Abstract
Background/Objectives: Ultrasonography is a diagnostic modality characterized by high sensitivity in detecting hepato-biliary pathology, particularly intrahepatic biliary duct dilation. This study compares the sonographic findings obtained by a radiographer/sonographer in a Basic Emergency Service (BES) using Point-of-Care Ultrasonography (POCUS) in Portugal with the sonographic findings from the same patients acquired by radiologists at a referral hospital (RH) for suspected intrahepatic biliary dilatation. Methods: Nineteen patients presenting with right upper quadrant (RUQ) pain and suspected abdominal pathology underwent sonographic screening using POCUS in the BES. Subsequently, the same patients were referred to the RH, where a radiologist performed a comprehensive ultrasound. Both examinations were compared to determine whether the findings obtained in the BES were confirmed by radiologists in the RH. Results: Cholestasis, cholangitis, lithiasis, pancreatitis, peri-ampullary lithiasis, and neoplasms were observed in association with intrahepatic biliary dilation in this study sample. All six variables showed a strong association between the BES and RH findings (Cramer’s V > 0.6; p < 0.006). A strong kappa measure of agreement between the radiographer and radiologist findings was obtained in “cholelithiasis/sludge/gallbladder acute sonographic changes” (k = 0.802; p = 0.000). A moderate kappa value was obtained for the variable “abdominal free fluid”, (k = 0.706; p = 0.001). Conclusions: In this study, all patients referred from the BES to the RH required hospitalization for treatment and additional imaging exams. Although pre-hospital screening ultrasound is not intended for definitive diagnoses, the early detection of intrahepatic biliary tract dilatation through screening sonography played a significant role in the clinical referral of patients, with a sensitivity of 94% and specificity of 75%.
1. Introduction
Point-of-Care Ultrasound (POCUS) consists of the application of ultrasound protocols to answer objective clinical questions in patient assessment/screening performed by non-radiologists [1,2,3,4,5]. This type of ultrasound has experienced rapid growth and an expanding range of clinical applications, particularly in emergency departments (EDs) [6,7], especially those situated far from referral hospitals (RHs) and facing challenges such as limited access to medical specialists and technological constraints [8,9,10]. Factors such as radiation exemption and a wide range of applicability in EDs—together with the growing evidence for financial savings [11,12]—have contributed to the global acceptance of POCUS. However, dependence on the operator’s skill has previously been a controversial point, and so specific training courses and study are mandatory to avoid technical errors in the acquisition and/or interpretation of acquired images [13,14].
POCUS has exhibited significant accuracy in detecting abdominal pathology within the ED setting [15,16]. In the Portuguese Basic Emergency Service (BES), POCUS has demonstrated a low rate of inconclusive exams, making it a valuable screening tool [17]. Sonography exhibits high sensitivity in detecting pathologies associated with right upper quadrant (RUQ) pain and biliary disorders [18,19,20], including the detection of intrahepatic biliary tract dilatation [21,22,23].
Pre-hospital ultrasound serves as a guiding tool rather than a definitive diagnostic method [23]. The detection of intrahepatic bile duct dilatation through ultrasound is an important clinical imaging finding that prompts clinicians to refer patients for further studies to determine the underlying cause of the dilation.
Intrahepatic bile duct dilatation (IHBD) is a pathology of multifactorial etiology and is fundamentally divided into obstructive and non-obstructive forms. Additionally, acute or chronic forms of cholangitis may occur as causes of IHBD [24,25].
The differential diagnosis, determination of etiology, and confirmation of IHBD conditions should be managed by radiologists and other relevant specialties. This is necessary due to the complexity of the clinical scenarios, which often require additional clinical and complementary diagnostic examinations to provide a more comprehensive understanding of the patient’s condition.
In healthy patients, the visualization of intrahepatic bile ducts using ultrasound is typically not possible [26]. Technically, the suspicion of intrahepatic bile duct dilatation is initially raised during a liver scan, where the observation of “more vessels inside the liver than expected” becomes evident. The presence of a double-rail or shotgun sign with closed pipes is considered a “pathognomonic” sonographic image that signifies this particular pathology [26,27,28]. Doppler can also be used to confirm the absence of flow in patent bile ducts [29]. Additional measurements of these dilations (over 2 mm) can be carried out to confirm the clinical suspicion [30]—when inflammation is present (cholangitis), the endovascular components of the bile duct may be thickened [31].
IHBD is a pathology often associated with life-threatening episodes like biliary obstructive or non-obstructive factors that lead to cholestatic [32] patterns often leading to cholangitis. Cholangitis is a multi-etiologic pathology and any delay in treatment is usually associated with high degrees of mortality [33,34,35]. Therefore, early detection of intrahepatic bile duct dilatation is crucial, particularly in the pre-hospital ED setting where comprehensive blood analysis to determine the laboratory parameters of cholestasis may not be available. In addition, symptomatologic patterns in IHBD can often overlap with other biliary or hepatic diseases, making Charcot’s triad and Reynold’s pentad less accurate [36,37] for cholangitis screening and making referral clinical decisions less obvious.
Prospective evidence on the diagnostic accuracy of POCUS for IHBD in Portuguese BES is scarce so the reliability of this bedside tool in resource-constrained settings remains largely undefined. Therefore, this study has two objectives: The primary objective is to verify whether IHBD detected by POCUS in the BES is confirmed by the comprehensive imaging later performed in the RH. The second objective is to characterize the etiological spectrum linked to the IHBD sonographic patterns observed. By quantifying the agreement between findings at the BES and examinations at the RH, this study will clarify the robustness and clinical value of POCUS in this context.
2. Materials and Methods
2.1. Sample and Instruments
From an initial sample of 201 abdominal ultrasounds performed on patients with non-specific abdominal pain, only 24 were selected based on the presence of suspected sonographic signs of intrahepatic biliary dilatation and/or RUQ pain.
This study was conducted in a BES located in Southern Portugal using a Toshiba Némio XG ultrasound system with a convex probe. The RH sonography exams were performed by radiologists operating a General Electric S8 with 3 probes (linear, convex, and micro convex). This prospective study was observational and longitudinal. Data were recorded from 2016 to December 2022 and descriptively analyzed in the Microsoft Office Excel program version 2019. Statistical analyses and correlation tests between variables were conducted using IBM SPSS Statistics version 26. Sonographic images and their respective reports from the RH were accessed through the local Picture Archiving and Communication System (PACS) and digital clinical reporting systems.
The inclusion criteria for the study were as follows: (1) RUQ pain (discomfort or pain in the right quadrant, vomiting; fever or jaundice recorded but not mandatory); (2) present or uncertain echographic images suggesting intrahepatic biliary dilatation (IHBD was suggested when the anechoic tubular structures measuring more than 2 mm in internal diameter were visualized within second-order portal tracts, with or without the “double-rail” (shotgun) sign, and no intraluminal flow was detected on color Doppler); (3) screening sonography performed in the BES by a radiographer/sonographer; (4) comprehensive sonography performed by a radiologist in the RH under the same emergency episode; (5) imaging data and clinical information available through the PACS and integrated clinical report systems. Our study methodology selected patients who presented with a presumptive suspicion of biliary pathology, based on clinical history and signs such as RUQ pain, vomiting, and/or jaundice (either in combination or individually). From this group were included patients who had an ultrasound performed in the emergency setting (BES) that was compatible with IHBD, and who were subsequently referred to the RH, where further imaging exams (CT and/or ultrasound, etc.) were performed. The findings from the BES were then compared with those reported in the RH imaging, which was considered the gold standard (some of the ultrasounds in the RH were performed after the CT scans).
Out of the initial sample of twenty-four selected patients, five individuals were excluded from this study as they did not meet one or more of the pre-defined inclusion criteria. Therefore, the final sample size for this study consisted of 19 patients.
2.2. Statistical Analysis
Descriptive statistical analysis (percentages and frequencies) was performed for the variables under study (Table 1). Cramer’s V test was used to measure the association between variables and Cohen’s kappa coefficient was used to measure inter-rater reliability among sonography performers, both with 95% confidence intervals. Cramer’s V and Cohen’s kappa are both measures used in categorical data analysis. Cramer’s V ranges from 0 to 1.0, and the closer it is to 1.0, the stronger the association (below 0.2 the result is weak; 0.21 to 0.6 is moderate; and above 0.6 is strong). Cohen’s kappa also ranges from 0 to 1, with values below 0.2 suggesting poor agreement; 0.21–0.40 fair agreement; 0.41–0.60 moderate agreement; 0.61–0.80 strong agreement; and above 0.80 indicating very strong agreement.

Table 1.
Criteria for data evaluation and classification options in ultrasound assessment.
2.3. Ethics Statement
This study was approved by the Institutional Review Board from the BES. All ultrasound exams were ordered by emergency physicians. Some patients were unable to provide informed consent due to their health conditions. In these cases, consent was obtained by the legal representative. To ensure compliance with the general data protection law, no patient or institutional data were recorded. The primary aim of this study was to demonstrate the significance and utility of sonographic screening in a pre-hospital setting. This study adhered to ethical standards for scientific investigation, including the principles outlined in the Declaration of Helsinki and the applicable national data protection legislation.
2.4. Ultrasound Protocol Covered in This Study
The abdominal protocol applied in this study was summarized into nine steps: first—left liver, 2 perpendicular planes (2pp); second—gallbladder scan, 2pp; third—supra-hepatic veins; fourth—portal vein and main biliary tract, 2pp; fifth—lower liver, 2pp; sixth—pancreas, 2pp; seventh—color Doppler technology was used to aid in the detection of potential vascular abnormalities. The protocol was adapted according to the patient’s condition/collaboration.
The ultrasound findings or image and clinical observation were recorded in Table 1.
All screening ultrasound examinations were performed by a single radiographer–sonographer who had completed extensive postgraduate training, including several ultrasound courses and a 200-h master’s degree internship in emergency ultrasound at a tertiary hospital under the direct supervision of an experienced radiologist. In this context, he worked in collaboration with the emergency physician at the BES in this patient’s multifactorial approach (imaging and clinical). Based on sonographic and clinical findings, a decision was made about the referral of patients to the emergency department. The BES physician provided a succinct written summary in the patient’s clinical record regarding any sonographic images deemed potentially abnormal. This information served as the sole source of data for the RH regarding the screening ultrasounds performed at the BES.
The data were collected and recorded by the main investigator in a dedicated data file. Ultrasound data were analyzed, and the results were classified according to the criteria shown in Figure 1.
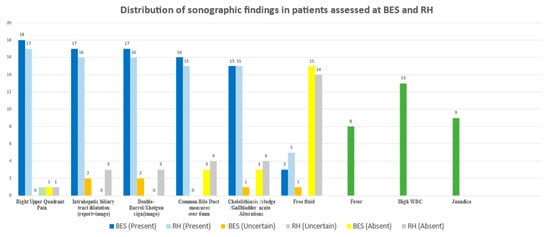
Figure 1.
Comparison of ultrasound findings between patients assessed at BES and RH. The chart presents the distribution of sonographic variables recorded during abdominal ultrasound examinations. Green bars indicate findings observed in both settings.
3. Results
The final number of patients considered for this study was 19 in total; 6 (31.6%) were male and 13 (68.4%) were female. The average age was 70 ± 17.9 years old.
From this sample, six patients had a single exam in the RH (comprehensive sonography) and the remaining thirteen patients received two or more complementary diagnostic tests. The diagnostic modalities used for each patient, as well as the etiology of the IHBD, are available in Table 2.

Table 2.
Etiology of intrahepatic biliary dilatation of the sample.
Four patients underwent sonography and endoscopic retrograde cholangiopancreatography (ERCP); another four patients received sonography and computed tomography (CT); three patients underwent sonography, ERCP, and CT; and two patients received sonography, CT, and magnetic resonance cholangiopancreatography (MRCP).
Figure 1 illustrates the total results obtained for the echographic variables in this study. For each category/variable, the following was considered: BES+/RH+ (%) as well as uncertain and absent classifications for BES/RH, respectively. The percentages were calculated based on 19 patients.
In this study, right upper quadrant (RUQ) pain showed high agreement between the BES and the RH: 18/17 patients (89.4%) were positively classified with RUQ pain; and both observers agreed on one patient (5.26%) being uncertain. One patient was considered by the RH to have no RUQ pain.
For intrahepatic biliary tract dilatation (image, report, or both), concordance between observers was 17/16 (84.2%) for the presence of IHBD. Radiologists classified three patients (15.7%) as not having IHBD, while the sonographer classified two patients (10.5%) as uncertain. It is important to note that, in several cases, the comprehensive ultrasound at the RH was performed several hours after the patient’s admission and after therapeutic measures had already begun, as will be discussed later.
Regarding the double-barrel/shotgun sign—a specific echographic indicator—observer concordance was 16/15 (78.9%) for the presence of the sign. Radiologists determined that three patients (15.7%) had no such sign, while the sonographer considered two patients (10.5%) as uncertain.
For the common bile duct diameter, specifically for measurements above 6 mm, there was concordance in 16/15 cases (78.9%), indicating positive agreement. There was a discrepancy in only one patient (5.26%), showing minor interpretation differences. There were no uncertain cases in either the BES or RH. Radiologists classified four cases (21.0%) as having a normal CBD diameter, while the sonographer classified three patients (15.7%) as normal.
Regarding cholelithiasis, sludge, or acute gallbladder sonographic changes, total concordance for positive identification was 15/15 (78.9%) among the 19 patients. The sonographer considered one patient (5.26%) as uncertain, and three patients (15.7%) as absent. The radiologist classified four patients (21.0%) as not having any of these abnormalities.
For abdominal free fluid, there was concordance in 3/5 (15.7%) positive findings, with differences in two patients (10.2%). The sonographer classified one patient (5.26%) as uncertain, while the radiologist had no uncertain cases. Agreement regarding the absence of free fluid was high: 15 patients (78.9%) were identified as negative by the sonographer and 14 (73.6%) by the radiologist.
Cramer’s V was used to assess the strength of association between ultrasound findings, and Cohen’s kappa was applied to evaluate inter-rater reliability between ultrasound performers.
A summary of the results is presented in Table 3.

Table 3.
Cramer’s V and Cohen’s kappa, alongside significance values, for the different tested variables.
Cramer’s V test demonstrates a strong association between the BES and RH findings (Cramer’s V > 0.6; p < 0.01) in all six variables (“right upper quadrant pain”, “intrahepatic biliary tract dilatation”, “double-barrel/shotgun sign”, “common bile duct measures over 6 mm”, “cholelithiasis/sludge/gallbladder acute sonographic changes”, and “abdominal free fluid”).
The Kappa values demonstrated very strong agreement between observers for “cholelithiasis/sludge/gallbladder acute sonographic changes” and “common bile duct measures over 6 mm” variables with (k = 0.81–1, p < 0.01). Strong agreement was also found for “right upper quadrant pain” and “abdominal free fluid” with (k = 0.61–0.80, p < 0.01).
Moderate agreement was found between “intrahepatic biliary tract dilatation” and “double-barrel/shotgun sign” (k = 0.21–0.40, p < 0.01).
All patients required hospitalization. The minimum length of stay was 2 days, the maximum was 120 days, and the average was 15.82 ± 24.95 days.
Eleven patients (57.8%) had at least one previous attendance at the BES for related symptoms within the previous three months.
4. Discussion
In this sample, comprising 19 patients, intrahepatic biliary tract dilatation was confirmed in 16 individuals. Three patients were considered differently for the presence of IHBD between the referral hospital and the Basic Emergency Service, although it must be emphasized that two patients left the BES with uncertain IHBD findings. Of these two, one was diagnosed with pancreatitis and the other with cholangitis. The third patient was initially considered to have evidence of IHBD but, possibly, the echographic findings normalized as a result of the therapy implemented and the time elapsed between the screening ultrasound and the comprehensive sonography at the RH.
Cholangitis was identified in five patients. One case was associated with lithiasis-induced pancreatitis. Two cases presented with a cholestatic pattern: one due to an obstructive distal choledochal calculus and the other caused by an obstructive tumor (cholangiocarcinoma). An additional case of non-obstructive cholangitis also exhibited a cholestatic pattern. The fifth case occurred in the context of gallbladder rupture, accompanied by multi-organ dysfunction.
There were three cases of IHBD associated with pancreatitis. The other case of pancreatitis was associated with cholangitis and did not present IHBD. Nevertheless, all four cases were of calculus-related pancreatitis.
Distal choledochal (extrahepatic) calculi were identified as the cause of IHBD in four cases. A single case of IHBD was attributed to a calculus located in the intrahepatic portion of the common bile duct. Neoplasms were responsible for IHBD in four patients: two cases of cholangiocarcinoma (one previously described) and two cases involving pancreatic head tumors. The final case of IHBD was caused by a perforated peptic ulcer leading to peritonitis.
Abdominal radiographs (ARX) can be useful for confirming or excluding certain potential causes of pathology. However, in the case of abdominal organs—and particularly in biliary pathology—they often fail to provide clear or diagnostic imaging findings [38,39]. In this study, ARX were executed in 12 (63.1%) of the patients, and all ARX were considered normal or had abnormalities not related to the episode. White blood cell count (WBC) was acquired in 19 (100%) patients (it was high in 13 (68.3%) patients; in 6 (31.5%) it was normal or reduced). Various forms and degrees of jaundice [40,41,42] were present in nine patients; eight patients presented with fever. Although the gold standard (radiologist’s report) at the referral hospital identified 16 patients with IHBD, and the BES identified 17, the calculated sensitivity and specificity for detecting this pathology at the BES were approximately 94% and 75%, respectively. These results must be interpreted with caution because the sample size is small and no control group was included; therefore, they represent preliminary, hypothesis-generating evidence rather than definitive conclusions.
Hospitalization was required for 18 patients. The standard deviation was 24.95 days, which reflects a considerable dispersion of the data, indicating that the values show a large variation around the mean (15 days). Although our sample size does not allow for strong inferences regarding hospitalization duration, it is known that, for example, cholangitis has an average described hospitalization of 15 days [43,44], although this varies with severity. Treatment may only require antibiotics and/or biliary decompression; all of these processes require hospitalization. Older patients with comorbidities tend to remain hospitalized longer than the average. Pancreatitis has a wide hospitalization range, from 5 to 10 days in milder cases [45,46], with longer stays in more severe cases [47]. This aligns with our four cases in which the average hospital stay was 10 days. Intra- and extrahepatic obstructions result in variable hospitalization durations depending on severity, inflammatory state, and obstruction location. ERCP is the preferred approach [48], although advanced techniques like Endoscopic Ultrasound (EUS)-guided interventions [49] are still at an early stage in the RH of this study. Reserved prognoses were associated with neoplastic pancreatic and unresectable cholangiocarcinomas [50,51], where patients are often referred for palliative care [52] and average hospitalization stays are described as approximately 10 days [53].
It was also found that 63% of patients had previously visited the BES with symptoms potentially related to the episode that later led to their re-admission. Based on the available data, it was not possible to conclusively determine whether the same pathology was involved in both episodes. Several biliary or neoplastic conditions can present with scattered and inconsistent symptoms over time [54,55,56], only becoming evident when they cause organ/system failure.
In this study, the association between variables between the BES and RH through inferential statistics proved to be strong, (Cramer’s V > 0.6) in all sonographic variables such as intrahepatic biliary tract dilatation; double-barrel/shotgun sign; common bile duct measuring over 6 mm; cholelithiasis/sludge/gallbladder acute changes; and abdominal free fluid. This means that using specific echographic protocols and guidelines to support the operator’s evaluation of anatomical structures is likely to yield more accurate results, even though ultrasound performance still depends on the operator’s experience, as well as the patient’s body composition and cooperation during the exam. Factors such as greater experience and knowledge of the radiologist—combined with the quality of the ultrasound machine—may explain some differences in the achieved Cramer’s values.
These findings are consistent with previous research [57] that demonstrated a high degree of concordance among different professionals, indicating a consistent interpretation of ultrasound findings in the context of biliary pathology, particularly in remote or resource-limited settings.
Pathology detection often relies on the interpretation of imaging exams [58]. Consequently, inter-observer concordance between the sonographers and radiologists was analyzed using kappa values, which measure agreement in nominal or ordinal evaluations of the same sample. The kappa values demonstrated strong agreement between observers for the “cholelithiasis/sludge/gallbladder acute sonographic changes” and “common bile duct measuring over 6 mm” variables with (k = 0.81–1, p < 0.01). This range represents an almost perfect agreement, suggesting that the BES and the RH observers consistently reached the same conclusions when evaluating these variables.
Strong agreement between professionals was also found for ”right upper quadrant pain” and “abdominal free fluid”, with (k = 0.61–0.80, p < 0.01) for both variables. This range reflects a substantial consensus among observers, although slightly lower than the latter categories.
A moderate association between observers (k = 0.21–0.4, p < 0.01) was obtained in “intrahepatic biliary tract dilatation” and the “double-barrel/shotgun sign”, indicating only a fair agreement between observers, implying greater variability in interpretations for these findings. The results are still statistically significant (p < 0.01), suggesting that while the agreement is modest, it is unlikely to be due to chance. These differences in the evaluation of suspected IHBD cases may be explained by temporal factors and the effects of treatment, as suggested in the literature [59].
Although few studies directly compare inter-observer agreement in sonographic findings between pre-hospital and hospital settings, our results appear to align with the recent and relevant literature [60].
Limitations of This Study
This study had several limitations. First, the number of cases considered may appear somewhat low; however, given that it addresses a very specific emergency clinical situation, it is very important that these cases were identified early within the primary stages of the national emergency network (BES). Additionally, it is also relevant to note that the ultrasound equipment in the BES was older and of lower quality compared to that in the RH, which may have influenced the analysis of IHBD findings. The lesser experience of the BES operator compared to the RH radiologists must also be taken into account.
Furthermore, some IHBD cases were referred to RHs but left the facility before further diagnostic confirmation—such as comprehensive sonography or other methods—could be performed, making it impossible to validate the BES sonographic findings. In all included cases, the comprehensive imaging performed at the referral hospital followed the initial BES POCUS examination, with an inter-examination interval ranging from several hours to more than 24 h, which may contribute to the discrepancies in findings and interpretations between operators.
The inclusion of a control group could have strengthened the robustness of our findings. However, due to the operational constraints of our setting—specifically, the fact that only one sonographer was performing these examinations—and the nature of urgent care workflows, the inclusion of a control group was not feasible at the time
Finally, screening ultrasound evaluations in the BES are still in an active and experimental phase. There are likely emergency physicians who do not yet fully recognize the scope and practicality of ultrasound as a screening tool, leading them to refer patients directly to the RH without performing a screening ultrasound in the BES, thereby limiting the sample scope.
The authors are also fully aware that false negatives can occur, particularly in emergency settings where patient cooperation may be limited due to pain or lack of preparation. However, this was not the focus of the present study. Our objective was to assess the appropriateness of referrals based on positive cases identified in the BES.
5. Conclusions
While the decision to refer patients from the BES to the RH is based on a comprehensive clinical context with multiple factors involved, the presence of intrahepatic biliary duct (IHBD) dilatation was a significant sonographic clue that strongly influenced the decision to refer patients in this study. The correct orientation of patients is reflected in the clinical findings obtained at the referral hospital, as well as the hospitalization of all referred patients.
The wide range of complementary diagnostic tests carried out in the referral hospital confirmed the complexity of the several pathologies found, and the cases identified in this study confirm the potential of ultrasound as a screening tool for biliary pathology, particularly in the detection of IHBD dilatation. It is important to note that, although ultrasound does not provide a definitive diagnosis or interfere with the diagnostic process conducted by other specialties at the RH, a high level of association in sonographic findings was observed, along with a high degree of concordance between the BES screening exam and the comprehensive ultrasound performed by radiologists at the RH. The process of referring patients based on clinical evidence obtained through screening ultrasound represents a reliable support for clinical decision-making, and possibly a strategy that safeguards the interests of both patients and the broader healthcare system.
These findings, albeit preliminary, suggest that a structured BES-POCUS protocol could both shorten the time to treatment in biliary emergencies and serve as a scalable training model for other resource-limited regions.
Further studies are warranted in Portugal to validate the findings of this study and to potentially expand the use of screening sonography in the specific context of institutions like the BES. This would contribute to strengthening the consistency of the results and provide a more comprehensive understanding of the benefits of such an approach.
Author Contributions
Conceptualization, S.M.; methodology, S.M., M.D.L. and R.P.d.A.; validation, all authors; formal analysis, all authors; data curation, S.M. and B.V.; writing—original draft preparation, S.M., B.V., M.D.L. and R.P.d.A.; writing—review and editing, all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board from the BES (ACES/ARS/11/02/06—ARS Algarve, IP, approved date:11 February 2016).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author due to ethical reasons.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ARX | Abdominal radiographs |
| BES | Basic Emergency Service |
| CBD | Common bile duct |
| CT | Computed tomography |
| ED | Emergency department |
| ERCP | Endoscopic retrograde cholangiopancreatography |
| IHBD | Intrahepatic bile duct dilatation |
| MRCP | Magnetic resonance cholangiopancreatography |
| POCUS | Point-of-Care Ultrasonography |
| RH | Referral hospital |
| PACS | Picture Archiving and Communication System |
| RUQ | Right upper quadrant |
| WBC | White blood cell count |
References
- Harrison, G.; Kraus, B.; Martins Dos Santos, R.; Noij-Rijkes, S.; Pedersen, M.R.V. The role of radiographers in ultrasound: A survey of the national societies within the European Federation of Radiographer Societies (EFRS). Radiography 2021, 27, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Miles, N.; Cowling, C.; Lawson, C. The role of the sonographer: An investigation into the scope of practice for the sonographer internationally. Radiography 2022, 28, e33–e39. [Google Scholar] [CrossRef] [PubMed]
- Totenhofer, R.; Luck, L.; Wilkes, L. Point of care ultrasound use by Registered Nurses and Nurse Practitioners in clinical practice: An integrative review. Collegian 2021, 28, 456–463. [Google Scholar] [CrossRef]
- Abu-Zidan, F.M.; Cevik, A.A. Diagnostic point-of-care ultrasound (POCUS) for gastrointestinal pathology: State of the art from basics to advanced. World J. Emerg Surg. 2018, 13, 1–14. [Google Scholar] [CrossRef]
- Andronikou, S.; Otero, H.J.; Belard, S.; Heuvelings, C.C.; Ruby, L.C.; Grobusch, M.P. Radiologists should support non-radiologist point-of-care ultrasonography in children: A case for involvement and collaboration. Pediatr. Radiol. 2022, 52, 604–607. [Google Scholar] [CrossRef]
- Ann Galdamez, L. The Evolving Role of Ultrasound in Emergency Medicine. In Essentials of Accident and Emergency Medicine; IntechOpen Limited: London, UK, 2019. [Google Scholar]
- Jain, A.R.; Stead, L.; Decker, W. Ultrasound in emergency medicine: A colorful future in black and white. Int. J. Emerg. Med. 2008, 1, 251–252. [Google Scholar] [CrossRef]
- Burleson, S.L.; Pigott, D.C.; Gullett, J.P.; Greene, C.; Gibson, C.B.; Irvine, S.; Kaminstein, D. Point-of-care ultrasound in resource-limited settings: The PURLS fellowship. Ultrasound J. 2020, 12, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Shaddock, L.; Smith, T. Potential for Use of Portable Ultrasound Devices in Rural and Remote Settings in Australia and Other Developed Countries: A Systematic Review. J. Multidiscip Healthc. 2022, 15, 605–625. [Google Scholar] [CrossRef]
- Arnold, A.C.; Fleet, R.; Lim, D. A case for mandatory ultrasound training for rural general practitioners: A commentary. Rural. Remote Health 2021, 21, 6552. [Google Scholar] [CrossRef]
- Lentz, B.; Fong, T.; Rhyne, R.; Risko, N. A systematic review of the cost-effectiveness of ultrasound in emergency care settings. Ultrasound J. 2021, 13, 16. [Google Scholar] [CrossRef]
- Yang, N.; Yang, H.; Guo, J.J.; Hu, M.; Li, S. Cost-Effectiveness Analysis of Ultrasound Screening for Thyroid Cancer in Asymptomatic Adults. Front. Public Health 2021, 9, 729684. [Google Scholar] [CrossRef] [PubMed]
- Necas, M.; Lambie, B. Pitfalls of Point of Care Ultrasound (POCUS)—A Perspective. J. Urgent Care Med. 2021. Available online: https://www.jucm.com/pitfalls-of-point-of-care-ultrasound-pocus-a-perspective/ (accessed on 1 April 2025).
- HealthManagement.org. Ultrasound Quality is Operator Dependent [Internet]. 2015. Available online: https://healthmanagement.org/c/imaging/news/ultrasound-quality-is-operator-dependent (accessed on 1 April 2025).
- Brau, F.; Martin, S.; Le Bastard, Q.; Ricaud, P.; Legrand, A.; Montassier, E.; Le Conte, P. Impact of emergency physician-performed ultrasound for the evaluation of patients with acute abdominal pain, prospective randomized dual Centre study: Study protocol for a diagnostic trial. Trials 2022, 23, 804. [Google Scholar] [CrossRef] [PubMed]
- Radonjić, T.; Popović, M.; Zdravković, M.; Jovanović, I.; Popadić, V.; Crnokrak, B.; Klašnja, S.; Mandić, O.; Dukić, M.; Branković, M. Point-of-Care Abdominal Ultrasonography (POCUS) on the Way to the Right and Rapid Diagnosis. Diagnostics 2022, 12, 2052. [Google Scholar] [CrossRef]
- Lobo, M.J.C.D.; Tavares, S.C.C.N.M.; Pereira de Almeida, R.P. Point of care prehospital ultrasound in Basic Emergency Services in Portugal. Health Sci. Rep. 2022, 5, e847. [Google Scholar] [CrossRef]
- Revzin, M.V.; Scoutt, L.M.; Garner, J.G.; Moore, C.L. Right Upper Quadrant Pain: Ultrasound First. J. Ultrasound Med. 2017, 36, 1975–1985. [Google Scholar] [CrossRef]
- Spence, S.C.; Teichgraeber, D.; Chandrasekhar, C. Emergent right upper quadrant sonography. J. Ultrasound Med. 2009, 28, 479–496. [Google Scholar] [CrossRef]
- Joshi, G.; Crawford, K.A.; Hanna, T.N.; Herr, K.D.; Dahiya, N.; Menias, C.O. US of right upper quadrant pain in the emergency department: Diagnosing beyond gallbladder and biliary disease. Radiographics 2018, 38, 766–793. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, E.E.; Dewbury, K.C. Biliary Tract Ultrasound. BMUS Bulletin. 2003, 11, 6–14. [Google Scholar] [CrossRef]
- Fenerty, S.D.; Kunchala, S.; Morgan, M.A. Biliary tract emergencies: What the radiologist should know. Appl. Radiol. 2019, 48, 9–16. Available online: https://cdn.agilitycms.com/applied-radiology/PDFs/Issues/AR_07-19_Fenerty-MorganCME_all.pdf (accessed on 1 April 2025). [CrossRef]
- Willis, G.C. Cholangitis: Deadly Cause of Right Upper Quadrant Abdominal Pain. 2016. Available online: http://www.emdocs.net/cholangitis-deadly-cause-of-right-upper-quadrant-abdominal-pain/ (accessed on 1 April 2025).
- Radiology Assistant. Biliary duct pathology—Dilatation [Internet]. Available online: https://radiologyassistant.nl/abdomen/biliary-system/biliary-duct-pathology (accessed on 1 April 2025).
- Pötter-Lang, S.; Ba-Ssalamah, A.; Bastati, N.; Messner, A.; Kristic, A.; Ambros, R.; Herold, A.; Hodge, J.C.; Trauner, M. Modern imaging of cholangitis. Br. J. Radiol. 2021, 94, 20210417. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9327751/ (accessed on 1 April 2025). [CrossRef]
- Emory University School of Medicine, Department of Emergency Medicine. Double Barrel Shotgun. 2018. Available online: https://med.emory.edu/departments/emergency-medicine/sections/ultrasound/case-of-the-month/abdominal/double_barrel_shotgun.html (accessed on 1 April 2025).
- Carbonatto, G. Biliary Obstruction: Double Barrel Sign, Monkey Puzzle Sign. 2017. Available online: https://www.criticalcare-sonography.com/2017/07/31/biliary-obstruction-double-barrel-sign-monkey-puzzle-sign/ (accessed on 1 April 2025).
- European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB). Double Barrel Shotgun Sign [Internet]. Available online: https://efsumb.org/portfolio-item/double-barrel-shotgun-sign/ (accessed on 1 April 2025).
- Indiran, V.; Kokilavani, J. Double-barrel shotgun sign. Abdom. Radiol. 2019, 44, 1197–1198. [Google Scholar] [CrossRef] [PubMed]
- Skoczylas, K.; Pawełas, A. Ultrasound imaging of the liver and bile ducts—Expectations of a clinician. J. Ultrason. 2015, 15, 292–306. Available online: https://pubmed.ncbi.nlm.nih.gov/26673784/ (accessed on 1 April 2025). [CrossRef]
- Virgile, J.; Marathi, R. Cholangitis. 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK558946/ (accessed on 1 April 2025).
- Pollock, G.; Minuk, G.Y. Diagnostic considerations for cholestatic liver disease. J. Gastroenterol. Hepatol. 2017, 32, 1303–1309. [Google Scholar] [CrossRef]
- Ahmed, M. Acute colangites—An update.pdf. World J. Gastrointest. Pathophysiol. 2018, 9, 1–7. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5823698/ (accessed on 1 April 2025). [CrossRef]
- Touzani, S.; El Bouazzaoui, A.; Bouyarmane, F.; Faraj, K.; Houari, N.; Boukatta, B.; Kanjaa, N.; Ardengh, J.C. Factors Associated with Mortality in Severe Acute Cholangitis in a Moroccan Intensive Care Unit: A Retrospective Analysis of 140 Cases. Gastroenterol Res. Pract. 2021, 2021, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.; Jensen, T.G.; Nielsen, S.L.; Schaffalitzky de Muckadell, O.B.; Laursen, S.B. Analysis of patterns of bacteremia and 30-day mortality in patients with acute cholangitis over a 25-year period. Scand J. Gastroenterol 2021, 56, 578–584. [Google Scholar] [CrossRef]
- Rumsey, S.; Winders, J.; MacCormick, A.D. Diagnostic accuracy of Charcot’s triad: A systematic review. ANZ J. Surg. 2017, 87, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Thuluvath, A.J.; Ahn, J.C.; Rattan, P.; Kurdi, A.T.; Peeraphatdit, T.B.; Kamath, M.J.; Lennon, R.J.; Poterucha, J.J.; Petersen, B.T.; Kamath, P.S. Evaluation of Charcot Triad, Reynolds Pentad, and Tokyo Guidelines for Diagnosis of Cholangitis Secondary to Choledocholithiasis Across Patient Age Groups. Mayo Clin. Proc. Innov. Qual Outcomes 2021, 5, 377–387. [Google Scholar] [CrossRef]
- Lindenmeyer, C. Imaging Tests of the Liver and Gallbladder—Hepatic and Biliary Disorders. MSD Man. Prof. Ed. 2019, 1–6. [Google Scholar]
- Steel, P.A.D.; Brenner, B.E. Acute Cholecystitis and Biliary Colic, MEDSCAPE. 2019, pp. 345–348. Available online: https://emedicine.medscape.com/article/1950020-overview (accessed on 1 April 2025).
- Soares, C.B.F.; Braga, F.A.A. Icterícia. In Semiologia em Checklists Abordando Casos Clínicos; Silva, R.A.B., Cunha, T.A., Silva, S.L., Eds.; Atena Editora: Ponta Grossa, Brazil, 2019; pp. 127–133. Available online: https://educapes.capes.gov.br/bitstream/capes/553407/1/E-book-Semiologia-em-Checklists-Abordando-Casos-Clinicos.pdf (accessed on 1 April 2025).
- Javitt, N.B. Cholestatic jaundice. Med. Clin. N. Am. 1975, 59, 817–821. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482279/ (accessed on 1 April 2025). [CrossRef]
- Soliman, M.; Jewell, T. Types of Jaundice What Are the Different Types of. Available online: https://www.healthline.com/health/jaundice-types (accessed on 1 April 2025).
- Henrrique, P.T.N. Acute Cholangitis: Does the Timing of ERCP Alter Outcomes? Universidade de São Paulo Faculdade de Medicina de Ribeirão Preto Centro de Ciências das Imagens E Física Médica. 2019. Available online: https://teses.usp.br/teses/disponiveis/17/17158/tde-05082019-131934/publico/PEDROHENRIQUETARTERNUNES.pdf (accessed on 1 April 2025).
- Tse, F.; Barkun, J.S.; Romagnuolo, J.; Friedman, G.; Bornstein, J.D.; Barkun, A.N. Nonoperative imaging techniques in suspected biliary tract obstruction. HPB 2006, 8, 409–425. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tinusz, B.; Szapáry, L.; Paládi, B.; Tenk, J.; Rumbus, Z.; Pécsi, D.; Szakács, Z.; Varga, G.; Rakonczay, Z., Jr.; Szepes, Z.; et al. Short-Course Antibiotic Treatment Is Not Inferior to a Long-Course One in Acute Cholangitis: A Systematic Review. Dig. Dis. Sci. 2019, 64, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Directory, S. NHS Inform Acute Pancreatitis. Available online: https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-and-gastrointestinal-tract/acute-pancreatitis#treating-acute-pancreatitis (accessed on 1 April 2025).
- Lima, J.C.; Belem, L.F.; Trindade, A.V. ESTUDO DA PANCREATITE AGUDA BILIAR E SUA CORRELAÇÃO COM A DEMORA NO TRATAMENTO DA LITÍASE BILIAR. PIC 2020 2021. [Google Scholar] [CrossRef]
- Sarri, G.; Guo, Y.; Iheanacho, I.; Puelles, J. Moderately severe and severe acute pancreatitis: A systematic review of the outcomes in the USA and European Union-5. BMJ Open Gastroenterol 2019, 6, 1–19. [Google Scholar] [CrossRef]
- Dell’anna, G.; Nunziata, R.; Delogu, C.; Porta, P.; Grassini, M.V.; Dhar, J.; Barà, R.; Bencardino, S.; Fanizza, J.; Mandarino, F.V.; et al. The Role of Therapeutic Endoscopic Ultrasound in Management of Malignant Double Obstruction (Biliary and Gastric Outlet): A Comprehensive Review with Clinical Scenarios. J. Clin. Med. 2024, 13, 7731. [Google Scholar] [CrossRef]
- Li, Q.; Feng, Z.; Miao, R.; Liu, X.; Liu, C.; Liu, Z. Prognosis and survival analysis of patients with pancreatic cancer: Retrospective experience of a single institution. World J. Surg. Oncol. 2022, 20, 1–16. [Google Scholar] [CrossRef]
- Witzigmann, H.; Berr, F.; Ringel, U.; Caca, K.; Uhlmann, D.; Schoppmeyer, K.; Tannapfel, A.; Wittekind, C.; Mossner, J.; Hauss, J.; et al. Surgical and palliative management and outcome in 184 patients with hilar cholangiocarcinoma: Palliative photodynamic therapy plus stenting is comparable to R1/R2 resection. Ann. Surg. 2006, 244, 230–239. [Google Scholar] [CrossRef]
- Neuzillet, C.; Emery, C.; Teissier, C.; Bouée, S.; Lièvre, A. Patient healthcare trajectories of intrahepatic cholangiocarcinoma in France: A nationwide retrospective analysis. Lancet Reg. Health Eur. 2022, 15, 1–9. [Google Scholar] [CrossRef]
- Boyd, C.A.; Branch, D.W.; Sheffield, K.M.; Han, Y.; Kuo, Y.-F.; Goodwin, J.S.; Riall, T.S. Hospital and medical care days in pancreatic cancer. Ann. Surg. Oncol. 2012, 23, 1–7. Available online: https://link.springer.com/article/10.1245/s10434-012-2326-2 (accessed on 1 April 2025). [CrossRef]
- Braconi, C.; Patel, T. Cholangiocarcinoma: New insights into disease pathogenesis and biology. Infect. Dis. Clin. North. Am. 2010, 24, 871–884, vii. [Google Scholar] [CrossRef]
- Ole, I.I.R.; Ko, C.W.; Lee, S.P. Epidemiology and natural history of common bile duct stones. Gastrointest. Endosc. Clin. N. Am. 2002, 12, 165–169. Available online: https://pubmed.ncbi.nlm.nih.gov/12447261/ (accessed on 1 April 2025).
- Biliary Disease. 2018. Available online: https://emedicine.medscape.com/article/171386-overview (accessed on 1 April 2025).
- Miravent, S.; Lobo, M.; Figueiredo, T.; Jiménez, C. Effectiveness of ultrasound screening in right upper quadrant pain: A comparative study in a basic emergency service. Health Sci. Rep. 2023, 6, e1251. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/hsr2.1251 (accessed on 1 April 2025). [CrossRef] [PubMed]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. Available online: https://pubmed.ncbi.nlm.nih.gov/23092060/ (accessed on 1 April 2025). [CrossRef]
- Miravent, S.; Figueiredo, T.; Donchenko, I.; Lobo, M.D.; Cruz, G.; Almeida, R.P. Discrepancies between Screening Sonography and Ultrasound in Emergency Department—A Case Report. Curr. Med. Imaging 2023, 20, 1–4. Available online: https://pubmed.ncbi.nlm.nih.gov/37904564/ (accessed on 1 April 2025). [CrossRef]
- Necas, M.; Prout, K.; Wackrow, W.; Manunui, E.; Lewis, E. The accuracy of sonographers in reporting abnormal ultrasound findings: A prospective study comparing sonographers’ and radiologists’ reports in 1000 hospital patients. Sonography 2023, 10, 57–65. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).