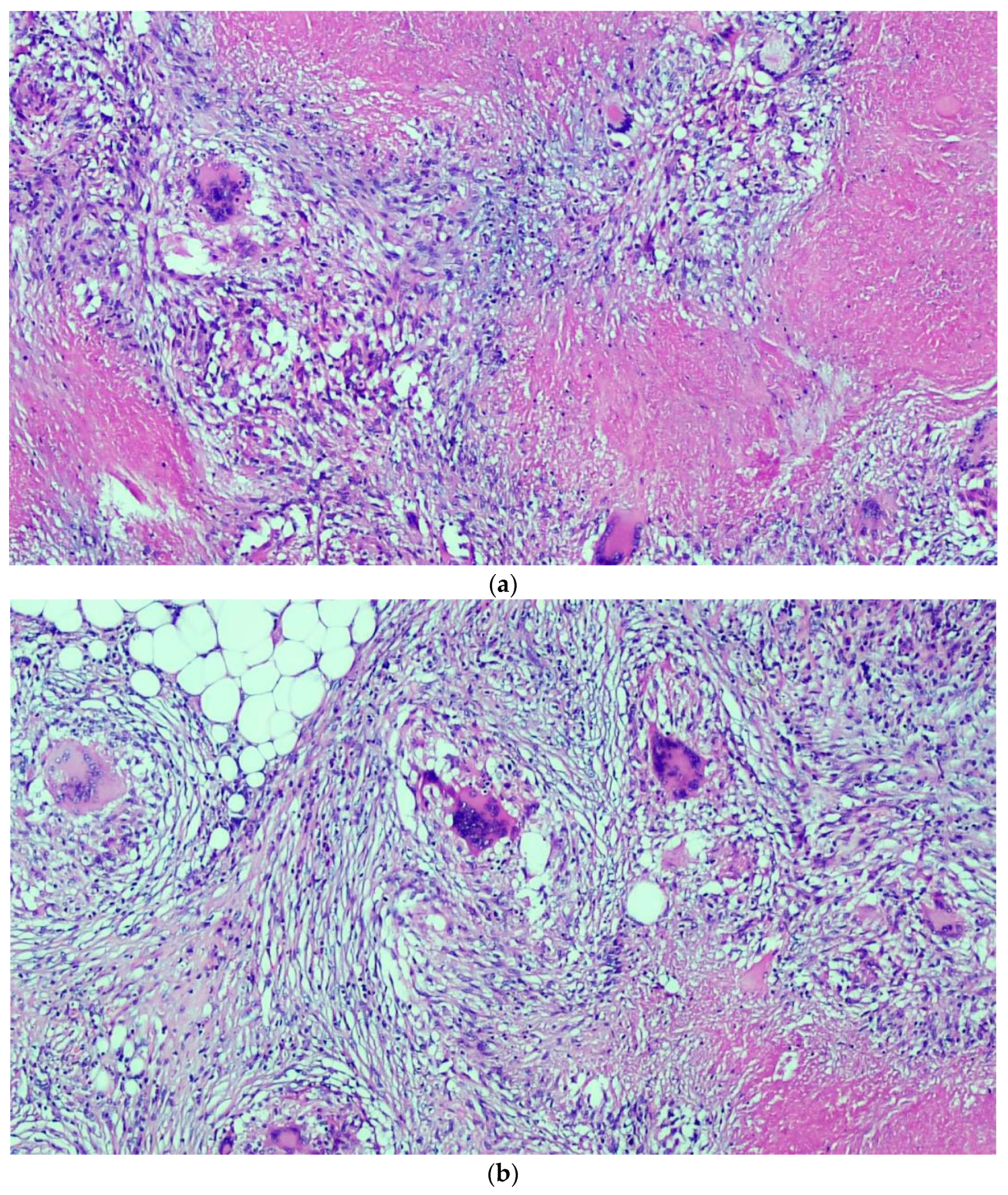
Peritoneal Tuberculosis Mimicking Ovarian Cancer: Gynecologic Ultrasound Evaluation with Histopathological Confirmation
Abstract
1. Introduction
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Gopalaswamy, R.; Shanmugam, S.; Mondal, R.; Subbian, S. Of tuberculosis and non-tuberculous mycobacterial infections—A comparative analysis of epidemiology, diagnosis and treatment. J. Biomed. Sci. 2020, 27, 74. [Google Scholar] [CrossRef] [PubMed]
- Adigun, R.; Singh, R. Tuberculosis. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan; StatPearls: Orlando, FL, USA, 2020. [Google Scholar]
- Migliori, G.B.; Tiberi, S.; García-Basteiro, A.L.; Duarte, R. Tuberculosis and its future in the COVID-19 era: The Pulmonology series 2021. Pulmonology 2021, 27, 94–96. [Google Scholar] [CrossRef] [PubMed]
- Sharma, J.B.; Jain, S.K.; Pushparaj, M.; Roy, K.K.; Malhotra, N.; Zutshi, V.; Rajaram, S. Abdomino-peritoneal tuberculosis masquerading as ovarian cancer: A retrospective study of 26 cases. Arch. Gynecol. Obstet. 2010, 282, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Qu, X.; Liu, X.; Ding, L.; Yue, Y. Female Peritoneal Tuberculosis with Ascites, Pelvic Mass, or Elevated CA 125 Mimicking Advanced Ovarian Cancer: A Retrospective Study of 26 Cases. J. Coll Physicians Surg Pak 2019, 29, 588–589. [Google Scholar] [CrossRef] [PubMed]
- Sophia De Saram, J.S.F. Gastrointestinal and Peritoneal Tuberculosis. In Extrapulmonary Tuberculosis, 1st ed.; Alper, S., Hakan, E., Eds.; Springer International Publishing: Cham, Switzerland; pp. 25–42.
- Norbis, L.; Alagna, R.; Tortoli, E.; Codecasa, L.; Migliori, G.B.; Cirillo, D.M. Challenges and perspectives in the diagnosis of extrapulmonary tuberculosis. Expert Rev. Anti-Infective Ther. 2014, 12, 633–647. [Google Scholar] [CrossRef] [PubMed]
- Hulnick, D.H.; Megibow, A.; Naidich, D.; Hilton, S.; Cho, K.C.; Balthazar, E.J. Abdominal tuberculosis: CT evaluation. Radiology 1985, 157, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Flores, L.S.; Solís, A.H.; Gutiérrez, A.E.; José, L.C.C.; Ortiz, I.C.; González, H.G.; Martínez, E.L.; Sabido, R.C. Peritoneal tuberculosis: A persistent diagnostic dilemma, use complete diagnostic methods. Rev. Méd. Hosp. Gen. Méx. 2015, 78, 55–61. [Google Scholar]
- Koff, A.; Azar, M.M. Diagnosing peritoneal tuberculosis. BMJ Case Rep. 2020, 13, e233131. [Google Scholar] [CrossRef] [PubMed]
- Guirat, A.; Koubaa, M.; Mzali, R.; Abid, B.; Ellouz, S.; Affes, N.; Ben Jemaa, M.; Frikha, F.; Ben Amar, M.; Beyrouti, M.I. Peritoneal tuberculosis. Clin. Res. Hepatol. Gastroenterol. 2011, 35, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Zhang, Q.; Guan, Q.; Xu, J.F.; Shi, Q.L. Abdominopelvic tuberculosis mimicking advanced ovarian cancer and pelvic inflammatory disease: A series of 28 female cases. Arch. Gynecol. Obstet. 2014, 289, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Devi, L.; Tandon, R.; Goel, P.; Huria, A.; Saha, P.K. Pelvic tuberculosis mimicking advanced ovarian malignancy. Trop. Dr. 2012, 42, 144–146. [Google Scholar] [CrossRef] [PubMed]
- Martingano, D.; Cagle-Colon, K.; Chiaffarano, J.; Marcus, A.; Contreras, D. Pelvic Tuberculosis Diagnosed during Operative Laparoscopy for Suspected Ovarian Cancer. Case Rep. Obstet. Gynecol. 2018, 6452721. [Google Scholar] [CrossRef] [PubMed]
- Sharma, J.B.; Roy, K.K.; Pushparaj, M.; Kumar, S.; Malhotra, N.; Mittal, S. Laparoscopic findings in female genital tuberculosis. Arch. Gynecol. Obstet. 2008, 278, 359–364. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arezzo, F.; Cazzato, G.; Loizzi, V.; Ingravallo, G.; Resta, L.; Cormio, G. Peritoneal Tuberculosis Mimicking Ovarian Cancer: Gynecologic Ultrasound Evaluation with Histopathological Confirmation. Gastroenterol. Insights 2021, 12, 278-282. https://doi.org/10.3390/gastroent12020024
Arezzo F, Cazzato G, Loizzi V, Ingravallo G, Resta L, Cormio G. Peritoneal Tuberculosis Mimicking Ovarian Cancer: Gynecologic Ultrasound Evaluation with Histopathological Confirmation. Gastroenterology Insights. 2021; 12(2):278-282. https://doi.org/10.3390/gastroent12020024
Chicago/Turabian StyleArezzo, Francesca, Gerardo Cazzato, Vera Loizzi, Giuseppe Ingravallo, Leonardo Resta, and Gennaro Cormio. 2021. "Peritoneal Tuberculosis Mimicking Ovarian Cancer: Gynecologic Ultrasound Evaluation with Histopathological Confirmation" Gastroenterology Insights 12, no. 2: 278-282. https://doi.org/10.3390/gastroent12020024
APA StyleArezzo, F., Cazzato, G., Loizzi, V., Ingravallo, G., Resta, L., & Cormio, G. (2021). Peritoneal Tuberculosis Mimicking Ovarian Cancer: Gynecologic Ultrasound Evaluation with Histopathological Confirmation. Gastroenterology Insights, 12(2), 278-282. https://doi.org/10.3390/gastroent12020024










