Platelet Count/Spleen Diameter Ratio as a Non-Invasive Predictor of Esophageal Varices in Cirrhotic Patients: A Single-Center Experience
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection Methods
2.2. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bacon, B.R. Cirrhosis and its complications. In Chapter 308. Harrison’s Principles of Internal Medicine, 18th ed.; McGraw-Hill: New York, NY, USA, 2014; pp. 1971–1974. [Google Scholar]
- Gupta, T.K.; Chen, L.; Groszmann, R.J. Pathophysiology of portal hypertension. Clin. Liver Dis. 1997, 1, 1–12. [Google Scholar] [CrossRef] [PubMed]
- De Franchis, F.; Primignani, M. Naturalhistory of portal hypertension in patients with cirrhosis. Clin. Liv. Dis. 2001, 5, 645–663. [Google Scholar] [CrossRef] [PubMed]
- Rigo, G.P.; Merighi, A.; Chahin, N.J.; Mastronardi, M.; Codeluppi, P.L.; Ferrari, A.; Armocida, C.; Zanasi, G.; Cristani, A.; Cioni, G.; et al. A prospective study of the ability of three endoscopic classifications to predict hemorrhage from esophageal varices. Gastrointest. Endos. 1992, 38, 425–429. [Google Scholar] [CrossRef]
- DeFranchis, R.; Bosch, J.; Garcia-Tsao, G.; Reiberger, T.; Ripoll, C.; Abraldes, J.G.; Albillos, A.; Baiges, A.; Bajaj, J.; Bañares, R.; et al. Baveno VII-Renewing consensus in portal hypertension. J. Hepatol. 2022, 76, 959–974. [Google Scholar] [CrossRef] [PubMed]
- D’amico, G.; Pagliaro, L.; Bosch, J. The treatment of portal hypertension, ameta-analysis review. Hepatology 1995, 22, 332–354. [Google Scholar] [PubMed]
- Spiegel, B.M.; Targownik, L.; Dulai, G.S.; Karsan, H.A.; Gralnek, I.M. Endoscopic screening for esophageal varices in cirrhosis: Is it ever cost effective? Hepatology 2003, 37, 366–377. [Google Scholar] [CrossRef] [PubMed]
- DeFranchis, R.; Dell’Era, A.; Primignani, M. Diagnosis and monitoring of portal hypertension. Dig. Liver Dis. 2008, 40, 312–317. [Google Scholar] [CrossRef]
- Boregowda, U.; Umapathy, C.; Halim, N.; Desai, M.; Nanjappa, A.; Arekapudi, S.; Theethira, T.; Wong, H.; Roytman, M.; Saligram, S. Update on the management of gastrointestinal varices. World J. Gastrointest. Pharmacol. Ther. 2019, 10, 1–21. [Google Scholar] [CrossRef]
- Pilette, C.; Oberti, F.; Aubé, C.; Rousselet, M.C.; Bedossa, P.; Gallois, Y.; Rifflet, H.; Calès, P. Non-invasive diagnosis of esophageal varices in chronic liver disease. J. Hepatol. 1999, 31, 867–873. [Google Scholar] [CrossRef]
- Ong, J.; Younossi, Z.M. Clinical predictors of large esophageal varices: How accurate are they? Am. J. Gastroenterol. 1999, 94, 3103–3105. [Google Scholar] [CrossRef]
- Madhotra, R.; Mulcahy, H.E.; Willner, I.; Reuben, A. Prediction of esophageal varices in patients with cirrhosis. J. Clin. Gastroenterol. 2002, 34, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Giannini, E.; Botta, F.; Borro, P.; Risso, D.; Romagnoli, P.; Fasoli, A.; Mele, M.R.; Testa, E.; Mansi, C.; Savarino, V.; et al. Platelet count/spleen diameter ratio: Proposal and validation of a non-invasive parameter to predict the presence of oesophageal varices in patients with liver cirrhosis. Gut 2003, 52, 1200–1205. [Google Scholar] [CrossRef]
- D’Amico, G.; Morabito, A. Noninvasive markers of esophageal varices: Another round, not the last. Hepatology 2004, 39, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Chalasani, N.; Imperiale, T.F.; Ismail, A.; Sood, G.; Carey, M.; Wilcox, M.C.; Madichetty, H.; Kwo, P.Y.; Boyer, T.D. Predictors of large esophageal varices in patients with cirrhosis. Am. J. Gastroenterol. Suppl. 1999, 94, 3285–3291. [Google Scholar] [CrossRef] [PubMed]
- Ng, F.H.; Wong, S.Y.; Loo, C.K.; Lam, K.M.; Lai, C.W.; Cheng, C.S. Prediction of esophageal varices in patients with liver cirrhosis. J. Gastroenterol. Hepatol. 1999, 14, 785–790. [Google Scholar] [CrossRef]
- GarciaTsao, G.; Escorsell, A.; Zakko, M.; Patch, D.; Matloff, D.; Grace, N.; Burroughs, A.; Bosch, J.; Groszmann, R.J. Predicting the presence of significant portal hypertension and varices in compensated cirrhotic patients. Hepatology 1997, 26, 257–275. [Google Scholar]
- Goh, S.H.; Tan, W.P.; Lee, S.W. Clinical predictors of bleeding esophageal varices in the ED. Am. J. Emerg. Med. 2005, 23, 531–535. [Google Scholar] [CrossRef]
- Gorka, W.; AlMulla, A.; AlSebayel, M.; Altraif, I.; Gorka, T.S. Qualitative hepatic venous Doppler sonography versus portal flowmetry in predicting the severity of esophageal varices in hepatitis C cirrhosis. Am. J. Roentgenol. 1997, 169, 511–515. [Google Scholar] [CrossRef][Green Version]
- Ishibashi, H.; Higuchi, N.; Shimamura, R.; Hirata, Y.; Kudo, J.; Niho, Y. Sonographic assessment and grading of spleen size. J. Clin. Ultrasound JCU 1991, 19, 21–25. [Google Scholar] [CrossRef]
- Thomopoulos, K.C.; Labropoulou-Karatza, C.; Mimidis, K.P.; Katsakoulis, E.C.; Iconomou, G.; Nikolopoulou, V.N. Non-invasive predictors of the presence of large oesophageal varices in patients with cirrhosis. Dig. Liver Dis. 2003, 35, 473–478. [Google Scholar] [CrossRef]
- Sharma, S.K.; Aggarwal, R. Prediction of large esophageal varices in patients with cirrhosis of the liver using clinical, laboratory and imaging parameters. J. Gastroenterol. Hepatol. 2007, 22, 1909–1915. [Google Scholar] [CrossRef] [PubMed]
- Zaman, A.; Becker, T.; Lapidus, J.; Benner, K. Risk factors for the presence of varices in cirrhotic patients without a history of variceal hemorrhage. Arch. Intern. Med. 2001, 161, 2564–2570. [Google Scholar] [CrossRef] [PubMed]
- Baig, W.W.; Nagaraja, M.V.; Varma, M.; Prabhu, R. Platelet count to spleen diameter ratio for the diagnosis of esophageal varices: Is it feasible? Can. J. Gastroenterol. 2008, 22, 825–828. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Tsao, G.; Bosch, J. Management of varices and variceal hemorrhage in cirrhosis. N. Engl. J. Med. 2010, 362, 823. [Google Scholar] [CrossRef]
- Miceli, G.; Calvaruso, V.; Casuccio, A.; Pennisi, G.; Licata, M.; Pintus, C.; Basso, M.G.; Velardo, M.; Daidone, M.; Amodio, E.; et al. Heart rate variability is associated with disease severity and portal hypertension in cirrhosis. Hepatol. Commun. 2023, 7, e0050. [Google Scholar] [CrossRef]
- Schwarzenberger, E.; Meyer, T.; Golla, V.; Sahdala, N.P.; Min, A.D. Utilization of Platelet Count/Spleen Diameter Ratio in Predicting the Presence of Esophageal Varices in Patients with Cirrhosis. J. Clin. Gastroenterol. 2010, 44, 146–150. [Google Scholar] [CrossRef]
- Sarangapani, A.; Shanmugam, C.; Kalyanasundaram, M.; Rangachari, B.; Thangavelu, P.; Subbarayan, J.K. Non-invasive prediction of large esophageal varices in chronic liver disease patients. Saudi J. Gastroenterol. 2010, 16, 38–42. [Google Scholar] [CrossRef]
- Chawla, S.; Katz, A.; Attar, B.M.; Gupta, A.; Sandhu, D.S.; Agarwal, R. Platelet count/spleen diameter ratio to predict the presence of esophageal varices in patients with cirrhosis. Eur. J. Gastroenterol. Hepatol. 2012, 24, 431–436. [Google Scholar] [CrossRef]
| Baseline Parameters | Study Population (N = 125) | |
|---|---|---|
| Mean ± SD | Median (IQR) | |
| Age (years) | 53.85 ± 12.52 | 53 (45–63) |
| Hb (g/dL) | 10.99 ± 2.42 | 11 (9–13) |
| PC(/cu mm) | 122,935 ± 59,402 | 112,000 (94,500–138,000) |
| SD (mm) | 116.83 ± 25.54 | 121 (93.5–137) |
| PC/SD | 1195.85 ± 864.10 | 963 (749–1283) |
| TB (mg/dL) | 6.26 ± 6.28 | 4.30 (2.6–8.6) |
| DB (mg/dL) | 4.14 ± 4.89 | 2.6 (1.65–4.85) |
| AST (IU/L) | 75.2 ± 45.47 | 65 (42.5–98) |
| ALT (IU/L) | 72.1 ± 55.84 | 61 (31.5–101) |
| TP (gm/dL) | 6.71 ± 0.83 | 6.8 (6.2–7.4) |
| Alb (gm/dL) | 2.71 ± 0.6 | 2.7 (2.4–3.2) |
| ALP (IU/L) | 205 ± 126 | 177 (98.5–287) |
| PT (s) | 23.13 ± 8.34 | 21 (17.45–27.26) |
| INR | 1.43 ± 0.60 | 1.27 (1–1.80) |
| Varices | N | Mean ± SD | Median (IQR) | p Value * | |
|---|---|---|---|---|---|
| Hb (g/dL) | Present | 99 | 10.713 ± 2.3 | 10.6 (9–13) | 0.023 |
| Absent | 26 | 12.019 ± 2.6 | 12.5 (9.7–14) | ||
| PC | Present | 99 | 107,434.3 ± 45,308.5 | 104,000 (90,000–123,000) | <0.001 |
| Absent | 26 | 181,957.7 ± 69,857.8 | 183,000 (146,500–206,250) | ||
| SD | Present | 99 | 121.62 ± 25 | 125 (100–138) | <0.001 |
| Absent | 26 | 98.62 ± 19.1 | 93 (88.5–101.5) | ||
| PC/SD | Present | 99 | 985.3162 ± 730.44 | 873.13 (725.92–873.13) | <0.001 |
| Absent | 26 | 1997.467 ± 876.46 | 1994.62 (1502.5–2455.6) | ||
| TB | Present | 99 | 5.973 ± 6.15 | 3.8 (2.4–7.8) | 0.132 |
| Absent | 26 | 7.396 ± 6.76 | 6.05 (2.88–9.25) | ||
| Age | Present | 99 | 54.93 ± 12.64 | 55 (48–64) | 0.033 |
| Absent | 26 | 49.73 ± 11.34 | 47.5 (43–55) | ||
| DB | Present | 99 | 4.0141 ± 4.76 | 2.6 (1.5–5.1) | 0.391 |
| Absent | 26 | 4.6392 ± 5.43 | 2.85 (2.06–4.76) | ||
| AST | Present | 99 | 72.02 ± 39.89 | 65 (43–96) | 0.321 |
| Absent | 26 | 87.46 ± 61.82 | 82.5 (42–103.26) | ||
| ALT | Present | 99 | 64.55 ± 40.54 | 58 (25–97) | 0.016 |
| Absent | 26 | 100.73 ± 89.1 | 96 (51.75–112.5) | ||
| TP | Present | 99 | 6.794 ± 0.8 | 6.9 (6.2–7.4) | 0.026 # |
| Absent | 26 | 6.385 ± 0.9 | 6.5 (5.73–7.1) | ||
| Alb | Present | 99 | 2.682 ± 0.5 | 2.6 (2.3–3.1) | 0.078 |
| Absent | 26 | 2.835 ± 0.6 | 3.1 (2.6–3.3) | ||
| ALP | Present | 99 | 205.81 ± 126 | 177 (101–287) | 0.631 |
| Absent | 26 | 200 ± 130 | 136.5 (88.25–299.9) | ||
| PT | Present | 99 | 23.796 ± 7.7 | 22 (19–27.6) | 0.015 |
| Absent | 26 | 20.577 ± 10 | 19.8 (13.76–22.5) | ||
| INR | Present | 99 | 1.4817 ± 0.6 | 1.31 (1.1–1.8) | 0.104 |
| Absent | 26 | 1.2458 ± 0.6 | 1.05 (0.8–1.27) |
| Parameters | Grade of Varices | Total | p-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Nil | I | II | III | ||||||||
| n | % | n | % | n | % | n | % | ||||
| SD | 100–150 | 19 | 15.2 | 13 | 10.4 | 4 | 3.2 | 6 | 4.8 | 42 | |
| 150–200 | 7 | 5.6 | 22 | 17.6 | 34 | 27.2 | 20 | 16 | 83 | ||
| Total | 26 | 20.8 | 35 | 28 | 38 | 30.4 | 26 | 20.8 | 125 | 0.735 | |
| PC | 50,000–100,000 | 3 | 2.4 | 9 | 7.2 | 15 | 12 | 20 | 16 | 47 | |
| 100,000–150,000 | 3 | 2.4 | 22 | 17.6 | 19 | 15.2 | 6 | 4.8 | 50 | ||
| >150,000 | 20 | 16 | 4 | 3.2 | 4 | 3.2 | 0 | 0 | 28 | ||
| Total | 26 | 20.8 | 35 | 28 | 38 | 30.4 | 26 | 20.8 | 125 | <0.001 | |
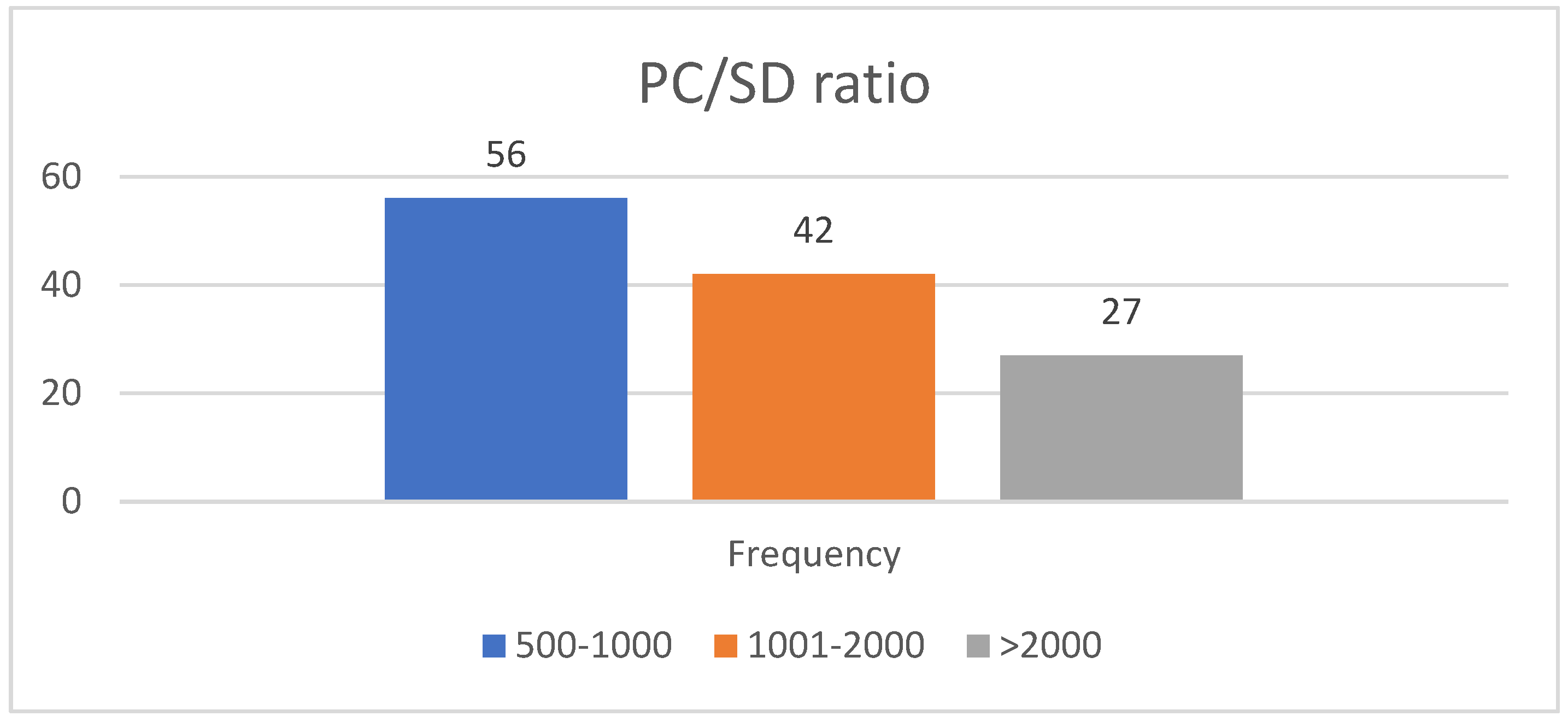
| PC/SD ratio | 500–1000 | 2 | 1.6 | 14 | 11.2 | 23 | 18.4 | 17 | 13.6 | 56 | |
| 1000–2000 | 11 | 8.8 | 16 | 12.8 | 10 | 8 | 5 | 4 | 42 | ||
| >2000 | 13 | 10.4 | 5 | 4 | 5 | 4 | 4 | 3.2 | 27 | ||
| Total | 26 | 35 | 38 | 26 | 125 | <0.001 | |||||
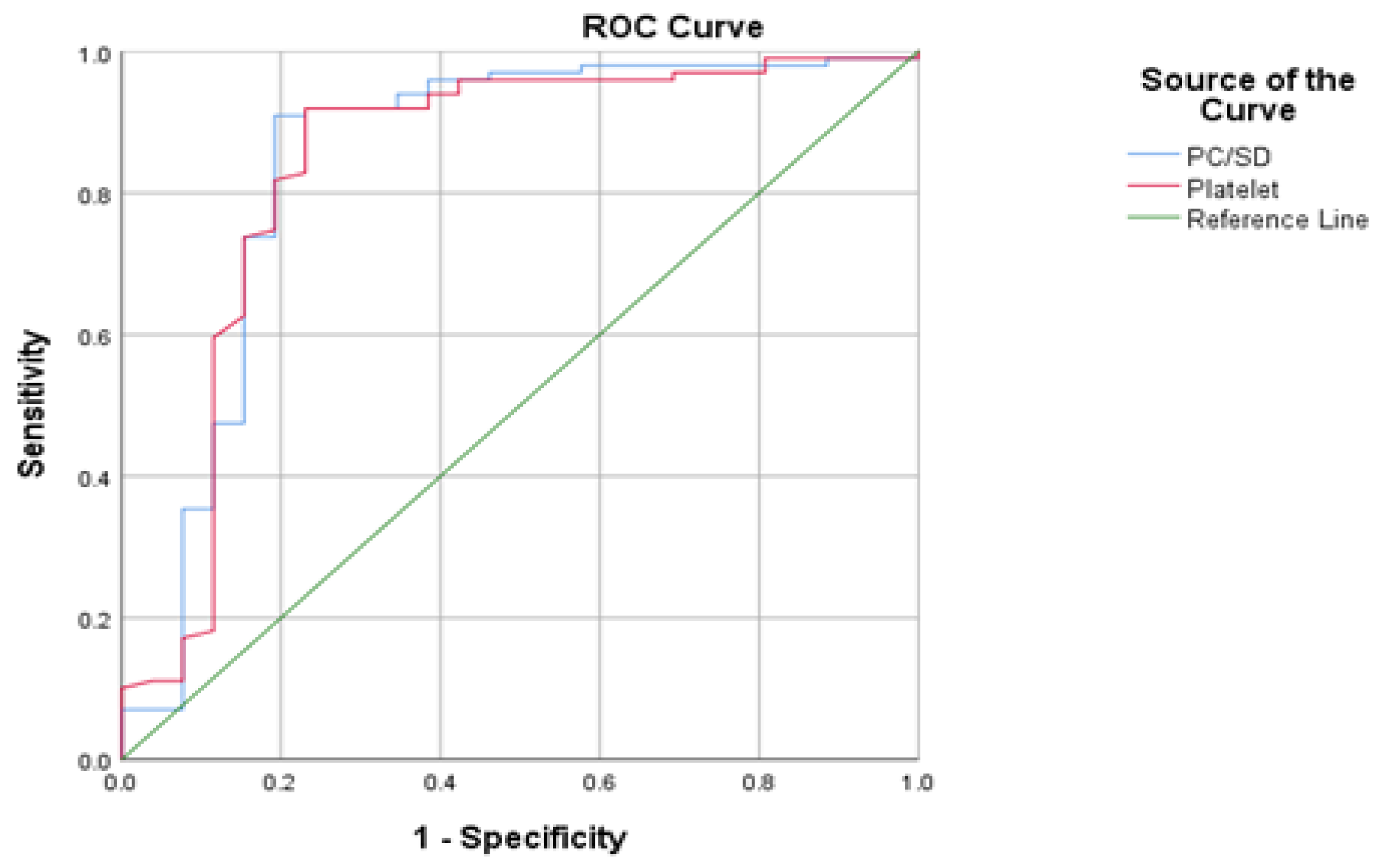
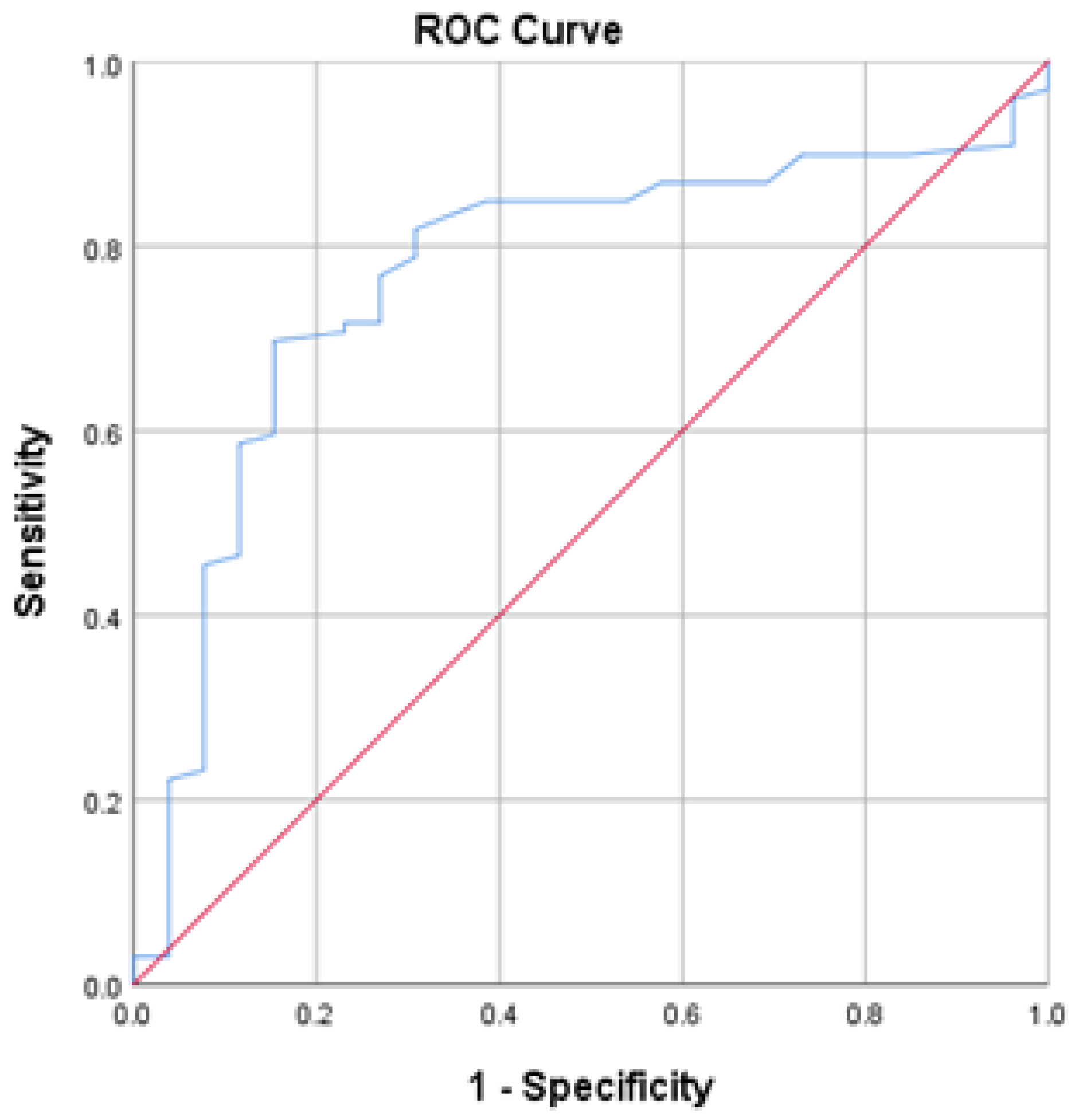
| Study | PC/SD Ratio | Sensitivity (%) | Specificity (%) |
|---|---|---|---|
| Gianni et al. [13] | 909 | 100 | 93 |
| Baig et al. [24] | 909 | 80 | 89 |
| Sarangapani et al. [28] | 909 | 88.5 | 83 |
| Schwarzenberger et al. [27] | 909 | 80 | 40 |
| Present study | 909 | 52.5 | 54.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patil, S.; Patnaik, S.K.; Kanungo, M.; Uthansingh, K.; Narayan, J.; Pradhan, S.; Mishra, D.; Sahu, M.K.; Pati, G.K. Platelet Count/Spleen Diameter Ratio as a Non-Invasive Predictor of Esophageal Varices in Cirrhotic Patients: A Single-Center Experience. Gastroenterol. Insights 2024, 15, 98-106. https://doi.org/10.3390/gastroent15010007
Patil S, Patnaik SK, Kanungo M, Uthansingh K, Narayan J, Pradhan S, Mishra D, Sahu MK, Pati GK. Platelet Count/Spleen Diameter Ratio as a Non-Invasive Predictor of Esophageal Varices in Cirrhotic Patients: A Single-Center Experience. Gastroenterology Insights. 2024; 15(1):98-106. https://doi.org/10.3390/gastroent15010007
Chicago/Turabian StylePatil, Srinith, Swarup Kumar Patnaik, Manjit Kanungo, Kanishka Uthansingh, Jimmy Narayan, Subhasis Pradhan, Debakanta Mishra, Manoj Kumar Sahu, and Girish Kumar Pati. 2024. "Platelet Count/Spleen Diameter Ratio as a Non-Invasive Predictor of Esophageal Varices in Cirrhotic Patients: A Single-Center Experience" Gastroenterology Insights 15, no. 1: 98-106. https://doi.org/10.3390/gastroent15010007
APA StylePatil, S., Patnaik, S. K., Kanungo, M., Uthansingh, K., Narayan, J., Pradhan, S., Mishra, D., Sahu, M. K., & Pati, G. K. (2024). Platelet Count/Spleen Diameter Ratio as a Non-Invasive Predictor of Esophageal Varices in Cirrhotic Patients: A Single-Center Experience. Gastroenterology Insights, 15(1), 98-106. https://doi.org/10.3390/gastroent15010007






