. Seroprevalence of West Nile Virus among Equids in Bulgaria in 2022 and Assessment of Some Risk Factors. Vet. Sci. 2024, 11, 209. [Google Scholar] [CrossRef]
- Rusenova, N.; Rusenov, A.; Monaco, F. A Retrospective Study on the Seroprevalence of West Nile Virus Among Donkeys and Mules in Bulgaria. Vector Borne Zoonotic Dis. 2024, 24, 274–277. [Google Scholar] [CrossRef]
- Trifonova, I.; Christova, I.; Ivanova-Aleksandrova, N.; Gladnishka, T.; Ivanova, V.; Panayotova, E.; Taseva, E.; Dimitrov, D.; Marinov, M.; Kamenov, G.; et al. Survey of Borrelia burgdorferi sensu lato and West Nile fever virus in wild birds in Bulgaria. Biologia 2022, 77, 3519–3524. [Google Scholar] [CrossRef]
- WorldData. Climate and Temperature Development in Bulgaria. Available online: https://www.worlddata.info/europe/bulgaria/climate.php (accessed on 25 December 2024).
- European Centre for Disease Prevention and Control. Historical Data by Year—West Nile Virus Seasonal Surveillance. Available online: https://www.ecdc.europa.eu/en/west-nile-fever/surveillance-and-disease-data/historical (accessed on 25 December 2024).
- Knyazhanskaya, E.; Morais, M.C.; Choi, K.H. Flavivirus enzymes and their inhibitors. Enzymes 2021, 49, 265. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Wu, Z.; Wang, M.; Cheng, A. Innate Immune Evasion Mediated by Flaviviridae Non-Structural Proteins. Viruses 2017, 9, 291. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, J.A.; Wang, T.; Barrett, A.D. Virulence determinants of West Nile virus: How can these be used for vaccine design? Future Virol. 2017, 12, 283. [Google Scholar] [CrossRef] [PubMed]
- Serman, T.; Chiang, C.; Liu, G.; Sayyad, Z.; Pandey, S.; Volcic, M.; Lee, H.; Muppala, S.; Acharya, D.; Goins, C.; et al. Acetylation of the NS3 helicase by KAT5γ is essential for flavivirus replication. Cell Host Microbe. 2023, 31, 1317. [Google Scholar] [CrossRef]
| Age/Sex | Symptoms | Underlying Conditions | Outcome | Positive WNV Laboratory Findings | Case Classification |
|---|---|---|---|---|---|
| Mild/Moderate | |||||
| 30/F | Fever, malaise, headache, rash, eye pain | Hashimoto thyroiditis, vitiligo | Recovered | Serum IgM and IgG positive | Probable |
| 46/F | Malaise, rash, eye swelling | Recovered | Serum IgM and IgG positive | Probable | |
| 57/F | Fever, chills, headache, rash | Recovered | CSF IgM positive Serum IgM positive | Confirmed | |
| 63/F | Fever, rash | Recovered | Serum IgM positive | Probable | |
| 55/F | Fever, headache | Recovered | Serum IgM positive | Probable | |
| 71/M | Fever, vomiting, stomach pain, diarrhoea, diplopia, myalgia | Diabetes mellitus | Recovered | RT-qPCR positive (urine) Serum IgM and IgG positive | Confirmed |
| 41/M | Fever, toxic–infectious syndrome | Recovered | RT-qPCR positive (blood) Serum IgM positive | Confirmed | |
| 34/F | Fever, headache, nausea, vomiting, arthralgia | Recovered | Serum IgM and IgG positive | Probable | |
| 50/M | Fever, malaise, myalgia | Cancer | Recovered | Serum IgM positive | Probable |
| 74/F | Fever, malaise, headache, dark skin spots, cervical lymphadenopathy | Recovered | Serum IgM and IgG positive | Probable | |
| 75/F | N/A | N/A | N/A | Serum IgM positive Serum IgG borderline | Probable |
| Severe | |||||
| 73/M | Fever, chills, fatigue, lower limb weakness, coma | Congestive heart disease | Fatal | RT-qPCR positive (urine) Serum IgM positive | Confirmed |
| 60/M | Fever, fatigue, dyspnoea, oliguria/anuria, increased muscle tone in limbs, deteriorated general condition, unresponsiveness | Parkinson disease | Fatal | Serum IgM positive Serum IgG borderline | Probable |
| 74/M | Fever, dyspnoea, fatigue, numbness and muscle pain, somnolence, unconsciousness, vomiting | Recovered | RT-qPCR positive (serum) Serum IgM and IgG positive | Confirmed | |
| 61/M | Fever, chills, arthralgia, myalgia, disoriented, psychoemotionally agitated, neck stiffness, positive Kernig’s sign, headache, vomiting | Bronchial asthma, anaemia | Recovered | RT-qPCR positive (CSF, urine, serum) Serum IgM and IgG positive | Confirmed |
| 49/M | Fever, chills, rash, jaw stiffness, tongue biting, difficulty communicating, myoclonic contractions of the limbs, hypersensitivity, hydrophobia, quantitative changes in consciousness, headache | Recovered | CSF IgM and IgG positive Serum IgM and IgG positive | Confirmed | |
| 66/M | Fever, rash, disoriented, difficulty communicating, deteriorated general condition, headache, vomiting | Urothelial papilloma, diabetes mellitus with complications, chronic renal failure, chronic obstructive pulmonary disease, Hashimoto thyroiditis | Recovered | Serum IgM positive | Probable |
| 59/M | Fever, chills, fatigue, myalgia, rash, increased muscle tone in limbs, quantitative changes in consciousness, deteriorated general condition, hypersensitivity, headache | Recovered | RT-qPCR positive (urine) Serum IgM and IgG positive | Confirmed | |
| 55/M | Psychomotor agitation, neck stiffness, positive Kernig’s sign, increased muscle tone in limbs | Arterial hypertension, diabetes mellitus, chronic renal failure | Fatal | CSF IgM positive Serum IgM and IgG positive | Confirmed |
| 73/M | Fever, nausea, vomiting, tremors, deteriorated general condition | Recovered | RT-qPCR positive (urine) Serum IgM and IgG positive | Confirmed | |
| 67/M | Fever, myalgia, disoriented, inadequate, difficult to communicate with, immobile, deteriorated general condition, headache, nausea | Arterial hypertension, gout | Recovered | Serum IgM and IgG positive | Probable |
| 57/M | Chills, headache, vomiting, dizziness | Recovered | CSF IgM positive Serum IgM and IgG positive | Confirmed | |
| 67/F | Fever, fatigue, nausea, myalgia, arthralgia, headache, diplopia, dizziness, bradyphasia | Recovered | Serum IgM and IgG positive | Probable | |
| 90/M | Fever, dyspnoea, deteriorated general condition, unresponsive, clonic seizures | Chronic obstructive pulmonary disease, chronic congestive heart disease, arterial hypertension | Recovered | Serum IgM and IgG positive | Probable |
| 80/F | Fever, chills, fatigue, cough, headache, vomiting, confusion, unresponsive, left gaze deviation, mild seizures with apnoeic pauses, neck stiffness, positive Kernig’s sign; weak somatic reflexes | Arterial hypertension, diabetes mellitus | Recovered | Serum IgM and IgG positive | Probable |
| 55/M | Deteriorated general condition, inadequate, difficult verbal contact, tremor of the upper limbs, exsiccosis, facial asymmetry, absent bilateral patellar and Achilles reflexes, unresponsive to pain, coma, hyperglycaemia, pleural effusions | Alcohol abuse, diabetes mellitus, chronic pancreatitis | Recovered | Serum IgM and IgG positive | Probable |
| 26/M | Fever, syncope, seizures, tongue biting, vomiting | Recovered | Serum IgM positive | Probable | |
| 47/F | Fever, partially disoriented, bradypsychic, neck stiffness, severe headache, vomiting | Recovered | Serum IgM and IgG positive | Probable | |
| 71/M | Fever, positive pathological reflexes, somnolence, severe headache, vomiting | Recovered | RT-qPCR positive (urine) Serum IgM and IgG positive | Confirmed | |
| 71/M | Brain edema | Recovered | Serum IgM positive | Probable | |
| 72/M | Fever, fatigue, myalgia, arthralgia, rash, headache, disorientation, dizziness, sleepiness; deteriorated general condition, unconsciousness | Recovered | Serum IgM and IgG positive | Probable | |
| 17/F | Meningoencephalitis | Recovered | Serum IgM positive | Probable | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ngoc, K.; Stoikov, I.; Trifonova, I.; Panayotova, E.; Trifonova, I.; Christova, I. Epidemiological, Clinical and Phylogenetic Characteristics of West Nile Virus in Bulgaria, 2024. Microbiol. Res. 2025, 16, 82. https://doi.org/10.3390/microbiolres16040082
Ngoc K, Stoikov I, Trifonova I, Panayotova E, Trifonova I, Christova I. Epidemiological, Clinical and Phylogenetic Characteristics of West Nile Virus in Bulgaria, 2024. Microbiology Research. 2025; 16(4):82. https://doi.org/10.3390/microbiolres16040082
Chicago/Turabian StyleNgoc, Kim, Ivan Stoikov, Ivelina Trifonova, Elitsa Panayotova, Iva Trifonova, and Iva Christova. 2025. "Epidemiological, Clinical and Phylogenetic Characteristics of West Nile Virus in Bulgaria, 2024" Microbiology Research 16, no. 4: 82. https://doi.org/10.3390/microbiolres16040082
APA StyleNgoc, K., Stoikov, I., Trifonova, I., Panayotova, E., Trifonova, I., & Christova, I. (2025). Epidemiological, Clinical and Phylogenetic Characteristics of West Nile Virus in Bulgaria, 2024. Microbiology Research, 16(4), 82. https://doi.org/10.3390/microbiolres16040082





