Trends and Patterns of Antimicrobial Resistance in a Tertiary Care Hospital in Bangladesh
Abstract
1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Isolation and Identification of Bacteria
2.3. Antimicrobial Susceptibility Testing
2.4. Data Collection and Management
2.5. Data Management and Analysis
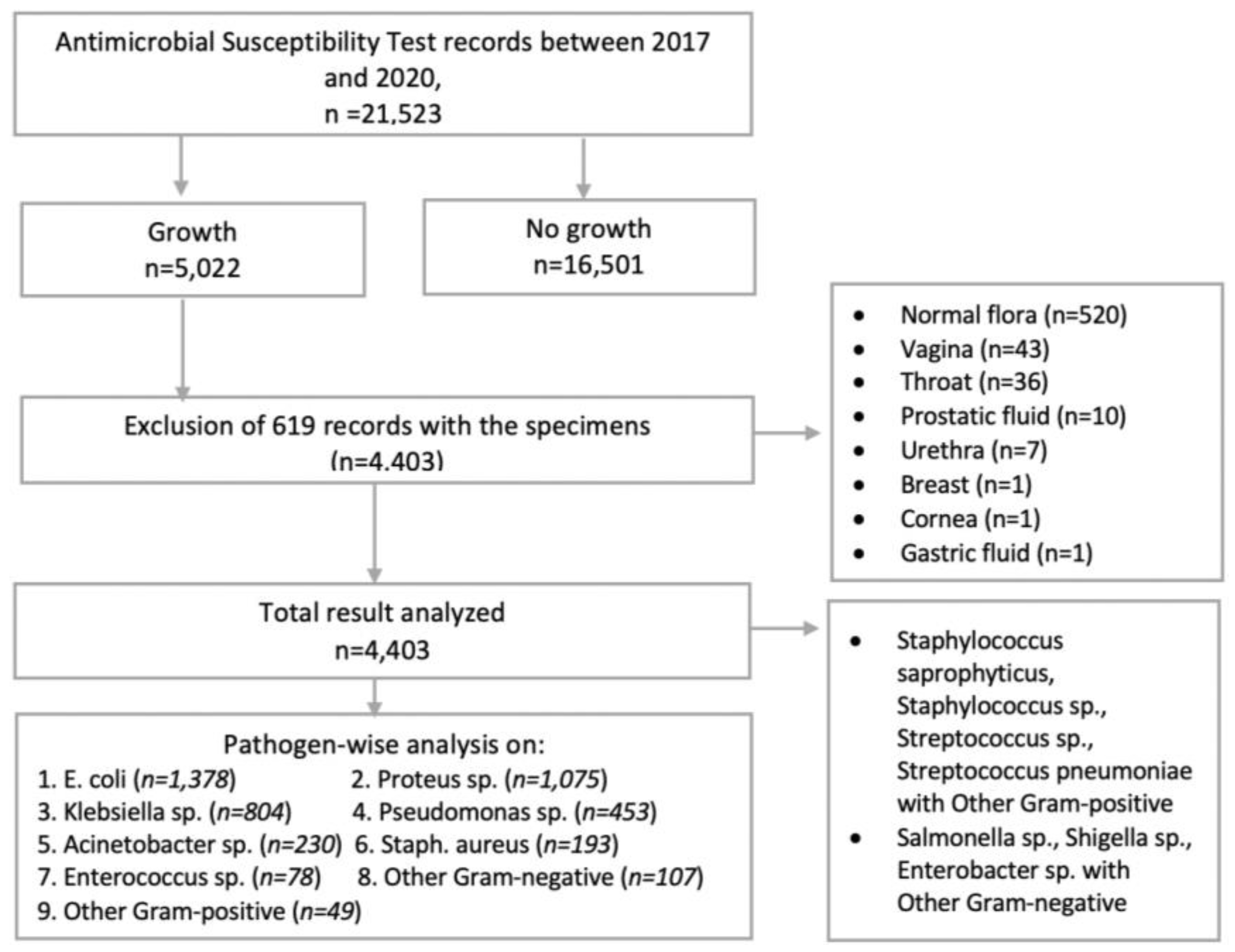
2.6. Inclusion and Exclusion Criteria
2.7. Quality Control
2.8. Ethical Consideration
3. Results
3.1. Demographic Characteristics
3.2. Frequency of Bacterial Isolates
3.3. Antimicrobial Resistance Patterns
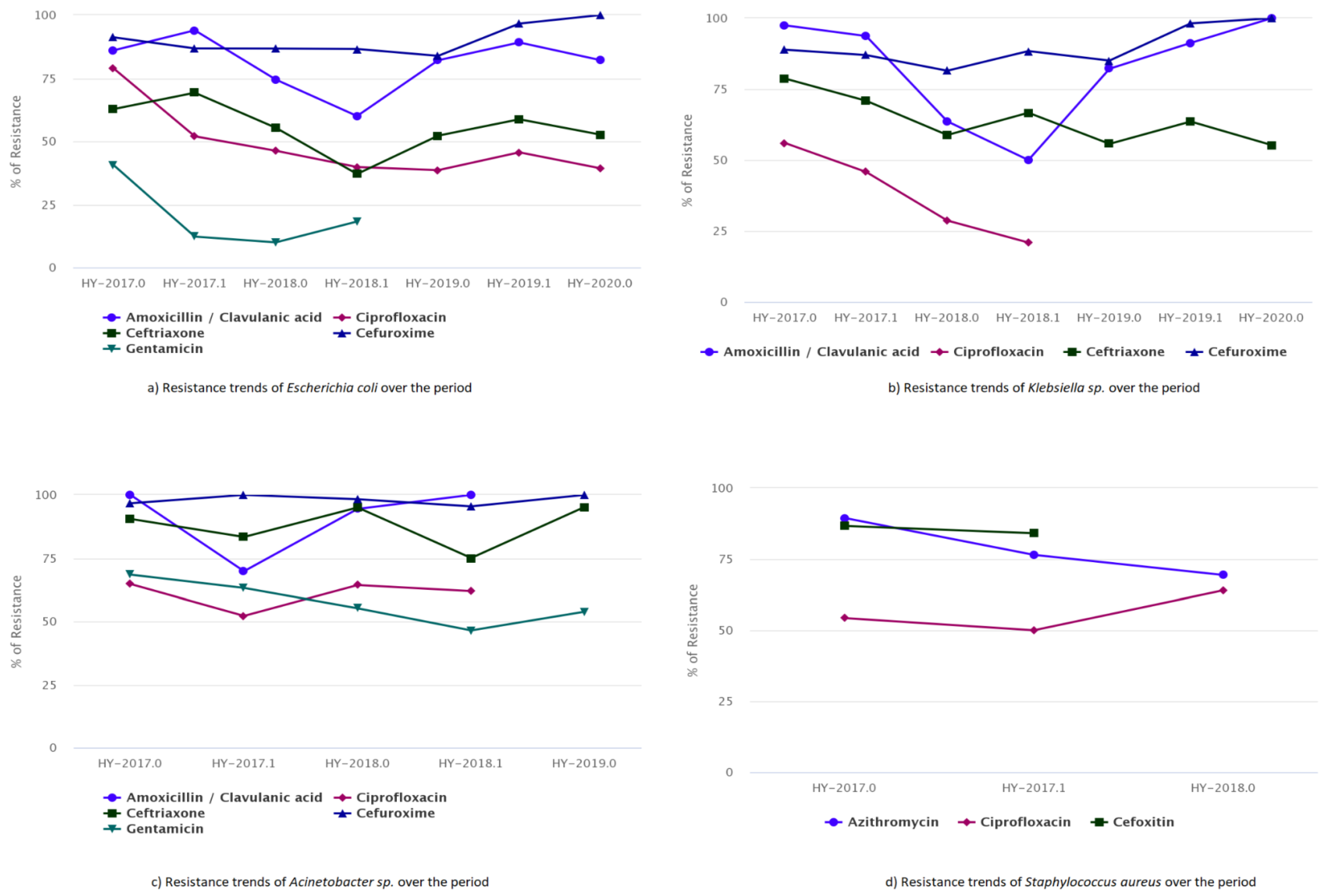
3.4. Antimicrobial Resistance Trends
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ahmed, I.; Rabbi, M.B.; Sultana, S. Antibiotic resistance in Bangladesh: A systematic review. Int. J. Infect. Dis. 2019, 80, 54–61. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Antimicrobial Resistance 2018 July 17, 2021. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 26 August 2024).
- Michael, C.A.; Dominey-Howes, D.; Labbate, M. The Antimicrobial Resistance Crisis: Causes, Consequences, and Management. Front. Public Health 2014, 2, 145. [Google Scholar] [CrossRef]
- Mogasale, V.V.; Saldanha, P.; Pai, V.; Rekha, P.D.; Mogasale, V. A descriptive analysis of antimicrobial resistance patterns of WHO priority pathogens isolated in children from a tertiary care hospital in India. Sci. Rep. 2021, 11, 5116. [Google Scholar] [CrossRef]
- Luepke, K.H.; Mohr, J.F. The antibiotic pipeline: Reviving research and development and speeding drugs to market. Expert. Rev. Anti-Infect. Ther. 2017, 15, 425–433. [Google Scholar] [CrossRef]
- Hassan, R.; Gilany, A.H.; Elaal, A.M.; El-Mashad, N.; Abdelazim, D. Antibiotic Resistance Pattern of Bacteria Causing Hospital Acquired Infections in the New Mansoura General Hospital, Egypt. Arch. Community Med. 2021, 3, 16–21. [Google Scholar]
- Azimi, T.; Maham, S.; Fallah, F.; Azimi, L.; Gholinejad, Z. Evaluating the antimicrobial resistance patterns among major bacterial pathogens isolated from clinical specimens taken from patients in Mofid Children’s Hospital, Tehran, Iran: 2013–2018. Infect. Drug Resist. 2019, 12, 2089–2102. [Google Scholar] [CrossRef] [PubMed]
- Abebe, M.; Tadesse, S.; Meseret, G.; Derbie, A. Type of bacterial isolates and antimicrobial resistance profile from different clinical samples at a Referral Hospital, Northwest Ethiopia: Five years data analysis. BMC Res. Notes 2019, 12, 568. [Google Scholar] [CrossRef]
- Lin, M.; Weinstein, R.; Hayden, M.K. Multidrug-resistant organisms: Epidemiology and control. In Bennett & Brachman’s Hospital Infections, 6th ed.; Wolters Kluwer Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014; pp. 198–199. [Google Scholar]
- Bernatchez, S.F. Reducing antimicrobial resistance by practising better infection prevention and control. Am. J. Infect. Control 2023, 51, 1063–1066. [Google Scholar] [CrossRef] [PubMed]
- Storr, J.; Twyman, A.; Zingg, W.; Damani, N.; Kilpatrick, C.; Reilly, J.; Price, L.; Egger, M.; Grayson, M.L.; WHO Guidelines Development Group; et al. Core components for effective infection prevention and control programmes: New WHO evidence-based recommendations. Antimicrob. Resist. Infect. Control 2017, 6, 6. [Google Scholar] [CrossRef]
- Harun, M.G.D.; Anwar, M.M.U.; Sumon, S.A.; Hassan, M.Z.; Haque, T.; Mah-E-Muneer, S.; Rahman, A.; Abdullah, S.A.H.M.; Islam, M.S.; Styczynski, A.R.; et al. Infection prevention and control in tertiary care hospitals of Bangladesh: Results from WHO infection prevention and control assessment framework (IPCAF). Antimicrob. Resist. Infect. Control 2022, 11, 125. [Google Scholar] [CrossRef]
- Ayukekbong, J.A.; Ntemgwa, M.; Atabe, A.N. The threat of antimicrobial resistance in developing countries: Causes and control strategies. Antimicrob. Resist. Infect. Control 2017, 6, 47. [Google Scholar] [CrossRef] [PubMed]
- OECD. Stemming the Superbug Tide; OECD: Paris, France, 2018. [Google Scholar]
- World Health Organization (WHO). Global Action Plan on Antimicrobial Resistance. Available online: https://www.emro.who.int/health-topics/drug-resistance/global-action-plan.html (accessed on 26 August 2024).
- Ministry of Health and Family Welfare (MoHFW). G of B. National Action Plan: Antimicrobial Resistance Containment in Bangladesh 2017–22. Available online: https://cdn.who.int/media/docs/default-source/antimicrobial-resistance/amr-spc-npm/nap-library/antimicrobial-resistance-containment-in-bangladesh-2017-2022.pdf?sfvrsn=bfa46b_3&download=true (accessed on 22 August 2024).
- Habib, Z.H.; Rasul, S.B.G.; Alam, M.A.; Bably, N.N.; Khan, I.A.; Rizvi, S.M.S.; Shirin, T.; Alam, A.N.; Uzzaman, M.S.; Alamgir, A.; et al. The findings of Antimicrobial Resistance Surveillance in Bangladesh (2016–2020). medRxiv 2021. [Google Scholar] [CrossRef]
- Afroz, S.; Habib, Z.H.; Billah, S.M.B.; Akhter, H.; Jahan, H.; Parveen, R. Spectrum and Antibiotic Resistance Pattern of Bacteria Causing Urinary Tract Infections (UTI) in a Tertiary Care Hospital. J. Surg. Sci. 2020, 23, 13–18. [Google Scholar] [CrossRef]
- Nobel, F.; Akter, S.; Jebin, R.; Sarker, T.; Rahman; Zamane, S.; Islam, K.; Sabrina, S.; Akther, N.; Islam, A.; et al. Prevalence of multidrug resistance patterns of Escherichia coli from suspected urinary tract infection in Mymensingh city, Bangladesh. J. Adv. Biotechnol. Exp. Ther. 2021, 4, 256. [Google Scholar] [CrossRef]
- Bangladesh Post. Bangladesh Post 2020, PM Joins as Co-Chair of Antimicrobial Resistance Group, Bangladesh Post. Available online: https://bangladeshpost.net/posts/pm-joins-as-co-chair-of-antimicrobial-resistance-group-47600 (accessed on 22 August 2024).
- WHONET. Internet. Available online: https://whonet.org (accessed on 10 August 2024).
- SQLite Database Browser. Internet. Available online: https://www.sqlite.org/about.html (accessed on 4 April 2024).
- Quick Analysis of Antimicrobial Patterns and Trends (QAAPT). Internet. Available online: https://qaapt.com (accessed on 5 March 2024).
- Stata Corporation. Stata Statistical Software: Release 18; StataCorp LLC: College Station, TX, USA, 2023. [Google Scholar]
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Haque, R.; Akter, M.L.; Salam, M.A. Prevalence and susceptibility of uropathogens: A recent report from a teaching hospital in Bangladesh. BMC Res. Notes 2015, 8, 416. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Han, S.W.; Kim, K.W.; Song, D.Y.; Kwon, K.T. Third-generation cephalosporin resistance of community-onset Escherichia coli and Klebsiella pneumoniae bacteremia in a secondary hospital. Korean J. Int. Med. 2014, 29, 49. [Google Scholar] [CrossRef] [PubMed]
- Rahaman, R.; Alroy, K.A.; Van Beneden, C.A.; Friedman, M.S.; Kennedy, E.D.; Rahman, M.; Balajee, A.; Muraduzzaman, A.; Shirin, T.; Flora, M.S.; et al. Etiology of Severe Acute Respiratory Infections, Bangladesh, 2017. Emerg. Infect. Dis. 2021, 27, 324–326. [Google Scholar] [CrossRef]
- Tanni, A.A.; Hasan, M.d.M.; Sultana, N.; Ahmed, W.; Mannan, A. Prevalence and molecular characterization of antibiotic resistance and associated genes in Klebsiella pneumoniae isolates: A clinical observational study in different hospitals in Chattogram, Bangladesh. PLoS ONE 2021, 16, e0257419. [Google Scholar] [CrossRef]
- Hu, F.-P.; Guo, Y.; Zhu, D.-M.; Wang, F.; Jiang, X.-F.; Xu, Y.-C.; Zhang, X.-J.; Zhang, C.-X.; Ji, P.; Xie, Y.; et al. Resistance trends among clinical isolates in China reported from CHINET surveillance of bacterial resistance, 2005–2014. Clin. Microbiol. Infect. 2016, 22, S9–S14. [Google Scholar] [CrossRef]
- Ifa, I.A.; Paul, S.K.; Hossain, M.A.; Haque, N.; Ahmed, S.; Nasreen, S.A.; Ahamed, F.; Roy, S.; Sakib, N.; Abedin, S.; et al. Isolation of Acinetobacter species from Clinical Specimens with Detection of Their Antimicrobial Susceptibility Pattern from a Tertiary Care Hospital, Bangladesh. Mymensingh Med. J. 2020, 29, 622–627. [Google Scholar] [PubMed]
- Rahman, M.H.; Ahmed, M.; Sarkar, D.; Rahman, M.A. Prevalence and antibiotic susceptibility pattern of pathogens from urinary tract infections (UTI) in a private diagnostic laboratory in Bangladesh. Asian J. Med. Biol. Res. 2020, 6, 564–569. [Google Scholar] [CrossRef]
| Characteristics | Frequency n = 4403 | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 1711 | 38.86 |
| Female | 2692 | 61.14 |
| Age group | ||
| ≤4 years | 587 | 13.33 |
| 5–14 years | 770 | 17.49 |
| 15–24 years | 659 | 14.97 |
| 25–34 years | 659 | 14.97 |
| 35–44 years | 538 | 12.22 |
| 45–54 years | 462 | 10.49 |
| 55–64 years | 367 | 8.34 |
| 65–74 years | 361 | 8.20 |
| Age category | ||
| Adult | 2829 | 64.25 |
| Pediatric | 1574 | 35.75 |
| Yearly AST | ||
| 2017 | 976 | 22.17 |
| 2018 | 1560 | 35.43 |
| 2019 | 1644 | 37.34 |
| 2020 | 223 | 5.06 |
| Location type | ||
| Inpatient | 2376 | 53.96 |
| Outpatient | 2027 | 46.04 |
| Specimen type | ||
| Urine | 3155 | 71.66 |
| Pus | 512 | 11.63 |
| Sputum | 295 | 6.70 |
| Wound swab | 295 | 6.70 |
| Stool | 84 | 1.91 |
| Endotracheal aspirate | 53 | 1.20 |
| Blood | 9 | 0.20 |
| Most common organisms | ||
| Escherichia coli | 1378 | 31.30 |
| Proteus sp. | 1075 | 24.42 |
| Klebsiella sp. | 840 | 19.08 |
| Pseudomonas sp. | 453 | 10.29 |
| Acinetobacter sp. | 230 | 5.22 |
| Staphylococcus aureus | 193 | 4.38 |
| Enterococcus sp. | 78 | 1.77 |
| Bacterial | Types of Specimens | |||||
|---|---|---|---|---|---|---|
| Urine (n = 3155) | Pus (n = 512) | Sputum (n = 295) | Wound (n = 295) | Endotracheal Aspirate (n = 53) | Blood (n = 9) | |
| Escherichia coli | 1277 (40.48%) | 70 (13.67%) | 3 (1.02%) | 28 (9.49%) | - | - |
| Proteus sp. | 905 (28.68%) | 93 (18.16%) | 31 (10.51%) | 44 (14.92%) | 2 (3.77%) | - |
| Klebsiella sp. | 525 (16.64%) | 83 (16.21%) | 166 (56.27%) | 44 (14.92%) | 22 (41.51%) | - |
| Pseudomonas sp. | 216 (6.85%) | 84 (16.41%) | 52 (17.63%) | 94 (31.86%) | 7 (13.21%) | - |
| Acinetobacter sp. | 118 (3.74%) | 46 (8.98%) | 15 (5.08%) | 37 (12.54%) | 14 (26.42%) | - |
| Enterococcus sp. | 69 (2.19%) | 5 (0.98%) | 1 (0.34%) | 2 (0.68%) | 1 (1.89%) | - |
| Staphylococcus aureus | 12 (0.38%) | 105 (20.51%) | 23 (7.80%) | 42 (14.24%) | 7 (13.21%) | 4 (44.44%) |
| Antibiotics | Bacterial Species Antibiotic Resistance/Total (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Gram-Negative | Gram Positive | |||||||
| Escherichia coli | Klebsiella sp. | Pseudomonas sp. | Proteus sp. | Salmonella sp. | Acinetobacter sp. | Staphylococcus aureus | Enterococcus sp. | |
| Amikacin | 8.92 (34/381) | 10.57 (28/265) | 19.05 (24/126) | 8.70 (26/299) | - | 27.12 (16/59) | - | - |
| Amoxicillin/clavulanic acid | 80.66 (926/1148) | 82.34 (592/719) | 90.60 (212/234) | 81.14 (766/944) | 80.36 (45/56) | 88.65 (125/141) | - | - |
| Ampicillin | 95.05 (96/101) | 100.00 (57/57) | - | 96.23 (51/53) | - | - | - | - |
| Azithromycin | 53.69 (189/352) | 47.69 (124/260) | 57.14 (72/126) | 60.84 (160/263) | 72.22 (26/36) | 71.05 (54/76) | 78.07 (89/114) | 74.29 (26/35) |
| Aztreonam | 55.17 (64/116) | 72.73 (72/99) | 67.92 (36/53) | 63.30 (69/109) | - | 85.71 (18/21) | - | - |
| Cefepime | 62.86 (132/210) | 67.81 (99/146) | 81.25 (52/64) | 74.84 (116/155) | - | 90.20 (46/51) | - | - |
| Cefoxitin | - | - | - | - | - | - | 85.71 (72/84) | - |
| Cefixime | 71.24 (109/153) | 77.12 (91/118) | 93.55 (58/62) | 71.96 (77/107) | - | 77.78 (21/27) | - | - |
| Ceftazidime | 68.23 (204/299) | 80.56 (145/180) | 80.80 (101/125) | 58.90 (129/219) | - | 92.73 (51/55) | - | - |
| Ceftriaxone | 57.46 (470/818) | 64.66 (311/481) | 73.90 (201/272) | 60.53 (414/684) | 42.22 (19/45) | 87.74 (93/106) | - | - |
| Cefuroxime | 90.28 (892/988) | 92.21 (568/616) | 96.21 (279/290) | 91.45 (770/842) | 88.00 (44/50) | 98.18 (162/165) | - | - |
| Ciprofloxacin | 46.31 (477/1030) | 32.32 (213/659) | 31.03 (108/348) | 32.91 (282/857) | 24.56 (14/57) | 59.49 (94/158) | 54.78 (86/157) | 55.77 (29/52) |
| Doxycycline | 48.96 (47/96) | 51.16 (44/86) | 72.41 (21/29) | 47.06 (40/85) | - | 33.33 (21/63) | - | - |
| Erythromycin | - | - | - | - | - | - | 86.84 (33/38) | - |
| Gentamicin | 17.51 (163/931) | 21.46 (115/536) | 27.78 (90/324) | 17.80 (141/792) | 8.33 (4/48) | 56.05 (88/157) | 32.43 (36/111) | 37.21 (16/43) |
| Imipenem | 14.29 (51/357) | 19.79 (57/288) | 27.03 (60/222) | 23.17 (73/315) | - | 36.75 (43/117) | - | - |
| Levofloxacin | 35.94 (23/64) | 29.79 (14/47) | 19.23 (5/26) | 39.58 (19/48) | - | - | - | - |
| Linezolid | - | - | - | - | - | - | 24.70 (41/166) | 48.21 (27/56) |
| Meropenem | 14.17 (18/127) | 7.55 (8/106) | 13.70 (10/73) | 15.12 (13/86) | - | 13.64 (3/22) | - | - |
| Nalidixic acid | 71.43 (40/56) | 53.97 (34/63) | 93.33 (28/30) | 77.27 (34/44) | 72.09 (31/43) | - | - | - |
| Nitrofurantoin | 15.35 (177/1153) | 32.79 (161/491) | 67.89 (129/190) | 35.14 (292/831) | - | 66.33 (65/98) | - | 16.67 (11/66) |
| Norfloxacin | 57.14 (8/14) | 66.67 (10/15) | - | - | - | - | - | - |
| Ofloxacin | 38.30 (18/47) | 25.00 (6/24) | - | 17.14 (6/35) | - | - | - | - |
| Oxacillin | - | - | - | - | - | - | 86.11 (31/36) | - |
| Piperacillin | 94.12 (16/17) | 81.12 (116/143) | - | - | 92.65 (63/68) | - | - | |
| Piperacillin/Tazobactam | 63.46 (33/52) | 79.73 (59/74) | 66.86 (226/338) | 71.88 (46/64) | - | 80.00 (64/80) | - | - |
| Penicillin G | - | - | - | - | - | - | 95.24 (40/42) | 95.00 (19/20) |
| Tetracycline | 56.79 (163/287) | 52.41 (98/187) | 77.01 (67/87) | 51.87 (111/214) | - | 41.79 (28/67) | 30.77 (8/26) | 42.31 (11/26) |
| Trimethoprim/Sulfamethoxazole | 72.12 (119/165) | 73.00 (73/100) | 71.43 (20/28) | 72.57 (82/113) | - | - | - | - |
| Vancomycin | - | - | - | - | - | - | 9.68 (9/93) | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roy, S.; Barua, H.T.; Sujan, M.J.; Hossain, A.; Paul, S.K.; Nasreen, S.A.; Ahmed, S.; Haque, N.; Habib, Z.H.; Rahman, A.; et al. Trends and Patterns of Antimicrobial Resistance in a Tertiary Care Hospital in Bangladesh. Microbiol. Res. 2025, 16, 30. https://doi.org/10.3390/microbiolres16020030
Roy S, Barua HT, Sujan MJ, Hossain A, Paul SK, Nasreen SA, Ahmed S, Haque N, Habib ZH, Rahman A, et al. Trends and Patterns of Antimicrobial Resistance in a Tertiary Care Hospital in Bangladesh. Microbiology Research. 2025; 16(2):30. https://doi.org/10.3390/microbiolres16020030
Chicago/Turabian StyleRoy, Sangjukta, Hridika Talukder Barua, Mohammad Julhas Sujan, Akram Hossain, Shyamal Kumar Paul, Syeda Anjuman Nasreen, Salma Ahmed, Nazia Haque, Zakir Hossain Habib, Aninda Rahman, and et al. 2025. "Trends and Patterns of Antimicrobial Resistance in a Tertiary Care Hospital in Bangladesh" Microbiology Research 16, no. 2: 30. https://doi.org/10.3390/microbiolres16020030
APA StyleRoy, S., Barua, H. T., Sujan, M. J., Hossain, A., Paul, S. K., Nasreen, S. A., Ahmed, S., Haque, N., Habib, Z. H., Rahman, A., Rizvi, S. M. S., Hasnat, M. A., Kwon, S. Y., Stelling, J., Gautam, S., Shaw, A., Marks, F., & Poudyal, N. (2025). Trends and Patterns of Antimicrobial Resistance in a Tertiary Care Hospital in Bangladesh. Microbiology Research, 16(2), 30. https://doi.org/10.3390/microbiolres16020030







