Impact of Statin Therapy on the Risk of Stroke Recurrence, Mortality, and Dementia After Ischemic Stroke (ISMARDD Study): A Comprehensive Meta-Analysis
Abstract
1. Introduction
Objectives
- Primary Questions
- (a)
- In the broader IS cohort:
- i.
- What is the prevalence of all-cause mortality, stroke recurrence and PSD/PSCI in statin users, nonusers and overall?
- ii.
- Is post-stroke statin use associated with all-cause mortality, stroke recurrence and PSD/PSCI?
- (b)
- Variations in statin parameters:
- i.
- Is increasing statin intensity associated with all-cause mortality and stroke recurrence?
- ii.
- What is the prevalence of all-cause mortality and stroke recurrence by statin intensity, type, timing of initiation and solubility?
- Secondary Questions
- (a)
- In CE/AF-related IS subgroups:
- i.
- What is the prevalence of all-cause mortality and stroke recurrence in statin users, nonusers and overall?
- ii.
- Is post-stroke statin use associated with all-cause mortality and stroke recurrence?
- (b)
- In IS patients with low baseline LDL-cholesterol:
- i.
- What is the prevalence of all-cause mortality in statin users, nonusers, and overall?
- ii.
- Is post-stroke statin use associated with all-cause mortality?
- (c)
- Is post-stroke statin use associated with changes in CRP levels in IS patients?
2. Materials and Methods
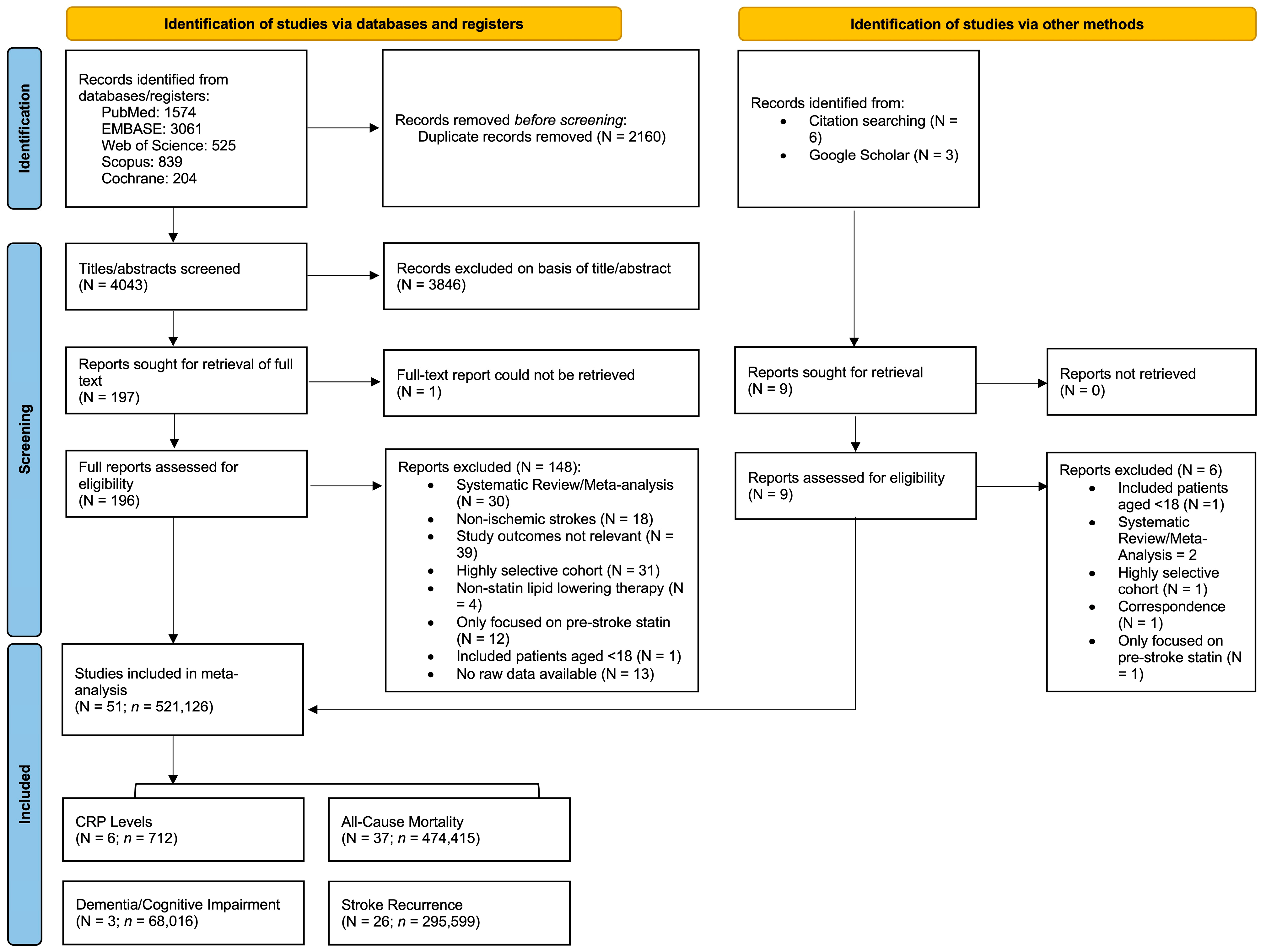
2.1. Literature Search and Study Selection
2.2. Inclusion and Exclusion Criteria
- (a)
- participants aged 18 years or older;
- (b)
- patients receiving statin therapy after IS (either pre-stroke statin continued or newly initiated statin after stroke);
- (c)
- studies recruiting patients with all IS subtypes, or those focused on CE/AF-related strokes or patients with low baseline LDL-cholesterol;
- (d)
- included data on the outcomes of PSD/PSCI, stroke recurrence, all-cause mortality; or reported mean and standard deviation or median and interquartile ranges of CRP levels;
- (e)
- English language publications or translated to English; and
- (f)
- sample size of at least 20 patients.
- (a)
- included hemorrhagic stroke patients;
- (b)
- restricted to highly select cohorts, such as those with cancer or excluded key IS subtypes, such as those focused only on non-CE strokes;
- (c)
- did not contain raw data for outcomes;
- (d)
- only reported on pre-stroke statin use;
- (e)
- case reports, small case series, or studies with insufficient sample size;
- (f)
- systematic reviews and meta-analyses;
- (g)
- non-English or not translated.
2.3. Data Extraction
- Study demographics—author, publication year, country, study design, cohort size.
- Control and intervention characteristics—statin type, dose, and timing of initiation.
- Patient demographics—age, sex, National Institute of Health Stroke Scale (NIHSS) score, IS subtype according to Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification, comorbidities (hypertension, diabetes mellitus, atrial fibrillation, coronary artery disease, dyslipidemia, previous stroke) and lifestyle factors (smoking and alcohol consumption).
- Clinical outcomes—all-cause mortality (within 3 months, 1 year and after 1 year), stroke recurrence (within and after 1 year), any PSD/PSCI diagnosis and CRP levels (within 3–7 days and after 7 days).
2.4. Methodological Quality Assessment of Included Studies
2.5. Statistical Analyses
2.5.1. Prevalence Estimations
2.5.2. Outcome Associations
2.5.3. Statistical Significance, Heterogeneity and Variance
2.5.4. Bias and Sensitivity Analyses
2.6. Certainty of Evidence Assessment
3. Results
3.1. Description of Included Studies
3.2. Primary Analysis
3.2.1. Impact of Post-Stroke Statin Use on Clinical Outcomes in Broader Ischemic Stroke Cohorts
Prevalence Estimations
- All-Cause Mortality
- Stroke Recurrence
- Post-Stroke Dementia/Cognitive Impairment
Outcome Associations
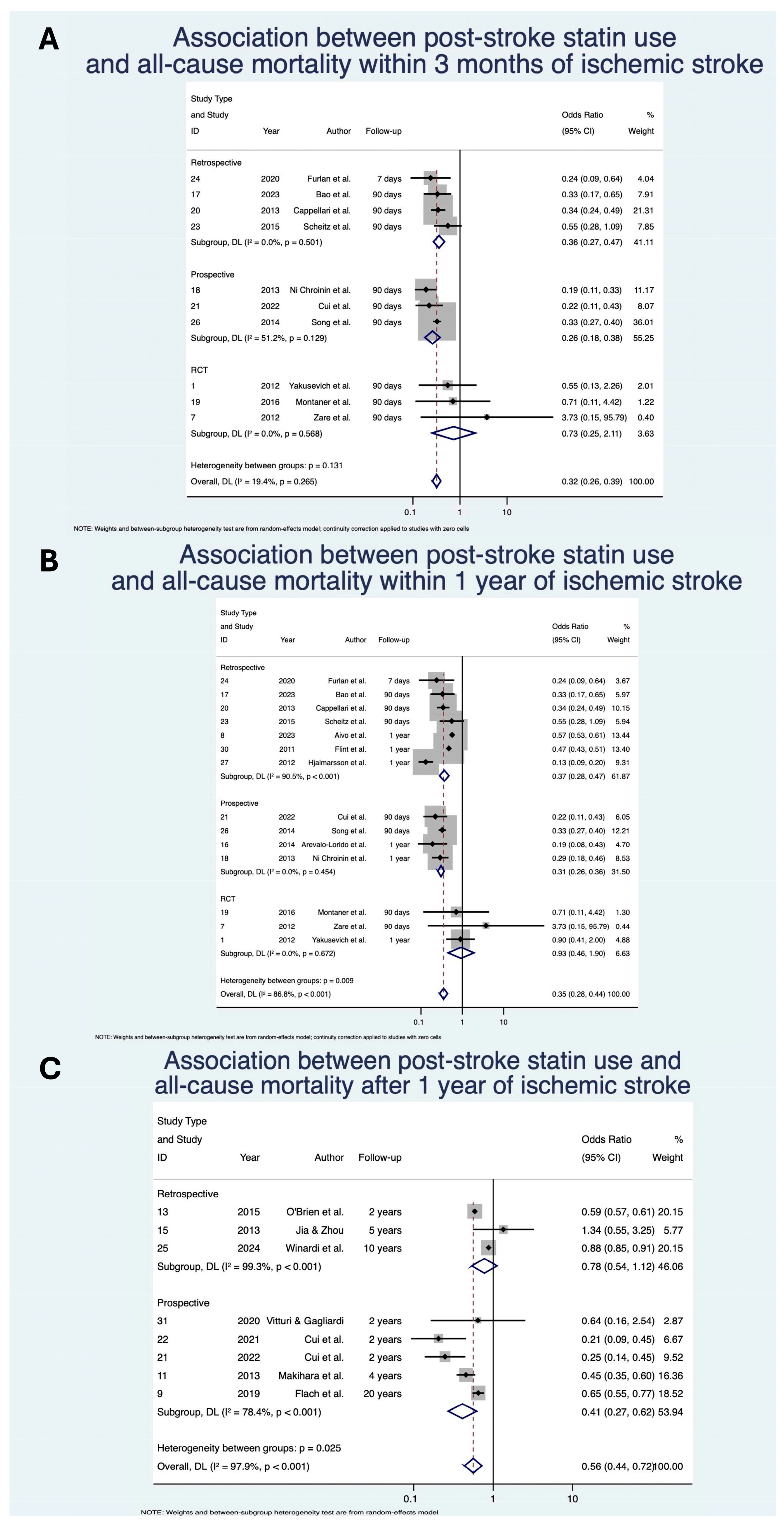
- All-Cause Mortality
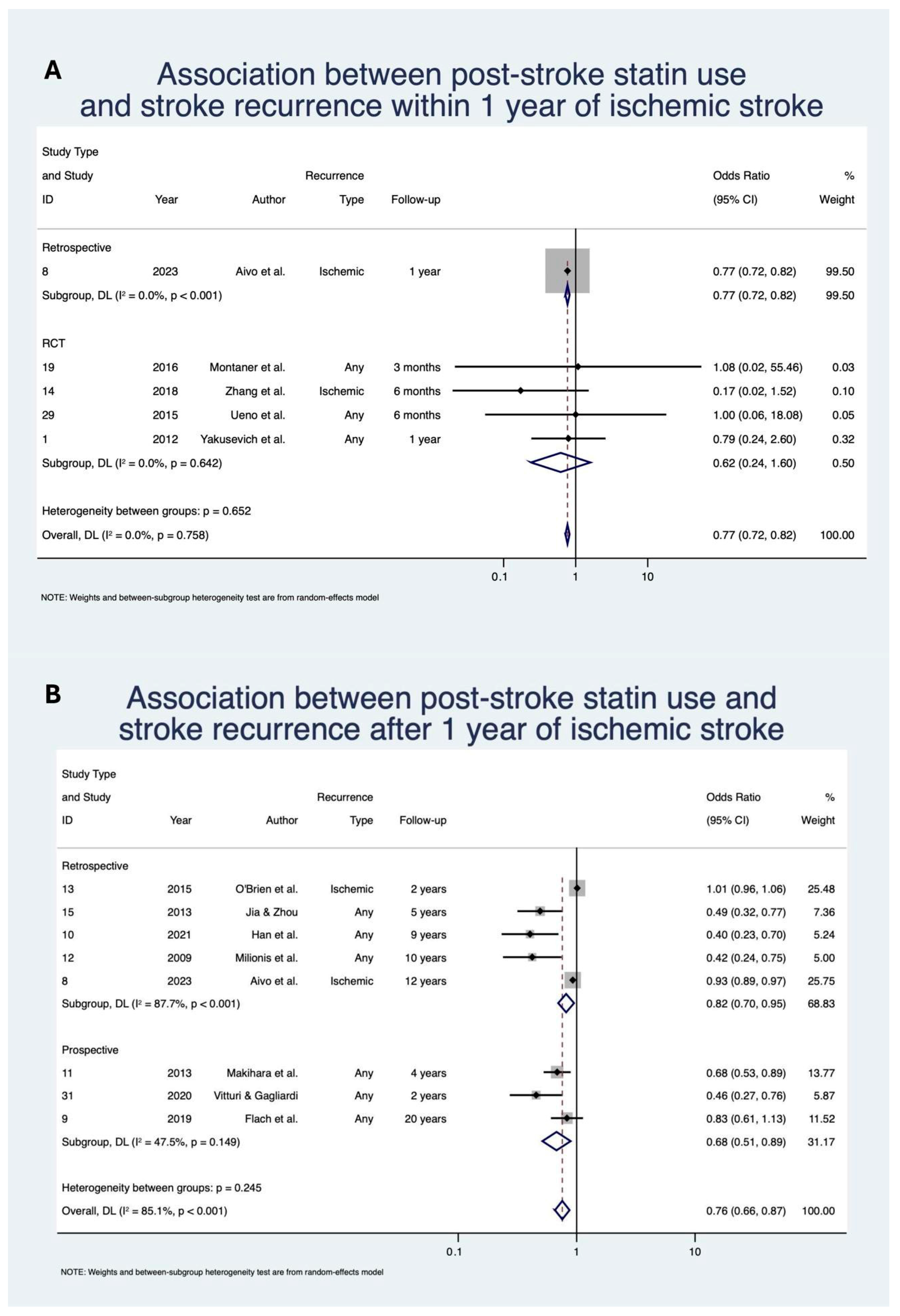
- Stroke Recurrence
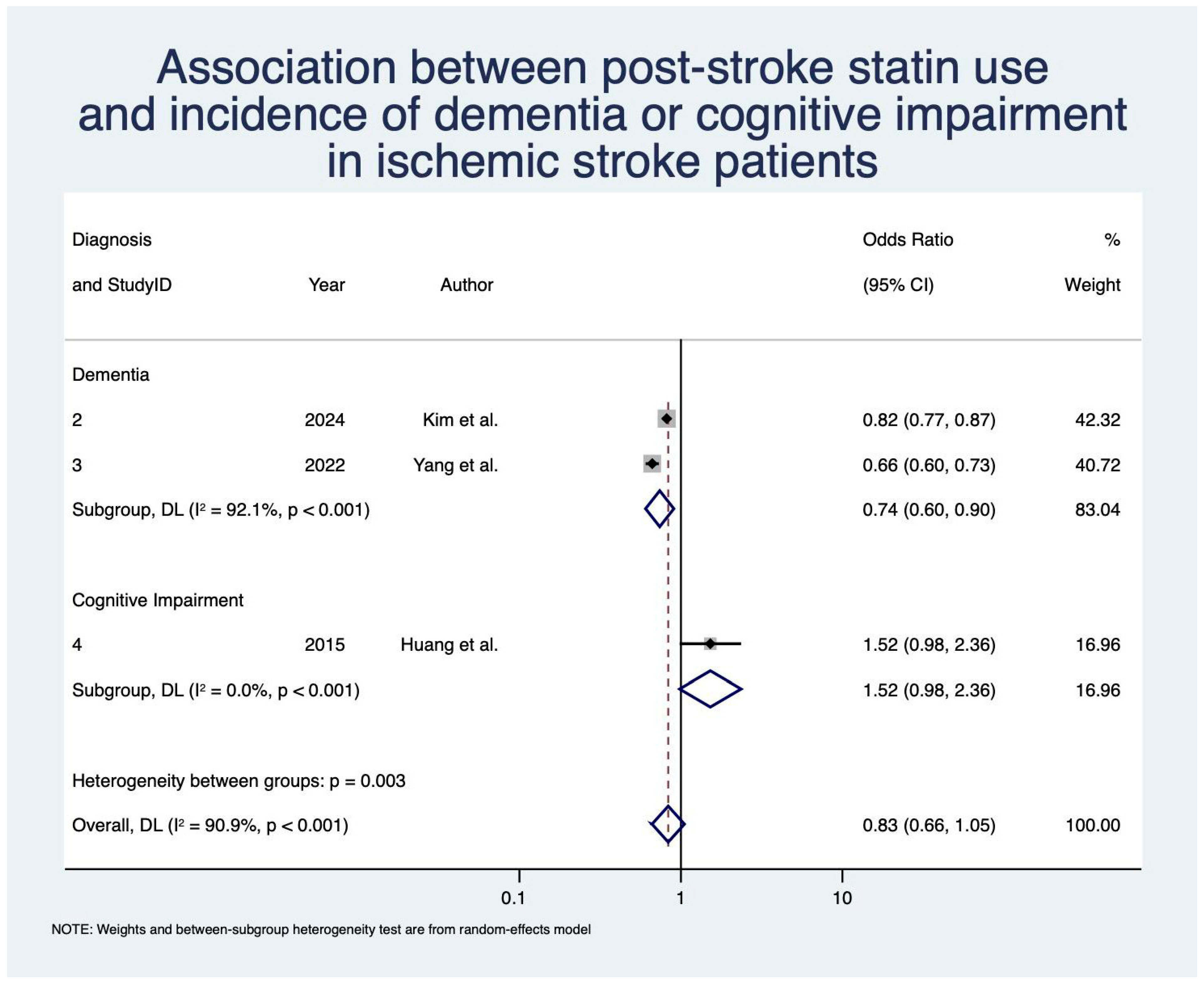
- Dementia/Cognitive Impairment
3.2.2. Impact of Variations in Statin Parameters on Clinical Outcomes
- Statin Timing
- Statin Type
- Statin Solubility
- Statin Intensity
3.3. Secondary Analysis
3.3.1. Impact of Post-Stroke Statin Use in Cardioembolic/Atrial Fibrillation-Related Strokes
Prevalence Estimations
- All-Cause Mortality
- Stroke Recurrence
Outcome Associations
- All-Cause Mortality
- Stroke Recurrence
3.3.2. Impact of Post-Stroke Statin Use in Ischemic Stroke Patients with Low Baseline LDL-Cholesterol Levels
- Prevalence Estimations
- Outcome Associations
3.3.3. Impact of Post-Stroke Statin Use on CRP Levels in Ischemic Stroke Patients
3.4. Bias & Sensitivity Analysis
4. Discussion
- Mechanistic Insights and Subgroup Effects
- Stroke Recurrence and Etiology-Specific Effects
- Cognitive Outcomes: Differentiating PSD and PSCI
- Optimizing Statin Therapy in Ischemic Stroke: Toward Precision Neurology
4.1. Strengths and Limitations
4.2. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Feigin, V.L.; Abate, M.D.; Abate, Y.H.; Abd ElHafeez, S.; Abd-Allah, F.; Abdelalim, A.; Abdelkader, A.; Abdelmasseh, M.; Abd-Elsalam, S.; Abdi, P.; et al. Global, regional, and national burden of stroke and its risk factors, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 2024, 23, 973–1003. [Google Scholar] [CrossRef]
- Craig, L.; Hoo, Z.L.; Yan, T.Z.; Wardlaw, J.; Quinn, T.J. Prevalence of dementia in ischaemic or mixed stroke populations: Systematic review and meta-analysis. J. Neurol. Neurosurg. Psychiatry 2022, 93, 180. [Google Scholar] [CrossRef]
- Skajaa, N.; Adelborg, K.; Horváth-Puhó, E.; Rothman, K.J.; Henderson, V.W.; Thygesen, L.C.; Sørensen, H.T. Risks of stroke recurrence and mortality after first and recurrent strokes in Denmark. Neurology 2022, 98, e329–e342. [Google Scholar] [CrossRef]
- Taylor, F.; Huffman, M.D.; Macedo, A.F.; Moore, T.H.M.; Burke, M.; Davey Smith, G.; Ward, K.; Ebrahim, S.; Gay, H.C. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2013, 1, CD004816. [Google Scholar] [CrossRef]
- German, C.A.; Liao, J.K. Understanding the molecular mechanisms of statin pleiotropic effects. Arch. Toxicol. 2023, 97, 1529–1545. [Google Scholar] [CrossRef]
- Amarenco, P.; Bogousslavsky, J.; Callahan, A.; Goldstein, L.B.; Hennerici, M.; Rudolph, A.E.; Sillesen, H.; Simunovic, L.; Szarek, M.; Welch, K.M.; et al. High-dose atorvastatin after stroke or transient ischemic attack. N. Engl. J. Med. 2006, 355, 549–559. [Google Scholar] [CrossRef]
- Bhatia, R.; Sharma, G.; Patel, C.; Garg, A.; Roy, A.; Bali, P.; Singh, N.; Sisodia, P.; Sreenivas, V.; Srivastava, M.V.P.; et al. Coronary artery disease in patients with ischemic stroke and TIA. J. Stroke Cerebrovasc. Dis. 2019, 28, 104400. [Google Scholar] [CrossRef] [PubMed]
- Escudero-Martínez, I.; Morales-Caba, L.; Segura, T. Atrial fibrillation and stroke: A review and new insights. Trends Cardiovasc. Med. 2023, 33, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Australian and New Zealand Living Clinical Guidelines for Stroke Management. Available online: https://informme.org.au/en/Guidelines/Clinical-Guidelines-for-Stroke-Management (accessed on 1 April 2025).
- Dawson, J.; Béjot, Y.; Christensen, L.M.; De Marchis, G.M.; Dichgans, M.; Hagberg, G.; Heldner, M.R.; Milionis, H.; Li, L.; Pezzella, F.R.; et al. European Stroke Organisation (ESO) guideline on pharmacological interventions for long-term secondary prevention after ischaemic stroke or transient ischaemic attack. Eur. Stroke J. 2022, 7, I–II. [Google Scholar] [CrossRef] [PubMed]
- Gladstone, D.J.; Lindsay, M.P.; Douketis, J.; Smith, E.E.; Dowlatshahi, D.; Wein, T.; Bourgoin, A.; Cox, J.; Falconer, J.B.; Graham, B.R.; et al. Canadian Stroke Best Practice Recommendations: Secondary prevention of stroke update 2020. Can. J. Neurol. Sci. 2022, 49, 315–337. [Google Scholar] [CrossRef]
- Kleindorfer, D.O.; Towfighi, A.; Chaturvedi, S.; Cockroft, K.M.; Gutierrez, J.; Lombardi-Hill, D.; Kamel, H.; Kernan, W.N.; Kittner, S.J.; Leira, E.C.; et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/American Stroke Association. Stroke 2021, 52, e364–e467. [Google Scholar] [CrossRef]
- Liu, L.; Li, Z.; Zhou, H.; Duan, W.; Huo, X.; Xu, W.; Li, S.; Nie, X.; Liu, H.; Liu, J.; et al. Chinese Stroke Association guidelines for clinical management of ischaemic cerebrovascular diseases: Executive summary and 2023 update. Stroke Vasc. Neurol. 2023, 8, e3. [Google Scholar] [CrossRef]
- Miyamoto, S.; Ogasawara, K.; Kuroda, S.; Itabashi, R.; Toyoda, K.; Itoh, Y.; Iguchi, Y.; Shiokawa, Y.; Takagi, Y.; Ohtsuki, T.; et al. Japan Stroke Society guideline 2021 for the treatment of stroke. Int. J. Stroke 2022, 17, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- Stroke and Transient Ischaemic Attack in over 16s: Diagnosis and Initial Management. Available online: https://www.ncbi.nlm.nih.gov/books/NBK542436/ (accessed on 1 April 2025).
- National Clinical Guideline for Stroke for the UK and Ireland. Available online: www.strokeguideline.org (accessed on 1 April 2025).
- Hong, K.S.; Lee, J.S. Statins in acute ischemic stroke: A systematic review. J. Stroke 2015, 17, 282–301. [Google Scholar] [CrossRef]
- Yin, Y.; Zhang, L.; Marshall, I.; Wolfe, C.; Wang, Y. Statin therapy for preventing recurrent stroke in patients with ischemic stroke: A systematic review and meta-analysis of randomized controlled trials and observational cohort studies. Neuroepidemiology 2022, 56, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Rost, N.S.; Brodtmann, A.; Pase, M.P.; van Veluw, S.J.; Biffi, A.; Duering, M.; Hinman, J.D.; Dichgans, M. Post-Stroke Cognitive Impairment and Dementia. Circ. Res. 2022, 130, 1252–1271. [Google Scholar] [CrossRef]
- Yang, Z.; Wang, H.; Edwards, D.; Ding, C.; Yan, L.; Brayne, C.; Mant, J. Association of blood lipids, atherosclerosis and statin use with dementia and cognitive impairment after stroke: A systematic review and meta-analysis. Ageing Res. Rev. 2020, 57, 100962. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- Climent, E.; Benaiges, D.; Pedro-Botet, J. Hydrophilic or lipophilic statins? Front. Cardiovasc. Med. 2021, 8, 687585. [Google Scholar] [CrossRef]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation 2019, 139, e1046–e1081. [Google Scholar] [CrossRef]
- Shen, H.; Killingsworth, M.C.; Bhaskar, S.M.M. Comprehensive meta-analysis of futile recanalization in acute ischemic stroke patients undergoing endovascular thrombectomy: Prevalence, factors, and clinical outcomes. Life 2023, 13, 1965. [Google Scholar] [CrossRef]
- Aivo, J.; Ruuskanen, J.O.; Tornio, A.; Rautava, P.; Kyto, V. Lack of statin therapy and outcomes after ischemic stroke: A population-based study. Stroke 2023, 54, 781–790. [Google Scholar] [CrossRef]
- Arevalo-Lorido, J.C.; Carretero-Gomez, J.; Fernandez-Recio, J.M.; Alvarez-Oliva, A.; Gutierrez-Montano, C.; Najarro-Diez, F.; Martin-Sanchez, M.J. Lowering C-reactive protein with statins after an ischemic stroke avoids mortality and readmissions. A prospective cohort study. Ann. Med. 2015, 47, 226–232. [Google Scholar] [CrossRef]
- Bach, F.; Skajaa, N.; Esen, B.O.; Fuglsang, C.H.; Horvath-Puho, E.; Sorensen, H.T.; Adelborg, K. High-intensity versus moderate-intensity statin treatment for patients with ischemic stroke: Nationwide cohort study. Eur. Stroke J. 2023, 8, 1041–1052. [Google Scholar] [CrossRef] [PubMed]
- Bao, J.J.; Zhang, Y.; Li, Y.B.; Guo, J.; He, L. Low-to-moderate dose statins improve the functional outcome of acute ischemic stroke with conventional medication treatment. Cardiovasc. Diagn. Ther. 2023, 13, 686. [Google Scholar] [CrossRef]
- Beer, C.; Blacker, D.; Bynevelt, M.; Hankey, G.J.; Puddey, I.B. A randomized placebo controlled trial of early treatment of acute ischemic stroke with atorvastatin and irbesartan. Int. J. Stroke 2012, 7, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Cao, G.-J.; Zhang, X.-F.; Zheng, K.-D. Effects of atorvastatin and rosuvastatin on blood lipids, platelet aggregation rate and inflammatory factors in patients with cerebral infarction. Afr. J. Online 2017, 16, 2507–2513. [Google Scholar] [CrossRef]
- Cappellari, M.; Bovi, P.; Moretto, G.; Zini, A.; Nencini, P.; Sessa, M.; Furlan, M.; Pezzini, A.; Orlandi, G.; Paciaroni, M.; et al. The THRombolysis and STatins (THRaST) study. Neurology 2013, 80, 655–661. [Google Scholar] [CrossRef]
- Chen, X.; Zhuang, X.; Peng, Z.; Yang, H.; Chen, L.; Yang, Q. Intensive statin therapy for acute ischemic stroke to reduce the number of microemboli: A preliminary, randomized controlled study. Eur. Neurol. 2018, 80, 163–170. [Google Scholar] [CrossRef]
- Choi, J.Y.; Seo, W.K.; Kang, S.H.; Jung, J.M.; Cho, K.H.; Yu, S.; Oh, K. Statins improve survival in patients with cardioembolic stroke. Stroke 2014, 45, 1849. [Google Scholar] [CrossRef]
- Choi, K.H.; Seo, W.K.; Park, M.S.; Kim, J.T.; Chung, J.W.; Bang, O.Y.; Kim, G.M.; Song, T.J.; Kim, B.J.; Heo, S.H.; et al. Effect of statin therapy on outcomes of patients with acute ischemic stroke and atrial fibrillation. J. Am. Heart Assoc. 2019, 8, e013941. [Google Scholar] [CrossRef]
- Choi, S.E.; Bucci, T.; Huang, J.Y.; Yiu, K.H.; Tsang, C.T.; Lau, K.K.; Hill, A.; Irving, G.; Lip, G.Y.H.; Abdul-Rahim, A.H. Early statin use is associated with improved survival and cardiovascular outcomes in patients with atrial fibrillation and recent ischaemic stroke: A propensity-matched analysis of a global federated health database. Eur. Stroke J. 2024, 10, 116–127. [Google Scholar] [CrossRef]
- Ni Chróinín, D.; Callaly, E.L.; Duggan, J.; Merwick, A.; Hannon, N.; Sheehan, O.; Marnane, M.; Horgan, G.; Williams, E.B.; Harris, D.; et al. Association between acute statin therapy, survival, and improved functional outcome after ischemic stroke The North Dublin Population Stroke Study. Stroke 2011, 42, 1021–1029. [Google Scholar] [CrossRef] [PubMed]
- Cui, C.; Dong, S.; Liu, Q.; Bao, J.; Gao, L.; Li, Y.; He, L. Low-dose statins improve prognosis of patients with ischaemic stroke undergoing intra-arterial thrombectomy: A prospective cohort study. J. Clin. Neurosci. 2022, 103, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Cui, C.; Li, Y.; Bao, J.; Dong, S.; Gao, L.; He, L. Low dose statins improve prognosis of ischemic stroke patients with intravenous thrombolysis. BMC Neurol. 2021, 21, 220. [Google Scholar] [CrossRef]
- Flach, C.; Elstad, M.; Muruet, W.; Wolfe, C.D.A.; Rudd, A.G.; Douiri, A. The impact of pre- and post-stroke statin use on stroke severity and long-term outcomes: A population-based cohort study. Cerebrovasc. Dis. 2019, 47, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Flint, A.C.; Kamel, H.; Navi, B.B.; Rao, V.A.; Faigeles, B.S.; Conell, C.; Klingman, J.G.; Sidney, S.; Hills, N.K.; Sorel, M.; et al. Statin use during ischemic stroke hospitalization is strongly associated with improved poststroke survival. Stroke 2012, 43, 147–154. [Google Scholar] [CrossRef]
- Furlan, N.E.; de Souza, J.T.; Bazan, S.G.Z.; Franco, R.J.D.; Luvizutto, G.J.; Gut, A.L.; Modolo, G.P.; Winckler, F.C.; Martin, L.C.; Bazan, R. Association between statin use and mortality risks during the acute phase of ischemic stroke in patients admitted to an intensive care unit. Arq. Neuro-Psiquiatr. 2020, 78, 158–162. [Google Scholar] [CrossRef]
- Gong, C.; Liu, C.; Wang, Y.; Chen, L.; Yuan, J.; Zhang, J.; Xiaoming, L.; Chen, Y.; Huang, L.; Xu, T.; et al. Effect of statin treatment on clinical outcomes in cardioembolic stroke with endovascular thrombectomy. J. Neurointerv. Surg. 2024, 16, 947–954. [Google Scholar] [CrossRef]
- Han, J.; Choi, Y.K.; Leung, W.K.; Hui, M.T.; Leung, M.K.W. Long term clinical outcomes of patients with ischemic stroke in primary care—A 9-year retrospective study. BMC Fam. Pract. 2021, 22, 164. [Google Scholar] [CrossRef]
- Hjalmarsson, C.; Bokemark, L.; Manhem, K.; Mehlig, K.; Andersson, B. The effect of statins on acute and long-term outcome after ischemic stroke in the elderly. Am. J. Geriatr. Pharmacother. 2012, 10, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Jia, W.H.; Zhou, L.C. Effect of 20 mg/day atorvastatin: Recurrent stroke survey in chinese ischemic stroke patients with prior intracranial hemorrhage. J. Clin. Neurol. 2013, 9, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Kim, N.; Park, T.H.; Bang, O.Y.; Lee, J.S.; Lee, J.; Han, M.K.; Park, S.H.; Gorelick, P.B.; Bae, H.J. Early statin use in ischemic stroke patients treated with recanalization therapy: Retrospective observational study. BMC Neurol. 2015, 15, 122. [Google Scholar] [CrossRef]
- Kim, J.T.; Lee, J.S.; Kim, B.J.; Kang, J.; Lee, K.J.; Park, J.M.; Kang, K.; Lee, S.J.; Kim, J.G.; Cha, J.K.; et al. Statin treatment in patients with stroke with low-density lipoprotein cholesterol levels below 70 mg/dL. J. Am. Heart Assoc. 2023, 12, e030738. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.T.; Lee, J.S.; Kim, H.; Kim, B.J.; Kang, J.H.; Lee, K.J.; Park, J.M.; Kang, K.Y.S.; Lee, S.J.; Kim, J.G.; et al. Comparative effectiveness of rosuvastatin versus atorvastatin in acute ischemic stroke treatment. J. Am. Heart Assoc. 2025, 14, e038080. [Google Scholar] [CrossRef]
- Kim, T.J.; Lee, J.S.; Oh, M.S.; Park, S.H.; Lee, K.B.; Kyung-Ho, Y.; Lee, B.C.; Yoon, B.W.; Ko, S.B. Risk of long-term post-stroke dementia using a linked dataset of patients with ischemic stroke without a history of dementia. Int. J. Stroke 2024, 20, 601–610. [Google Scholar] [CrossRef]
- Kytö, V.; Åivo, J.; Ruuskanen, J.O. Intensity of statin therapy after ischaemic stroke and long-term outcomes: A nationwide cohort study. Stroke Vasc. Neurol. 2025, 10, 142–145. [Google Scholar] [CrossRef]
- Lee, K.P.; Huang, H.C.; Tsai, J.Y.; Hsu, L.C. Statin treatment in stroke patient with low-density lipoprotein cholesterol levels below 70 mg/dL. J. Stroke Cerebrovasc. Dis. 2024, 33, 107645. [Google Scholar] [CrossRef]
- Lin, H.C.; Tsai, W.C.; Lin, J.R.; Chang, W.N.; Huang, C.C.; Wang, H.C.; Kung, C.T.; Su, C.M.; Su, Y.J.; Lin, W.C.; et al. Adjunctive statin therapy reduces intracranial hemorrhage and 1-year mortality in patients with atrial fibrillation after acute ischemic stroke: A population-based epidemiological study from Taiwan. J. Clin. Neurosci. 2019, 69, 224–229. [Google Scholar] [CrossRef]
- Makihara, N.; Kamouchi, M.; Hata, J.; Matsuo, R.; Ago, T.; Kuroda, J.; Kuwashiro, T.; Sugimori, H.; Kitazono, T. Statins and the risks of stroke recurrence and death after ischemic stroke: The Fukuoka Stroke Registry. Atherosclerosis 2013, 231, 211–215. [Google Scholar] [CrossRef]
- Marvardi, M.; Paciaroni, M.; Caso, V. Statin therapy in ischemic stroke patients with atrial fibrillation: Efficacy and safety outcomes. Eur. Stroke J. 2025, 10, 775–783. [Google Scholar] [CrossRef]
- Milionis, H.J.; Giannopoulos, S.; Kosmidou, M.; Panoulas, V.; Manios, E.; Kyritsis, A.P.; Elisaf, M.S.; Vemmos, K. Statin therapy after first stroke reduces 10-year stroke recurrence and improves survival. Neurology 2009, 72, 1816–1822. [Google Scholar] [CrossRef]
- Montaner, J.; Bustamante, A.; Garcia-Matas, S.; Martinez-Zabaleta, M.; Jimenez, C.; De La Torre, J.; Rubio, F.R.; Segura, T.; Masjuan, J.; Canovas, D.; et al. Combination of thrombolysis and statins in acute stroke is safe: Results of the STARS randomized trial (Stroke Treatment with Acute Reperfusion and Simvastatin). Stroke 2016, 47, 2870–2873. [Google Scholar] [CrossRef]
- Muscari, A.; Puddu, G.M.; Santoro, N.; Serafini, C.; Cenni, A.; Rossi, V.; Zoli, M. The atorvastatin during ischemic stroke study: A pilot randomized controlled trial. Clin. Neuropharmacol. 2011, 34, 141–147. [Google Scholar] [CrossRef]
- Ntaios, G.; Papavasileiou, V.; Makaritsis, K.; Milionis, H.; Manios, E.; Michel, P.; Lip, G.Y.; Vemmos, K. Statin treatment is associated with improved prognosis in patients with AF-related stroke. Int. J. Cardiol. 2014, 177, 129–133. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, E.C.; Greiner, M.A.; Xian, Y.; Fonarow, G.C.; Olson, D.M.; Schwamm, L.H.; Bhatt, D.L.; Smith, E.E.; Maisch, L.; Hannah, D.; et al. Clinical effectiveness of statin therapy after ischemic stroke: Primary results from the statin therapeutic area of the Patient-Centered Research Into Outcomes Stroke Patients Prefer and Effectiveness Research (PROSPER) Study. Circulation 2015, 132, 1404–1413. [Google Scholar] [CrossRef]
- Park, H.K.; Lee, J.S.; Hong, K.S.; Cho, Y.J.; Park, J.M.; Kang, K.; Lee, S.J.; Kim, J.G.; Cha, J.K.; Kim, D.H.; et al. Statin therapy in acute cardioembolic stroke with no guidance-based indication. Neurology 2020, 94, e1984–e1995. [Google Scholar] [CrossRef]
- Sakurai, K.; Ishaya, K.; Takaishi, S.; Kato, B.; Shimizu, K.; Shimomura, K.; Tokuyama, Y.; Hasegawa, Y. Effects of early statin treatment on inflammatory biomarkers and clinical deterioration in patients with acute ischemic stroke. Clin. Neurol. 2011, 51, 6–13. [Google Scholar] [CrossRef]
- Scheitz, J.F.; Endres, M.; Heuschmann, P.U.; Audebert, H.J.; Nolte, C.H. Reduced risk of poststroke pneumonia in thrombolyzed stroke patients with continued statin treatment. Int. J. Stroke 2015, 10, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Song, B.; Wang, Y.; Zhao, X.; Liu, L.; Wang, C.; Wang, A.; Du, W.; Wang, Y.; Xu, Y. Inpatient statin use Is associated with decreased mortality of acute stroke patients with very low low-density lipoprotein cholesterol. J. Stroke Cerebrovasc. Dis. 2015, 24, 2369–2374. [Google Scholar] [CrossRef]
- Song, B.; Wang, Y.L.; Zhao, X.Q.; Liu, L.P.; Wang, C.X.; Wang, A.X.; Du, W.L.; Wang, Y.J. Association between statin use and short-term outcome based on severity of ischemic stroke: A cohort study. PLoS ONE 2014, 9, e84389. [Google Scholar] [CrossRef]
- Ueno, Y.; Yamashiro, K.; Tanaka, Y.; Watanabe, M.; Miyamoto, N.; Shimada, Y.; Kuroki, T.; Tanaka, R.; Miyauchi, K.; Daida, H.; et al. Rosuvastatin may stabilize atherosclerotic aortic plaque: Transesophageal echocardiographic study in the EPISTEME trial. Atherosclerosis 2015, 239, 476–482. [Google Scholar] [CrossRef]
- Vitturi, B.K.; Gagliardi, R.J. The role of statins in cardioembolic stroke. J. Clin. Neurosci. 2019, 72, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Vitturi, B.K.; Gagliardi, R.J. The influence of statin withdrawal and adherence on stroke outcomes. Neurol. Sci. 2020, 42, 2317–2323. [Google Scholar] [CrossRef]
- Winardi, W.; Moi, S.H.; Winardi, T.; Cheng, Y.W.; Chen, P.Y.; Lin, C.K. Nationwide big data analysis of statin use and intracerebral hemorrhage risk in acute ischemic stroke patients in Taiwan. Medicina 2024, 60, 939. [Google Scholar] [CrossRef]
- Wu, Y.L.; Saver, J.L.; Chen, P.C.; Lee, J.D.; Wang, H.H.; Rao, N.M.; Lee, M.; Ovbiagele, B. Effect of statin use on clinical outcomes in ischemic stroke patients with atrial fibrillation. Medicine 2017, 96, e5918. [Google Scholar] [CrossRef]
- Yakusevich, V.V.; Malygin, A.Y.; Lychenko, S.V.; Petrochenko, A.S.; Kabanov, A.V. The efficacy of high-dose simvastatin in acute period of ischemic stroke. Ration. Pharmacother. Cardiol. 2012, 8, 4–16. [Google Scholar] [CrossRef]
- Yang, W.Y.; Li, Y.F.; Wang, Z.R.; Yu, T.X.; Xu, D.J.; Yang, N.; Niu, X.Y.; Cai, X.L.; Zhuo, W.Y.; Wu, X.M.; et al. Combined therapy of intensive statin plus intravenous rt-PA in acute ischemic stroke: The INSPIRE randomized clinical trial. J. Neurol. 2021, 268, 2560–2569. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Toh, S.; Li, X.; Edwards, D.; Brayne, C.; Mant, J. Statin use is associated with lower risk of dementia in stroke patients: A community-based cohort study with inverse probability weighted marginal structural model analysis. Eur. J. Epidemiol. 2022, 37, 615–627. [Google Scholar] [CrossRef]
- Zare, M.; Saadatnia, M.; Mousavi, S.A.; Keyhanian, K.; Davoudi, V.; Khanmohammadi, E. The effect of statin therapy in stroke outcome: A double blind clinical trial. Int. J. Prev. Med. 2012, 3, 68–72. [Google Scholar]
- Zhang, Z.; Yao, X.; Wang, M.; Huang, Y.; Shen, T.; Zhang, W.; Liu, Y. Therapeutic effects of aspirin combined with atorvastatin on ischemic strokes. Int. J. Clin. Exp. Med. 2018, 11, 11104–11111. [Google Scholar]
- Huang, Y.; Yang, S.; Jia, J. Factors related to long-term post-stroke cognitive impairment in young adult ischemic stroke. Med. Sci. Monit. 2015, 21, 654–660. [Google Scholar] [CrossRef]
- Eun, M.; Jung, J.; Choi, K.; Seo, W. Statin effects in atrial fibrillation-related stroke: A systematic review and meta-analysis. Front. Neurol. 2020, 11, 589684. [Google Scholar] [CrossRef]
- Xu, T.; Wang, Y.; Yuan, J.; Chen, Y. The effect of statin treatment on outcomes of cardioembolic stroke: A systematic review and meta-analysis of real-world Studies. CNS Drugs 2021, 35, 717–726. [Google Scholar] [CrossRef]
- Patel, J.; Bhaskar, S.M.M. Diagnosis and Management of Atrial Fibrillation in Acute Ischemic Stroke in the Setting of Reperfusion Therapy: Insights and Strategies for Optimized Care. J. Cardiovasc. Dev. Dis. 2023, 10, 458. [Google Scholar] [CrossRef]
- Guasti, L.; Lupi, A. Lipidology Update: Targets and Timing of Well-Established Therapies. Available online: https://www.escardio.org/Councils/Council-for-Cardiology-Practice-(CCP)/Cardiopractice/lipidology-update-targets-and-timing-of-well-established-therapies (accessed on 1 April 2025).
- Rajesh, K.; Spring, K.J.; Smokovski, I.; Upmanyue, V.; Mehndiratta, M.M.; Strippoli, G.F.M.; Beran, R.G.; Bhaskar, S.M.M. The impact of chronic kidney disease on prognosis in acute stroke: Unraveling the pathophysiology and clinical complexity for optimal management. Clin. Exp. Nephrol. 2025, 29, 149–172. [Google Scholar] [CrossRef]
- Singh, R.J.; Chen, S.; Ganesh, A.; Hill, M.D. Long-term neurological, vascular, and mortality outcomes after stroke. Int. J. Stroke 2018, 13, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Kolmos, M.; Christoffersen, L.; Kruuse, C. Recurrent ischemic stroke—A systematic review and meta-analysis. J. Stroke Cerebrovasc. Dis. 2021, 30, 105935. [Google Scholar] [CrossRef] [PubMed]
- Herder, M.; Arntzen, K.A.; Johnsen, S.H.; Eggen, A.E.; Mathiesen, E.B. Long-term use of lipid-lowering drugs slows progression of carotid atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 858–862. [Google Scholar] [CrossRef] [PubMed]
- Oesterle, A.; Laufs, U.; Liao, J.K. Pleiotropic effects of statins on the cardiovascular system. Circ. Res. 2017, 120, 229–243. [Google Scholar] [CrossRef]
- Stephan, B.C.M.; Hunter, S.; Harris, D.; Llewellyn, D.J.; Siervo, M.; Matthews, F.E.; Brayne, C. The neuropathological profile of mild cognitive impairment (MCI): A systematic review. Mol. Psychiatry 2012, 17, 1056–1076. [Google Scholar] [CrossRef]
- Doyle, K.P.; Buckwalter, M.S. Immunological mechanisms in poststroke dementia. Curr. Opin. Neurol. 2020, 33, 30–36. [Google Scholar] [CrossRef]
- Du, S.; Wang, X.; Xiao, L.; Tu, J.; Zhu, W.; He, T.; Liu, C. Molecular mechanisms of vascular dementia: What can be learned from animal models of chronic cerebral hypoperfusion? Mol. Neurobiol. 2017, 54, 3670–3682. [Google Scholar] [CrossRef]
- Moskowitz, M.A.; Lo, E.H.; Iadecola, C. The science of stroke: Mechanisms in search of treatments. Neuron 2010, 67, 181–198. [Google Scholar] [CrossRef] [PubMed]
- Rajab, H.A.; Al-Kuraishy, H.M.; Shokr, M.M.; Al-Gareeb, A.I.; Al-Harchan, N.A.; Alruwaili, M.; Papadakis, M.; Alexiou, A.; Batiha, G.E. Statins for vascular dementia: A hype or hope. Neuroscience 2025, 567, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Arboix, A.; García-Eroles, L.; Oliveres, M.; Targa, C.; Balcells, M.; Massons, J. Pretreatment with statins improves early outcome in patients with first-ever ischaemic stroke: A pleiotropic effect of statins or a beneficial effect of hypercholesterolemia? BMC Neurol. 2010, 10, 47. [Google Scholar] [CrossRef]
- Azizi, E.; Prabhakaran, S.; Brorson, J.R. Statin initiation and early stroke recurrence in the Platelet-Oriented Inhibition in New TIA and Minor Ischemic Stroke Trial (POINT) trial population. J. Stroke Cerebrovasc. Dis. 2025, 34, 108349. [Google Scholar] [CrossRef]
- Gao, Y.; Jiang, L.; Pan, Y.; Chen, W.; Jing, J.; Wang, C.; Johnston, S.C.; Amarenco, P.; Bath, P.M.; Yang, Y.; et al. Immediate- or delayed-intensive statin in acute cerebral ischemia: The INSPIRES randomized clinical trial. JAMA Neurol. 2024, 81, 741–751. [Google Scholar] [CrossRef] [PubMed]
- Costa, F.M.; Lobo, K.; Lalor Tavares, J.L.; da Silva Gomes, R.P.; Santos, L.; Oliveira, R.C.S. Intensive versus non-intensive statin therapy in patients with ischemic stroke: A systematic review and meta-analysis. J. Clin. Neurosci. 2025, 138, 111361. [Google Scholar] [CrossRef]
- Lee, M.; Cheng, C.; Wu, Y.; Lee, J.; Hsu, C.; Ovbiagele, B. Association between intensity of low-density lipoprotein cholesterol reduction with statin-based therapies and secondary stroke prevention: A meta-analysis of randomized clinical trials. JAMA Neurol. 2022, 79, 349–358. [Google Scholar] [CrossRef]
- Fong, C.W. Statins in therapy: Understanding their hydrophilicity, lipophilicity, binding to 3-hydroxy-3-methylglutaryl-CoA reductase, ability to cross the blood brain barrier and metabolic stability based on electrostatic molecular orbital studies. Eur. J. Med. Chem. 2014, 85, 661–674. [Google Scholar] [CrossRef]
- Chrispin, J.; Martin, S.S.; Hasan, R.K.; Joshi, P.H.; Minder, C.M.; McEvoy, J.W.; Kohli, P.; Johnson, A.E.; Wang, L.; Blaha, M.J.; et al. Landmark lipid-lowering trials in the primary prevention of cardiovascular disease. Clin. Cardiol. 2013, 36, 516–523. [Google Scholar] [CrossRef]
- Nissen, S.E.; Tuzcu, E.M.; Schoenhagen, P.; Brown, B.G.; Ganz, P.; Vogel, R.A.; Crowe, T.; Howard, G.; Cooper, C.J.; Brodie, B.; et al. Effect of Intensive Compared with Moderate Lipid-Lowering Therapy on Progression of Coronary AtherosclerosisA Randomized Controlled Trial. JAMA 2004, 291, 1071–1080. [Google Scholar] [CrossRef]
- McPherson, R.; Adreak, N.; Sharma, A. Medications for Lipid Control: Statins vs Newer Drugs. Can. J. Cardiol. 2024, 40, S26–S34. [Google Scholar] [CrossRef]
- Temporelli, P.L.; Arca, M.; D’Erasmo, L.; De Caterina, R. Lipid-Lowering Therapy in Patients with Coronary Heart Disease and Prior Stroke: Mission Impossible? J. Clin. Med. 2021, 10, 886. [Google Scholar] [CrossRef]
- Sierra, S.; Ramos, M.C.; Molina, P.; Esteo, C.; Vázquez, J.A.; Burgos, J.S. Statins as neuroprotectants: A comparative in vitro study of lipophilicity, blood-brain-barrier penetration, lowering of brain cholesterol, and decrease of neuron cell death. J. Alzheimers Dis. 2011, 23, 307–318. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.-C.; Lei, S.-Y.; Zhang, D.-H.; He, Q.-Y.; Sun, Y.-Y.; Zhu, H.-J.; Qu, Y.; Zhou, S.-Y.; Yang, Y.; Li, C.; et al. The pleiotropic effects of statins: A comprehensive exploration of neurovascular unit modulation and blood–brain barrier protection. Mol. Med. 2024, 30, 256. [Google Scholar] [CrossRef] [PubMed]
- Oesterle, A.; Liao, J.K. The Pleiotropic Effects of Statins—From Coronary Artery Disease and Stroke to Atrial Fibrillation and Ventricular Tachyarrhythmia. Curr. Vasc. Pharmacol. 2019, 17, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Fracassi, A.; Marangoni, M.; Rosso, P.; Pallottini, V.; Fioramonti, M.; Siteni, S.; Segatto, M. Statins and the Brain: More than Lipid Lowering Agents? Curr. Neuropharmacol. 2019, 17, 59–83. [Google Scholar] [CrossRef]
- Luvai, A.; Mbagaya, W.; Hall, A.S.; Barth, J.H. Rosuvastatin: A review of the pharmacology and clinical effectiveness in cardiovascular disease. Clin. Med. Insights Cardiol. 2012, 6, 17–33. [Google Scholar] [CrossRef]
- Reiner, Ž. Resistance and intolerance to statins. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 1057–1066. [Google Scholar] [CrossRef]
- Gupta, M.; Smokovski, I.; Chatzis, D.G.; Spring, K.J.; Mehndiratta, M.M.; Beran, R.G.; Bhaskar, S.M.M. Statins in acute ischemic stroke: Mechanisms, resistance, and precision strategies for neurovascular and cognitive protection. CNS Drugs 2025, 39, 1083–1107. [Google Scholar] [CrossRef]
- Liao, J.K. Safety and efficacy of statins in Asians. Am. J. Cardiol. 2007, 99, 410–414. [Google Scholar] [CrossRef]
- Link, E.; Parish, S.; Armitage, J.; Bowman, L.; Heath, S.; Matsuda, F.; Gut, I.; Lathrop, M.; Collins, R. SLCO1B1 variants and statin-induced myopathy—A genomewide study. N. Engl. J. Med. 2008, 359, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Chen, Y.; Wei, B.; Li, H.; Peng, Y.; Luo, Z. Impacts of ABCG2 loss of function variant (p. Gln141Lys, c.421 C > A, rs2231142) on lipid levels and statin efficiency: A systematic review and meta-analysis. BMC Cardiovasc. Disord. 2024, 24, 202. [Google Scholar] [CrossRef] [PubMed]
- Biswas, R.; Wijeratne, T.; Zelenak, K.; Huasen, B.B.; Iacobucci, M.; Killingsworth, M.C.; Beran, R.G.; Gebreyohanns, M.; Sekhar, A.; Khurana, D.; et al. Disparities in Access to Reperfusion Therapy for Acute Ischemic Stroke (DARTS): A comprehensive meta-analysis of ethnicity, socioeconomic status, and geographical factors. CNS Drugs 2025, 39, 417–442. [Google Scholar] [CrossRef]
- Venketasubramanian, N. Stroke demographics, risk factors, subtypes, syndromes, mechanisms and inter-ethnic differences between Chinese, Malays and Indians in Singapore—A hospital-based study. J. Cardiovasc. Dev. Dis. 2024, 11, 180. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.; Bhaskar, S. Unifying Vascular Injury and Neurodegeneration: A Mechanistic Continuum in Cerebral Small Vessel Disease and Dementia. Eur. J. Neurosci. 2025, 62, e70246. [Google Scholar] [CrossRef]
| Study ID | Author | Year | Country | Study Design | Study Cohort | Control | Intervention | Cohort Size n (%) | Male n (%) | Age Mean (SD) | NIHSS Score Mean (SD) | TOAST n (%) | Outcomes Reported | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LAA | CE | SVO | Other | Undetermined | ||||||||||||||||||||||||||
| Overall | C ^ | I ^ | Overall ^ | C * | I + | Overall | C | I | Overall | C | I | C * | I + | C * | I + | C * | I + | C * | I + | C * | I + | |||||||||
| All IS Subtypes | ||||||||||||||||||||||||||||||
| 1 | Yakusevich et al. [70] | 2012 | Russia | RCT | First acute cerebrovascular incident | Standard IS therapy | Simvastatin 40 mg + Standard IS therapy | 183 (100) | 97 (53.0) | 86 (47.0) | 80 (44) | 43 (44) | 37 (43) | 65.7 (8.3) | 65.8 (9.3) | 65.6 (7.2) | NR | 9.2 (3.7) | 8.9 (4.0) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| 2 | Kim et al. [49] | 2024 | South Korea | Retrospective | IS | No statin | Discharge statin | 37,553 (100) | 8764 (23.3) | 28,789 (76.7) | 23,237 (61.9) | NR | NR | 64.9 (12.4) | NR | NR | 3.0 (3.0) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | PSD |
| 3 | Yang et al. [72] | 2022 | United Kingdom | Retrospective | IS | No statin | Statin | 30,113 (100) | 12,207 (40.5) | 17,906 (59.5) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | PSD |
| 4 | Huang et al. [75] | 2015 | China | Retrospective | First-ever IS | No statin | Statin | 350 (100) | 214 (61.1) | 136 (38.9) | 244 (69.7) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | PSCI |
| 5 | Beer et al. [29] | 2012 | Australia | RCT | Acute IS | Placebo | Atorvastatin 80 mg | 40 (100) | 23 (57.5) | 17 (42.5) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | CRP Levels |
| 6 | Muscari et al. [57] | 2011 | Italy | RCT | IS | Placebo | Atorvastatin 80 mg | 62 (100) | 31 (50.0) | 31 (50.0) | 20 (32.2) | 12 (38.7) | 8 (25.8) | 75.3 (11.9) | 75.6 (12.2) | 74.9 (11.8) | NR | 13.7 (10.1) | 13.7 (10.9) | 6 (19.4) | 6 (19.4) | 10 (32.3) | 10 (32.3) | 6 (19.4) | 5 (16.1) | 1 (3.2) | 0 (0) | 7 (22.6) | 10 (32.2) | CRP Levels |
| 7 | Zare et al. [73] | 2012 | Iran | RCT | Acute moderate stroke in MCA | No statin | Lovastatin 20 mg | 55 (100) | 30 (54.5) | 25 (45.5) | 29 (52.7) | 16 (53.3) | 13 (52.0) | NR | 68.3 (10.7) | 63.3 (10.8) | NR | 14.5 (4.3) | 16.0 (4.3) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality |
| 8 | Aivo et al. [25] | 2023 | Finland | Retrospective | IS | No statin | Statin | 59,588 (100) | 16,171 (27.1) | 43,417 (72.9) | 32,604 (54.5) | 8377 (51.2) | 24,227 (55.8) | NR | 71.7 (14.4) | 70.1 (11.4) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| 9 | Flach et al. [39] | 2019 | England | Prospective | IS | No statin | Statin | 3061 (100) | 2108 (68.9) | 953 (31.1) | 1536 (50.2) | 1026 (48.7) | 510 (53.5) | NR | NR | NR | NR | NR | NR | 93 (4.4) | 116 (12.2) | 321 (15.2) | 170 (17.8) | 235 (11.1) | 289 (30.3) | 38 (1.8) | 24 (2.5) | 364 (17.3) | 266 (27.9) | Mortality, Stroke Recurrence |
| 10 | Han et al. [43] | 2021 | China | Retrospective | Non-acute IS | No statin | Statin | 466 (100) | 279 (59.9) | 187 (40.1) | NR | NR | NR | 71.5 (11.2) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Stroke Recurrence |
| 11 | Makihara et al. [53] | 2013 | Japan | Prospective | First ever acute IS | No statin | Statin | 2822 (100) | 1829 (64.8) | 993 (35.2) | 1677 (59.4) | 1137 (62.2) | 540 (54.4) | NR | 71.2 (13.5) | 70.0 (10.9) | NR | 4.0 (3.7) | 3.0 (3.0) | 316 (17.3) | 239 (24.1) | 475 (26.0) | 139 (14.0) | 452 (24.7) | 260 (26.2) | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| 12 | Milionis et al. [55] | 2009 | Greece | Retrospective | First ever acute IS | No statin | Statin | 794 (100) | 596 (75.1) | 198 (24.9) | 543 (68.4) | 404 (67.8) | 139 (70.2) | NR | 68.8 (11.1) | 67.0 (10.3) | NR | NR | NR | 177 (29.7) | 62 (31.3) | 146 (24.5) | 49 (24.7) | 166 (27.9) | 53 (26.8) | NR | NR | 107 (18.0) | 34 (17.2) | Stroke Recurrence |
| 13 | O’Brien et al. [59] | 2015 | United States | Retrospective | IS | No statin | Statin | 77,468 (100) | 22,477 (29.0) | 54,991 (71.0) | 31,252 (40.3) | 8541 (38.0) | 22,711 (41.3) | NR | 81.2 (8.3) | 78.6 (8.2) | NR | 6.0 (6.7) | 5.0 (5.2) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| 14 | Zhang et al. [74] | 2018 | China | RCT | IS | Aspirin | Aspirin + Statin | 127 (100) | 61 (48.0) | 66 (52.0) | 83 (65.4) | 40 (65.6) | 43 (65.2) | NR | 65.9 (1.8) | 64.6 (1.2) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Stroke Recurrence, CRP Levels |
| 15 | Jia & Zhou [45] | 2013 | China | Retrospective | IS with prior ICH | No statin | Atorvastatin 20 mg | 354 (100) | 193 (54.5) | 161 (45.5) | 212 (59.9) | 117 (60.6) | 95 (59.0) | NR | 62.4 (12.8) | 64.3 (12.0) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| 16 | Arevalo-Lorido et al. [26] | 2014 | Germany | Prospective | IS | No statin | Statin | 313 (100) | 108 (34.5) | 205 (65.5) | 150 (47.9) | 34 (31.5) | 116 (56.6) | NR | 77.5 (8.9) | NR | NR | 7.9 (5.1) | NR | 39 (36.1) | 59 (28.8) | 29 (26.9) | 44 (21.5) | 34 (31.5) | 84 (41.0) | 3 (2.8) | 5 (2.4) | 3 (2.8) | 13 (6.3) | Mortality, CRP levels |
| 17 | Bao et al. [28] | 2023 | China | Retrospective | Acute IS | No statin | Low-to-moderate and high-dose statin | 327 (100) | 48 (14.7) | 279 (85.3) | 181 (55.4) | 25 (52.1) | 156 (55.9) | 70.0 (14.2) | 66.0 (17.8) | NR | 9.7 (8.9) | 16.7 (7.6) | NR | 12 (25.0) | 100 (35.8) | 26 (54.2) | 117 (41.9) | 0 (0.0) | 26 (9.3) | 2 (4.2) | 8 (2.9) | 8 (16.7) | 28 (10.0) | Mortality |
| 18 | Ni Chroinin et al. [36] | 2011 | Ireland | Prospective | New IS | No statin | Statin | 301 (100) | 112 (37.2) | 189 (62.8) | 153 (50.1) | 52 (46.4) | 101 (53.4) | NR | 73.4 (15.6) | 69.9 (13.1) | NR | NR | NR | 1 (0.9) | 23 (12.2) | 51 (45.5) | 56 (29.6) | 12 (10.7) | 33 (17.5) | 4 (3.6) | 4 (2.1) | 44 (39.3) | 72 (38.1) | Mortality |
| 19 | Montaner et al. [56] | 2016 | Spain | RCT | IS | Placebo | Simvastatin 40 mg | 104 (100) | 54 (51.9) | 50 (48.1) | 56 (53.8) | 32 (59.3) | 24 (48.0) | 72.8 (14.7) | 71.3 (19.0) | 73.2 (13.7) | 8.2 (4.1) | 8.0 (5.3) | 8.0 (3.8) | 8 (14.8) | 2 (4.0) | 24 (44.4) | 17 (34.0) | 4 (7.4) | 5 (10.0) | 1 (1.9) | 0 (0.0) | 15 (2.8) | 25 (50.0) | Mortality, Stroke Recurrence |
| 20 | Cappellari et al. [31] | 2013 | Italy | Retrospective | Acute IS with IVT | No statin | Statin | 2072 (100) | 1233 (59.5) | 839 (40.5) | 1210 (58.4) | 705 (57.2) | 505 (60.2) | 66.6 (12.5) | 66.1 (13.7) | 67.3 (10.6) | 12.6 (6.0) | 13.3 (6.1) | 11.7 (5.9) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality |
| 21 | Cui et al. [37] | 2022 | China | Prospective | Acute IS with EVT | No statin | Low-dose statin | 256 (100) | 73 (28.5) | 183 (71.5) | 139 (54.3) | 39 (53.4) | 100 (54.6) | NR | 67.4 (13.1) | 67.1 (13.7) | NR | 16.0 (6.1) | 15.0 (6.0) | 38 (52.1) | 104 (56.8) | 34 (46.6) | 76 (41.5) | NR | NR | NR | NR | NR | NR | Mortality |
| 22 | Cui et al. [38] | 2021 | China | Prospective | Acute IS with IVT | No statin | Low-dose statin | 215 (100) | 35 (16.3) | 180 (83.7) | 102 (47.4) | 17 (48.9) | 85 (47.2) | NR | 72.2 (14.5) | 70.7 (12.1) | NR | 14.0 (7.0) | 8.7 (7.5) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality |
| 23 | Scheitz et al. [62] | 2015 | Germany | Retrospective | Acute IS with IVT | No statin | Statin | 481 (100) | 398 (82.7) | 83 (17.3) | 241 (50.1) | 198 (49.7) | 43 (51.8) | NR | 74.3 (12.6) | 75.7 (9.1) | NR | 11.7 (8.9) | 10.7 (7.5) | 162 (40.7) | 41 (49.4) | 179 (45.0) | 30 (36.1) | 11 (2.8) | 3 (3.6) | 12 (3.0) | 2 (2.4) | 34 (8.5) | 7 (8.4) | Mortality |
| 24 | Furlan et al. [41] | 2020 | Brazil | Retrospective | IS | No statin | Statin | 97 (100) | 34 (35.1) | 63 (64.9) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality |
| 25 | Winardi et al. [68] | 2024 | Taiwan | Retrospective | IS | No statin | Statin | 78,732 (100) | 39,366 (50.0) | 39,366 (50.0) | 42,936 (54.5) | 21,468 (54.5) | 21,468 (54.5) | NR | 67.7 (9.1) | 68.2 (9.2) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality |
| 26 | Song et al. [64] | 2014 | China | Prospective | First IS | No statin | Statin | 7455 (100) | 4224 (56.7) | 3231 (43.3) | 4584 (61.5) | 2585 (61.2) | 1999 (61.9) | NR | 64.5 (13.2) | 64.2 (12.3) | NR | 5.7 (5.9) | 4.7 (4.4) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality |
| 27 | Hjalmarsson et al. [44] | 2012 | Sweden | Retrospective | Acute IS | No statin | Statin | 744 (100) | 291 (39.1) | 453 (60.9) | 358 (48.1) | 117 (40.2) | 241 (53.2) | NR | 80.8 (8.0) | 76.3 (7.6) | NR | NR | NR | 50 (17.2) | 139 (30.7) | 134 (46.0) | 115 (25.4) | 64 (22.0) | 125 (27.6) | 4 (1.4) | 5 (1.1) | 39 (13.4) | 69 (15.2) | Mortality |
| 28 | Sakurai et al. [61] | 2011 | Japan | Prospective | IS | No statin | Statin | 146 (100) | 101 (69.2) | 45 (30.8) | 91 (62.3) | 63 (62.4) | 28 (62.2) | NR | 71.5 (13.6) | 69.9 (12.5) | NR | 7.1 (7.4) | 5.0 (4.6) | 22 (21.8) | 17 (37.8) | 51 (50.5) | 14 (31.1) | 21 (20.8) | 13 (28.9) | NR | NR | NR | NR | CRP Levels |
| 29 | Ueno et al. [65] | 2015 | Japan | RCT | Acute IS | No statin | Rosuvastatin 5 mg | 24 (100) | 12 (50.0) | 12 (50.0) | 23 (95.8) | 12 (100.0) | 11 (91.7) | 71.3 (9.0) | 71.5 (10.6) | 71.0 (7.6) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Stroke Recurrence, CRP Levels |
| 30 | Flint et al. [40] | 2011 | United States | Retrospective | IS | No statin | Statin | 12,689 (100) | 6395 (50.4) | 6294 (49.6) | 5959 (47.0) | 2800 (43.8) | 3159 (50.2) | NR | 76.5 (NR) | 73.5 (NR) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality |
| 31 | Vitturi & Gagliardi [67] | 2020 | Brazil | Prospective | First ever IS | No statin | Statin | 440 (100) | 96 (21.8) | 344 (78.2) | 189 (43.0) | NR | NR | 58.3 (NR) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| Cardioembolic or AF-related Stroke | ||||||||||||||||||||||||||||||
| 32 | Choi et al. [34] | 2019 | South Korea | Prospective | Acute IS with AF | No statin | Low-moderate- or high-intensity statin | 2153 (100) | 574 (26.7) | 1579 (73.3) | 1120 (52.0) | 322 (56.1) | 798 (50.5) | 73.2 (9.8) | 72.7 (11.0) | NR | 7.7 (8.9) | 8.7 (10.4) | NR | N/A | N/A | 499 (86.9) | 1294 (82.0) | N/A | N/A | N/A | N/A | 75 (13.1) | 285 (18.0) | Mortality, Stroke Recurrence |
| 33 | Lin et al. [52] | 2019 | Taiwan | Retrospective | Acute IS with AF | No statin | Statin | 47,882 (100) | 43,242 (90.3) | 4640 (9.7) | 27,177 (56.8) | 24,553 (56.8) | 2624 (56/6) | NR | 69.6 (14.2) | 65.6 (12.8) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality |
| 34 | Ntaios et al. [58] | 2014 | Greece | Retrospective | Acute IS with AF | No statin | Statin | 404 (100) | 302 (74.8) | 102 (25.2) | NR | NR | NR | 67.2 (12.3) | 74.6 (11.5) | 73.7 (9.8) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| 35 | Choi et al. [33] | 2014 | South Korea | Retrospective | Cardioembolic stroke | No statin | Statin | 535 (100) | 295 (55.1) | 240 (44.9) | 295 (55.1) | 163 (55.3) | 132 (55.0) | NR | 68.6 (13.3) | NR | NR | NR | NR | N/A | N/A | 295 (100) | 240 (100) | N/A | N/A | N/A | N/A | N/A | N/A | Mortality, Stroke Recurrence |
| 36 | Choi et al. [35] | 2024 | Various | Retrospective | Acute IS with AF | No statin | Statin | 20,902 (100) | 13,402 (64.1) | 7500 (35.9) | 10,947 (52.4) | 6941 (51.8) | 4006 (53.4) | NR | 73.5 (12.2) | 73.8 (11.1) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| 37 | Vitturi & Gagliardi [66] | 2019 | Brazil | Prospective | Cardioembolic stroke | No statin | Statin | 91 (100) | 18 (19.8) | 73 (80.2) | 47 (51.6) | 7 (38.9) | 40 (85.1) | NR | 55.9 (13) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| 38 | Gong et al. [42] | 2023 | China | Retrospective | Cardioembolic stroke | No statin | Statin | 510 (100) | 106 (20.8) | 404 (79.2) | 227 (44.5) | 47 (44.3) | 180 (44.6) | 70.7 (10.4) | 70.7 (10.5) | 70.7 (10.4) | 16.3 (5.2) | 17.0 (4.5) | 16.3 (5.2) | N/A | N/A | 106 (20.8) | 404 (79.2) | N/A | N/A | N/A | N/A | N/A | N/A | Mortality |
| 39 | Park et al. [60] | 2020 | South Korea | Prospective | Cardioembolic stroke | No statin | Statin | 2888 (100) | 1025 (35.5) | 1863 (64.5) | 1289 (44.6) | 469 (45.8) | 820 (44.0) | 75.3 (NR) | 75.2 (1.2) | 75.4 (0.9) | NR | 12.3 (10.4) | 8.7 (8.9) | N/A | N/A | 1025 | 1863 | N/A | N/A | N/A | N/A | N/A | N/A | Mortality, Stroke Recurrence |
| 40 | Marvardi et al. [54] | 2025 | Various | Prospective | Acute IS with AF | No statin | Statin | 1742 (100) | 844 (48.5) | 898 (51.5) | 811 (46.6) | 357 (42.3) | 454 (50.6) | NR | 77.2 (10.5) | 74.3 (9.1) | NR | 9.2 (7.2) | 7.6 (6.5) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Stroke Recurrence |
| 41 | Wu et al. [69] | 2017 | Taiwan | Retrospective | Acute IS with AF | No statin | Statin | 4638 (100) | 3092 (66.7) | 1546 (33.3) | 2277 (49.1) | 1518 (49.1) | 759 (49.1) | NR | 75.6 (7.4) | 75.6 (7.4) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Stroke Recurrence |
| Low Baseline LDL-C Levels | ||||||||||||||||||||||||||||||
| 42 | Kim et al. [47] | 2023 | South Korea | Prospective | Acute IS with LDL-C <70 mg/dL | No statin | Statin | 2850 (100) | 735 (25.8) | 2115 (74.2) | 1810 (63.5) | 448 (61.0) | 1362 (64.4) | 69.5 (13.4) | 70.1 (13.9) | 69.3 (13.2) | 5.7 (6.7) | 7.7 (9.7) | 4.7 (5.9) | 229 (31.2) | 903 (42.7) | 400 (54.4) | 775 (36.6) | 106 (14.4) | 437 (20.7) | NR | NR | NR | NR | Mortality |
| 43 | Lee et al. [51] | 2024 | Taiwan | Retrospective | Acute IS with LDL-C <70 mg/dL | No statin | Statin | 956 (100) | 631 (66.0) | 325 (34.0) | NR | NR | NR | 76.6 (13.7) | NR | NR | NR | 11.8 (9.6) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality |
| 44 | Song et al. [63] | 2015 | China | Prospective | Acute IS with LDL-C <1.8 mmol/L | No statin | Statin | 1018 (100) | 659 (64.7) | 359 (35.3) | 687 (67.5) | 440 (66.8) | 247 (68.8) | NR | 65.0 (13.8) | 65.6 (12.1) | NR | 6.0 (6.7) | 5.0 (5.2) | 236 (35.8) | 176 (49.0) | 121 (18.4) | 59 (16.4) | 55 (8.3) | 23 (6.4) | 12 (1.8) | 6 (1.7) | 235 (35.7) | 95 (26.5) | Mortality |
| Statin Intensity | ||||||||||||||||||||||||||||||
| 17 | Bao et al. [28] | 2023 | China | Retrospective | Acute IS | Low-moderate intensity statin | High-intensity statin | 279 (100) | 152 (54.5) | 127 (45.5) | 156 (55.9) | 76 (50.0) | 80 (63.0) | NR | 71.1 (13.4) | 67.6 (13.5) | NR | 8.3 (8.2) | 8.7 (9.0) | 43 (28.3) | 57 (44.9) | 72 (47.4) | 45 (35.4) | 22 (14.5) | 4 (3.1) | 1 (0.7) | 7 (5.5) | 14 (9.2) | 14 (11.0) | Mortality |
| 45 | Yang et al. [71] | 2021 | China | RCT | Acute IS | Rosuvastatin 5 mg | Rosuvastatin 20 mg | 310 (100) | 155 (50.0) | 155 (50.0) | 228 (73.5) | 116 (74.8) | 112 (72.3) | NR | 66.6 (12.0) | 65.0 (11.8) | NR | 7.7 (6.0) | 6.0 (4.5) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality |
| 46 | Chen et al. [32] | 2018 | China | RCT | Anterior circulation infarct | Atorvastatin 20 mg | Atorvastatin 60 mg | 117 (100) | 57 (48.7) | 60 (51.3) | 73 (62.4) | 34 (59.6) | 39 (65.0) | NR | 60.9 (11.9) | 62.4 (11.5) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| 13 | O’Brien et al. [59] | 2015 | United States | Retrospective | IS | Low-moderate intensity statin | High-intensity statin | 29,631 (100) | 20,486 (69.1) | 9145 (30.9) | 12,462 (42.1) | 8502 (41.5) | 3960 (43.3) | NR | 78.9 (8.3) | 77.9 (8.2) | NR | 4.7 (4.4) | 5.3 (5.9) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| 47 | Bach et al. [27] | 2023 | Denmark | Retrospective | First IS | Moderate intensity statin | High-intensity statin | 27,387 (100) | 14,355 (52.4) | 13,032 (47.6) | 15,495 (56.6) | 7905 (55.1) | 7590 (58.2) | NR | 68.7 (14.1) | 68.3 (13.3) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| 48 | Kyto et al. [50] | 2024 | Finland | Retrospective | Acute IS | Low-moderate intensity statin | High-intensity statin | 45,512 (100) | 38,228 (84.0) | 7284 (16.0) | 25,293 (55.6) | 20,762 (54.3) | 4531 (62.2) | NR | NR | 68.4 (10.7) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Mortality, Stroke Recurrence |
| Statin Timing | ||||||||||||||||||||||||||||||
| 49 | Kang et al. [46] | 2015 | South Korea | Retrospective | Acute IS | Delayed statin (after 24 h) | Early statin (within 24 h) | 167 (100) | 122 (73.1) | 45 (26.9) | 107 (64.1) | 67 (54.9) | 30 (66.7) | NR | NR | 67.7 (11.6) | NR | NR | 13.3 (8.4) | 48 (39.3) | 20 (44.4) | 61 (50.0) | 13 (28.9) | NR | NR | NR | NR | NR | NR | Stroke Recurrence |
| Statin Type | ||||||||||||||||||||||||||||||
| 50 | Kim et al. [48] | 2025 | South Korea | Prospective | Acute IS | Atorvastatin | Rosuvastatin | 43,512 (100) | 36,903 (84.8) | 6609 (15.2) | 26,001 (59.8) | 21,992 (59.6) | 4009 (60.7) | 69.2 (12.5) | 69.2 (12.5) | 69.7 (12.8) | 3.7 (4.4) | 3.7 (4.4) | 3.3 (3.7) | 13,976 (37.9) | 2436 (36.9) | 7087 (19.2) | 1314 (19.9) | 6609 (17.9) | 1542 (23.3) | NR | NR | 9231 (25.0) | 1317 (19.9) | Mortality, Stroke Recurrence |
| 51 | Cao et al. [30] | 2017 | China | RCT | Cerebral infarction | Atorvastatin 20 mg | Rosuvastatin 10 mg | 120 (100) | 60 (50.0) | 60 (50.0) | 65 (54.2) | 35 (58.3) | 30 (50.0) | NR | 45.8 (7.5) | 46.8 (7.5) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Stroke Recurrence |
| Author | Year | Hypertension n (%) | Baseline Systolic Blood Pressure Mean (SD) | Diabetes Mellitus n (%) | Atrial Fibrillation n (%) | Coronary Artery Disease n (%) | Dyslipidaemia ^ n (%) | Previous Stroke n (%) | Smoking n (%) | Alcohol Use n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C * | I + | C | I | C * | I + | C * | I + | C * | I + | C * | I + | C * | I + | C * | I + | C * | I + | ||
| All IS Subtypes | |||||||||||||||||||
| Yakusevich et al. [70] | 2012 | 74 (76.3) | 36 (41.9) | 156.4 (15.8) | 156.4 (15.3) | 10 (10.3) | 8 (9.3) | 12 (12.4) | 14 (16.3) | 8 (8.2) | 10 (11.6) | NR | NR | NR | NR | NR | NR | NR | NR |
| Kim et al. [49] | 2024 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Yang et al. [72] | 2022 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Huang et al. [75] | 2015 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Beer et al. [29] | 2012 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Muscari et al. [57] | 2011 | 30 (96.8) | 27 (87.1) | NR | NR | 5 (16.1) | 8 (25.8) | NR | NR | NR | NR | NR | NR | 3 (9.7) | 5 (16.1) | 6 (19.4) | 4 (12.9) | NR | NR |
| Zare et al. [73] | 2012 | 20 (66.7) | 13 (52.0) | NR | NR | 5 (16.7) | 4 (16.0) | NR | NR | NR | NR | 6 (20.0) | 4 (16.0) | NR | NR | 8 (26.7) | 9 (36.0) | NR | NR |
| Aivo et al. [25] | 2015 | 95 (55.9) | 102 (61.1) | NR | NR | 30 (17.6) | 32 (19.2) | 54 (31.8) | 64 (38.3) | NR | NR | NR | NR | 46 (27.1) | 30 (18.0) | NR | NR | NR | NR |
| Flach et al. [39] | 2023 | 8894 (55.0) | 26,614 (61.3) | NR | NR | 3250 (20.1) | 9639 (22.2) | 4964 (30.7) | 9421 (21.7) | 1326 (8.2) | 4211 (9.7) | NR | NR | NR | NR | NR | NR | NR | NR |
| Han et al. [43] | 2019 | 749 (35.5) | 377 (39.6) | NR | NR | 1649 (78.2) | 800 (83.9) | 1562 (74.1) | 833 (87.4) | 1654 (78.5) | 829 (87.0) | 118 (5.6) | 764 (80.2) | NR | NR | 1255 (59.5) | 629 (66.0) | NR | NR |
| Makihara et al. [53] | 2021 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Milionis et al. [55] | 2013 | 1327 (72.3) | 836 (84.2) | NR | NR | 429 (23.5) | 388 (39.1) | 506 (27.7) | 147 (14.8) | 207 (11.3) | 185 (18.6) | NR | NR | NR | NR | 935 (51.1) | 476 (47.9) | NR | NR |
| O’Brien et al. [59] | 2009 | 440 (73.8) | 135 (68.2) | 159.0 (29.0) | 158.0 (26.0) | 211 (35.4) | 55 (27.8) | 77 (12.9) | 24 (12.1) | 144 (24.2) | 45 (22.7) | 151 (25.3) | 57 (28.8) | NR | NR | 233 (39.1) | 80 (40.4) | NR | NR |
| Zhang et al. [74] | 2015 | 17,397 (77.4) | 41,518 (75.5) | NR | NR | 5147 (22.9) | 12,648 (23.0) | NR | NR | 5237 (23.3) | 11,163 (20.3) | 4046 (18.0) | 13,858 (25.2) | NR | NR | 2113 (9.4) | 7259 (13.7) | NR | NR |
| Jia & Zhou [45] | 2018 | 22 (36.1) | 24 (36.4) | NR | NR | 25 (41.0) | 28 (42.4) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Arevalo-Lorido et al. [26] | 2013 | 137 (71.0) | 109 (67.7) | NR | NR | 94 (48.7) | 83 (51.6) | 27 (14.0) | 26 (16.1) | 93 (48.2) | 81 (50.3) | NR | NR | NR | NR | 80 (41.5) | 73 (45.3) | NR | NR |
| Bao et al. [28] | 2014 | 92 (85.2) | 168 (82.0) | 160.4 (27.4) | NR | 29 (26.9) | 64 (31.2) | NR | NR | NR | NR | NR | NR | NR | NR | 16 (14.8) | 45 (22.0) | NR | NR |
| Ni Chroinin et al. [36] | 2023 | 22 (45.8) | 158 (56.6) | 139.0 (23.8) | NR | 7 (14.6) | 44 (15.8) | 17 (35.4) | 77 (27.6) | 3 (6.3) | 39 (14.0) | 0 (0.0) | 10 (3.6) | 12 (25.0) | 53 (19.0) | 13 (27.1) | 103 (36.9) | NR | NR |
| Montaner et al. [56] | 2011 | 59 (52.7) | 84 (44.4) | NR | NR | 6 (5.4) | 11 (5.8) | 44 (39.3) | 52 (27.5) | 17 (15.2) | 21 (11.1) | 18 (16.1) | 37 (19.6) | 12 (10.7) | 16 (8.5) | 23 (20.5) | 70 (37.0) | NR | NR |
| Cappellari et al. [31] | 2016 | 35 (64.8) | 29 (58.0) | NR | NR | 7 (13.0) | 10 (20.0) | 3 (5.6) | 12 (24.0) | 1 (1.9) | 2 (4.0) | 8 (14.8) | 7 (14.0) | 3 (5.6) | 4 (8.0) | 13 (24.1) | 10 (20.0) | NR | NR |
| Cui et al. [37] | 2013 | 706 (57.3) | 595 (70.9) | 146.6 (20.7) | 146.6 (19.6) | 197 (16.0) | 147 (17.5) | 316 (25.6) | 146 (17.4) | NR | NR | 308 (25.0) | 478 (57.0) | 113 (9.2) | 65 (7.7) | 294 (23.8) | 209 (24.9) | NR | NR |
| Cui et al. [38] | 2022 | 34 (46.6) | 92 (50.3) | 135.8 (24.0) | 141.4 (25.1) | 12 (16.4) | 32 (17.5) | NR | NR | 10 (13.7) | 31 (16.9) | NR | NR | NR | NR | 13 (17.8) | 57 (31.1) | NR | NR |
| Scheitz et al. [62] | 2021 | 18 (51.4) | 85 (47.2) | 153.2 (32.2) | 148.5 (24.7) | 8 (22.9) | 34 (18.9) | 17 (48.6) | 46 (25.6) | 4 (11.4) | 22 (12.2) | NR | NR | NR | NR | 10 (28.6) | 59 (32.8) | NR | NR |
| Furlan et al. [41] | 2015 | 320 (80.4) | 79 (95.2) | NR | NR | 87 (21.9) | 30 (36.1) | 169 (42.5) | 32 (38.6) | 63 (15.8) | 33 (39.8) | 148 (37.2) | 60 (72.3) | 83 (20.9) | 29 (34.9) | 94 (23.6) | 19 (22.9) | NR | NR |
| Winardi et al. [68] | 2020 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Song et al. [64] | 2024 | NR | NR | NR | NR | 17,275 (43.9) | 17,524 (44.5) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Hjalmarsson et al. [44] | 2014 | 2300 (54.5) | 1961 (60.7) | NR | NR | 692 (16.4) | 646 (20.0) | 333 (7.9) | 156 (4.8) | 540 (12.8) | 358 (11.1) | NR | NR | NR | NR | 1651 (39.1) | 1304 (40.4) | 431 (10.2) | 379 (11.7) |
| Sakurai et al. [61] | 2012 | 162 (55.7) | 262 (57.8) | 142.9 (22.5) | 141.4 (21.3) | 30 (10.3) | 69 (26.3) | 115 (39.5) | 101 (38.5) | NR | NR | 10 (3.4) | 108 (41.2) | 123 (42.3) | 90 (34.4) | NR | NR | NR | NR |
| Ueno et al. [65] | 2011 | 77 (76.2) | 37 (82.2) | NR | NR | 22 (21.8) | 12 (26.7) | 43 (42.6) | 8 (17.8) | 19 (18.8) | 10 (22.2) | 7 (6.9) | 45 (100.0) | NR | NR | 33 (32.7) | 18 (40.0) | NR | NR |
| Flint et al. [40] | 2015 | 9 (75.0) | 11 (91.7) | NR | NR | 6 (50.0) | 3 (25.0) | 1 (8.3) | 2 (16.7) | NR | NR | 12 (100.0) | 12 (100.0) | 3 (25.0) | 3 (25.0) | 5 (41.7) | 6 (50.0) | NR | NR |
| Vitturi & Gagliardi [67] | 2011 | 4816 (75.3) | 5363 (85.2) | NR | NR | 1769 (27.7) | 2449 (38.9) | 1771 (27.7) | 1403 (22.3) | 1154 (18.0) | 1914 (30.4) | NR | NR | 654 (10.2) | 475 (7.5) | NR | NR | NR | NR |
| Yakusevich et al. [70] | 2020 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Cardioembolic or AF-related stroke | |||||||||||||||||||
| Choi et al. [34] | 2019 | 395 (68.8) | 1109 (70.2) | NR | NR | 156 (27.2) | 434 (27.5) | 574 (100.0) | 1579 (100.0) | 61 (10.6) | 206 (13.0) | 98 (17.1) | 404 (25.6) | NR | NR | 94 (16.4) | 219 (13.9) | NR | NR |
| Lin et al. [52] | 2019 | 31,698 (73.3) | 3579 (77.1) | NR | NR | 15,951 (36.9) | 1857 (40.0) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Ntaios et al. [58] | 2014 | 224 (74.2) | 83 (81.4) | NR | NR | 63 (20.9) | 20 (19.6) | 262 (86.8) | 86 (84.3) | NR | NR | 83 (27.5) | 53 (52.0) | NR | NR | 52 (17.2) | 21 (20.6) | NR | NR |
| Choi et al. [33] | 2014 | 199 (67.5) | 171 (71.3) | NR | NR | 56 (19.0) | 67 (27.9) | NR | NR | 30 (10.2) | 43 (17.9) | NR | NR | NR | NR | 76 (25.8) | 67 (27.9) | NR | NR |
| Choi et al. [35] | 2024 | 9424 (70.3) | 3693 (49.2) | NR | NR | 1305 (9.7) | 1597 (21.3) | 11,298 (84.3) | 4219 (56.3) | NR | NR | 5468 (40.8) | 2420 (32.3) | NR | NR | NR | NR | NR | NR |
| Vitturi & Gagliardi [66] | 2019 | 12 (66.7) | 58 (79.5) | NR | NR | 4 (22.2) | 21 (28.8) | 9 (50.0) | 40 (54.8) | 2 (11.1) | 18 (24.7) | 2 (11.1) | 14 (19.2) | 4 (22.2) | 16 (21.9) | 6 (33.3) | 18 (24.7) | NR | NR |
| Gong et al. [42] | 2023 | 52 (49.1) | 207 (51.2) | 144.0 (25.4) | 144.0 (24.4) | 18 (17.0) | 65 (16.1) | 77 (72.6) | 276 (68.3) | 14 (13.2) | 84 (20.8) | 12 (11.3) | 43 (10.6) | 23 (21.7) | 73 (18.1) | 13 (12.3) | 50 (12.4) | NR | NR |
| Park et al. [60] | 2020 | 708 (69.1) | 1297 (69.6) | 142.0 (2.6) | 140.5 (1.7) | 267 (26.0) | 460 (24.7) | 940 (91.7) | 1615 (86.7) | NR | NR | 153 (14.9) | 569 (30.5) | NR | NR | 114 (11.1) | 215 (11.5) | NR | NR |
| Marvardi et al. [54] | 2025 | 623 (73.8) | 720 (80.2) | NR | NR | 165 (19.5) | 231 (25.7) | 312 (37.0) | 420 (46.8) | 92 (10.9) | 163 (18.2) | 130 (15.4) | 445 (49.6) | 199 (23.6) | 257 (28.6) | NR | NR | 51 (6.0) | 70 (7.8) |
| Wu et al. [69] | 2017 | 2986 (96.6) | 1493 (96.6) | NR | NR | 1036 (33.5) | 518 (33.5) | NR | NR | 2028 (65.6) | 1014 (65.6) | NR | NR | NR | NR | NR | NR | NR | NR |
| Low Baseline LDL-C Levels | |||||||||||||||||||
| Kim et al. [47] | 2023 | 437 (59.5) | 1365 (64.5) | NR | NR | 240 (32.7) | 807 (38.2) | 325 (44.2) | 627 (29.6) | NR | NR | 37 (5.0) | 239 (11.3) | NR | NR | 173 (23.5) | 604 (28.6) | NR | NR |
| Lee et al. [51] | 2024 | 476 (75.4) | NR | NR | NR | 254 (40.3) | NR | 192 (30.4) | NR | 132 (20.9) | NR | NR | NR | 202 (32.0) | NR | 143 (22.7) | NR | NR | NR |
| Song et al. [63] | 2015 | 373 (56.6) | 230 (70.8) | NR | NR | 121 (18.4) | 71 (21.8) | 95 (14.4) | 38 (11.7) | 87 (13.2) | 47 (14.5) | NR | NR | 215 (32.6) | 115 (35.4) | 294 (44.6) | 151 (46.5) | 71 (10.8) | 34 (10.5) |
| Statin Intensity | |||||||||||||||||||
| Bao et al. [28] | 2023 | 93 (61.2) | 65 (51.2) | 146.5 (24.2) | 151.1 (26.1) | 28 (18.4) | 16 (12.6) | 53 (34.9) | 24 (18.9) | 24 (15.8) | 15 (11.8) | 5 (3.3) | 5 (3.9) | 36 (23.7) | 17 (13.4) | 55 (36.2) | 48 (37.8) | NR | NR |
| Yang et al. [71] | 2021 | 85 (54.8) | 85 (54.8) | NR | NR | 21 (13.5) | 19 (12.3) | 25 (16.1) | 9 (5.8) | 21 (13.5) | 11 (7.1) | 9 (5.8) | 7 (4.5) | 28 (18.1) | 25 (16.1) | NR | NR | NR | NR |
| Chen et al. [32] | 2018 | 41 (71.9) | 45 (75.0) | 144.0 (22.6) | 143.5 (22.1) | 17 (29.8) | 21 (35.0) | NR | NR | 3 (5.3) | 5 (8.3) | 18 (31.6) | 23 (38.3) | 5 (8.8) | 7 (11.7) | 25 (43.9) | 28 (46.7) | 25 (43.9) | 22 (36.7) |
| O’Brien et al. [59] | 2015 | 15,201 (74.2) | 6850 (74.9) | NR | NR | 4650 (22.7) | 2268 (24.8) | NR | NR | 4261 (20.8) | 2094 (22.9) | 5183 (25.3) | 2405 (26.3) | NR | NR | 2684 (13.1) | 1244 (13.6) | NR | NR |
| Bach et al. [27] | 2023 | 8100 (56.4) | 7387 (56.7) | NR | NR | 1147 (8.0) | 1078 (8.3) | NR | NR | NR | NR | NR | NR | NR | NR | 4688 (32.7) | 3862 (29.6) | 13,528 (94.2) | 11,667 (89.5) |
| Kyto et al. [50] | 2024 | 23,107 (50.8) | 4786 (10.5) | NR | NR | 8625 (19.0) | 1981 (4.4) | 8410 (18.5) | 1508 (3.3) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Statin Timing | |||||||||||||||||||
| Kang et al. [46] | 2015 | 74 (60.7) | 28 (62.2) | NR | NR | 22 (18.0) | 10 (22.2) | 49 (40.2) | 15 (33.3) | NR | NR | NR | NR | 18 (14.8) | 12 (26.7) | NR | NR | NR | NR |
| Statin Type | |||||||||||||||||||
| Kim et al. [48] | 2025 | 24,562 (66.6) | 4550 (68.8) | 146.1 (27.7) | 152.4 (27.7) | 12,426 (33.7) | 2372 (35.9) | 7214 (19.5) | 1275 (19.3) | 3146 (8.5) | 625 (9.5) | 12,656 (34.3) | 2519 (38.1) | 7274 (19.7) | 1543 (23.3) | 9010 (24.4) | 1490 (22.5) | NR | NR |
| Cao et al. [30] | 2017 | 28 (46.7) | 25 (41.7) | NR | NR | 10 (16.7) | 11 (18.3) | NR | NR | NR | NR | 15 (25.0) | 16 (26.7) | NR | NR | 7 (11.7) | 8 (13.3) | NR | NR |
| Outcome | Time Frame | Analysis Subgroup | Overall | Statin Nonusers | Statin Users | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Summary Effects | Heterogeneity | Heterogeneity Variance Estimates | Summary Effects | Heterogeneity | Heterogeneity Variance Estimates | Summary Effects | Heterogeneity | Heterogeneity Variance Estimates | |||||||||||||||
| Pooled Prevalence (95% CI) | Test of ES = 0 | Chi-Squared | H | I2 (%) | p-Value | τ2 ≤ Φ | Pooled Prevalence (95% CI) | Test of ES = 0 | Chi-Squared | H | I2 (%) | p-Value | τ2 ≤ Φ | Pooled Prevalence (95% CI) | Test of ES = 0 | Chi-squared | H | I2 (%) | p-Value | τ2 ≤ Φ | |||
| Dementia or Cognitive Impairment | Dementia | - | - | - | - | - | - | - | 0.12 [0.11, 0.12] | z = 98.99, p < 0.01 | - | - | - | - | - | 0.11 [0.11, 0.11] | z = 144.13, p < 0.01 | - | - | - | - | - | |
| Cognitive Impairment | - | - | - | - | - | - | - | 0.36 [0.29, 0.42] | z = 17.72, p < 0.01 | - | - | - | - | - | 0.46 [0.37, 0.54] | z = 16.33, p < 0.01 | - | - | - | - | - | ||
| Overall | 0.18 [0.09, 0.30] | z = 6.16, p < 0.01 | 1939.56 | - | 99.90 | <0.01 | 0.06 | 0.19 [0.09, 0.31] | z = 6.05, p < 0.01 | 619.12 | - | 99.68 | <0.01 | 0.06 | 0.19 [0.09, 0.31] | z = 5.67, p < 0.01 | 1444.50 | - | 99.86 | <0.01 | 0.06 | ||
| All-Cause Mortality | ≤3 months | Retrospective | 0.18 [0.12, 0.24] | z = 9.75, p < 0.01 | - | 36.14 | 91.70 | <0.01 | - | 0.25 [0.16, 0.34] | z = 8.93, p < 0.01 | - | 27.15 | 88.95 | <0.01 | - | 0.11 [0.06, 0.19] | z = 5.77, p < 0.01 | - | 26.21 | 88.55 | <0.01 | - |
| Prospective | 0.13 [0.07, 0.21] | z = 6.34, p < 0.01 | - | - | - | - | - | 0.25 [0.08, 0.47] | z = 4.13, p < 0.01 | - | - | - | - | - | 0.07 [0.03, 0.13] | z = 5.14, p < 0.01 | - | - | - | - | - | ||
| RCT | 0.04 [0.02, 0.07] | z = 6.17, p < 0.01 | - | - | - | - | - | 0.04 [0.01, 0.09] | z = 3.28, p < 0.01 | - | - | - | - | - | 0.03 [0.01, 0.07] | z = 3.50, p < 0.01 | - | - | - | - | - | ||
| Overall | 0.12 [0.09, 0.16] | z = 11.67, p < 0.01 | - | 160.04 | 94.38 | <0.01 | 0.03 | 0.18 [0.13, 0.24] | z = 10.38, p < 0.01 | - | 140.81 | 93.61 | <0.01 | 0.04 | 0.08 [0.05, 0.11] | z = 8.38, p < 0.01 | - | 77.56 | 88.40 | <0.01 | 0.02 | ||
| ≤1 year | Retrospective | 0.17 [0.08, 0.30] | z = 5.31, p < 0.01 | - | 4303.98 | 99.86 | <0.01 | - | 0.26 [0.13, 0.42] | z = 5.86, p < 0.01 | - | 2321.27 | 99.74 | <0.01 | - | 0.11 [0.05, 0.19] | z = 5.01, p < 0.01 | - | 1364.31 | 99.56 | <0.01 | - | |
| Prospective | 0.14 [0.07, 0.24] | z = 5.86, p < 0.01 | - | 113.27 | 97.35 | <0.01 | - | 0.26 [0.10, 0.45] | z = 4.76, p < 0.01 | - | 97.91 | 96.94 | <0.01 | - | 0.08 [0.03, 0.16] | z = 4.32, p < 0.01 | - | 73.56 | 95.92 | <0.01 | - | ||
| RCT | 0.07 [0.01, 0.17] | z = 2.82, p < 0.01 | - | - | - | - | - | 0.06 [0.00, 0.18] | z = 2.08, p < 0.01 | - | - | - | - | - | 0.08 [0.02, 0.17] | z = 3.37, p < 0.01 | - | - | - | - | - | ||
| Overall | 0.14 [0.08, 0.21] | z = 7.82 p < 0.01 | - | 4436.65 | 99.71 | <0.01 | 0.11 | 0.21 [0.14, 0.30] | z = 8.49, p < 0.01 | - | 2445.12 | 99.47 | <0.01 | 0.13 | 0.09 [0.06, 0.14] | z = 7.30, p < 0.01 | - | 1453.11 | 99.11 | <0.01 | 0.07 | ||
| >1 year | Retrospective | 0.35 [0.07, 0.71] | z = 3.28, p < 0.01 | - | - | - | - | - | 0.38 [0.12, 0.69] | z = 4.01, p < 0.01 | - | - | - | - | - | 0.34 [0.05, 0.72] | z = 3.04, p < 0.01 | - | - | - | - | - | |
| Prospective | 0.17 [0.06, 0.31] | z = 4.79, p < 0.01 | - | 576.47 | 99.31 | <0.01 | - | 0.26 [0.13, 0.42] | z = 5.73, p < 0.01 | - | 305.38 | 98.69 | <0.01 | - | 0.12 [0.04, 0.24] | z = 4.26, p < 0.01 | - | 223.24 | 98.21 | <0.01 | - | ||
| Overall | 0.23 [0.07, 0.44] | z = 4.20, p = 0.01 | - | 36,960.44 | 99.98 | <0.01 | 0.42 | 0.30 [0.14, 0.50] | z = 5.30, p < 0.01 | - | 11,553.88 | 99.94 | <0.01 | 0.33 | 0.19 [0.05, 0.41] | z = 3.58, p < 0.01 | - | 23,089.78 | 99.97 | <0.01 | 0.46 | ||
| Stroke Recurrence | ≤1 year | Retrospective | 0.03 [0.00, 0.09] | z = 2.53, p = 0.01 | - | 14.26 | 78.97 | <0.01 | - | 0.08 [0.08, 0.09] | z = 73.79, p < 0.01 | - | - | - | - | - | 0.07 [0.06, 0.07] | z = 107.27, p < 0.01 | - | - | - | - | - |
| RCT | 0.07 [0.07, 0.07] | z = 130.56, p < 0.01 | - | - | - | - | - | 0.04 [0.00, 0.11] | z = 2.43, p = 0.02 | - | 8.57 | 65.01 | 0.04 | - | 0.02 [0.00, 0.06] | z = 1.84, p = 0.07 | - | 5.90 | 49.13 | 0.12 | - | ||
| Overall | 0.04 [0.02, 0.08] | z = 4.38, p < 0.01 | - | 21.48 | 81.38 | <0.01 | 0.02 | 0.05 [0.02, 0.10] | z = 4.59, p < 0.01 | - | 11.34 | 64.74 | 0.02 | 0.02 | 0.03 [0.01, 0.07] | z = 3.41, p < 0.01 | - | 10.91 | 63.32 | 0.03 | 0.02 | ||
| >1 year | Retrospective | 0.20 [0.12, 0.30] | z = 7.62, p < 0.01 | - | 4717.49 | 99.92 | <0.01 | - | 0.23 [0.13, 0.34] | z = 7.58, p < 0.01 | - | 1566.58 | 99.74 | <0.01 | - | 0.15 [0.08, 0.25] | z = 6.47, p < 0.01 | - | 3191.48 | 99.87 | <0.01 | - | |
| Prospective | 0.12 [0.07, 0.18] | z = 7.99, p < 0.01 | - | - | - | - | - | 0.14 [0.08, 0.22] | z = 7.28, p < 0.01 | - | - | - | - | - | 0.10 [0.05, 0.16] | z = 6.92, p < 0.01 | - | - | - | - | - | ||
| Overall | 0.17 [0.11, 0.24] | z = 9.02, p < 0.01 | - | 5040.67 | 99.86 | <0.01 | 0.06 | 0.20 [0.13, 0.28] | z = 9.31, p < 0.01 | - | 1761.82 | 99.60 | <0.01 | 0.07 | 0.13 [0.08, 0.20] | z = 7.69, p < 0.01 | - | 3338.94 | 99.79 | <0.01 | 0.06 | ||
| Outcome | Time Frame | N | n | Effect Measure | Analysis Subgroup | Summary Effects | Heterogeneity | Heterogeneity Variance Estimates | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | SMD (95% CI) | Test of Overall Effect | Cochran’s Q | H | I2 (%) | p-Value | τ2 ≤ Φ | ||||||
| Post-Stroke Dementia or Cognitive Decline | - | 2 | 67,666 | OR | Post-Stroke Dementia | 0.74 [0.60, 0.90] | - | z = −2.94, p < 0.01 | 12.69 | - | 92.1 | <0.01 | 0.02 |
| 1 | 350 | Post-Stroke Cognitive Impairment | 1.52 [0.98, 2.36] | z = 1.886, p = 0.06 | 0.00 | - | - | - | |||||
| 3 | 68,016 | Overall | 0.83 [0.66, 1.05] | z = −1.54, p = 0.12 | 21.95 | 3.31 | 90.9 | <0.01 | 0.03 | ||||
| All-Cause Mortality | ≤3 months | 4 | 2749 | OR | Retrospective | 0.36 [0.27, 0.47] | - | z = −7.41, p < 0.01 | 2.36 | - | 0.0 | 0.50 | - |
| 3 | 8142 | Prospective | 0.26 [0.18, 0.39] | z = −7.09, p < 0.01 | 4.10 | 51.2 | 0.13 | 0.06 | |||||
| 3 | 342 | RCT | 0.73 [0.25, 2.11] | z = −0.58, p = 0.57 | 1.13 | 0.0 | 0.57 | - | |||||
| 10 | 11,233 | Overall | 0.32 [0.26, 0.39] | z = −12.438, p < 0.01 | 11.16 | 1.11 | 19.4 | 0.27 | 0.02 | ||||
| ≤1 year | 7 | 75,770 | OR | Retrospective | 0.37 [0.28, 0.47] | - | z = −7.554, p < 0.01 | 63.30 | - | 90.5 | <0.01 | 0.08 | |
| 4 | 8455 | Prospective | 0.31 [0.26, 0.36] | z = −13.26, p < 0.01 | 2.62 | 0.0 | 0.45 | - | |||||
| 3 | 342 | RCT | 0.93 [0.46, 1.90] | z = −0.20, p = 0.84 | 0.80 | 0.0 | 0.81 | - | |||||
| 14 | 84,567 | Overall | 0.35 [0.28, 0.44] | z = −9.30, p < 0.01 | 96.31 | 2.75 | 86.8 | <0.01 | 0.09 | ||||
| >1 year | 3 | 156,554 | OR | Retrospective | 0.78 [0.54, 1.12] | - | z = −1.36, p = 0.17 | 292.93 | - | 99.3 | <0.01 | 0.08 | |
| 5 | 6794 | Prospective | 0.41 [0.27, 0.62] | z = −4.20, p < 0.01 | 18.56 | 78.4 | 0.01 | 0.14 | |||||
| 8 | 163,348 | Overall | 0.56 [0.44, 0.72] | z = −4.51, p < 0.01 | 326.91 | 6.83 | 97.9 | <0.01 | 0.08 | ||||
| Stroke Recurrence | ≤1 year | 1 | 59,588 | OR | Retrospective | 0.77 [0.72, 0.82] | - | z = −7.59, p < 0.01 | 0.00 | - | - | - | - |
| 4 * | 438 | RCT | 0.62 [0.24, 1.60] | z = −0.99, p = 0.32 | 1.68 | 0.0 | 0.64 | - | |||||
| 5 * | 60,026 | Overall | 0.77 [0.72, 0.82] | z = −7.64, p < 0.01 | 1.88 | 0.69 | 0.0 | 0.76 | <0.01 | ||||
| >1 year | 5 | 138,670 | OR | Retrospective | 0.82 [0.70, 0.95] | - | z = −2.60, p = 0.01 | 32.50 | - | 87.1 | <0.001 | 0.02 | |
| 3 | 6323 | Prospective | 0.68 [0.51, 0.89] | z = −2.79, p = 0.01 | 3.81 | 47.5 | 0.15 | 0.03 | |||||
| 8 | 144,993 | Overall | 0.76 [0.66, 0.87] | z = −3.88, p < 0.01 | 46.86 | 2.59 | 85.1 | <0.01 | 0.02 | ||||
| CRP Levels | 3–7 days | 3 | 248 | SMD | - | - | −0.41 [−0.75, −0.06] | z = −2.33, p = 0.02 | 0.01 | 0.08 | 0.0 | 0.993 | <0.01 |
| >7 days | 4 | 504 | SMD | - | - | −2.64 [−5.26, −0.03] | z = −1.98, p < 0.01 | 207.97 | 8.33 | 98.6 | < 0.01 | 6.96 | |
| Parameter | Outcome | Timeframe | N | n | Effect Measure | Variation/ Comparison | Effect Size | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Pooled Prevalence (95% CI) | Test of ES = 0 | OR (95% CI) | Test of Overall Effect | |||||||
| Statin Type | All-Cause Mortality | ≤1 year | 2 | 136 | Prevalence | Simvastatin | 0.10 [0.06, 0.16] | z = 6.44, p < 0.01 | N/A | N/A |
| 1 | 25 | Lovastatin | 0.04 [0.00, 0.20] | z = 1.42, p = 0.16 | N/A | N/A | ||||
| 3 | 37,020 | Atorvastatin | 0.05 [0.02, 0.08] | z = 5.18, p < 0.01 | N/A | N/A | ||||
| 3 | 6919 | Rosuvastatin | 0.04 [0.01, 0.07] | z = 4.55, p < 0.01 | N/A | N/A | ||||
| Stroke Recurrence | ≤1 year | 2 | 136 | Prevalence | Simvastatin | 0.03 [0.00, 0.06] | z = 2.89, p < 0.01 | N/A | N/A | |
| 4 | 37,080 | Atorvastatin | 0.04 [0.03, 0.05] | z = 10.93, p < 0.01 | N/A | N/A | ||||
| 3 | 6681 | Rosuvastatin | 0.02 [0.00, 0.07] | z = 1.47, p = 0.14 | N/A | N/A | ||||
| Statin Solubility | All-Cause Mortality | ≤1 year | 2 | 6919 | Prevalence | Hydrophilic | 0.06 [0.05, 0.06] | z = 36.84, p < 0.01 | N/A | N/A |
| 5 | 37,181 | Lipophilic | 0.06 [0.03, 0.10] | z = 5.88, p < 0.01 | N/A | N/A | ||||
| Stroke Recurrence | ≤1 year | 3 | 6681 | Prevalence | Hydrophilic | 0.02 [0.00, 0.07] | z = 1.47, p = 0.14 | N/A | N/A | |
| 5 | 37,216 | Lipophilic | 0.04 [0.02, 0.06] | z = 6.37, p < 0.01 | N/A | N/A | ||||
| Statin Timing | All-Cause Mortality | 90-day | 3 | 316 | Prevalence | ≤1 day | 0.10 [0.06, 0.12] | z = 7.13, p < 0.01 | N/A | N/A |
| 3 | 1169 | >1 day | 0.06 [0.03, 0.09] | z = 7.45, p < 0.01 | N/A | N/A | ||||
| Stroke Recurrence | 90-day | 2 | 95 | Prevalence | ≤1 day | 0.05 [0.01, 0.11] | z = 3.44, p < 0.01 | N/A | N/A | |
| 2 | 239 | >1 day | 0.09 [0.06, 0.14] | z = 8.45, p < 0.01 | N/A | N/A | ||||
| Statin Intensity | All-Cause Mortality | ≤2 years | 1 | 25 | Prevalence | Low | 0.04 [0.00, 0.20] | z = 1.42, p = 0.16 | N/A | N/A |
| 4 | 21,001 | Low-moderate | 0.19 [0.12, 0.28] | z = 8.31, p < 0.01 | N/A | N/A | ||||
| 4 | 348 | Moderate | 0.05 [0.01, 0.13] | z = 2.68, p = 0.01 | N/A | N/A | ||||
| 2 | 471 | Moderate-high | 0.04 [0.02, 0.06] | z = 7.54, p < 0.01 | N/A | N/A | ||||
| 3 | 9360 | High | 0.09 [0.00, 0.32] | z = 1.48, p = 0.14 | N/A | N/A | ||||
| N/A | 6 | 103,028 | OR | Lower intensity vs. higher intensity | N/A | N/A | 0.92 [0.76, 1.12] | z = −0.80, p = 0.42 | ||
| Stroke Recurrence | ≤2 years | 1 | 20,486 | Prevalence | Low-moderate | 0.10 [0.10, 0.11] | z = 93.47, p = 0.01 | N/A | N/A | |
| 4 | 205 | Moderate | 0.04 [0.00, 0.10] | z = 2.40, p = 0.02 | N/A | N/A | ||||
| 1 | 344 | Moderate-high | 0.17 [0.13, 0.22] | z = 14.90, p < 0.01 | N/A | N/A | ||||
| 2 | 9205 | High | 0.10 [0.10, 0.11] | z = 55.10, p = 0.12 | N/A | N/A | ||||
| N/A | 4 | 102,647 | OR | Lower intensity vs. higher intensity | N/A | N/A | 1.10 [0.88, 1.38] | z = −0.82, p = 0.41 | ||
| Outcome | No. of Studies (Participants) | Study Design | Relative Effect (95% CI) | Assumed Risk (Control) | Risk with Statin | Absolute Effect | Certainty of Evidence | Reasons |
|---|---|---|---|---|---|---|---|---|
| All-cause mortality, ≤1 year | 14 (n = 84,567) | Observational and RCTs (adjusted estimates pooled via random-effects) | OR 0.35 (0.28–0.44) | 210 per 1000 | 90 per 1000 | 120 fewer per 1000 | ⊕⊕◯◯ Low to Moderate | −1 risk of bias; −1 inconsistency; +1 large effect |
| Stroke recurrence, ≤1 year | 5 (n = 60,026) | Observational and RCTs (random-effects) | OR 0.77 (0.72–0.82) | — | — | — | ⊕⊕◯◯ Low | −1 risk of bias; −1 inconsistency; −1 zero-event handling |
| Post-stroke dementia (any time) | 2 (subset) | Observational (random-effects) | OR 0.74 (0.60–0.90) | — | — | — | ⊕⊕◯◯ Low | −1 risk of bias; −1 imprecision; −1 inconsistency likely |
| CRP (3–7 d/>7 d) | 3/4; n = 248/504 | Observational and RCTs; continuous outcome (SMD) | SMD −0.41 (−0.75 to −0.06) at 3–7 d; SMD −2.64 (−5.26 to −0.03) at >7 d | — | — | — | ⊕◯◯◯ Very low | −1 risk of bias; −1 inconsistency; −1 indirectness |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gupta, M.; Spring, K.J.; Beran, R.G.; Bhaskar, S. Impact of Statin Therapy on the Risk of Stroke Recurrence, Mortality, and Dementia After Ischemic Stroke (ISMARDD Study): A Comprehensive Meta-Analysis. Neurol. Int. 2025, 17, 176. https://doi.org/10.3390/neurolint17110176
Gupta M, Spring KJ, Beran RG, Bhaskar S. Impact of Statin Therapy on the Risk of Stroke Recurrence, Mortality, and Dementia After Ischemic Stroke (ISMARDD Study): A Comprehensive Meta-Analysis. Neurology International. 2025; 17(11):176. https://doi.org/10.3390/neurolint17110176
Chicago/Turabian StyleGupta, Muskaan, Kevin J. Spring, Roy G. Beran, and Sonu Bhaskar. 2025. "Impact of Statin Therapy on the Risk of Stroke Recurrence, Mortality, and Dementia After Ischemic Stroke (ISMARDD Study): A Comprehensive Meta-Analysis" Neurology International 17, no. 11: 176. https://doi.org/10.3390/neurolint17110176
APA StyleGupta, M., Spring, K. J., Beran, R. G., & Bhaskar, S. (2025). Impact of Statin Therapy on the Risk of Stroke Recurrence, Mortality, and Dementia After Ischemic Stroke (ISMARDD Study): A Comprehensive Meta-Analysis. Neurology International, 17(11), 176. https://doi.org/10.3390/neurolint17110176








