Dietary Supplements as Concentrated Sources of Nutrients with a Nutritional or Physiological Effect for Children with Inflammatory Bowel Disease
Abstract
1. Introduction
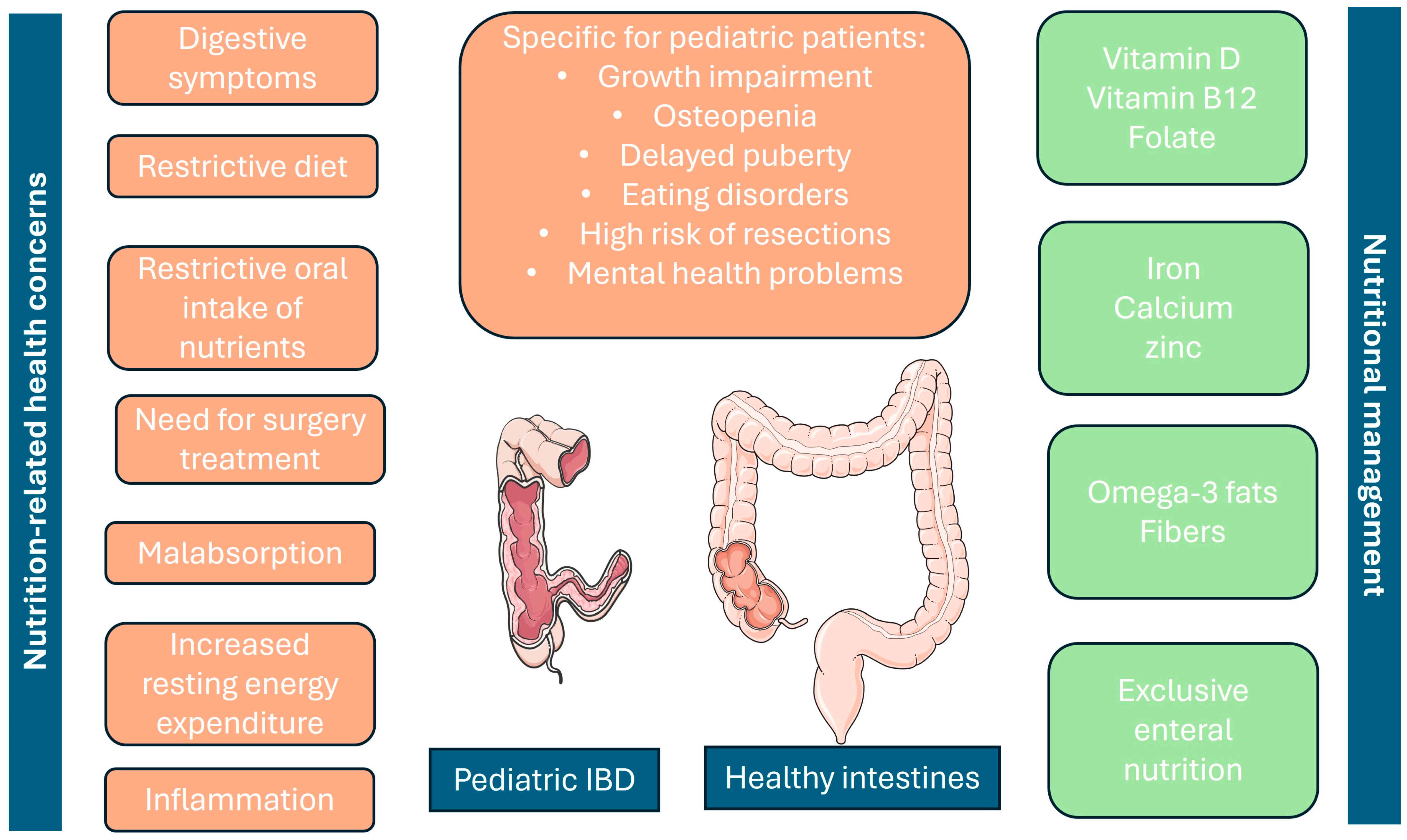
2. Nutritional Concerns in Children with IBD
3. Nutritional Management of Pediatric IBD Patients
4. Vitamin Supplements for Children with IBD
4.1. Vitamin D
4.2. Vitamin B12
4.3. Folate/Folic Acid
4.4. Other Vitamins
5. Mineral Supplements for Pediatric IBD
5.1. Calcium
5.2. Iron
5.3. Zinc
6. Other Supplements under Investigation for Pediatric IBD Nutritional Management
6.1. Omega-3 Fatty Acids
6.2. Boswellia serrata
6.3. Curcumin
6.4. Butyric Acid
6.5. Cannabidiol (CBD) Oil
7. Probiotics in Pediatric IBD
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oliveira, S.B.; Monteiro, I.M. Diagnosis and management of inflammatory bowel disease in children. BMJ 2017, 357, j2083. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, W.S.; Arai, K.; Alex, G.; Treepongkaruna, S.; Kim, K.M.; Choong, C.L.; Mercado, K.C.; Darma, A.; Srivastava, A.; Aw, M.M.; et al. Management and monitoring of pediatric inflammatory bowel disease in the Asia-Pacific region: A position paper by the Asian Pan-Pacific Society for Pediatric Gastroenterology, Hepatology, and Nutrition (APPSPGHAN) PIBD Working Group: Surgical management, disease monitoring, and special considerations. J. Gastroenterol. Hepatol. 2023, 38, 510–522. [Google Scholar] [CrossRef] [PubMed]
- Pigneur, B.; Seksik, P.; Viola, S.; Viala, J.; Beaugerie, L.; Girardet, J.-P.; Ruemmele, F.M.; Cosnes, J. Natural history of Crohn’s disease: Comparison between childhood- and adult-onset disease. Inflamm. Bowel Dis. 2010, 357, 953–961. [Google Scholar] [CrossRef] [PubMed]
- Buderus, S.; Scholz, D.; Behrens, R.; Classen, M.; De Laffolie, J.; Keller, K.M.; Zimmer, K.P.; Koletzko, S. Inflammatory bowel disease in pediatric patients: Characteristics of newly diagnosed patients from the CEDATA-GPGE Registry. Dtsch. Arztebl. Int. 2015, 357, 121–127. [Google Scholar]
- Benchimol, E.I.; Fortinsky, K.J.; Gozdyra, P.; Van den Heuvel, M.; Van Limbergen, J.; Griffiths, A.M. Epidemiology of pediatric inflammatory bowel disease: A systematic review of international trends. Inflamm. Bowel Dis. 2011, 357, 423–439. [Google Scholar] [CrossRef]
- Légeret, C.; Furlano, R.; Köhler, H. Therapy Strategies for Children Suffering from Inflammatory Bowel Disease (IBD)-A Narrative Review. Children 2022, 9, 617. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Day, A.S.; Ledder, O.; Leach, S.T.; Lemberg, D.A. Crohn’s and colitis in children and adolescents. World J. Gastroenterol. 2012, 357, 5862–5869. [Google Scholar] [CrossRef]
- Kim, Y.J. Nutritional concerns in pediatric inflammatory bowel disease. Korean J. Pediatr. 2016, 59, 247–251. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Vortia, E.; Kay, M.; Wyllie, R. The role of growth hormone and insulin-like growth factor-1 in Crohn’s disease: Implications for therapeutic use of human growth hormone in pediatric patients. Curr. Opin. Pediatr. 2011, 23, 545–551. [Google Scholar] [CrossRef]
- Shamir, R.; Phillip, M.; Levine, A. Growth retardation in pediatric Crohn’s disease: Pathogenesis and interventions. Inflamm. Bowel Dis. 2007, 13, 620–628. [Google Scholar] [CrossRef]
- Malik, S.; Ahmed, S.F.; Wilson, M.L.; Shah, N.; Loganathan, S.; Naik, S.; Bourke, B.; Thomas, A.; Akobeng, A.K.; Fagbemi, A.; et al. The effects of anti-TNF-α treatment with adalimumab on growth in children with Crohn’s disease (CD). J. Crohns Colitis 2012, 6, 337–344. [Google Scholar] [CrossRef]
- Gavin, J.; Anderson, C.E.; Bremner, A.R.; Beattie, R.M. Energy intakes of children with Crohn’s disease treated with enteral nutrition as primary therapy. J. Hum. Nutr. Diet. 2005, 18, 337–342. [Google Scholar] [CrossRef]
- Smith, W.J.; Underwood, L.E.; Clemmons, D.R. Effects of caloric or protein restriction on insulin-like growth factor-I (IGF-I) and IGF-binding proteins in children and adults. J. Clin. Endocrinol. Metab. 1995, 80, 443–449. [Google Scholar]
- Burnham, J.; Shults, J.; Semeao, E.; Foster, B.J.; Zemel, B.S.; Stallings, V.A.; Leonard, M.B. Body-composition alterations consistent with cachexia in children and young adults with Crohn disease. Am. J. Clin. Nutr. 2005, 82, 413–420. [Google Scholar] [CrossRef]
- Werkstetter, K.J.; Ullrich, J.; Schatz, S.B.; Prell, C.; Koletzko, B.; Koletzko, S. Lean body mass, physical activity and quality of life in paediatric patients with inflammatory bowel disease and in healthy controls. J. Crohns Colitis 2012, 6, 665–673. [Google Scholar] [CrossRef]
- Gavin, J.; Ashton, J.J.; Heather, N.; Marino, L.V.; Beattie, R.M. Nutritional support in pediatric Crohn’s disease: Outcome at 12 months. Acta Paediatr. 2018, 107, 156–162. [Google Scholar] [CrossRef]
- Gerasimidis, K.; McGrogan, P.; Edwards, C.A. The aetiology and impact of malnutrition in paediatric inflammatory bowel disease. J. Hum. Nutr. Diet. 2011, 24, 313–326. [Google Scholar] [CrossRef]
- Cucinotta, U.; Romano, C.; Dipasquale, V. Diet and Nutrition in Pediatric Inflammatory Bowel Diseases. Nutrients 2021, 13, 655. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Hou, J.K.; Abraham, B.; El-Serag, H. Dietary intake and risk of developing inflammatory bowel disease: A systematic review of the literature. Am. J. Gastroenterol. 2011, 106, 563–573. [Google Scholar] [CrossRef]
- Schreiner, P.; Martinho-Grueber, M.; Studerus, D.; Vavricka, S.R.; Tilg, H.; Biedermann, L. On behalf of Swiss IBDnet, an official working group of the Swiss Society of Gastroenterology Nutrition in Inflammatory Bowel Disease. Digestion 2020, 101, 120–135. [Google Scholar] [CrossRef] [PubMed]
- Forbes, A.; Escher, J.; Hébuterne, X.; Kłęk, S.; Krznaric, Z.; Schneider, S.; Shamir, R.; Stardelova, K.; Wierdsma, N.; Wiskin, A.E.; et al. ESPEN guideline: Clinical nutrition in inflammatory bowel disease. Clin. Nutr. 2017, 36, 321–347. [Google Scholar] [CrossRef]
- Levine, A.; Sigall Boneh, R.; Wine, E. Evolving role of diet in the pathogenesis and treatment of inflammatory bowel diseases. Gut 2018, 67, 1726–1738. [Google Scholar] [CrossRef]
- Khalili, H.; Chan, S.S.; Lochhead, P.; Ananthakrishnan, A.N.; Hart, A.R.; Chan, A.T. The role of diet in the aetiopathogenesis of inflammatory bowel disease. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 525–535. [Google Scholar] [CrossRef]
- Miele, E.; Shamir, R.; Aloi, M.; Assa, A.; Braegger, C.; Bronsky, J.; De Ridder, L.; Escher, J.C.; Hojsak, I.; Kolacek, S.; et al. Nutrition in pediatric inflammatory bowel disease: A position paper on behalf of the Porto Inflammatory Bowel Disease Group of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 687–708. [Google Scholar] [CrossRef] [PubMed]
- Wiskin, A.E.; Wootton, S.A.; Hunt, T.M.; Cornelius, V.R.; Afzal, N.A.; Jackson, A.A.; Beattie, R.M. Body composition in childhood inflammatory bowel disease. Clin. Nutr. 2011, 30, 112–115. [Google Scholar] [CrossRef]
- Massironi, S.; Rossi, R.E.; Cavalcoli, F.A.; Della Valle, S.; Fraquelli, M.; Conte, D. Nutritional deficiencies in inflammatory bowel disease: Therapeutic approaches. Clin. Nutr. 2013, 32, 904–910. [Google Scholar] [CrossRef] [PubMed]
- Fritz, J.; Walia, C.; Elkadri, A.; Pipkorn, R.; Dunn, R.K.; Sieracki, R.; Goday, P.S.; Mariano Cabrera, J. A systematic review of micronutrient deficiencies in pediatric inflammatory bowel disease. Inflamm. Bowel Dis. 2019, 25, 445–459. [Google Scholar] [CrossRef]
- Weisshof, R.; Chermesh, I. Micronutrient deficiencies in inflammatory bowel disease. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 576–581. [Google Scholar] [CrossRef]
- Kaenkumchorn, T.; Kesavan, A. Dietary Management of Pediatric Inflammatory Bowel Disease. J. Med. Food 2019, 22, 1092–1099. [Google Scholar] [CrossRef] [PubMed]
- Directive 2002/46/EC of the European Parliament and of the Council of 10 June 2002 on the approximation of the laws of the Member States relating to food supplements. Off. J. L 2002, 183, 51–57.
- El-Matary, W. Advances in Nutritional Management of Pediatric Inflammatory Bowel Disease. Nutrients 2021, 13, 324. [Google Scholar] [CrossRef] [PubMed]
- Holick, M. Vitamin D deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef] [PubMed]
- Alpert, P.; Shaikh, U. The effects of vitamin D deficiency and insufficiency on the endocrine and paracrine systems. Biol. Res. Nurs. 2007, 9, 117–129. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, I.; Dalzell, A.M.; El-Matary, W. Vitamin D as a therapy for colitis: A systematic review. J. Crohns Colitis 2012, 6, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Narula, N.; Marshall, J.K. Management of inflammatory bowel disease with vitamin D: Beyond bone health. J. Crohns Colitis 2012, 6, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Na, S.Y.; Kim, K.B.; Lim, Y.J.; Song, H.J. Vitamin D and Colorectal Cancer: Current Perspectives and Future Directions. J. Cancer Prev. 2022, 27, 147–156. [Google Scholar] [CrossRef]
- Ehrlich, S.; Mark, A.G.; Rinawi, F.; Shamir, R.; Assa, A. Micronutrient Deficiencies in Children with Inflammatory Bowel Diseases. Nutr. Clin. Pract. 2020, 35, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Liu, Y.; Guo, H.; Jabir, M.S.; Liu, X.; Cui, W.; Li, D. Associations between Folate and Vitamin B12 Levels and Inflammatory Bowel Disease: A Meta-Analysis. Nutrients 2017, 9, 382. [Google Scholar] [CrossRef]
- Aghdassi, E.; Wendland, B.E.; Stapleton, M.; Raman, M.; Allard, J.P. Adequacy of nutritional intake in a Canadian population of patients with Crohn’s disease. J. Am. Diet. Assoc. 2007, 107, 1575–1580. [Google Scholar] [CrossRef]
- Cimpoca, B.A.; Nedelea, F.; Furtuna, M.; Peltecu, G.; Panaitescu, A.M. Managing Crohn’s Disease during Pregnancy. Maedica 2016, 11, 221–226. [Google Scholar]
- Crohn’s & Colitis Foundation of America. Diet, Nutrition and Inflammatory Bowel Disease; Crohn’s & Colitis Foundation of America: New York, NY, USA, 2019. [Google Scholar]
- Ratajczak, A.E.; Szymczak-Tomczak, A.; Rychter, A.M.; Zawada, A.; Dobrowolska, A.; Krela-Kaźmierczak, I. Does Folic Acid Protect Patients with Inflammatory Bowel Disease from Complications? Nutrients 2021, 13, 4036. [Google Scholar] [CrossRef]
- Heyman, M.B.; Garnett, E.A.; Shaikh, N.; Huen, K.; Jose, F.A.; Harmatz, P.; Winter, H.S.; Baldassano, R.N.; Cohen, S.A.; Gold, B.D.; et al. Folate concentrations in pediatric patients with newly diagnosed inflammatory bowel disease. Am. J. Clin. Nutr. 2009, 89, 545–550. [Google Scholar] [CrossRef]
- Temtem, T.A.; Vickers, M.; Whitworth, J. Weekly Folic Acid Is a Convenient and Well-Tolerated Alternative to Daily Dosing in Pediatric Patients with Inflammatory Bowel Disease on Methotrexate. Nutrients 2023, 15, 1586. [Google Scholar] [CrossRef]
- Ghishan, F.K.; Kiela, P.R. Vitamins and Minerals in Inflammatory Bowel Disease. Gastroenterol. Clin. N. Am. 2017, 46, 797–808. [Google Scholar] [CrossRef]
- Valvano, M.; Capannolo, A.; Cesaro, N.; Stefanelli, G.; Fabiani, S.; Frassino, S.; Monaco, S.; Magistroni, M.; Viscido, A.; Latella, G. Nutrition, Nutritional Status, Micronutrients Deficiency, and Disease Course of Inflammatory Bowel Disease. Nutrients 2023, 15, 3824. [Google Scholar] [CrossRef]
- Dignass, A.; Gasche, C.; Dominik Bettenworth, D.; Birgegård, G.; Danese, S.; Gisbert, J.P.; Gomollon, F.; Iqbal, T.; Katsanos, K.; Koutroubakis, I.; et al. European Consensus on the Diagnosis and Management of Iron Deficiency and Anaemia in Inflammatory Bowel Diseases. J. Crohn’s Colitis 2015, 9, 211–222. [Google Scholar] [CrossRef]
- Dunleavy, K.A.; Ungaro, R.C.; Manning, L.; Gold, S.; Novak, J.; Colombel, J.F. Vitamin C Deficiency in Inflammatory Bowel Disease: The Forgotten Micronutrient. Crohns Colitis 2021, 360, otab009. [Google Scholar] [CrossRef]
- Micronutrient Requirements of Children Ages 4 to 13 Years. Linus Pauling Institute, Oregon State University. Available online: https://lpi.oregonstate.edu/mic/life-stages/children#vitamin-A (accessed on 17 July 2024).
- Owczarek, D.; Rodacki, T.; Domagała-Rodacka, R.; Cibor, D.; Mach, T. Diet and nutritional factors in inflammatory bowel diseases. World J. Gastroenterol. 2016, 22, 895–905. [Google Scholar] [CrossRef]
- Calder, P.C. N-3 polyunsaturated fatty acids, inflammation, and inflammatory diseases. Am. J. Clin. Nutr. 2006, 83, 1505S–1519S. [Google Scholar] [CrossRef]
- Calder, P.C. Fatty acids and immune function: Relevance to inflammatory bowel diseases. Int. Rev. Immunol. 2009, 28, 506–534. [Google Scholar] [CrossRef]
- Cabre, E.; Manosa, M.; Gassull, M.A. Omega-3 fatty acids and inflammatory bowel diseases—A systematic review. Br. J. Nutr. 2012, 107, S240–S252. [Google Scholar] [CrossRef]
- Abdel-Tawab, M.; Werz, O.; Schubert-Zsilavecz, M. Boswellia serrata: An overall assessment of in vitro, preclinical, pharmacokinetic and clinical data. Clin. Pharmacokinet. 2011, 50, 349–369. [Google Scholar] [CrossRef]
- Gupta, I.; Parihar, A.; Malhotra, P.; Singh, G.B.; Lüdtke, R.; Safayhi, H.; Ammon, H.P. Effects of Boswellia serrata gum resin in patients with ulcerative colitis. Eur. J. Med. Res. 1997, 2, 37–43. [Google Scholar]
- Gerhardt, H.; Seifert, F.; Buvari, P.; Vogelsang, H.; Repges, R. Therapy of active Crohn disease with Boswellia serrata extract H 15. Z. Gastroenterol. 2001, 39, 11–17. [Google Scholar] [CrossRef]
- Aggarwal, B.B.; Kumar, A.; Bharti, A.C. Anticancer potential of curcumin: Preclinical and clinical studies. Anticancer Res. 2003, 23, 363–398. [Google Scholar]
- Ramsewak, R.S.; DeWitt, D.L.; Nair, M.G. Cytotoxicity, antioxidant and anti-inflammatory activities of curcumins I–III from Curcuma longa. Phytomedicine 2000, 7, 303–308. [Google Scholar] [CrossRef]
- Chan, M.M. Inhibition of tumor necrosis factor by curcumin, a phytochemical. Biochem. Pharmacol. 1995, 49, 1551–1556. [Google Scholar] [CrossRef]
- Kang, B.Y.; Chung, S.W.; Chung, W.; Im, S.; Hwang, S.Y.; Kim, T.S. Inhibition of interleukin-12 production in lipopolysaccharide-activated macrophages by curcumin. Eur. J. Pharmacol. 1999, 384, 191–195. [Google Scholar] [CrossRef]
- Xu, Y.X.; Pindolia, K.R.; Janakiraman, N.; Chapman, R.A.; Gautam, S.C. Curcumin inhibits IL1 alpha and TNF-alpha induction of AP-1 and NF-kB DNA-binding activity in bone marrow stromal cells. Hematopathol. Mol. Hematol. 1997, 11, 49–62. [Google Scholar]
- Taylor, R.A.; Leonard, M.C. Curcumin for inflammatory bowel disease: A review of human studies. Altern. Med. Rev. 2011, 16, 152–156. [Google Scholar]
- Burge, K.; Gunasekaran, A.; Eckert, J.; Chaaban, H. Curcumin and Intestinal Inflammatory Diseases: Molecular Mechanisms of Protection. Int. J. Mol. Sci. 2019, 20, 1912. [Google Scholar] [CrossRef]
- Holt, P.R.; Katz, S.; Kirshoff, R. Curcumin therapy in inflammatory bowel disease: A pilot study. Dig. Dis. Sci. 2005, 50, 2191–2193. [Google Scholar] [CrossRef]
- Hanai, H.; Iida, T.; Takeuchi, K.; Watanabe, F.; Maruyama, Y.; Andoh, A.; Tsujikawa, T.; Fujiyama, Y.; Mitsuyama, K.; Sata, M.; et al. Curcumin maintenance therapy for ulcerative colitis: Randomized, multicenter, double-blind, placebo-controlled trial. Clin. Gastroenterol. Hepatol. 2006, 4, 1502–1506. [Google Scholar] [CrossRef]
- Suskind, D.L.; Wahbeh, G.; Burpee, T.; Cohen, M.; Christie, D.; Weber, W. Tolerability of curcumin in pediatric inflammatory bowel disease: A forced-dose titration study. J. Pediatr. Gastroenterol. Nutr. 2013, 56, 277–279. [Google Scholar] [CrossRef]
- Berni Canani, R.; Di Costanzo, M.; Leone, L.; Pedata, M.; Meli, R.; Calignano, A. Potential beneficial effects of butyrate in intestinal and extraintestinal disease. World J. Gastroenterol. 2011, 17, 1519–1528. [Google Scholar] [CrossRef]
- Hamer, H.M.; Jonkers, D.M.A.E.; Vanhoutvin, S.A.L.W.; Troost, F.J.; Rijkers, G.; de Bruine, A.; Bast, A.; Venema, K.; Brummer, R.-J.M. Effect of butyrate enemas on inflammation and antioxidant status in the colonic mucosa of patients with ulcerative colitis in remission. Clin. Nutr. 2010, 29, 738–744. [Google Scholar] [CrossRef]
- Scheppach, W.; Weiler, F. The butyrate story: Old wine in new bottles? Curr. Opin. Clin. Nutr. Metab. Care 2004, 7, 563–567. [Google Scholar] [CrossRef]
- Büning, C.; Geissler, N.; Prager, M.; Sturm, A.; Baumgart, D.C.; Büttner, J.; Bühner, S.; Haas, V.; Lochs, H. Increased small intestinal permeability in ulcerative colitis: Rather genetic than environmental and a risk factor for extensive disease? Inflamm. Bowel Dis. 2012, 18, 1932–1939. [Google Scholar] [CrossRef]
- Assisi, R.F.; GISDI Study Group. Combined butyric acid/mesalazine treatment in ulcerative colitis with mild-moderate activity. Minerva Gastroenterol. Dietol. 2008, 54, 231–238. [Google Scholar]
- Di Sabotino, A.; Morera, R.; Ciccocioppo, R.; Cazzola, P.; Gotti, S.; Tinozzi, F.P.; Tinozzi, S.; Corazza, G.R. Oral butyrate for mild to moderately active Crohn’s disease. Aliment. Pharmacol. Ther. 2005, 22, 789–794. [Google Scholar] [CrossRef]
- Vernia, P.; Annese, V.; Bresci, G.; d’Albasio, G.; D’Incà, R.; Giaccari, S.; Ingrosso, M.; Mansi, C.; Riegler, G.; Valpiani, D.; et al. Topical butyrate improbe efficacy of 5-ASA in refractory distal ulcerative colitis: Results of a multicentre trial. Eur. J. Clin. Investig. 2003, 33, 244–248. [Google Scholar] [CrossRef] [PubMed]
- Vernia, P.; Monteleone, G.; Grandinetti, G.; Villotti, G.; Di Giulio, E.; Frieri, G.; Marcheggiano, A.; Pallone, F.; Caprilli, R.; Torsoli, A. Combined oral sodium butyrate and mesalazine treatment compared to oral mesalazine alone in ulcerative colitis. Randomized, double-blind, placebo-controlled pilot study. Dig. Dis. Sci. 2000, 45, 976–981. [Google Scholar] [CrossRef]
- Steinhart, A.H.; Hiruki, T.; Brzezinski, A.; Baker, J.P. Treatment of left-sided ulcerative colitis with butyrate enemas: A controlled trial. Aliment. Pharmacol. Ther. 1996, 10, 729–736. [Google Scholar] [CrossRef]
- Vernia, P.; Marcheggiano, A.; Caprilli, R.; Frieri, G.; Corrao, G.; Valpini, D.; DI Paolo, M.C.; Paoluzi, P.; Torsoli, A. Short-chain fatty acid topical treatment in distal ulcerative colitis. Aliment. Pharmacol. Ther. 1995, 9, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Steinhart, A.H.; Brzezinski, A.; Baker, J.P. Treatment of refractory ulcerative proctosigmoiditis with butyrate enemas. Am. J. Gastroenterol. 1994, 89, 179–183. [Google Scholar]
- Scheppach, W.; Sommer, H.; Kirchner, T.; Paganelli, G.M.; Bartram, P.; Christl, S.; Richter, F.; Dusel, G.; Kasper, H. Effect of butyrate enemas on the colonic mucosa in distal ulcerative colitis. Gastroenterology 1992, 103, 51–56. [Google Scholar] [CrossRef]
- Nduma, B.N.; Mofor, K.A.; Tatang, J.; Ekhator, C.; Ambe, S.; Fonkem, E. The Use of Cannabinoids in the Treatment of Inflammatory Bowel Disease (IBD): A Review of the Literature. Cureus 2023, 15, e36148. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Halbmeijer, N.; Groeneweg, M.; De Ridder, L. Cannabis, a potential treatment option in pediatric IBD? Still a long way to go. Expert Rev. Clin. Pharmacol. 2019, 12, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Hoffenberg, E.J.; Mcwilliams, S.K.; Mikulich-Gilbertson, S.K.; Murphy, B.V.; Lagueux, M.; Robbins, K.; Hoffenberg, A.S.; de Zoeten, E.; Hopfer, C.J. Marijuana Use by Adolescents and Young Adults with Inflammatory Bowel Disease. J. Pediatr. 2018, 199, 99–105. [Google Scholar] [CrossRef]
- Hoffenberg, E.J.; Mcwilliams, S.; Mikulich-Gilbertson, S.; Murphy, B.; Hoffenberg, A.; Hopfer, C.J. Cannabis Oil Use by Adolescents and Young Adults With Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Phatak, U.P.; Rojas-Velasquez, D.; Porto, A.; Pashankar, D.S. Prevalence and Patterns of Marijuana Use in Young Adults with Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 261–264. [Google Scholar] [CrossRef] [PubMed]
- Committee on Substance Abuse, Committee on Adolescence; Committee on Substance Abuse Committee on Adolescence. The impact of marijuana policies on youth: Clinical, research, and legal update. Pediatrics 2015, 135, 584–587. [Google Scholar] [CrossRef]
- Miele, E.; Pascarella, F.; Giannetti, E.; Quaglietta, L.; Baldassano, R.N.; Staiano, A. Effect of a probiotic preparation (VSL#3) on induction and maintenance of remission in children with ulcerative colitis. Am. J. Gastroenterol. 2009, 104, 437–443. [Google Scholar] [PubMed]
- Oliva, S.; Di Nardo, G.; Ferrari, F.; Mallardo, S.; Rossi, P.; Patrizi, G.; Cucchiara, S.; Stronati, L. Randomised clinical trial: The effectiveness of Lactobacillus reuteri ATCC 55730 rectal enema in children with active distal ulcerative colitis. Aliment. Pharmacol. Ther. 2012, 35, 327–334. [Google Scholar] [CrossRef]
- Bousvaros, A.; Guandalini, S.; Baldassano, R.N.; Botelho, C.; Evans, J.; Ferry, G.D.; Goldin, B.; Hartigan, L.; Kugathasan, S.; Levy, J.; et al. A randomized, double-blind trial of Lactobacillus GG versus placebo in addition to standard maintenance therapy for children with Crohn’s disease. Inflamm. Bowel Dis. 2005, 11, 833–839. [Google Scholar] [CrossRef]
| Dietary Supplement | Concentration in Pediatric IBD | Biological Function | Needed Daily Intake for Children | Sources |
|---|---|---|---|---|
| Vitamin D (cholecalciferol, ergocalciferol) | Reduced | Bone health, immune function, calcium absorption | 600–1000 IU | Sunlight, fortified milk, fatty fish |
| Vitamin B12 (cyanocobalamin, methylcobalamin) | Reduced | DNA synthesis, hematopoiesis, support neurological function | 250 to 1000 μg of cyanocobalamin every other day | Meat, dairy, fortified cereals |
| Folate (Vitamin B9) (folic acid supplements) | Reduced | DNA synthesis, cell division, red blood cell formation | 800 µg to 1 mg/day | Leafy greens, beans, fortified cereals |
| Vitamin C (ascorbic acid) | Normal to Reduced | Antioxidant, collagen synthesis, immune function | 15–45 mg (varies by age) | Citrus fruits, strawberries, bell peppers |
| Vitamin A (retinyl acetate or retinyl palmitate (preformed vitamin A), beta-carotene (provitamin A), | Normal to Reduced | Vision, immune function, skin health | 300–600 µg (varies by age) | Carrots, sweet potatoes, leafy greens |
| Vitamin B1 (thiamine) | Normal to Reduced | Energy metabolism, nerve function | 0.5–1.2 mg (varies by age) | Whole grains, pork, legumes |
| Vitamin B6 (pyridoxine, pyridoxal, and pyridoxamine) | Normal to Reduced | Protein metabolism, cognitive development, immune function | 600 µg (varies by age) | Poultry, fish, potatoes, bananas |
| Vitamin E (d-alpha-tocopherol or natural mixed tocopherols) | Normal to Reduced | Antioxidant, protects cell membranes | 9–16.4 IU/daily (varies by age) | Nuts, seeds, vegetable oils |
| Vitamin K (phylloquinone or phytonadione) | Normal to Reduced | Blood clotting, bone metabolism | 30–75 µg (varies by age) | Leafy greens, broccoli, brussel sprouts |
| Dietary Supplement | Concentration in Pediatric IBD | Role in the Body | Needed Daily Intake for Children | Sources |
|---|---|---|---|---|
| Iron (ferrous sulfate, ferrous gluconate) | Reduced | Hemoglobin production, oxygen transport | 6 mg/kg/day (varies by age) | Red meat, beans, fortified cereals |
| Calcium (calcium carbonate, calcium citrate) | Reduced | Bone health, muscle function, nerve signaling | 1200–1500 mg/day (varies by age) | Dairy products, leafy greens, tofu |
| Zinc (zinc sulfate, zinc gluconate) | Reduced | Immune function, wound healing, DNA synthesis | 5–10 mg/day (varies by age) | Meat, shellfish, legumes |
| Magnesium (magnesium citrate, etc.) | Reduced | Muscle and nerve function, bone health, energy production | 80–240 mg (varies by age) | Nuts, seeds, whole grains |
| Supplements | Type of Supplements | Effects/Benefits |
|---|---|---|
| Omega-3 fatty acids | Fish oil supplements | Anti-inflammatory effects, improved mucosal healing. |
| Boswellia serrata | Boswellia extract supplements | Anti-inflammatory effects, pain relief. |
| Curcumin | Curcumin extract supplements | Anti-inflammatory effects, antioxidant properties. |
| Butyric acid | Butyrate supplements | Gut mucosal integrity support, anti-inflammatory effects. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shentova, R.; Mihova, A.; Velikova, T. Dietary Supplements as Concentrated Sources of Nutrients with a Nutritional or Physiological Effect for Children with Inflammatory Bowel Disease. Gastroenterol. Insights 2024, 15, 647-660. https://doi.org/10.3390/gastroent15030047
Shentova R, Mihova A, Velikova T. Dietary Supplements as Concentrated Sources of Nutrients with a Nutritional or Physiological Effect for Children with Inflammatory Bowel Disease. Gastroenterology Insights. 2024; 15(3):647-660. https://doi.org/10.3390/gastroent15030047
Chicago/Turabian StyleShentova, Rayna, Antoaneta Mihova, and Tsvetelina Velikova. 2024. "Dietary Supplements as Concentrated Sources of Nutrients with a Nutritional or Physiological Effect for Children with Inflammatory Bowel Disease" Gastroenterology Insights 15, no. 3: 647-660. https://doi.org/10.3390/gastroent15030047
APA StyleShentova, R., Mihova, A., & Velikova, T. (2024). Dietary Supplements as Concentrated Sources of Nutrients with a Nutritional or Physiological Effect for Children with Inflammatory Bowel Disease. Gastroenterology Insights, 15(3), 647-660. https://doi.org/10.3390/gastroent15030047






