The New Reality of Infective Endocarditis: Changes in Patient Demographics and Outcomes in South Carolina
Abstract
1. Introduction
2. Methods
2.1. Data Sources and Definitions
2.2. Statistical Analyses
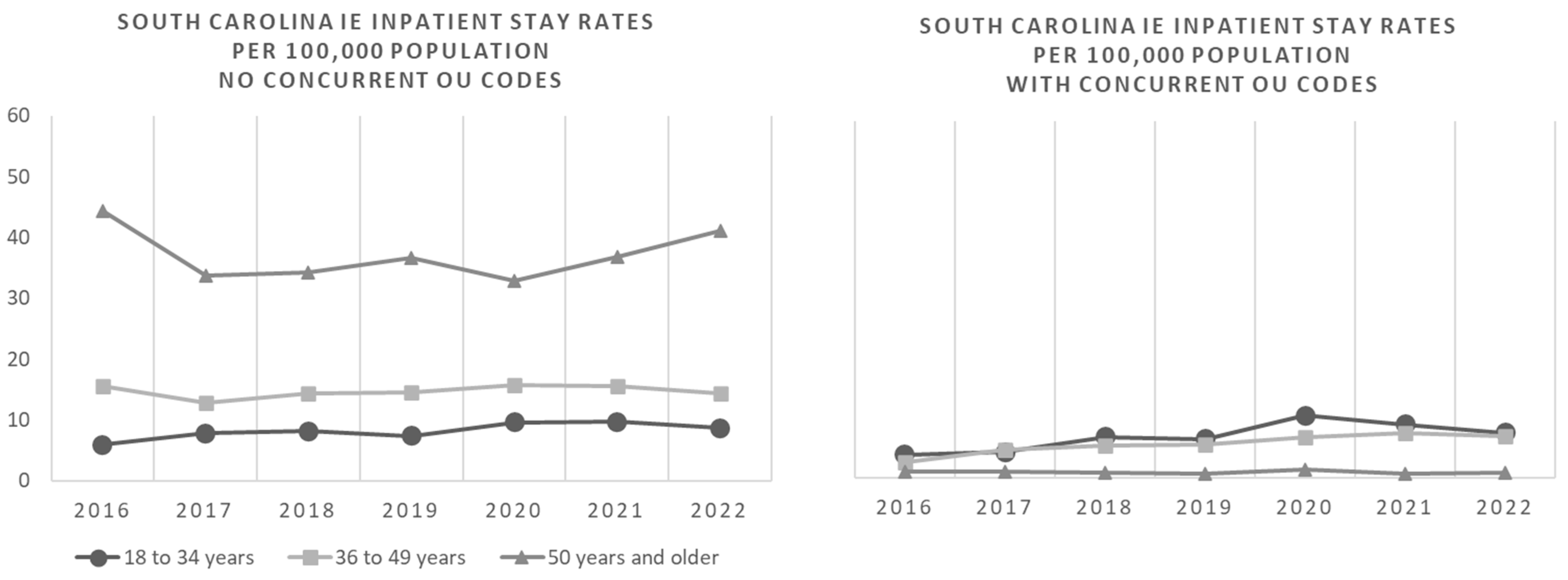
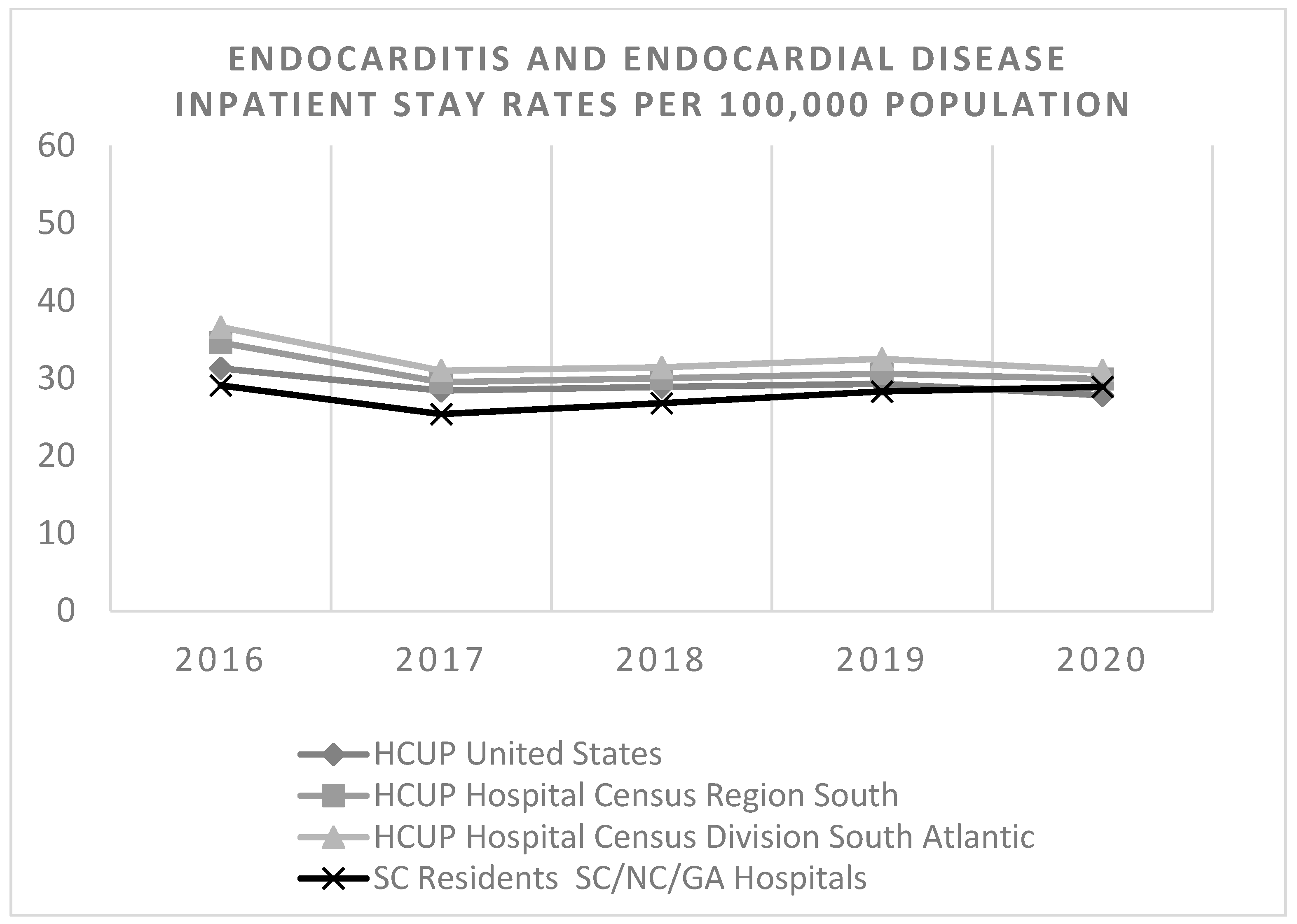
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| ICD-10-CM Code | ICD-10-CM Code Description |
|---|---|
| A3282 | Listerial endocarditis |
| A3951 | Meningococcal endocarditis |
| A5203 | Syphilitic endocarditis |
| A5483 | Gonococcal heart infection |
| B3321 | Viral endocarditis |
| B376 | Candidal endocarditis |
| I011 | Acute rheumatic endocarditis |
| I330 | Acute and subacute infective endocarditis |
| I339 | Acute and subacute endocarditis, unspecified |
| I38 | Endocarditis, valve unspecified |
| I39 | Endocarditis and heart valve disorders in diseases classified elsewhere |
| M3211 | Endocarditis in systemic lupus erythematosus |
| F111 * | Opioid abuse |
| F112 * | Opioid dependence |
| F119 * | Opioid use |
| T400X * | Poisoning by, adverse effect of and underdosing of opium |
| T401X * | Poisoning by and adverse effect of heroin |
| T402X * | Poisoning by, adverse effect of and underdosing of other opioids |
| T403X * | Poisoning by, adverse effect of and underdosing of methadone |
| T404 * | Poisoning by, adverse effect of and underdosing of synthetic narcotics |
| T507X * | Poisoning by, adverse effect of and underdosing of analeptics and opioid receptor antagonists |
References
- Baddour, L.M.; Weimer, M.B.; Wurcel, A.G.; McElhinney, D.B.; Marks, L.R.; Fanucchi, L.C.; Garrigos, Z.E.; Pettersson, G.B.; DeSimone, D.C. Management of Infective Endocarditis in People Who Inject Drugs: A Scientific Statement From the American Heart Association. Circulation 2022, 146, e187–e201. [Google Scholar] [CrossRef]
- Baddour, L.M.; Wilson, W.R.; Bayer, A.S.; Fowler, V.G.; Tleyjeh, I.M.; Rybak, M.J.; Barsic, B.; Lockhart, P.B.; Gewitz, M.H.; Levison, M.E.; et al. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Scientific Statement for Healthcare Professionals From the American Heart Association. Circulation 2015, 132, 1435–1486. [Google Scholar] [CrossRef]
- Hartman, L.; Barnes, E.; Bachmann, L.; Schafer, K.; Lovato, J.; Files, D.C. Opiate Injection-associated Infective Endocarditis in the Southeastern United States. Am. J. Med. Sci. 2016, 352, 603–608. Available online: https://www.sciencedirect.com/science/article/pii/S0002962916304347 (accessed on 20 May 2025). [CrossRef]
- Nenninger, E.K.; Carwile, J.L.; Ahrens, K.A.; Armstrong, B.; Thakarar, K. Rural–Urban Differences in Hospitalizations for Opioid Use–Associated Infective Endocarditis in the United States, 2003–2016. Open Forum Infect. Dis. 2020, 7, ofaa045. [Google Scholar] [CrossRef]
- Chirillo, F.; Scotton, P.; Rocco, F.; Rigoli, R.; Borsatto, F.; Pedrocco, A.; De Leo, A.; Minniti, G.; Polesel, E.; Olivari, Z. Impact of a Multidisciplinary Management Strategy on the Outcome of Patients with Native Valve Infective Endocarditis. Am. J. Cardiol. 2013, 112, 1171–1176. Available online: https://www.sciencedirect.com/science/article/pii/S000291491301285X (accessed on 20 May 2025). [CrossRef]
- Vogel, M.; Schmitz, R.P.H.; Hagel, S.; Pletz, M.W.; Gagelmann, N.; Scherag, A.; Schlattmann, P.; Brunkhorst, F.M. Infectious disease consultation for Staphylococcus aureus bacteremia—A systematic review and meta-analysis. J. Infect. 2016, 72, 19–28. Available online: https://www.sciencedirect.com/science/article/pii/S0163445315003151 (accessed on 20 May 2025). [CrossRef]
- Yamamoto, S.; Hosokawa, N.; Sogi, M.; Inakaku, M.; Imoto, K.; Ohji, G.; Doi, A.; Iwabuchi, S.; Iwata, K. Impact of infectious diseases service consultation on diagnosis of infective endocarditis. Scand. J. Infect. Dis. 2012, 44, 270–275. [Google Scholar] [CrossRef]
- Okura, T.; Iwata, K.; Koyama, T.; Ebisawa, K.; Arakawa, Y.; Kusuki, M.; Ohji, G. Impact of Infectious Disease Consultation on Management and Outcomes of Infective Endocarditis. Ann. Thorac. Surg. 2021, 112, 1228–1234. Available online: https://www.sciencedirect.com/science/article/pii/S0003497520320142 (accessed on 20 May 2025). [CrossRef]
- Walensky, R.P.; McQuillen, D.P.; Shahbazi, S.; Goodson, J.D. Where Is the ID in COVID-19? Ann. Intern. Med. 2020, 173, 587–589. [Google Scholar] [CrossRef]
- Maamari, J.; Chen, Z.; Motairek, I.; Al-Kindi, S.; Fleisher, J. Mapping Proximity to Infectious Disease Physicians Across the United States. Open Forum Infect. Dis. 2024, 11, ofae208. [Google Scholar] [CrossRef]
- Nunes, M.C.P.; Guimarães-Júnior, M.H.; Murta Pinto, P.H.O.; Coelho, R.M.P.; Souza Barros, T.L.; Faleiro Maia Nde, P.A.; Madureira, D.A.; Reis, R.C.P.; Costa, P.H.N.; Bráulio, R.; et al. Outcomes of infective endocarditis in the current era: Early predictors of a poor prognosis. Int. J. Infect. Dis. 2018, 68, 102–107. Available online: https://www.sciencedirect.com/science/article/pii/S1201971218300171 (accessed on 20 May 2025). [CrossRef]
- Shrestha, N.K.; Kim, S.L.; Rehm, S.J.; Everett, A.; Gordon, S.M. Emergency department visits during outpatient parenteral antimicrobial therapy: A retrospective cohort study. J. Antimicrob. Chemother. 2018, 73, 1972–1977. [Google Scholar] [CrossRef]
- Schranz, A.J.; Tak, C.; Wu, L.T.; Chu, V.H.; Wohl, D.A.; Rosen, D.L. The Impact of Discharge Against Medical Advice on Readmission After Opioid Use Disorder-Associated Infective Endocarditis: A National Cohort Study. J. Gen. Intern. Med. 2023, 38, 1615–1622. [Google Scholar] [CrossRef]
- Elixhauser Comorbidity Software; Version 2023.1; Software Refined for Icd-10-cm Diagnoses; Agency for Healthcare Research and Quality Healthcare Cost and Utilization: Rockville, MD, USA, 2022. Available online: https://hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/CMR-User-Guide-v2023-1.pdf (accessed on 20 May 2025).
- Agency for Healthcare Research and Quality. Using Appropriate Price Indices for Analyses of Health Care Expenditures or Income Across Multiple Years. Available online: https://meps.ahrq.gov/about_meps/Price_Index.shtml#t1a1 (accessed on 20 May 2025).
- Clinical Classifications Software Refined (CCSR). Available online: https://hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp (accessed on 20 May 2025).
- Bureau, U.C.; Census.gov. County Population by Characteristics: 2020–2022. Available online: https://www.census.gov/data/tables/time-series/demo/popest/2020s-counties-detail.html (accessed on 20 May 2025).
- HCUPnet Data Tools—Healthcare Cost and Utilization Project (HCUPnet). Available online: https://datatools.ahrq.gov/hcupnet/ (accessed on 20 May 2025).
- Wurcel, A.G.; Anderson, J.E.; Chui, K.K.H.; Skinner, S.; Knox, T.A.; Snydman, D.R.; Stopka, T.J. Increasing Infectious Endocarditis Admissions Among Young People Who Inject Drugs. Open Forum Infect. Dis. 2016, 3, ofw157. [Google Scholar] [CrossRef]
- Siddiqi, K.; Freeman, P.R.; Fanucchi, L.C.; Slavova, S. Rural-urban differences in hospitalizations for opioid use-associated infective endocarditis in Kentucky, 2016–2019. J. Rural. Health 2021, 38, 604–611. [Google Scholar] [CrossRef]
- Wang, L.; Volkow, N.D.; Berger, N.A.; Davis, P.B.; Kaelber, D.C.; Xu, R. Association of COVID-19 with endocarditis in patients with cocaine or opioid use disorders in the US. Mol. Psychiatry 2023, 28, 543–552. [Google Scholar] [CrossRef]
- Bearnot, B.; Mitton, J.A.; Hayden, M.; Park, E.R. Experiences of care among individuals with opioid use disorder-associated endocarditis and their healthcare providers: Results from a qualitative study. J. Subst. Abus. Treat. 2019, 102, 16–22. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0740547218305956 (accessed on 20 May 2025). [CrossRef]
- Serota, D.P.; Rosenbloom, L.; Hervera, B.; Seo, G.; Feaster, D.J.; Metsch, L.R.; Suarez, E.; A Chueng, T.; Hernandez, S.; E Rodriguez, A.; et al. Integrated Infectious Disease and Substance Use Disorder Care for the Treatment of Injection Drug Use–Associated Infections: A Prospective Cohort Study With Historical Control. Open Forum Infect. Dis. 2023, 10, ofac688. [Google Scholar] [CrossRef]
- Javorski, M.J.; Rosinski, B.F.; Shah, S.; Thompson, M.A.; Streem, D.; Gordon, S.M.; Insler, S.; Houghtaling, P.L.; Griffin, B.; Blackstone, E.H.; et al. Infective Endocarditis in Patients Addicted to Injected Opioid Drugs. J. Am. Coll. Cardiol. 2024, 83, 811–823. [Google Scholar] [CrossRef] [PubMed]
- Ganesh, S.S.; Goldshear, J.L.; Wilkins, P.; Kovalsky, E.; Simpson, K.A.; Page, C.J.; Corsi, K.; Ceasar, R.C.; Barocas, J.A.; Bluthenthal, R.N. Risk Factors for Infective Endocarditis and Serious Injection Related Infections Among People Who Inject Drugs in Los Angeles, CA and Denver, CO. Drug Alcohol Depend. 2025, 269, 112588. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shrestha, N.K.; Shrestha, J.; Everett, A.; Carroll, D.; Gordon, S.M.; Butler, R.S.; Rehm, S.J. Vascular access complications during outpatient parenteral antimicrobial therapy at home: A retrospective cohort study. J Antimicrob. Chemother. 2016, 71, 506–512. [Google Scholar] [CrossRef]
- Thakarar, K.; Appa, A.; Abdul Mutakabbir, J.C.; Goff, A.; Brown, J.I.I.I.; Tuell, C.; Fairfield, K.; Wurcel, A. Frame Shift: Focusing on Harm Reduction and Shared Decision Making for People Who Use Drugs Hospitalized with Infections. Clin Infect. Dis. 2024, 78, e12–e26. [Google Scholar] [CrossRef]
- Al-Hasan, M.N.; Rac, H. Transition from intravenous to oral antimicrobial therapy in patients with uncomplicated and complicated bloodstream infections. Clin. Microbiol. Infect. 2020, 26, 299–306. Available online: https://www.sciencedirect.com/science/article/pii/S1198743X19302277 (accessed on 20 May 2025). [CrossRef]
- McDonald, E.G.; Aggrey, G.; Tarık Aslan, A.; Casias, M.; Cortes-Penfield, N.; Dong, M.Q.; Egbert, S.; Footer, B.; Isler, B.; King, M.; et al. Guidelines for Diagnosis and Management of Infective Endocarditis in Adults: A WikiGuidelines Group Consensus Statement. JAMA Netw. Open 2023, 6, e2326366. [Google Scholar] [CrossRef]
- Iversen, K.; Ihlemann, N.; Gill, S.U.; Madsen, T.; Elming, H.; Jensen, K.T.; Bruun, N.E.; Høfsten, D.E.; Fursted, K.; Christensen, J.J.; et al. Partial Oral versus Intravenous Antibiotic Treatment of Endocarditis. N. Engl. J. Med. 2019, 380, 415–424. [Google Scholar] [CrossRef]
- Antosz, K.; Al-Hasan, M.N.; Lu, Z.K.; Tabor, B.; Justo, J.A.; Milgrom, A.; Kohn, J.; Bookstaver, P.B. Clinical Utility and Cost Effectiveness of Long-Acting Lipoglycopeptides Used in Deep-Seated Infections among Patients with Social and Economic Barriers to Care. Pharm. J. Pharm. Educ. Pract. 2021, 10, 1. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8788434/ (accessed on 20 May 2025). [CrossRef]
| Infective Endocarditis Without Concurrent Opioid Use, Abuse, or Dependence Codes | Infective Endocarditis with Concurrent Opioid Use, Abuse, or Dependence Codes | ||||
|---|---|---|---|---|---|
| Number | Percentage | Number | Percentage | Adjusted p-Value * | |
| Inpatient Stays | 6634 | 100.0% | 1047 | 100.0% | |
| Unique Patients | 5441 | − | 721 | − | |
| Sex | |||||
| Males | 3877 | 58.4% | 472 | 45.1% | |
| Females | 2757 | 41.6% | 575 | 54.9% | <0.01 |
| Race | |||||
| White | 4578 | 69.0% | 952 | 90.9% | |
| Black | 1880 | 28.3% | 68 | 6.5% | |
| Other/Missing | 176 | 2.7% | 27 | 2.6% | <0.01 |
| Age Group | |||||
| 18 to 35 | 707 | 10.7% | 599 | 57.2% | |
| 36 to 49 | 912 | 13.7% | 328 | 31.3% | |
| 50 and older | 5015 | 75.6% | 120 | 11.5% | <0.01 |
| Resident Rurality ** | |||||
| Urban | 4983 | 75.3% | 839 | 80.9% | |
| Rural | 1632 | 24.7% | 198 | 19.1% | <0.01 |
| Average Number of Comorbid Conditions | 3.5 | 2.3 | <0.01 | ||
| Study Year | |||||
| 2016 | 1018 | 15.4% | 84 | 8.0% | |
| 2017 | 836 | 12.6% | 110 | 10.5% | |
| 2018 | 880 | 13.3% | 144 | 13.8% | |
| 2019 | 936 | 14.1% | 141 | 13.5% | |
| 2020 | 898 | 13.5% | 209 | 20.0% | |
| 2021 | 989 | 14.9% | 188 | 18.0% | |
| 2022 | 1077 | 16.2% | 171 | 16.3% | <0.01 |
| Patient Disposition Status | |||||
| Expired/Hospice | 1476 | 22.3% | 80 | 7.6% | |
| Left Against Medical Advice | 271 | 4.1% | 340 | 32.5% | |
| Home/Home with Home Health | 3484 | 52.5% | 533 | 50.9% | |
| Other *** | 1403 | 21.2% | 94 | 9.0% | <0.01 |
| Presenting Hospital Bed Size | |||||
| Less than 100 Beds | 630 | 9.5% | 96 | 9.2% | |
| 100–299 Beds | 2638 | 39.8% | 425 | 40.6% | |
| 300 or more Beds | 3366 | 50.7% | 526 | 50.2% | 0.8597 |
| Infective Endocarditis Without Concurrent Opioid Use, Abuse, or Dependence Codes | Infective Endocarditis with Concurrent Opioid Use, Abuse, or Dependence Codes | ||||||
|---|---|---|---|---|---|---|---|
| N | Mean | (95% CL Mean) | N | Mean | (95% CL Mean) | Adjusted p-Value | |
| Where patient discharged home or home with home health | |||||||
| Length of Stay in Days | |||||||
| Acute Hospital Care | 3484 | 15.3 | (14.6, 15.9) | 533 | 32.9 | (31.1, 34.7) | <0.01 |
| Specialty Hospital Care | 202 | 25.1 | (22.6, 27.5) | 33 | 29.9 | (25.6, 34.2) | 0.41 |
| Home healthcare | 1277 | 48.2 | (46.6, 49.9) | 37 | 45.4 | (34.4, 56.5) | 0.89 |
| Sum Hospital and Home Health | 3484 | 34.4 | (33.2, 35.6) | 533 | 37.9 | (35.7, 40.2) | 0.18 |
| Total Charges * | |||||||
| Acute Hospital Care | 3484 | $188,862 | ($180,367, $197,356) | 533 | $308,874 | ($284,052, $333,696) | <0.01 |
| Specialty Hospital Care | 202 | $118,826 | ($105,266, $132,386) | 33 | $187,539 | ($127,388, $247,689) | <0.01 |
| Home healthcare | 1277 | $3427 | ($3263, $3591) | 37 | $2357 | ($1587, $3127) | 0.18 |
| Sum Hospital and Home Health | 3484 | $197,007 | ($188,292, $205,722) | 533 | $320,649 | ($294,338, $346,960) | <0.01 |
| Where patient left against medical advice | |||||||
| Length of Stay in Days | |||||||
| Acute Hospital Care | 271 | 15.2 | (13.0, 17.4) | 340 | 14.2 | (12.7, 15.7) | 0.89 |
| Total Charges * | |||||||
| Acute Hospital Care | 271 | $160,727 | ($134,468, $186,987) | 340 | $134,770 | ($116,957, $152,583) | 0.39 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garrison, G.; Royer, J.; Habicht, M.; Battle, S.; Winders, H.R.; Antosz, K.; Burch, A.-K.; Al-Hasan, M.N.; Justo, J.A.; Bailey, P. The New Reality of Infective Endocarditis: Changes in Patient Demographics and Outcomes in South Carolina. Infect. Dis. Rep. 2025, 17, 67. https://doi.org/10.3390/idr17030067
Garrison G, Royer J, Habicht M, Battle S, Winders HR, Antosz K, Burch A-K, Al-Hasan MN, Justo JA, Bailey P. The New Reality of Infective Endocarditis: Changes in Patient Demographics and Outcomes in South Carolina. Infectious Disease Reports. 2025; 17(3):67. https://doi.org/10.3390/idr17030067
Chicago/Turabian StyleGarrison, Grant, Julie Royer, Max Habicht, Sarah Battle, Hana R. Winders, Kayla Antosz, Anna-Kathryn Burch, Majdi N. Al-Hasan, Julie Ann Justo, and Pamela Bailey. 2025. "The New Reality of Infective Endocarditis: Changes in Patient Demographics and Outcomes in South Carolina" Infectious Disease Reports 17, no. 3: 67. https://doi.org/10.3390/idr17030067
APA StyleGarrison, G., Royer, J., Habicht, M., Battle, S., Winders, H. R., Antosz, K., Burch, A.-K., Al-Hasan, M. N., Justo, J. A., & Bailey, P. (2025). The New Reality of Infective Endocarditis: Changes in Patient Demographics and Outcomes in South Carolina. Infectious Disease Reports, 17(3), 67. https://doi.org/10.3390/idr17030067







