Musculoskeletal Injuries in the Endoscopy Practitioner Risk Factors, Ergonomic Challenges and Prevention—Narrative Review and Perspectives
Abstract
1. Introduction
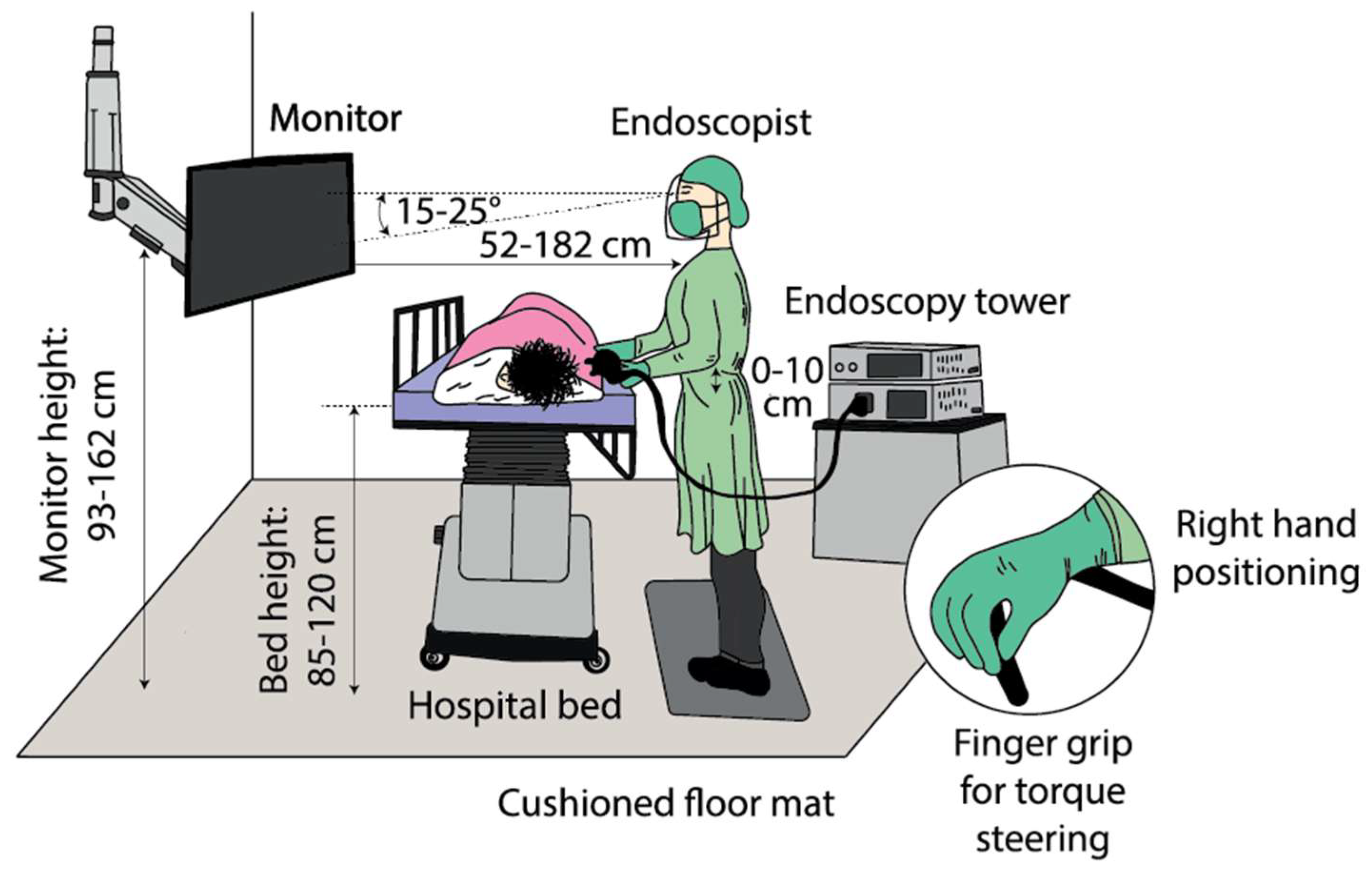
2. Ergonomic Challenges
3. General Problem of the Endoscope Layout
4. New Possibilities in Endoscopy with Regard to Reducing and Preventing Musculoskeletal Injuries
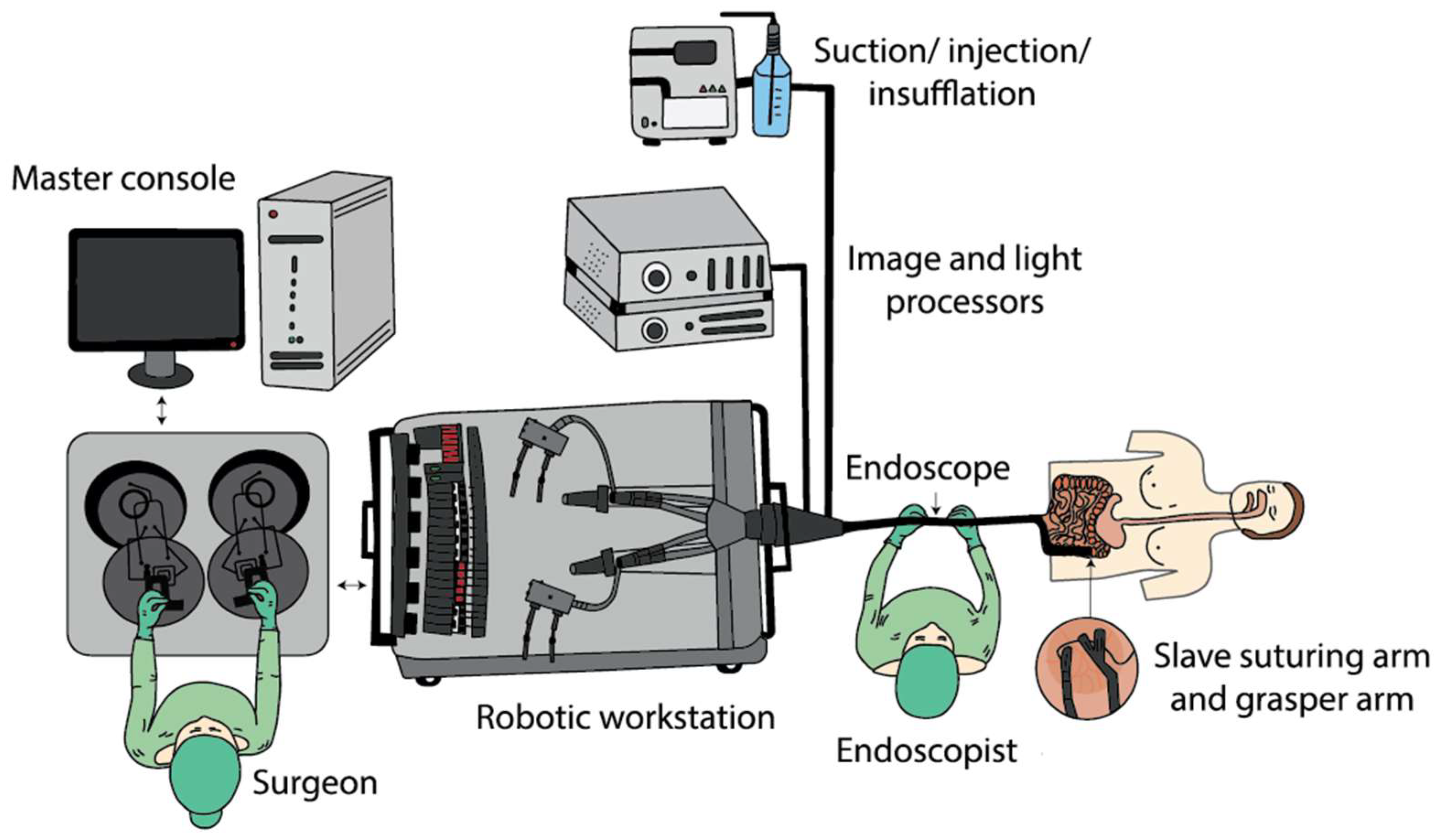
4.1. Robotics
- Platforms capable of high degrees of freedom in forceps manipulation for ESD (endoscopic submucosal dissection) and NOTES (natural orifice transluminal endoscopic surgery).
- Active introduction of the endoscopes to reduce the influence of the operator’s ability and to reduce the discomfort and pain referred by the patients.
- Endoscopic capsule evolution for use in screening for GI pathologies and as a therapeutic method [24].
4.2. “Hands-Free” Endoscopy
4.3. Personal Care Strategies—Floor Mats and Cushioned Insoles
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ESGE | European Society of Gastrointestinal Endoscopy |
| ASGE | American Society for Gastrointestinal Endoscopy |
| GI | Gastrointestinal |
| TSE | Third-space endoscopy |
| MSI | Musculoskeletal injuries |
| ESD | Endoscopic submucosal dissection |
| NOTES | Natural orifice transluminal endoscopic surgery |
| EMG | Electromyography |
References
- Shergill, A.K.; Harris Adamson, C. Failure of an engineered system: The gastrointestinal endoscope. Tech. Gastrointest. Endosc. 2019, 21, 116–123. [Google Scholar] [CrossRef]
- Yung, D.E.; Banfi, T.; Ciuti, G.; Arezzo, A.; Dario, P.; Koulaouzidis, A. Musculoskeletal injuries in gastrointestinal endoscopists: A systematic review. Expert Rev. Gastroenterol. Hepatol. 2017, 11, 939–947. [Google Scholar] [CrossRef] [PubMed]
- Villa, E.; Attar, B.; Trick, W.; Kotwal, V. Endoscopy-related musculoskeletal injuries in gastroenterology fellows. Endosc. Int. Open 2019, 7, E808–E812. [Google Scholar] [CrossRef] [PubMed]
- Austin, K.; Schoenberger, H.; Sesto, M.; Gaumnitz, E.; Teo Broman, A.; Saha, S. Musculoskeletal Injuries Are Commonly Reported Among Gastroenterology Trainees: Results of a National Survey. Dig. Dis. Sci. 2019, 64, 1439–1447. [Google Scholar] [CrossRef]
- Shergill, A.K.; McQuaid, K.R.; Rempel, D. Ergonomics and GI endoscopy. Gastrointest. Endosc. 2009, 70, 145–153. [Google Scholar] [CrossRef]
- Siau, K.; Anderson, J.T. Ergonomics in endoscopy: Should the endoscopist be considered and trained like an athlete? Endosc. Int. Open 2019, 7, E813–E815. [Google Scholar] [CrossRef]
- Walsh, C.M.; Qayed, E.; Aihara, H.; Anand, G.S.; Byrne, K.; Chahal, P.; Dacha, S.; James, T.W.; Kowalski, T.E.; Repaka, A.; et al. Core curriculum for ergonomics in endoscopy. Gastrointest. Endosc. 2021, 93, 1222–1227. [Google Scholar] [CrossRef]
- Shergill, A.K.; McQuaid, K.R. Ergonomic endoscopy: An oxymoron or realistic goal? Gastrointest. Endosc. 2019, 90, 966–970. [Google Scholar] [CrossRef]
- Chang, M.A.; Mitchell, J.; Abbas Fehmi, S.M. Optimizing ergonomics during endoscopy. VideoGIE 2017, 2, 170. [Google Scholar] [CrossRef]
- Anderson, J.T. Optimizing ergonomics during endoscopy training. Tech. Gastrointest. Endosc. 2019, 21, 143–149. [Google Scholar] [CrossRef]
- Singla, M.; Kwok, R.M.; Deriban, G.; Young, P.E. Training the Endo-Athlete: An Update in Ergonomics in Endoscopy. Clin. Gastroenterol. Hepatol. 2018, 16, 1003–1006. [Google Scholar] [CrossRef] [PubMed]
- Ridtitid, W.; Coté, G.A.; Leung, W.; Buschbacher, R.; Lynch, S.; Fogel, E.L.; Watkins, J.L.; Lehman, G.A.; Sherman, S.; McHenry, L. Prevalence and risk factors for musculoskeletal injuries related to endoscopy. Gastrointest. Endosc. 2015, 81, 294–302.e4. [Google Scholar] [CrossRef] [PubMed]
- Harvin, G. Review of Musculoskeletal Injuries and Prevention in the Endoscopy Practitioner. J. Clin. Gastroenterol. 2014, 48, 590–594. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Hammad, H.T.; Wagh, M.S. High prevalence of musculoskeletal symptoms and injuries in third space endoscopists: An international multicenter survey. Endosc. Int. Open 2020, 8, E1481–E1486. [Google Scholar]
- Kamani, L.; Kalwar, H. Ergonomic Injuries in Endoscopists and Their Risk Factors. Clin. Endosc. 2021, 54, 356–362. [Google Scholar] [CrossRef]
- Shah, S.Z.; Rehman, S.T.; Khan, A.; Hussain, M.M.; Ali, M.; Sarwar, S.; Abid, S. Ergonomics of gastrointestinal endoscopies: Musculoskeletal injury among endoscopy physicians, nurses, and technicians. World J. Gastrointest. Endosc. 2022, 14, 142–152. [Google Scholar] [CrossRef]
- Anderson, J. Colonoscopy: Do operator motions and posture count? Endosc. Int. Open 2015, 3, E627–E628. [Google Scholar] [CrossRef][Green Version]
- Hierarchy of Controls|NIOSH|CDC. 2023. Available online: https://www.cdc.gov/niosh/topics/hierarchy/default.html (accessed on 7 July 2023).
- Park, A.E.; Zahiri, H.R.; Hallbeck, M.S.; Augenstein, V.; Sutton, E.; Yu, D.; Lowndes, B.R.; Bingener, J. Intraoperative “Micro Breaks” with Targeted Stretching Enhance Surgeon Physical Function and Mental Focus. Ann. Surg. 2017, 265, 340–346. [Google Scholar] [CrossRef]
- Baillie, J. The endoscope. Gastrointest. Endosc. 2007, 65, 886–893. [Google Scholar] [CrossRef]
- De Groen, P.C. History of the Endoscope [Scanning Our Past]. Proc. IEEE. 2017, 105, 1987–1995. [Google Scholar] [CrossRef]
- Yeung, B.P.M.; Chiu, P.W.Y. Application of robotics in gastrointestinal endoscopy: A review. World J. Gastroenterol. 2016, 22, 1811–1825. [Google Scholar] [CrossRef] [PubMed]
- Kume, K.; Sakai, N.; Goto, T. Development of a novel endoscopic manipulation system: The Endoscopic Operation Robot ver.3. Endoscopy 2015, 47, 815–819. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho Visconti, T.A.; Otoch, J.P.; de Almeida Artifon, E.L. Robotic Endoscopy. A Review of the Literature. Acta Cir. Bras. 2020, 35, e202000206. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.G. The development of robotic flexible endoscopic platforms. Int. J. Gastrointest. Interv. 2020, 9, 9–12. [Google Scholar] [CrossRef]
- Li, Z.; Chiu, P.W.Y. Robotic Endoscopy. Visc. Med. 2018, 34, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Choi, H.S.; Keum, B.; Chun, H.J. Robotics in Gastrointestinal Endoscopy. Appl. Sci. 2021, 11, 11351. [Google Scholar] [CrossRef]
- Bianchi, F.; Masaracchia, A.; Shojaei Barjuei, E.; Menciassi, A.; Arezzo, A.; Koulaouzidis, A.; Stoyanov, D.; Dario, P.; Ciuti, G. Localization strategies for robotic endoscopic capsules: A review. Expert Rev. Med. Devices 2019, 16, 381–403. [Google Scholar] [CrossRef]
- Pullens, H.J.; van der Stap, N.; Rozeboom, E.D.; Schwartz, M.P.; van der Heijden, F.; van Oijen, M.G.; Siersema, P.D.; Broeders, I.A. Colonoscopy with robotic steering and automated lumen centralization: A feasibility study in a colon model. Endoscopy 2016, 48, 286–290. [Google Scholar] [CrossRef]
- Kang, M.; Joe, S.; An, T.; Jang, H.; Kim, B. A novel robotic colonoscopy system integrating feeding and steering mechanisms with self-propelled paddling locomotion: A pilot study. Mechatronics 2021, 73, 102478. [Google Scholar] [CrossRef]
- Duric, T. Ergonometry in Endoscopic Procedures: Prevention of Musculoskeletal Injuries During Endoscopic Procedures by Using Belt-Like Manouvring Device with Joystick Capabilities. Endoscopy 2021, 52, S160. [Google Scholar] [CrossRef]
- Luttmann, A.; Jäger, M.; Laurig, W. Electromyographical indication of muscular fatigue in occupational field studies. Int. J. Ind. Ergon. 2000, 25, 645–660. [Google Scholar] [CrossRef]
- Albayrak, A.; van Veelen, M.A.; Prins, J.F.; Snijders, C.J.; de Ridder, H.; Kazemier, G. A newly designed ergonomic body support for surgeons. Surg. Endosc. 2007, 21, 1835–1840. [Google Scholar] [CrossRef] [PubMed]
- Wiggermann, N.; Keyserling, W. Effects of Anti-Fatigue Mats on Perceived Discomfort and Weight-Shifting During Prolonged Standing. Hum. Factors 2013, 55, 764–775. [Google Scholar] [CrossRef] [PubMed]
- Noor, S.N.A.M.; Ahmad, I.N.; Wahab, N.A.; Ma’arof, M.I.N. A Review of Studies Concerning Prolonged Standing Working Posture. Adv. Eng. Forum 2013, 10, 131–136. [Google Scholar] [CrossRef]
- King, P.M. A comparison of the effects of floor mats and shoe in-soles on standing fatigue. Appl. Ergon. 2002, 33, 477–484. [Google Scholar] [CrossRef]
- Speed, G.; Harris, K.; Keegel, T. The effect of cushioning materials on musculoskeletal discomfort and fatigue during prolonged standing at work: A systematic review. Appl. Ergon. 2018, 70, 300–314. [Google Scholar] [CrossRef]
- Korman, L.Y. An ounce of prevention: Ergonomic training in GI endoscopy. Gastrointest. Endosc. 2020, 92, 1081–1082. [Google Scholar] [CrossRef]
- Singh, S.; Sedlack, R.E.; Cook, D.A. Effects of Simulation-Based Training in Gastrointestinal Endoscopy: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2014, 12, 1611–1623.e4. [Google Scholar] [CrossRef]
- Khanicheh, A.; Shergill, A.K. Endoscope design for the future. Tech. Gastrointest. Endosc. 2019, 21, 167–173. [Google Scholar]

| Author | Year | Ref. No. | Title | Methodology | Key Argument |
|---|---|---|---|---|---|
| Harvin | 2014 | [13] | Review of Musculoskeletal Injuries and Prevention in the Endoscopy Practitioner | Systematic review | Strategies for the management of the risk of musculoskeletal injuries related to the practice of endoscopy include compliance with currently recommended ergonomic practices, education of trainees in ergonomic technique when practising endoscopy, and research toward the modification and development of more ergonomic endoscopes and procedure spaces. |
| Ridtitid et al. | 2015 | [12] | Prevalence and risk factors for musculoskeletal injuries related to endoscopy | Survey | Among endoscopists, there is a high prevalence of injuries definitely or potentially related to endoscopy. Higher procedure volume, more time performing endoscopy per week and cumulative years performing endoscopy are associated with more work-related injuries. |
| Yung et al. | 2017 | [2] | Musculoskeletal injuries in gastrointestinal endoscopists: a systematic review | Systematic review | Comprehensive investigation into the prevalence, types, pathophysiology and methods to minimize endoscopy-related musculoskeletal injuries is vital to ensure the continued efficient provision of endoscopy services in the face of rising demands worldwide. A paradigm shift is required in endoscopic devices and techniques to improve safety and comfort. |
| Villa et al. | 2019 | [3] | Endoscopy-related musculoskeletal injuries in gastroenterology fellows | Survey, cross-sectional study | Injuries were more common in fellows who did not receive proper ergonomic training and education. |
| Austin et al. | 2019 | [4] | Musculoskeletal Injuries Are Commonly Reported Among Gastroenterology Trainees: Results of a National Survey | Electronic survey | Musculoskeletal injuries may affect up to 20% of GI fellows. Female fellows more frequently report injuries and may be at particularly high risk, which has not been found in previously reported surveys of practising gastroenterologists. Standardized curricula on ergonomic considerations and injury prevention are needed to enhance GI fellowship training and reduce injury rates. |
| Han et al. | 2020 | [14] | High prevalence of musculoskeletal symptoms and injuries in third space endoscopists: an international multicenter survey | International multicenter survey | Over two-thirds of endoscopists performing TSE suffer from MSI, with many reporting onset of their symptoms after starting TSE in their practice. Further studies are needed to understand and reduce the risk of MSI in TSE given the growing demand for these procedures and the potential long-term impact of this occupational hazard. |
| Lubna Kamani, Hamid Kalwar | 2021 | [15] | Ergonomic Injuries in Endoscopists and Their Risk Factors | Survey, cross-sectional study | Endoscopists are at high risk of developing ergonomic injuries, representing the negative potential of the endoscopy-associated workload. To overcome these issues, an appropriate strategic framework needs to be designed to avoid occupational compromises. |
| Shah et al. | 2022 | [16] | Ergonomics of gastrointestinal endoscopies: Musculoskeletal injury among endoscopy physicians, nurses, and technicians | Observational cross-section study | Three-fourths of our endoscopists reported MSI, of whom more than half were not sure or attributed this problem to endoscopy. The prevalence of MSI warrants urgent attention. |
| NAME | APPROVAL STATUS | CLINICAL TRIAL | PURPOSE OF USE | TECHNICAL FEATURES |
|---|---|---|---|---|
| ENDOMASTER EASE SYSTEM (ENDOMASTER PTE., SINGAPORE) | No | Animal Human | Stomach ESD Colon ESD | Console for remote control of the robotic arms, independent endoscopic platform |
| ENDOLUMINAL ASSISTANT FOR SURGICAL ENDOSCOPY (ICUBE LABORATORY, STRASBOURG, FRANCE) | No | Animal | Colon ESD | Master console and a detachable flexible endoscope with three working channels |
| FLEX ROBOTIC SYSTEM (MEDROBOTICS, RAYNHAM, MA, USA) | FDA | Animal Human | Colon ESD | Robotic endoscope, mechanical single-use flexible instruments and a master console with a touchscreen, HD visual display and a joystick |
| K-FLEX (EASYENDO SURGICAL, DAEJEON, KOREA) | No | Explanted animal organs | Colon ESD | Bendable overtube, two exchangeable surgical instrument modules, a driving robot arm and a master console |
| NAME | SINGLE-USE | APPROVAL STATUS | ACTUATION PRINCIPLE | TECHNICAL FEATURES |
|---|---|---|---|---|
| THE AER-O-SCOPETM COLONOSCOPE SYSTEM (GI VIEW LTD., TEL AVIV, ISRAEL) | Yes | FDA, CE | Electro-pneumatic mechanisms | Self-propelled, disposable colonoscope |
| ENDOTICS (ERA ENDOSCOPY SRL, CASCINA, ITALY) | Yes | CE | Electro-pneumatic mechanisms | Self-propelled, joystick-controlled endoscope |
| COLONOSIGHT (STRYKER GI, HAIFA, ISRAEL) | Yes | FDA | Electro-pneumatic mechanisms | Self-advancing system composed of a reusable colonoscope and a wrapped disposable multilumen sheath |
| NEOGUIDE ENDOSCOPY SYSTEM (INTUITIVE SURGICAL INC., SUNNYVALE, CA, USA) | Yes | FDA | Electro-mechanical actuation | 16-segment insertion tube that controls the snake-like movement of the endoscope |
| ENDOCULUS (UNIVERSITY OF COLORADO, BOULDER, CO, USA) | No | No | Electrically actuated mechanisms | Small tank-like robot that can navigate the colon |
| MAGNETIC FLEXIBLE ENDOSCOPE (VANDERBILT UNIVERSITY, NASHVILLE, TN, USA) | No | No | Magnetic-actuated tethered robotic colonoscopes | Magnet-embedded endoscope, an actuated permanent magnet external to the patient and control software |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Durič, T.; Cibulková, I.; Hajer, J. Musculoskeletal Injuries in the Endoscopy Practitioner Risk Factors, Ergonomic Challenges and Prevention—Narrative Review and Perspectives. Gastroenterol. Insights 2023, 14, 352-362. https://doi.org/10.3390/gastroent14030026
Durič T, Cibulková I, Hajer J. Musculoskeletal Injuries in the Endoscopy Practitioner Risk Factors, Ergonomic Challenges and Prevention—Narrative Review and Perspectives. Gastroenterology Insights. 2023; 14(3):352-362. https://doi.org/10.3390/gastroent14030026
Chicago/Turabian StyleDurič, Tadej, Ivana Cibulková, and Jan Hajer. 2023. "Musculoskeletal Injuries in the Endoscopy Practitioner Risk Factors, Ergonomic Challenges and Prevention—Narrative Review and Perspectives" Gastroenterology Insights 14, no. 3: 352-362. https://doi.org/10.3390/gastroent14030026
APA StyleDurič, T., Cibulková, I., & Hajer, J. (2023). Musculoskeletal Injuries in the Endoscopy Practitioner Risk Factors, Ergonomic Challenges and Prevention—Narrative Review and Perspectives. Gastroenterology Insights, 14(3), 352-362. https://doi.org/10.3390/gastroent14030026






