Prevalence and Determinants of Medication Adherence among Patients with HIV/AIDS in Southern Vietnam
Abstract
1. Introduction
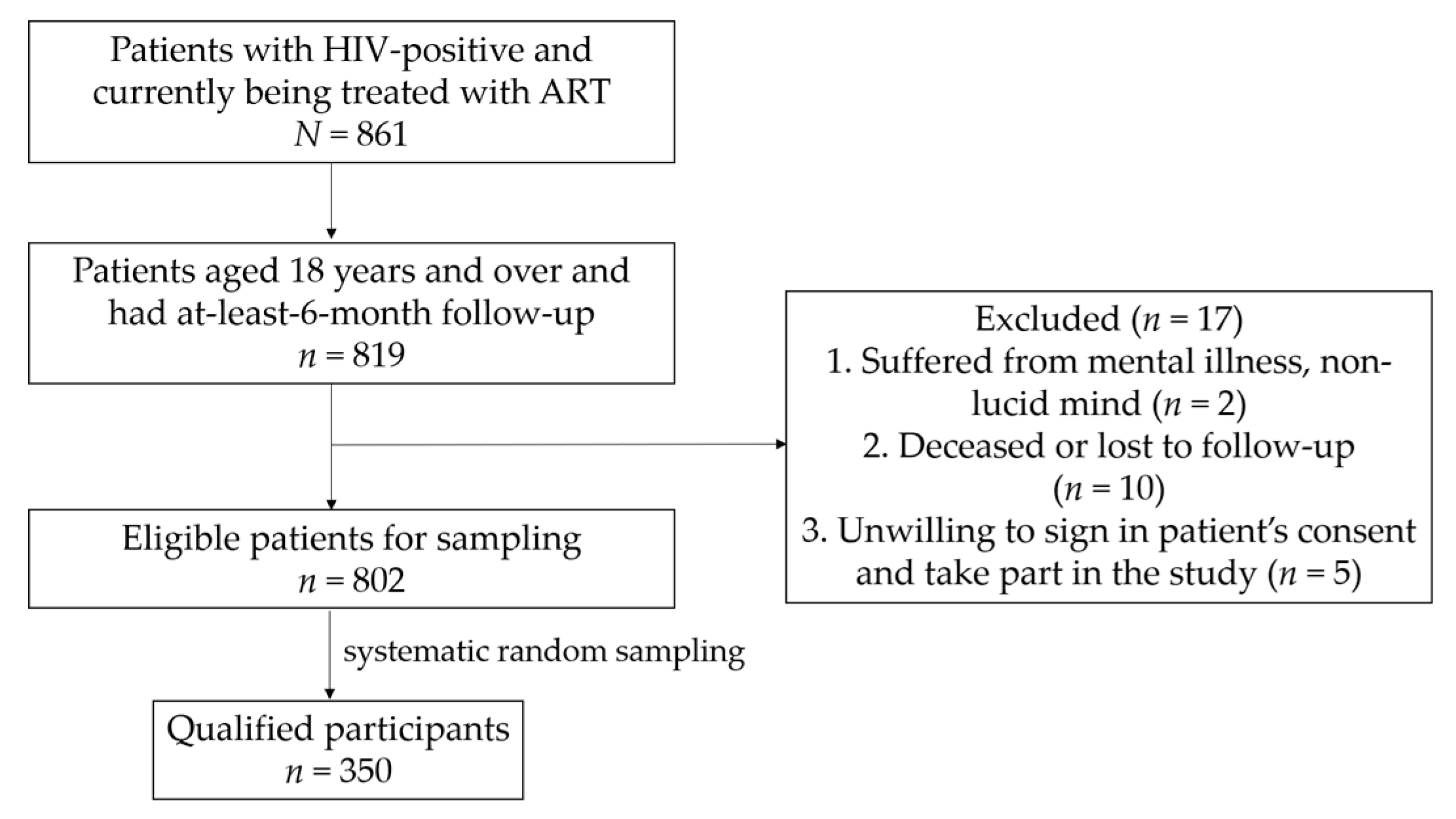
2. Materials and Methods
3. Results
3.1. Demographic and ART-Related Characteristics of Patients with HIV
3.2. The Proportion of Adherence to ART
3.3. Determinants of Patients’ Adherence
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Global HIV & AIDS Statistics—2020 Fact Sheet. Unaids.org. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 12 August 2020).
- UNAIDS Data 2020. Unaids.org. Available online: https://www.unaids.org/en/resources/documents/2020/unaids-data (accessed on 12 August 2020).
- Vietnam Ministry of Health. Report on Results of HIV/AIDS Prevention and Control in 2019 and Key Tasks in 2020; Vietnam Ministry of Health: Hanoi, Vietnam, 2020.
- Schaecher, K.L. The importance of treatment adherence in HIV. Am. J. Manag. Care 2013, 19 (Suppl. 12), s231–s237. [Google Scholar] [PubMed]
- Shrestha, R.; Altice, F.L.; Copenhaver, M.M. HIV-related stigma, motivation to adhere to antiretroviral therapy, and medication adherence among HIV-positive methadone-maintained patients. J. Acquir. Immune Defic. Syndr. 2019, 80, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Tennant, S.J.; Hester, E.K.; Caulder, C.R.; Lu, Z.K.; Bookstaver, P.B. Adherence among rural HIV-infected patients in the deep south: A comparison between single-tablet and multi-tablet once-daily regimens. J. Int. Assoc. Provid. AIDS Care 2015, 14, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Monnette, A.; Zhang, Y.; Shao, H.; Shi, L. Concordance of adherence measurement using self-reported adherence questionnaires and medication monitoring devices: An updated review. Pharmacoeconomics 2018, 36, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Vale, F.C.; Santa-Helena, E.T.D.; Santos, M.A.; Carvalho, W.M.D.E.S.; Menezes, P.R.; Basso, C.R.; Silva, M.H.; Alves, A.M.; Nemes, M.I.B. Development and validation of the WebAd-Q Questionnaire to monitor adherence to HIV therapy. Rev. Saude Publica 2018, 52, 62. [Google Scholar] [CrossRef] [PubMed]
- Du, T.N. Study the Adherence of Antiretroviral Therapy and other Relevant Factors in HIV/AIDS Patients at Can Tho Preventive Health Center, Ninh Kieu District, Can Tho City in 2014. Bachelor’s Thesis, Can Tho University of Medicine and Pharmacy, Can Tho City, Vietnam, 2015. [Google Scholar]
- Ministry of Health of Vietnam. Guidance on HIV Treatment and Care; Clinical Guideline; Ha Noi Medical Publishing House: Ha Noi City, Vietnam, 2019. Available online: http://vaac.gov.vn/Cms_Data/Contents/Vaac/Folders/DocumentLaw/Vanban/~contents/FGV2HFDVQ9CURN2F/Huong-dan-Dieu-tri-va-cham-soc-HIV-dang-web.pdf (accessed on 12 August 2020).
- Bukenya, D.; Mayanja, B.N.; Nakamanya, S.; Muhumuza, R.; Seeley, J. What causes non-adherence among some individuals on long term antiretroviral therapy? Experiences of individuals with poor viral suppression in Uganda. AIDS Res. Ther 2019, 16, 2. [Google Scholar] [CrossRef] [PubMed]
- Inzaule, S.C.; Hamers, R.L.; Kityo, C.; Rinke de Wit, T.F.; Roura, M. Long-term antiretroviral treatment adherence in HIV-infected adolescents and adults in Uganda: A qualitative study. PLoS ONE 2016, 11, e0167492. [Google Scholar] [CrossRef] [PubMed]
- George, S.; McGrath, N. Social support, disclosure and stigma and the association with non-adherence in the six months after antiretroviral therapy initiation among a cohort of HIV-positive adults in rural KwaZulu-Natal, South Africa. AIDS Care 2019, 31, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Dan, N.H. Investigating the ART Adherence Rate of HIV/AIDS Patients in an Outpatient Clinic of Vinh Long General Hospital in 2012. Master’s Thesis, Can Tho University of Medicine and Pharmacy, Can Tho City, Vietnam, 2012. [Google Scholar]
- Nam, V.T. Determination of rates and factors related to adherence to ART in HIV/AIDS patients in Can Tho City in 2009. In Proceedings of the 4th National Scientific Conference on HIV/AIDS, Ha Noi City, Vietnam, 2–3 December 2010; Ministry of Health of Vietnam: Ha Noi City, Vietnam, 2019. [Google Scholar]
- Quy, N.N. Investigating the ARV Drug Usage and Adherence of Patients at an Outpatient Department in Tran Yen–Yen Bai Health Centre. Master’s Thesis, Ha Noi University of Pharmacy, Ha Noi City, Vietnam, 2018. [Google Scholar]
- Xuyen, N.T. Survey the Use of ARV Drug and Adherence of Patients at an Outpatient Clinic in Bac Giang Center for Disease Control. Master’s Thesis, Ha Noi University of Pharmacy, Ha Noi City, Vietnam, 2017. [Google Scholar]
- Hamilton, M.M.; Razzano, L.A.; Martin, N.B. The relationship between type and quality of social support and HIV medication adherence. J. HIV AIDS Soc. Serv. 2007, 6, 39–63. [Google Scholar] [CrossRef]
- Roberts, S.T.; Nair, G.; Baeten, J.M.; Palanee-Philips, T.; Schwartz, K.; Reddy, K.; Kabwigu, S.; Kiweewa, F.M.; Govender, V.; Gaffoor, Z.; et al. Impact of male partner involvement on women’s adherence to the dapivirine vaginal ring during a phase III HIV prevention trial. AIDS Behav. 2020, 24, 1432–1442. [Google Scholar] [CrossRef] [PubMed]
- Turan, B.; Rice, W.S.; Crockett, K.B.; Johnson, M.; Neilands, T.B.; Ross, S.N.; Kempf, M.C.; Konkle-Parker, D.; Wingood, G.; Tien, P.C.; et al. Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: The mediating role of depression. AIDS 2019, 33, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Rosen, M.I.; Black, A.C.; Arnsten, J.H.; Goggin, K.; Remien, R.H.; Simoni, J.M.; Golin, C.E.; Bangsberg, D.R.; Liu, H. Association between use of specific drugs and antiretroviral adherence: Findings from MACH 14. AIDS Behav. 2013, 17, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Heestermans, T.; Browne, J.L.; Aitken, S.C.; Vervoort, S.C.; Klipstein-Grobusch, K. Determinants of adherence to antiretroviral therapy among HIV-positive adults in sub-Saharan Africa: A systematic review. BMJ Glob. Health 2016, 1, e000125. [Google Scholar] [CrossRef] [PubMed]
- Sohler, N.; Slawek, D.; Earnshaw, V.; Jost, J.; Lee, A.; Mancini, J.; Mompremier, A.; Cunningham, C.O. Drug use and HIV medication adherence in people living with HIV. Subst. Abus. 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Sileo, K.M.; Kizito, W.; Wanyenze, R.K.; Chemusto, H.; Reed, E.; Stockman, J.K.; Musoke, W.; Mukasa, B.; Kiene, S.M. Substance use and its effect on antiretroviral treatment adherence among male fisherfolk living with HIV/AIDS in Uganda. PLoS ONE 2019, 14, e0216892. [Google Scholar] [CrossRef] [PubMed]
- Sileo, K.M.; Kizito, W.; Wanyenze, R.K.; Chemusto, H.; Musoke, W.; Mukasa, B.; Kiene, S.M. A qualitative study on alcohol consumption and HIV treatment adherence among men living with HIV in Ugandan fishing communities. AIDS Care 2019, 31, 35–40. [Google Scholar] [CrossRef]
| Characteristics | Frequency and Percentage (n, %) | Adherence | p-Value ** | |
|---|---|---|---|---|
| Yes (n, %) | No (n, %) | |||
| Age | ||||
| ≥35 years old | 188 (53.7) | 151 (80.3) | 37 (19.7) | 0.03 |
| <35 years old | 162 (46.3) | 114 (70.4) | 48 (29.6) | |
| Gender | ||||
| Male | 220 (62.9) | 165 (75.0) | 55 (25.0) | 0.685 |
| Female | 130 (37.1) | 100 (76.9) | 30 (23.1) | |
| Marital status | ||||
| Married | 166 (47.4) | 140 (84.3) | 26 (15.7) | <0.001 |
| Single | 184 (52.6) | 125 (67.9) | 59 (32.1) | |
| Currently living with | ||||
| Relatives, friends | 295 (84.3) | 225 (76.3) | 70 (23.7) | 0.574 |
| Alone | 55 (15.7) | 40 (72.7) | 15 (27.3) | |
| Home-to-clinic distance | ||||
| <20 km | 108 (30.9) | 74 (68.5) | 34 (31.5) | 0.036 |
| ≥20 km | 242 (69.1) | 191 (78.9) | 51 (21.1) | |
| Level of education | ||||
| Upper secondary | 206 (58.9) | 161 (78.2) | 45 (21.8) | 0.203 |
| Lower secondary | 144 (41.1) | 104 (72.2) | 40 (27.8) | |
| Occupation | ||||
| Employment | 285 (81.4) | 216 (75.8) | 69 (24.2) | 0.945 |
| Unemployment | 65 (18.6) | 49 (75.4) | 16 (24.6) | |
| Work away from home | ||||
| Yes | 135 (38.6) | 94 (69.6) | 41 (30.4) | 0.035 |
| No | 215 (61.4) | 171 (79.5) | 44 (20.5) | |
| HIV transmission route | ||||
| Sexual behaviors | 333 (95.1) | 255 (76.6) | 78 (23.4) | 0.142 * |
| Drug abuse and mother–child | 17 (4.9) | 10 (58.8) | 7 (41.2) | |
| Clinical stage during treatment | ||||
| Stage I, II | 341 (97.4) | 257 (75.4) | 84 (24.6) | 0.693 * |
| Stage III, IV | 9 (2.6) | 8 (88.9) | 1 (11.1) | |
| CD4 count (cells/mm3) | ||||
| ≥200 | 283 (83.7) | 212 (74.9) | 71 (25.1) | 0.272 |
| <200 | 55 (16.3) | 45 (81.8) | 10 (18.2) | |
| Opportunistic infection | ||||
| Yes | 10 (2.9) | 5 (50.0) | 5 (50.0) | 0.067 * |
| No | 340 (97.1) | 260 (76.5) | 80 (23.5) | |
| Hepatitis B and C virus coinfection | ||||
| Yes | 312 (89.1) | 236 (75.6) | 76 (24.4) | 0.927 |
| No | 38 (10.9) | 29 (76.3) | 9 (23.7) | |
| ART regimen | ||||
| First-line ART | 340 (97.1) | 256 (75.3) | 84 (24.7) | 0.461 * |
| Second-line ART | 10 (2.9) | 9 (90.0) | 1 (10.0) | |
| Viral load (copies/mL) | ||||
| <20 cps | 305 (89.7) | 230 (75.4) | 75 (24.6) | 0.821 |
| >20 cps | 35 (10.3) | 27 (77.1) | 8 (22.9) | |
| Dosing times | ||||
| Once a day | 299 (85.4) | 224 (74.9) | 75 (25.1) | 0.399 |
| Twice a day | 51 (14.6) | 41 (80.4) | 10 (19.6) | |
| Drug abuse | ||||
| Yes | 244 (69.7) | 173 (70.9) | 71 (29.1) | 0.001 |
| No | 106 (30.3) | 92 (86.8) | 14 (13.2) | |
| Drug side effects | ||||
| Yes | 304 (86.9) | 228 (75.0) | 76 (25.0) | 0.423 |
| No | 46 (13.1) | 37 (80.4) | 9 (19.6) | |
| General knowledge about ART | ||||
| Yes | 217 (62.0) | 180 (82.9) | 37 (17.1) | <0.001 |
| No | 133 (38.0) | 85 (63.9) | 48 (36.1) | |
| Patients with stress, anxiety, depression | ||||
| Yes | 160 (45.7) | 128 (80.0) | 32 (20.0) | 0.086 |
| No | 190 (54.3) | 137 (72.1) | 53 (27.9) | |
| Patients’ quality of life after treatment | ||||
| Better | 239 (68.3) | 197 (82.4) | 42 (17.6) | <0.001 |
| Normal | 111 (31.7) | 68 (61.3) | 43 (38.7) | |
| Patients want to stop using drugs after improvement | ||||
| Yes | 56 (16.0) | 28 (50.0) | 28 (50.0) | <0.001 |
| No | 294 (84.0) | 237 (80.6) | 57 (19.4) | |
| Prompting of medication | ||||
| Self-managing | 293 (83.7) | 229 (78.2) | 64 (21.8) | 0.016 |
| Spouses, parents, siblings | 57 (16.3) | 36 (63.2) | 21 (36.8) | |
| Waiting time for medical examination | ||||
| Fast | 143 (40.9) | 120 (83.9) | 23 (16.1) | 0.003 |
| Normal | 207 (59.1) | 145 (70.0) | 62 (30.0) | |
| Satisfaction of medical services | ||||
| Very satisfied | 188 (53.7) | 160 (85.1) | 28 (14.9) | <0.001 |
| Satisfied | 162 (46.3) | 105 (64.8) | 57 (35.2) | |
| Feeling uncomfortable with treatment adherence | ||||
| Yes | 37 (10.6) | 27 (73.0) | 10 (27.0) | 0.681 |
| No | 313 (89.4) | 238 (76.0) | 75 (24.0) | |
| Self-assessment of adherence to treatment | ||||
| High adherence | 282 (80.6) | 240 (85.1) | 42 (14.9) | <0.001 |
| Medium and low adherence | 68 (19.4) | 25 (36.8) | 43 (63.2) | |
| Treatment period (months) | ||||
| Months (mean ± SD) | 350 (100) | 48.89 ± 36.13 | 51.25 ± 33.22 | 0.593 *** |
| Adherence Assessment | Frequency (n = 350) | Percentage (%) |
|---|---|---|
| Take the right medicine | ||
| Yes | 344 | 98.3 |
| No | 6 | 1.7 |
| Take correct dose | ||
| Yes | 302 | 86.3 |
| No | 48 | 13.7 |
| Take medicine on time | ||
| Yes | 306 | 87.4 |
| No | 44 | 12.6 |
| Take medicine properly in combination with eating and drinking | ||
| Yes | 332 | 94.9 |
| No | 18 | 5.1 |
| Routine follow-up | ||
| Yes | 348 | 99.4 |
| No | 2 | 0.6 |
| Adherence to treatment | ||
| Yes | 265 | 75.7 |
| No | 85 | 24.3 |
| Features | Univariable Regression Logistic | Multivariable Regression Logistic | ||
|---|---|---|---|---|
| OR (95%CI) | p-Value | OR (95%CI) | p-Value | |
| Marital Status | ||||
| Married | 2.54 (1.51–4.28) | <0.001 | 2.29 (1.25–4.19) | 0.007 |
| Single * | - | - | - | - |
| Work away from home | ||||
| No | 1.7 (1.03–2.78) | 0.036 | 2.15 (1.19–3.89) | 0.011 |
| Yes * | - | - | - | - |
| Drug abuse | ||||
| No | 2.7 (1.44–5.05) | 0.002 | 2.03 (1.01–4.08) | 0.048 |
| Yes * | - | - | - | - |
| General knowledge about ART treatment | ||||
| Yes | 2.75 (1.67–4.53) | <0.001 | 1.99 (1.1–3.64) | 0.026 |
| No * | - | - | - | - |
| Stop using drugs after improvement | ||||
| No | 4.16 (2.29–7.56) | <0.001 | 2.16 (1.04–4.46) | 0.039 |
| Yes * | - | - | - | - |
| Self-assessment of adherence to treatment | ||||
| High adherence | 9.83 (5.44–17.77) | <0.001 | 5.97 (3.07–11.61) | <0.001 |
| Medium and low adherence * | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, P.M.; Thach, A.N.; Pham, X.D.; Lam, A.N.; Nguyen, T.N.P.; Duong, C.X.; Nguyen, L.V.; Nguyen, T.H.; Pham, S.T.; Taxis, K.; et al. Prevalence and Determinants of Medication Adherence among Patients with HIV/AIDS in Southern Vietnam. Infect. Dis. Rep. 2021, 13, 126-135. https://doi.org/10.3390/idr13010014
Nguyen PM, Thach AN, Pham XD, Lam AN, Nguyen TNP, Duong CX, Nguyen LV, Nguyen TH, Pham ST, Taxis K, et al. Prevalence and Determinants of Medication Adherence among Patients with HIV/AIDS in Southern Vietnam. Infectious Disease Reports. 2021; 13(1):126-135. https://doi.org/10.3390/idr13010014
Chicago/Turabian StyleNguyen, Phuong M., Anh N. Thach, Xuan D. Pham, Anh N. Lam, Thao N. P. Nguyen, Chu X. Duong, Lam V. Nguyen, Thao H. Nguyen, Suol T. Pham, Katja Taxis, and et al. 2021. "Prevalence and Determinants of Medication Adherence among Patients with HIV/AIDS in Southern Vietnam" Infectious Disease Reports 13, no. 1: 126-135. https://doi.org/10.3390/idr13010014
APA StyleNguyen, P. M., Thach, A. N., Pham, X. D., Lam, A. N., Nguyen, T. N. P., Duong, C. X., Nguyen, L. V., Nguyen, T. H., Pham, S. T., Taxis, K., & Nguyen, T. (2021). Prevalence and Determinants of Medication Adherence among Patients with HIV/AIDS in Southern Vietnam. Infectious Disease Reports, 13(1), 126-135. https://doi.org/10.3390/idr13010014








