Antimicrobial Peptides Demonstrate Activity against Resistant Bacterial Pathogens
Abstract
:1. Introduction
| Family | AMP | Action | Additional Info |
|---|---|---|---|
| Defensin | Alpha- and beta-defensins Human neutrophil peptides (HNPs) [25] Human enteric defensins | Directly kill phagocytosed microbes. Can enhance the production of inflammatory cytokines, e.g., interleukin-1 [25] | Produced by neutrophils, lymphocytes, and epithelial cells of the skin and mucous membranes [1]. Stored in the azurophilic granules of human neutrophils. Secreted by paneth cells in the small intestinal |
| Cathelicidins | Bactenecins Human cathelicidin LL-37 [9] | Immunomodulatory activity, impacts quorum sensing mechanisms in P. aeruginosa biofilm formation [25], apoptosis induction, inflammasome activation, and phagocytosis [13] LL-37 inhibits Aspergillus fumigatus infection and reduces inflammation [9], LL37 analogue peptides (AC-1, AC-2, LL37-1, and D) effetive against C. albicans yeasts [3] | The bactenecin ChBac3.4 appears more active against bacterial membranes and tumor cells compared to normal cells [26] LL-37 effective against various Gram-positive and Gram-negative bacteria, and AMR species [9] |
| Hepcidins | Human liver-expressed antimicrobial peptide (LEAP) Fish hepcidins HAMP1 and HAMP2 | Antibacterial Iron regulatory mode of action [19] | Type II acute phase protein Results in a reduction in ferroportin expression |
| Histone- histidine-rich peptides | Histatins—cationic peptides secreted into human saliva by salivary glands | Antifungal action, antibacterial [27] | High biocompatibility, effective against azole-resistant fungi [27] |
| Piscidins | Present mainly in the tissues of gills, muscle, head kidney, skin, and intestine [15] | Potent and broad-spectrum [15], antibacterial, antifungal, and antiviral properties | Efficacy toward MDR MRSA, vancomycin-resistant Enterococci, piscidin has antitumor activity against cancer-derived cell lines [15] |
2. Clinical Bacterial Infectious Disease
2.1. AMP Activity against Gram-Positive Pathogens Assoicated with Infectious Disease
| Last-Resort Antibiotic | Mode of Action/Mode of Resistance | Resistant Species | Infectious Disease |
|---|---|---|---|
| Carbapenems, e.g., meropenem | beta-lactams/metallo-beta-lactamases | K. pneumoniae | UTIs, BSIs |
| Polymyxins, e.g., polymyxin B, colistin | Disruptions of LPS/efflux pump, capsule formation, alteration of LPS [57] | K. pneumoniae, E. coli, P. aeruginosa, Salmonella typhimurium [57] | |
| Aztreonam | Inhibition of cell wall synthesis/chromosomally encoded mutations | Inactive against Gram-positive bacteria, resistance seen in P. aeruginosa [58] | Cystic fibrous P. aeruginosa lung infection [58] |
| Cephalosporins of 4th, 5th generation | Beta-lactam rings bind to the penicillin-binding protein and inhibit cell wall formation [59]/hindered by production of beta lactamases | 4th gen, e.g., cefepime, has activity against beta-lactamase expressing bacteria, 5th gen, e.g., ceftaroline active against methicillin-resistant Staphylococci and penicillin-resistant pneumococci [59] | Cefepime has high activity against Enterobacteriaceae that resistant to third-generation cephalosporins, Salmonella ESBL-producing infections [60]. Ceftaroline used to treat osteomyelitis and acute bacterial skin and skin structure infections [61] |
| Tigecycline | 3rd generation tetracycline. glycylcycline antibiotic [62], inhibits protein translation [63]/hindered by production of beta lactamases | Potent action against Gram-positive and Gram-negative bacteria except Proteus and Pseudomonas [62], resistance observed in Klebsiella [63] | Skin and skin structure infections, complicated intra-abdominal infections, and community-acquired pneumonia (CAP) [63] |
| Fosfomycin | Irreversibly inhibits the initial phase of microbial cell wall synthesis [64]/MurA mutations | Active against Gram-positive and Gram-negative bacteria, e.g., vancomycin-resistant enterococci, MRSA, and carbapenem-resistant Enterobacteriaceae. Resistance seen in Acinetobacter species [64] | Treatment or severe soft tissue infections (STIs) in ICUs, serious systemic infections, e.g., acute osteomyelitis, nosocomial lower respiratory tract infections, complicated urinary tract infections, bacterial meningitis, and bacteremia [64] |
| Daptomycin | Cyclic lipopeptide core of 13 amino acids, results in membrane depolarization and subsequent loss of intracellular components [50]/altered membrane composition [6] | Intrinsic resistance to daptomycin in Gram-positive bacteria, daptomycin resistance gene mprF acquired resistance among Enterococcus spp. [50] | Daptomycin may also penetrate immune cells including neutrophils and macrophages—immunomodulatory [50], first-line agent to treat severe VRE infections, antibiofilm activity [50] |
2.2. AMP Activity against Gram-Negative Pathogens Associated with Infectious Disease
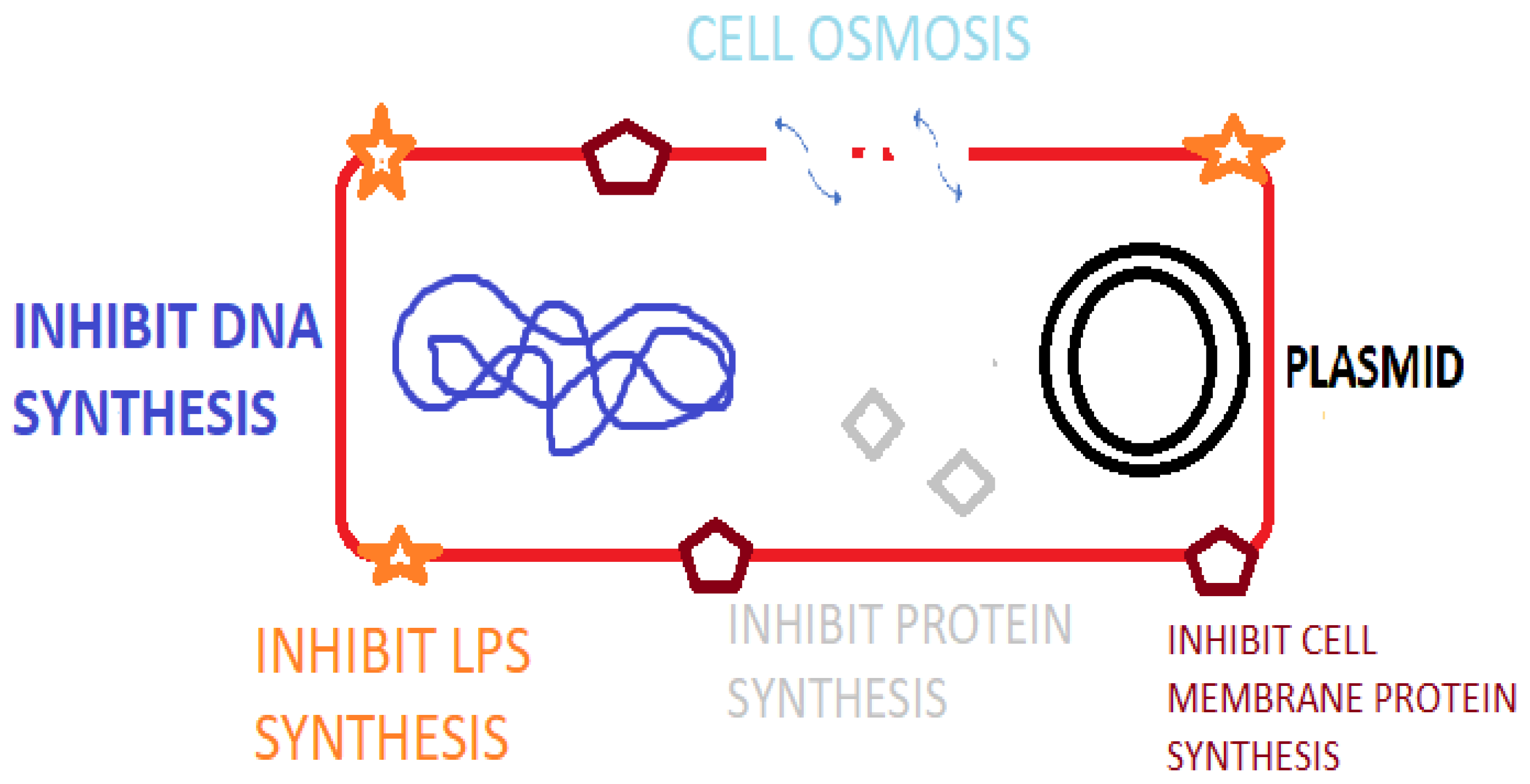
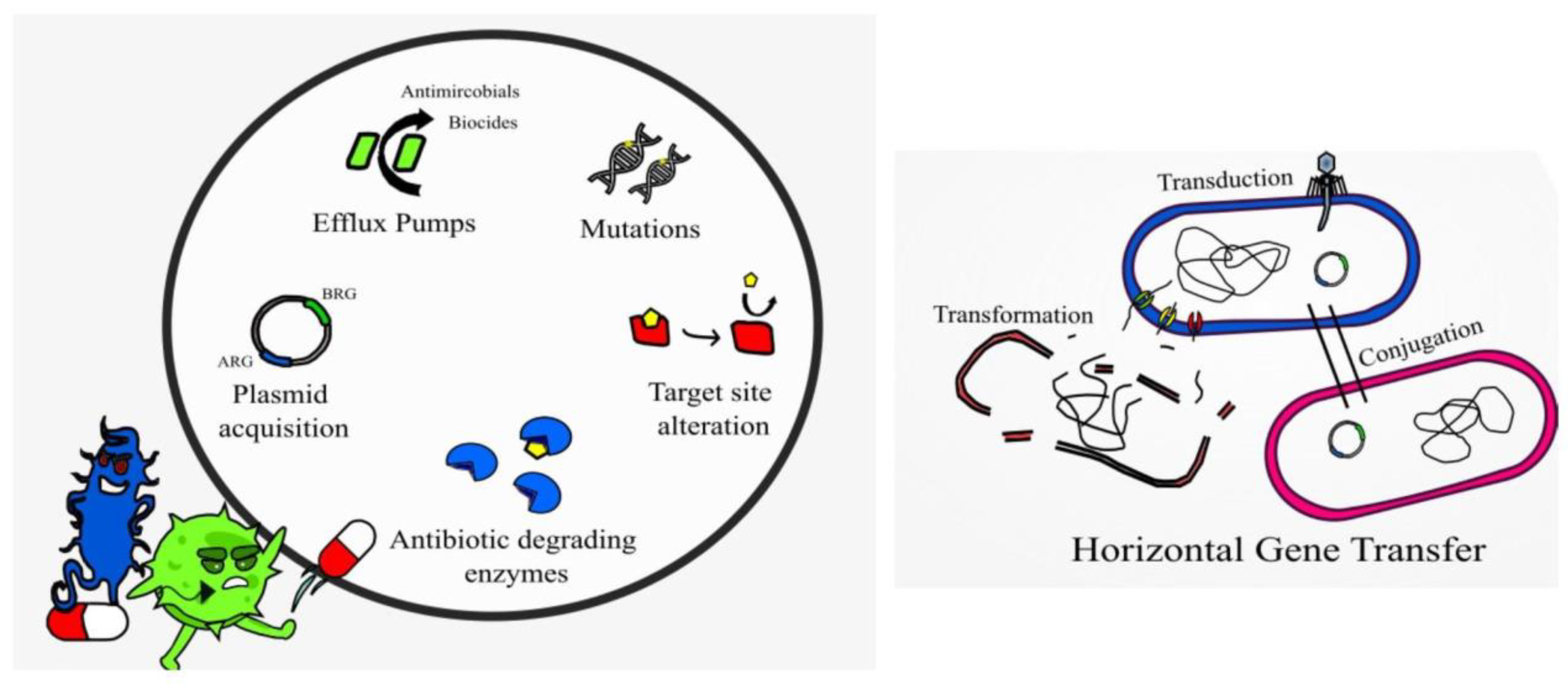
2.3. AMP Resistance
3. Issues Preventing the Application of AMPs as Broad-Spectrum Antimicrobials
3.1. Future Direction of AMP Production and Formulation to Overcome Current Issues
3.2. Pharmacokinetics and Pharmacodynamic Considerations
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guryanova, S.V.; Ovchinnikova, T.V. Immunomodulatory and Allergenic Properties of Antimicrobial Peptides. Int. J. Mol. Sci. 2022, 23, 2499. [Google Scholar] [CrossRef]
- Moravej, H.; Moravej, Z.; Yazdanparast, M.; Heiat, M.; Mirhosseini, A.; Moosazadeh Moghaddam, M.; Mirnejad, R. Antimicrobial Peptides: Features, Action, and Their Resistance Mechanisms in Bacteria. Microb. Drug Resist. 2018, 24, 747–767. [Google Scholar] [CrossRef]
- Pinilla, G.; Coronado, Y.T.; Chaves, G.; Muñoz, L.; Navarrete, J.; Salazar, L.M.; Taborda, C.P.; Muñoz, J.E. In Vitro Antifungal Activity of LL-37 Analogue Peptides against Candida spp. J. Fungi 2022, 7, 1173. [Google Scholar] [CrossRef] [PubMed]
- Decker, A.P.; Mechesso, A.F.; Wang, G. Expanding the Landscape of Amino Acid-Rich Antimicrobial Peptides: Definition, Deployment in Nature, Implications for Peptide Design and Therapeutic Potential. Int. J. Mol. Sci. 2022, 23, 12874. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.Y.; Yan, Z.B.; Meng, Y.M. Antimicrobial peptides: Mechanism of action, activity and clinical potential. Mil. Med. Res. 2021, 8, 48. [Google Scholar] [CrossRef]
- Huang, H.W. Daptomycin, its membrane-active mechanism vs. that of other antimicrobial peptides. Biochim. Biophys. Acta Biomembr. 2020, 1862, 183395. [Google Scholar] [CrossRef] [PubMed]
- Bahar, A.A.; Ren, D. Antimicrobial peptides. Pharmaceuticals 2013, 6, 1543–1575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Le, C.F.; Fang, C.M.; Sekaran, S.D. Intracellular Targeting Mechanisms by Antimicrobial Peptides. Antimicrob. Agents Chemother. 2017, 61, e02340-16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dijksteel, G.S.; Ulrich, M.M.W.; Middelkoop, E.; Boekema, B.K.H.L. Review: Lessons Learned from Clinical Trials Using Antimicrobial Peptides (AMPs). Front. Microbiol. 2021, 12, 616979. [Google Scholar] [CrossRef]
- Tan, L.T.H.; Chan, K.G.; Pusparajah, P.; Lee, W.L.; Chuah, L.H.; Khan, T.M.; Goh, B.H. Targeting Membrane Lipid a Potential Cancer Cure? Front. Pharmacol. 2017, 8, 12. [Google Scholar] [CrossRef] [Green Version]
- Meade, E.; Slattery, M.A.; Garvey, M. Bacteriocins, Potent Antimicrobial Peptides and the Fight against Multi Drug Resistant Species: Resistance Is Futile? Antibiotics 2020, 9, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rončević, T.; Puizina, J.; Tossi, A. Antimicrobial Peptides as Anti-Infective Agents in Pre-Post-Antibiotic Era? Int. J. Mol. Sci. 2019, 20, 5713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fasina, Y.O.; Obanla, T.; Dosu, G.; Muzquiz, S. Significance of Endogenous Antimicrobial Peptides on the Health of Food Animals. Front. Vet. Sci. 2021, 8, 585266. [Google Scholar] [CrossRef]
- Assoni, L.; Milani, B.; Carvalho, M.R.; Nepomuceno, L.N.; Waz, N.T.; Guerra, M.E.S.; Converso, T.R.; Darrieux, M. Resistance Mechanisms to Antimicrobial Peptides in Gram-Positive Bacteria. Front. Microbiol. 2020, 11, 593215. [Google Scholar] [CrossRef]
- Zaccone, G.; Capillo, G.; Fernandes, J.M.O.; Kiron, V.; Lauriano, E.R.; Alesci, A.; Lo Cascio, P.M.C.; Kuciel, M.; Zuwala, K.; Icardo, J.M.; et al. Expression of the Antimicrobial Peptide Piscidin 1 and Neuropeptides in Fish Gill and Skin: A Potential Participation in Neuro-Immune Interaction. Mar. Drugs 2022, 20, 145. [Google Scholar] [CrossRef] [PubMed]
- Kościuczuk, E.M.; Lisowski, P.; Jarczak, J.; Strzałkowska, N.; Jóźwik, A.; Horbańczuk, J.; Krzyżewski, J.; Zwierzchowski, L.; Bagnicka, E. Cathelicidins: Family of antimicrobial peptides. A review. Mol. Biol. Rep. 2012, 39, 10957–10970. [Google Scholar] [CrossRef] [Green Version]
- Zhang, F.; Cui, X.; Fu, Y.; Zhang, J.; Zhou, Y.; Sun, Y. Antimicrobial activity and mechanism of the human milk-sourced peptide Casein201. Biochem. Biophys. Res. Commun. 2017, 485, 698–704. [Google Scholar] [CrossRef]
- Dutta, P.; Sahu, R.K.; Dey, T.; Lahkar, M.D.; Manna, P.; Kalita, J. Beneficial role of insect-derived bioactive components against inflammation and its associated complications (colitis and arthritis) and cancer. Chem. Biol. Interact. 2019, 313, 108824. [Google Scholar] [CrossRef]
- Athira, P.P.; Anooja, V.V.; Anju, M.V.; Neelima, S.; Archana, K.; Muhammed Musthafa, S.; Antony, S.P.; Bright Singh, I.S.; Philip, R. A hepatic antimicrobial peptide, hepcidin from Indian major carp, Catla catla: Molecular identification and functional characterization. J. Genet. Eng. Biotechnol. 2022, 20, 49. [Google Scholar] [CrossRef]
- Koukoulas, K.; Lygoura, V.; Kartalidis, P.; Gatselis, N.K.; Petinaki, E.; Dalekos, G.N.; Simos, G. Hepcidin as a Sensitive and Treatment-Responsive Acute-Phase Marker in Patients with Bacteremia: A Pilot Study. Diagnostics 2022, 12, 1404. [Google Scholar] [CrossRef]
- Dicks, L.; Dreyer, L.; Smith, C.; van Staden, A.D. A Review: The Fate of Bacteriocins in the Human Gastro-Intestinal Tract: Do They Cross the Gut-Blood Barrier? Front. Microbiol. 2018, 9, 2297. [Google Scholar]
- Lbehiry, A.; Marzouk, E.; Abalkhail, A.; El-Garawany, Y.; Anagreyyah, S.; Alnafea, Y.; Almuzaini, A.M.; Alwarhi, W.; Rawway, M.; Draz, A. The Development of Technology to Prevent, Diagnose, and Manage Antimicrobial Resistance in Healthcare-Associated Infections. Vaccines 2022, 8, 2100. [Google Scholar] [CrossRef] [PubMed]
- Garvey, M. Bacteriophages and Food Production: Biocontrol and Bio-Preservation Options for Food Safety. Antibiotics 2022, 11, 1324. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Mechesso, A.F. Realistic and critical review of the state of systemic antimicrobial peptides. ADMET DMPK 2022, 10, 91–105. [Google Scholar] [CrossRef] [PubMed]
- Rima, M.; Rima, M.; Fajloun, Z.; Sabatier, J.-M.; Bechinger, B.; Naas, T. Antimicrobial Peptides: A Potent Alternative to Antibiotics. Antibiotics 2021, 10, 1095. [Google Scholar] [CrossRef]
- Kopeikin, P.M.; Zharkova, M.S.; Kolobov, A.A.; Smirnova, M.P.; Sukhareva, M.S.; Umnyakova, E.S.; Kokryakov, V.N.; Orlov, D.S.; Milman, B.L.; Balandin, S.V.; et al. Caprine Bactenecins as Promising Tools for Developing New Antimicrobial and Antitumor Drugs. Front. Cell. Infect. Microbiol. 2020, 10, 552905. [Google Scholar] [CrossRef]
- Khurshid, Z.; Najeeb, S.; Mali, M.; Moin, S.F.; Raza, S.Q.; Zohaib, S.; Sefat, F.; Zafar, M.S. Histatin peptides: Pharmacological functions and their applications in dentistry. Saudi Pharm. J. Off. Publ. Saudi Pharm. Soc. 2017, 25, 25–31. [Google Scholar] [CrossRef] [Green Version]
- Rabaan, A.A.; Eljaaly, K.; Alhumaid, S.; Albayat, H.; Al-Adsani, W.; Sabour, A.A.; Alshiekheid, M.A.; Al-Jishi, J.M.; Khamis, F.; Alwarthan, S.; et al. An Overview on Phenotypic and Genotypic Characterisation of Carbapenem-Resistant Enterobacterales. Medicina 2022, 58, 1675. [Google Scholar] [CrossRef]
- Calbo, E.; Boix-Palop, L.; Garau, J. Clinical and economic impact of bacterial resistance: An approach to infection control and antimicrobial stewardship solutions. Curr. Opin. Infect. Dis. 2020, 33, 458–463. [Google Scholar] [CrossRef]
- Jeck, J.; Wingen-Heimann, S.M.; Jakobs, F.; Franz, J.; Baltin, C.T.; Kron, A.; Böll, B.; Kochanek, M.; Cornely, O.A.; Kron, F. Last Resort Antibiotics Costs and Reimbursement Analysis of Real-Life ICU Patients with Pneumonia Caused by Multidrug-Resistant Gram-Negative Bacteria in Germany. Healthcare 2022, 10, 2546. [Google Scholar] [CrossRef]
- Ahmed, N.; Khalid, H.; Mushtaq, M.; Basha, S.; Rabaan, A.A.; Garout, M.; Halwani, M.A.; Al Mutair, A.; Alhumaid, S.; Al Alawi, Z.; et al. The Molecular Characterization of Virulence Determinants and Antibiotic Resistance Patterns in Human Bacterial Uropathogens. Antibiotics 2022, 11, 516. [Google Scholar] [CrossRef]
- Li, C.; Wang, J.; Wang, Q.; Liu, B.; Dang, H.; Li, J.; Hou, D. Predictive Value of a Quick Pitt Bacteremia Score for Prognosis of Patients with Bloodstream Infection Secondary to Urinary Tract Infection: A Retrospective Cohort Study. Infect. Drug Resist. 2022, 15, 4381–4391. [Google Scholar] [CrossRef] [PubMed]
- Mark, D.G.; Hung, Y.Y.; Salim, Z. Third-generation cephalosporin resistance and associated discordant antibiotic treatment in emergency department febrile urinary tract infections. Ann. Emerg. Med. 2021, 78, 357–369. [Google Scholar] [CrossRef] [PubMed]
- Nordmann, P.; Poirel, L. Epidemiology and diagnostics of carbapenem resistance in Gram-negative bacteria. Clin. Infect. Dis. 2019, 69 (Suppl. S7), S521–S528. [Google Scholar] [CrossRef] [Green Version]
- Yusof, N.Y.; Norazzman, N.I.I.; Hakim, S.N.W.A.; Azlan, M.M.; Anthony, A.A.; Mustafa, F.H.; Ahmed, N.; Rabaan, A.A.; Almuthree, S.A.; Alawfi, A.; et al. Prevalence of Mutated Colistin-Resistant Klebsiella pneumoniae: A Systematic Review and Meta-Analysis. Trop. Med. Infect. Dis. 2022, 7, 414. [Google Scholar] [CrossRef]
- GBD. Global mortality associated with 33 bacterial pathogens in 2019: A systematic analysis for the Global Burden of Disease Study 2019 GBD 2019 Antimicrobial Resistance Collaborators. Lancet 2022, 400, 2221–2248. [Google Scholar] [CrossRef]
- Mohapatra, S.S.; Dwibedy, S.K.; Padhy, I. Polymyxins, the last-resort antibiotics: Mode of action, resistance emergence, and potential solutions. J. Biosci. 2021, 46, 85. [Google Scholar] [CrossRef]
- Lei, M.; Jayaraman, A.; Van Deventer, J.A.; Lee, K. Annual Review of Biomedical Engineering Engineering Selectively Targeting Antimicrobial Peptides. Annu. Rev. Biomed. Eng. 2021, 23, 339–357. [Google Scholar] [CrossRef]
- Malanovic, N.; Lohner, K. Antimicrobial Peptides Targeting Gram-Positive Bacteria. Pharmaceuticals 2016, 9, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reiners, J.; Lagedroste, M.; Gottstein, J.; Adeniyi, E.T.; Kalscheuer, R.; Poschmann, G.; Stühler, K.; Smits Sander, H.J.; Schmitt, L. Insights in the Antimicrobial Potential of the Natural Nisin Variant Nisin H. Front. Microbiol. 2020, 11, 573614. [Google Scholar] [CrossRef]
- Mokoena, M.P. Lactic Acid Bacteria and Their Bacteriocins: Classification, Biosynthesis and Applications against Uropathogens: A Mini-Review. Molecules 2017, 22, 1255. [Google Scholar] [CrossRef] [Green Version]
- Patrulea, V.; Borchard, G.; Jordan, O. An Update on Antimicrobial Peptides (AMPs) and Their Delivery Strategies for Wound Infections. Pharmaceutics 2020, 12, 12840. [Google Scholar] [CrossRef] [PubMed]
- Laulund, A.S.; Schwartz, F.A.; Christophersen, L.; Høiby, N.; Svendsen, J.S.M.; Stensen, W.; Thomsen, K.; Cavanagh, J.P.; Moser, C. Lactoferricin-inspired peptide AMC-109 augments the effect of ciprofloxacin against Pseudomonas aeruginosa biofilm in chronic murine wounds. J. Glob. Antimicrob. Resist. 2022, 29, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Zhang, Y.; Mao, Q.; Huang, Z.; Yan, T.; Lin, T.; Chen, W.; Wang, Y.; Cai, X.; Liang, Y. Peptide–Polymer Conjugates: A Promising Therapeutic Solution for Drug-Resistant Bacteria. Int. J. Polym. Sci. 2022, 2022, 7610951. [Google Scholar] [CrossRef]
- Xin, B.; Zheng, J.; Liu, H.; Li, J.; Ruan, L.; Peng, D.; Sajid, M.; Sun, M. Thusin, a Novel Two-Component Lantibiotic with Potent Antimicrobial Activity against Several Gram-Positive Pathogens. Front. Microbiol. 2016, 7, 1115. [Google Scholar] [CrossRef] [Green Version]
- Benítez-Chao, D.F.; León-Buitimea, A.; Lerma-Escalera, J.A.; Morones-Ramírez, J.R. Bacteriocins: An Overview of Antimicrobial, Toxicity, and Biosafety Assessment by in vivo Models. Front. Microbiol. 2021, 12, 630695. [Google Scholar] [CrossRef] [PubMed]
- Ongey, E.L.; Neubauer, P. Lanthipeptides: Chemical synthesis versus in vivo biosynthesis as tools for pharmaceutical production. Microb. Cell Factories 2016, 15, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewies, A.; Wentzel, J.F.; Jordaan, A.; Bezuidenhout, C.; Du Plessis, L.H. Interactions of the antimicrobial peptide nisin Z with conventional antibiotics and the use of nanostructured lipid carriers to enhance antimicrobial activity. Int. J. Pharm. 2017, 526, 244–253. [Google Scholar] [CrossRef]
- Santos, C.; Rodriques, G.R.; Lima, L.F.; dos Reis, M.C.G.; Cunha, N.B.; Dias, S.C.; Franco, O.L. Advances and perspectives for antimicrobial peptide and combinatory therapies. Front. Bioeng. Biotechnol. 2020, 10, 1051456. [Google Scholar] [CrossRef]
- Heidary, M.; Khosravi, A.D.; Khoshnood, S.; Nasiri, M.J.; Soleimani, S.; Goudarzi, M. Daptomycin. J. Antimicrob. Chemother. 2018, 73, 1–11. [Google Scholar] [CrossRef]
- Barreto-Santamaria, A.; Patarroyo, M.E.; Curtidor, H. Designing and optimizing new antimicrobial peptides: All targets are not the same. Crit. Rev. Clin. Lab. Sci. 2019, 56, 351–373. [Google Scholar] [CrossRef] [PubMed]
- Mehta, K.; Sharma, P.; Mujawar, S.; Vyas, A. Role of Antimicrobial Peptides in Treatment and Prevention of Mycobacterium Tuberculosis: A Review. Int. J. Pept. Res. Ther. 2022, 28, 132. [Google Scholar] [CrossRef] [PubMed]
- Dong, N.; Wang, C.; Zhang, T.; Zhang, L.; Xue, C.; Feng, X.; Bi, C.; Shan, A. Bioactivity and Bactericidal Mechanism of Histidine-Rich β-Hairpin Peptide Against Gram-Negative Bacteria. Int. J. Mol. Sci. 2019, 20, 3954. [Google Scholar] [CrossRef] [Green Version]
- Pereira, A.G.; Jaramillo, M.L.; Remor, A.P.; Latini, A.; Davico, C.E.; da Silva, M.L.; Müller, Y.M.R.; Ammar, D. Low-concentration exposure to glyphosate-based herbicide modulates the complexes of the mitochondrial respiratory chain and induces mitochondrial hyperpolarization in the Danio rerio brain. Chemosphere 2018, 209, 353–362. [Google Scholar] [CrossRef]
- Rizzetto, G.; Gambini, D.; Maurizi, A.; Candelora, M.; Molinelli, E.; Cirioni, O.; Brescini, L.; Giacometti, A.; Offidani, A.; Simonetti, O. Our Experience over 20 Years: Antimicrobial Peptides against Gram Positives, Gram Negatives, and Fungi. Pharmaceutics 2023, 15, 40. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Mishra, B.; Lau, K.; Lushnikova, T.; Golla, R.; Wang, X. Antimicrobial peptides in 2014. Pharmaceuticals 2015, 8, 123–150. [Google Scholar] [CrossRef]
- Trimble, M.J.; Mlynárčik, P.; Kolář, M.; Hancock, R.E. Polymyxin: Alternative Mechanisms of Action and Resistance. Cold Spring Harb. Perspect. Med. 2016, 6, a025288. [Google Scholar] [CrossRef] [Green Version]
- Jorth, P.; McLean, K.; Ratjen, A.; Secor, P.R.; Bautista, G.E.; Ravishankar, S.; Salipante, S.J. Evolved Aztreonam Resistance Is Multifactorial and Can Produce Hypervirulence in Pseudomonas aeruginosa. MBio 2017, 8, 10–1128. [Google Scholar] [CrossRef] [Green Version]
- Bui, T.; Preuss, C.V. Cephalosporins; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Fu, Y.; Xu, X.; Zhang, L.; Xiong, Z.; Ma, Y.; Wei, Y.; Zhang, J. Fourth Generation Cephalosporin Resistance Among Salmonella enterica Serovar Enteritidis Isolates in Shanghai, China Conferred by blaCTX–M–55 Harboring Plasmids. Front. Microbiol. 2020, 11, 910. [Google Scholar] [CrossRef]
- Johnson, L.B.; Ramani, A.; Guervil, D.J. Use of Ceftaroline Fosamil in Osteomyelitis: CAPTURE Study Experience. BMC Infect. Dis. 2019, 19, 183. [Google Scholar] [CrossRef] [Green Version]
- Yu, R.; Zhang, Y.; Xu, Y.; Schwarz, S.; Li, X.S.; Shang, Y.H. Emergence of a tet(M) variant conferring resistance to Tigecycline in Streptococcus suis. Front. Vet. Sci. 2021, 8, 709327. [Google Scholar] [CrossRef] [PubMed]
- Anyanwu, M.U.; Nwobi, O.C.; Okpala, C.O.R.; Ezeonu, I.M. Mobile Tigecycline Resistance: An Emerging Health Catastrophe Requiring Urgent One Health Global Intervention. Front. Microbiol. 2022, 13, 808744. [Google Scholar] [CrossRef]
- Hashemian, S.M.R.; Farhadi, Z.; Farhadi, T. Fosfomycin: The characteristics, activity, and use in critical care. Ther. Clin. Risk Manag. 2019, 15, 525–530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bobde, S.S.; Alsaab, F.M.; Wang, G.; Van Hoek, M.L. Ab initio Designed Antimicrobial Peptides Against Gram-Negative Bacteria. Front. Microbiol. 2021, 12, 3460. [Google Scholar] [CrossRef] [PubMed]
- Gorr, S.U.; Brigman, H.V.; Anderson, J.C.; Hirsch, E.B. The antimicrobial peptide DGL13K is active against drug-resistant gram-negative bacteria and sub-inhibitory concentrations stimulate bacterial growth without causing resistance. PLoS ONE 2022, 17, e0273504. [Google Scholar] [CrossRef]
- Han, Y.; Zhang, M.; Lai, R.; Zhang, Z. Chemical modifications to increase the therapeutic potential of antimicrobial peptides. Peptides 2021, 146, 170666. [Google Scholar] [CrossRef]
- Gan, B.H.; Gaynord, J.; Rowe, S.M.; Deingruber, T.; Spring, D.R. The multifaceted nature of antimicrobial peptides: Current synthetic chemistry approaches and future directions. Chem. Soc. Rev. 2021, 50, 7820–7880. [Google Scholar] [CrossRef]
- Moffatt, J.H.; Harper, M.; Boyce, J.D. Mechanisms of polymyxin resistance. Adv. Exp. Med. Biol. 2019, 1145, 55–71. [Google Scholar]
- Rodríguez-Rojas, A.; Baeder, D.Y.; Johnston, P.; Regoes, R.R.; Rolff, J. Bacteria primed by antimicrobial peptides develop tolerance and persist. PLoS Pathog. 2021, 17, e1009443. [Google Scholar] [CrossRef]
- Wibowo, D.; Zhao, C.X. Recent achievements and perspectives for large-scale recombinant production of antimicrobial peptides. Appl. Microbiol. Biotechnol. 2018, 103, 659–671. [Google Scholar] [CrossRef] [Green Version]
- Sinha, R.; Shukla, P. Antimicrobial Peptides: Recent Insights on Biotechnological Interventions and Future Perspectives. Protein Pept. Lett. 2019, 26, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; de la Fuente-Nunez, C.; Ou, R.W.; Torres, M.D.; Pande, S.G.; Sinskey, A.J.; Lu, T.K. Yeast-based synthetic biology platform for antimicrobial peptide production. ACS Synth. Biol. 2018, 7, 896–902. [Google Scholar] [CrossRef] [PubMed]
- Shanmugaraj, B.; Bulaon, C.J.I.; Malla, A.; Phoolcharoen, W. Biotechnological Insights on the Expression and Production of Antimicrobial Peptides in Plants. Molecules 2021, 26, 4032. [Google Scholar] [CrossRef]
- Garvey, M. Non-Mammalian Eukaryotic Expression Systems Yeast and Fungi in the Production of Biologics. J. Fungi 2022, 8, 1179. [Google Scholar] [CrossRef]
- Kim, D.S.; Kim, S.W.; Song, J.M.; Kim, S.Y.; Kwon, K.C. A new prokaryotic expression vector for the expression of antimicrobial peptide abaecin using SUMO fusion tag. BMC Biotechnol. 2019, 19, 13. [Google Scholar] [CrossRef] [PubMed]
- Käßer, L.; Rotter, M.; Coletta, L.; Salzig, D.; Czermak, P. Process intensification for the continuous production of an antimicrobial peptide in stably-transformed Sf-9 insect cells. Sci. Rep. 2022, 12, 1086. [Google Scholar] [CrossRef]
- Sabino, Y.N.V.; Fochat, R.C.; Lima, J.C.F.; Ribeiro, M.T.; Arcuri, P.B.; Carneiro, J.; Machado, M.A.; de Lima Reis, D.R.; Machado, A.B.F.; Hungaro, H.M.; et al. Antibacterial activity and lantibiotic post-translational modification genes in Streptococcus spp. isolated from ruminal fluid. Ann. Microbiol. 2019, 69, 131–138. [Google Scholar] [CrossRef]
- Hoelscher, M.P.; Forner, J.; Calderone, S.; Krämer, C.; Taylor, Z.; Loiacono, F.V.; Agrawal, S.; Karcher, D.; Moratti, F.; Kroop, X.; et al. Expression strategies for the efficient synthesis of antimicrobial peptides in plastids. Nat. Commun. 2022, 13, 5856. [Google Scholar] [CrossRef]
- Rasines Mazo, A.; Allison-Logan, S.; Karimi, F.; Chan, N.J.A.; Qiu, W.; Duan, W.; Qiao, G.G. Ring opening polymerization of α-amino acids: Advances in synthesis, architecture and applications of polypeptides and their hybrids. Chem. Soc. Rev. 2020, 49, 4737–4834. [Google Scholar] [CrossRef]
- Fang, Z.; Wusgal, C.H.; Liang, L. Natural Biodegradable Medical Polymers. In Science and Principles of Biodegradable and Bioresorbable Medical Polymers; Elsevier: Amsterdam, The Netherlands, 2017; pp. 321–350. [Google Scholar] [CrossRef]
- Available online: https://www.europeanpharmaceuticalreview.com/news/178380/promising-first-in-human-study-results-for-orally-inhaled-antibiotic-macrocycle-compound/ (accessed on 2 April 2023).
| Advantages | Disadvantages | Limitations |
|---|---|---|
| Some AMPs show synergistic interactions with conventional antibiotics [9] | Cytotoxic/biocompatibility issues | Unfavorable pharmacokinetic profile—may be improved by formulating as a prodrug |
| Broad-spectrum of antimicrobial activity against yeast, fungi, viruses, and bacteria | Bacterial resistance may emerge to certain AMPs | No clear in vivo efficacy over conventional treatments [9] |
| Easier to synthesize—short amino acid sequences | Limited stability | Some require PTMs limiting expression systems [67] |
| Rapid onset of action | Short half-life | Downstream purification issues post production |
| Potent | Protein and enzymatic degradation | Formulation for oral delivery raises issues |
| Not effected by AMR phenotypes [25] | Reduced in vivo antimicrobial action | Not usually tolerant of low-pH environments |
| Some effective against biofilms | Over stimulation of immune system may be an issue | May lose activity in the presence of physiological salts or serum [24] |
| Potential for use as vaccine adjuvants [25] | Expensive to produce [67] | Binding to serum proteins such as albumin [67] |
| Some AMPs are stable and active in a wide pH range [6] | Toxicity to microbial expression systems during production [76] | Limited in vivo biocompatibility information currently available [44] |
| May not induce dysbiosis in the patient [38] | May induce pro-inflammatory cytokines [25] | |
| Immunomodulatory effects | ||
| AMPs can self-assemble in to various structures which may aid potency [42] | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garvey, M. Antimicrobial Peptides Demonstrate Activity against Resistant Bacterial Pathogens. Infect. Dis. Rep. 2023, 15, 454-469. https://doi.org/10.3390/idr15040046
Garvey M. Antimicrobial Peptides Demonstrate Activity against Resistant Bacterial Pathogens. Infectious Disease Reports. 2023; 15(4):454-469. https://doi.org/10.3390/idr15040046
Chicago/Turabian StyleGarvey, Mary. 2023. "Antimicrobial Peptides Demonstrate Activity against Resistant Bacterial Pathogens" Infectious Disease Reports 15, no. 4: 454-469. https://doi.org/10.3390/idr15040046
APA StyleGarvey, M. (2023). Antimicrobial Peptides Demonstrate Activity against Resistant Bacterial Pathogens. Infectious Disease Reports, 15(4), 454-469. https://doi.org/10.3390/idr15040046






