The Effects of Physical Activity in Children and Adolescents with Developmental Coordination Disorder
Abstract
1. Introduction
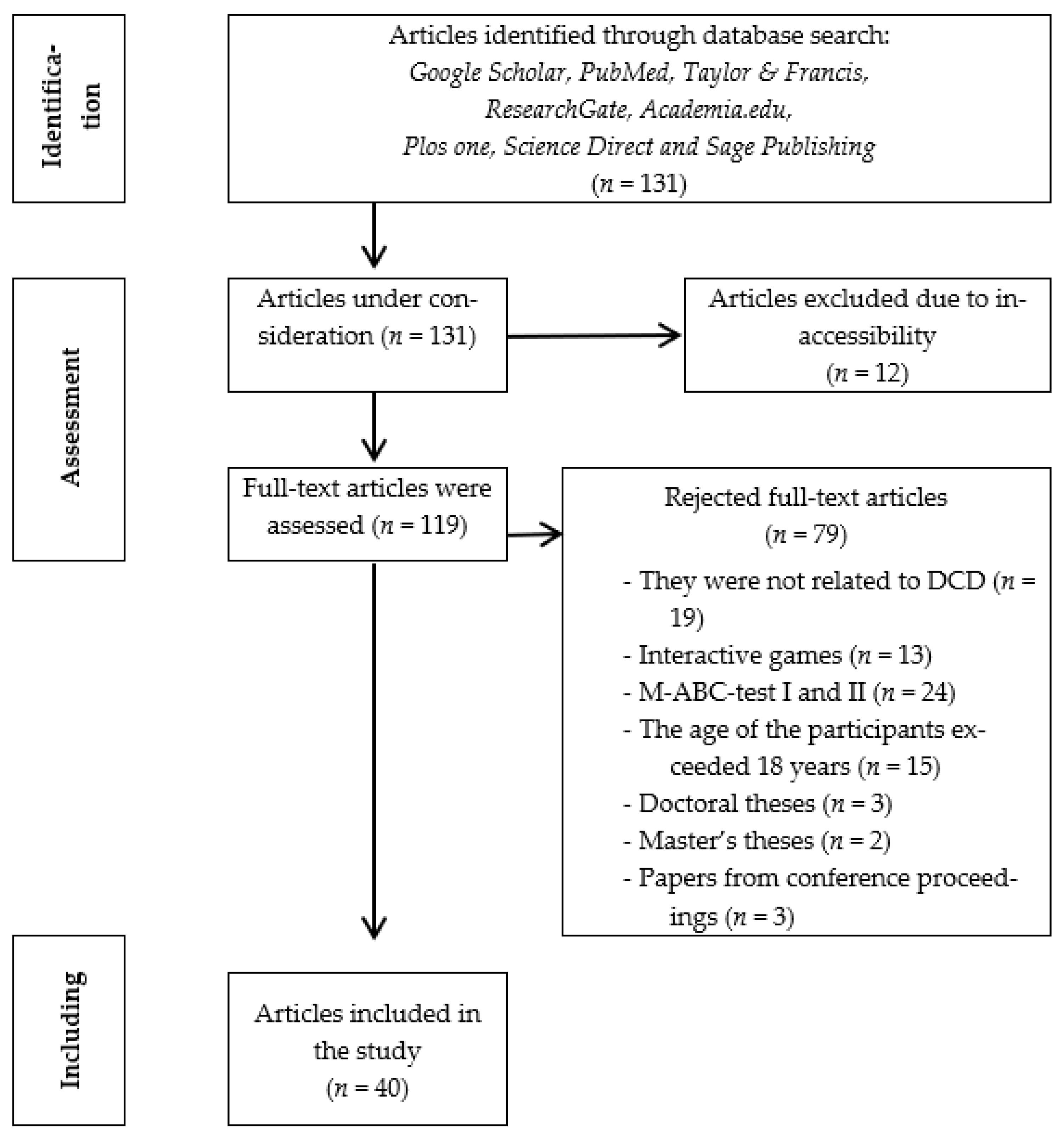
2. Purpose, Assumptions and Conditions of the Research
3. Research Methodology
3.1. Eligibility Criteria
3.2. Information Sources
3.3. Search Strategy and Study Selection
4. Results of the Survey
4.1. Results According to the First Hypothesis
4.1.1. Outcomes Related to Preschool Age
4.1.2. Outcomes of Combative Contact Sports Interventions
4.1.3. Interventions Results of Mixed Methods
4.1.4. Outcomes of Play-Based Interventions
4.1.5. Outcomes of Interventions Focused on a Specific Activity
4.1.6. Outcomes of Interventions Focused on Aerobic Activity
4.1.7. Outcomes of Trampoline Interventions
4.1.8. Outcomes of Therapeutic Riding Interventions
4.1.9. Outcomes of Interventions with Musical Motor Activities
4.2. Results According to the Second Hypothesis
| Number | Author, Author Team, Year of Publication | Total Duration of Intervention and Weekly Frequency of Physical Activity | Comorbidity | Physical Activity | Outcomes |
|---|---|---|---|---|---|
| 1. | Sit et al. (2019), [46] | 8 weeks, 40 min per week | It was not reported | School-based program of Fundamental Movement Skills (FMS) for motor functions, physical activity and other psychological outcomes. Practice 5 specific FMS skills (running, jumping, catching, kicking, and throwing). | FMS training has been shown to promote long-term physical and psychological health by improving certain factors: (1) Motor skills and object control skills. (2) The time spent by children with DCD in moderate to vigorous physical activity both on weekdays and on weekend days. (3) The enjoyment of their participation in physical activity during free time. These improvements were still evident 12 months after the intervention. |
| 2. | Hession et al. (2019), [40] | 2 times on September of 2013 and 8 weeks (January—February 2014), 1 session per week for 30 min | Attention Deficit Hyperactivity Disorder (ADHD), Asperger, Autism Spectrum (ASD) Disorders, Sensory Processing Disorder, Hypotonic Muscle Tone | Two intervention programs: (1) Therapeutic riding, (2) Audiovisual with exposure to the rhythm and movement of horses. | (1) Reduction in problematic behavior in both intervention groups (an improvement over time in emotional and behavioral functioning). (2) Reduction in depressive symptoms in both groups (3) Positive effect on the social response (social functioning) of the children of the two groups (4) Positive effect on gait and gross motor coordination in the therapeutic riding group, while no statistically significant changes were observed in the control group. |
| 3. | Díaz-Pérez et al. (2020), [41] | 10 weeks, 1 session per week for 50 min | It was not reported | Music–motor intervention program based on music, movement and dance. Specifically, singing games, (b) non-singing games and (c) dancing games. | Only the children in the intervention group had significant changes, improving their motor performance. This highlights the effectiveness of the program based on dance, movement and music activities as it activates cognitive areas. Indeed, many of the children who participated in the intervention program left their difficulties behind and achieved scores on the MABC-2 so that they were considered outside the risk level of motor coordination problems. |
| 4. | Zwicker et al. (2014), [31] | 2 weeks for July 2012 and 2 weeks for July 2013, 4 sessions per 2 weeks for 90 min each time | It was not reported | Intervention program implemented in a summer camp for children with DCD based on (1) Cognitive Orientation to daily Occupational Performance (CO-OP)—Functional Kinetic Objectives, (2) the sports activities that the camp program had (hiking, climbing). | The children themselves perceived a significant improvement in the achievement of their chosen goal and felt satisfied with their performance in relation to these goals. Self-confidence increased as the camp provided children with opportunities for trying new activities, learning strategies, being and working with other children with DCD, and knowledge about DCD. Parents of participants in both camps reported that their children continued to use the strategies learned at camp. No significant improvement was found in children’s perceived self-efficacy, goal-setting, self-concept and competence in predisposition to physical activity before and after the camp. |
| 5. | Heus et al. (2020), [29] | 20 sessions, 1 session per week for 60 min each time | ADHD, ASD and persons with possible existence of ADHD, ASD | An intervention program implemented in a rehabilitation center for DCD in which were used, among others, (1) Cognitive Orientation to daily Occupational Performance (CO-OP) (2) Neuromotor Task Training methods. | Positive results: (1) In setting goals to rehabilitate problems in everyday life. (2) In the quality and speed of execution of daily projects only for children between 5 and 8 years old. (3) In MABC-2. In some subscales, there were significant differences; however, these differences were very small regarding (1) the degree to which a child has problems in different types of behavior related to scales of cognitive functioning and (2) the measurement of general aspects of the quality of life, as related to health, was shown. |
| 6 | Rahman et al., 2021, [47] | 16 sessions, 3 times per week for 45 min | It was not reported | Included in Spark program: warm-up, motor skills, games such as jump rope, walk, shoot the ball, aiming and throwing the ball into the basket and bowling, based on educational activities in the form of a game to investigate its effects on some neuropsychological variables. | The intervention with the Spark program appeared to have a significant effect on some motor and neuropsychological performances of children with DCD. Significant improvement in manual dexterity, aiming and grasping and balance. Minor change to the Threading Lace component. |
| 7. | Cheng et al., 2019, [48] | 3 months, 2 sessions per week for 40 min each time | ADHD, ASD and Dyslexia | Neuromuscular training (NMT) program with exercises focused on adaptive balance performance and leg muscle activation. | Short-term neuromuscular training (NMT) failed to improve adaptive balance performance and leg muscle activation times in children with DCD. |
| 8. | Yam et al., 2019 [49] | ADHD, ASD | The use of Kinesio Tape (KT) on dynamic balance of the trunk and related muscle activity of the lower limbs in children with DCD. | Kinesio Tape (KT): (1) It had a direct beneficial effect on dynamic balance performance. (2) Positive results in the control of neuromuscular balance. (3) Increase in leg muscle peak activation and time-to-peak muscle activation of the dominant lower limb. | |
| 9. | (A) Fong et al., 2016 [36] | 3 months, 2 times per week for 90 min each time | ADHD, Dyslexia and persons with possibility of existence, ASD | Comparison of two intervention programs: (1) FMPT (Functional Movement Power Training) dynamic training exercises were intended to improve the posture of muscle strength and the speed of contraction in the legs. (2) FMT (Functional Movement Training) program (training in a specific task with electromyographic (EMG) biofeedback for rehabilitation motor learning difficulties and enhancing neuroplasticity and balance performance). | The FMPT program was more effective than the conventional FMT program in enhancing neuromuscular performance in children with DCD. FMPT effective intervention to improve balance strategies, peak knee extension strength and time-to-peak knee flexion strength. |
| 10. | De Milander et al. (2015), [21] | 10 weeks, 2 times per week, 30 min each time | It was not reported | Sensory–motor program based on Kinder Kinetics. Sensory–motor coordination, bilaterally, dynamic–static balance exercises. | After the intervention, the balance showed a significant change. Manual dexterity and aiming and grasping showed no significant changes. These three components contributed to the overall score, which revealed a nonsignificant difference in overall motor skill levels. |
| 11. | Farhat et al. (2016) [35] | 8 weeks, 3 times per week, 60 min each time | It was not reported | Group intervention in a school context-oriented towards the task of training skills in the motor and physical abilities of children with DCD (practice: agility, aerobic power, neuromuscular strength training, flexibility, balance, ball balance, reaction speed, aerobic power, ball skill, strength coordination, ball handling). | The results showed that 10 children in the intervention group with DCD improved their performance on the MABC test. Additionally, the intervention group with DCD children improved significantly in manual dexterity, ball skills and balance. Significant performance improvements were also found in sprinting, lower extremity strength and power, writing quality, overall fine motor skills (in which no intervention was made) and speed. Overall gross motor coordination and physical ability improved. The children in the intervention group also seemed to enjoy the process. |
| 12. | Farhat et al., 2015, [50] | 8 weeks, 3 times per week, 60 min | It was not reported | Practice in the following skills: agility, aerobic power, neuromuscular strength training, flexibility, balance, balance ball skill, speed reaction speed, aerobic power-ball skill, strength coordination, ball handling). | The intervention group of children with DCD: (1) Have a delay in anaerobic threshold and an improvement in aerobic endurance and tolerance to physical activity. (2) Have improved walking distance (3) Have a higher maximum heart rate (4) Have reduced perceptual physical fatigue (exertion). |
| 13. | Saidmamatov et al., 2021, [22] | 10 weeks, 2 times per week for 45 min | It was not reported | Motor skills training program with exercises in the areas of manual dexterity, throwing–catching and balance. | In general, the quality of motor skills of children in the intervention group with DCD improved. Specifically, there was an improvement in manual dexterity, aiming/throwing, grasping and balance, as well as an improvement in the overall MABC-2 final score in the intervention group. The effectiveness of the intervention was similar for both sexes. |
| 14. | Navarro-Patón et al., 2021, [23] | 6 weeks, 1 session per week, for 40 min | It was not reported | Intervention program based on different motor skills (manual dexterity, aiming/throwing, catching and balance). | Postintervention measures showed improvements in manual dexterity, aiming/throwing and catching and balance, as well as the intervention group’s overall final score. |
| 15. | Giagazoglou et al., 2015, [14] | 12 weeks, 3 times per week, 45 min each time | It was not reported | Balance training program with balance exercises in circuit training, which also included exercises on the trampoline. | Significant performance improvement in all balance post-tests. Despite the fact that most of the exercises were performed with eyes open, the balance of the participants without visual control was also significantly improved. |
| 16. | Saidmamatov Ozodovich (2021), [24] | 10 weeks, 1 time per week, 45 min each time | It was not reported | Motor skills training program (exercises of fine and gross mobility, motor coordination, balance, difficulty of the proprioception, touch, kinesthetic sensation, relaxation). | Improvement in motor skills (relative to the factors of MABC-2 and the control group except for one child). |
| 17. | Dannenbaum et al., 2021, [34] | 5 days, 5 h each day | ADHD, language disorder (verbal apraxia, dysphasia), Anxiety Disorder, idiopathic quadriceps contraction, sleep apnea, epilepsy | Vestibular dysfunction rehabilitation camp in a hospital setting (Vestibular Rehabilitation) with rehabilitation exercises in the form of a game (Static–Dynamic balance, trunk muscle strength, gaze stability, coordination, multisensory integration). | The results showed that the intervention produced significant improvements in functional gait and gaze stability. Motor function, static balance and participation outcomes were unchanged. It is interesting to note that while camp counselors subjectively noted improved quality of movement, improved stability, reduced need for guidance/corrections, and enhanced independence in performing various activities, these improvements were not reflected in many measures. The scores in the measurements related to the participation appeared higher, though, after the intervention and in the measurement at the follow-up, but it did not significantly affect the participation of the children in their daily environment. Another positive outcome of the intervention was the new friendships and camaraderie that developed. |
| 18. | Yu et al., 2016, [9] | 6 weeks, 2 times per week for 35 min each time | It was not reported | Fundamental Movement Skills (FMS: running, jumping, catching, throwing, kicking) training on FMS proficiency, self-perceived physical ability, physical activity, and sleep disturbance in children with DCD. | Improvement in motor skills (jumping) and object control skills (grasping and kicking) of children with DCD. Their improvements in object control skills (catching and throwing) were maintained for at least 6 weeks. Improvement of self; children’s perceived physical ability with DCD regarding physical coordination, physical strength and fitness immediately after training. Children with DCD showed fewer sleep disturbances 6 weeks after the intervention. Participation in physical activity did not increase. |
| 19. | Kuijpers et al., 2019, [15] | 6 sessions, 2 times per week for 30 min each time | It was not reported | Task-oriented treadmill training with projected visual context (C-mill) (step adjustment exercises, obstacle avoidance, hitting, targets). | Significant improvement in complex gait adaptation tasks and maintenance of results after remeasurement 6 months later in treadmill step adaptation exercises. There was also a generalization of the results of the intervention even when there was no treadmill exercise and an improvement in gait, but a nonsignificant improvement in the obstacle course and the single run. |
| 20. | Tan et al., 2020, [8] | 13 weeks, 2 sessions for 90 min per week | At risk for osteoporosis | Multimodal exercise intervention for bone health (cardiovascular exercises, core strength and flexibility exercises, motor skills and postural skills, resistance training for the lower body, resistance training in general, Plyometrics, team games and partner games). | Effective intervention in the improvement in muscle and bone parameters (at the tibial site for bone mass, cortical area). Lower body fitness measures were significantly associated with improvements in parameters of bone health. The improvement in bone parameters was maintained for at least 3 months. |
| 21. | Hashemi et al., 2016, [28] | 8 weeks (24 sessions), 3 sessions per week for 60 min each time | It was not reported | Set of natural activities (set of physical exercises aimed at strengthening coordination, control, inhibition, response and reaction time). | Significant improvement in balance, bilateral coordination, response speed, visual–motor control, speed and dexterity of the upper limb. No significant changes were observed in the components (1) speed and dexterity and (2) strength. |
| 22 | Balayi and Sedaghati, 2021, [27] | 8 weeks, 3 sessions per week for 60 min each time | Intellectual Disability | Combination of physiotherapy exercises; hemsball. In motor skills, trunk stability exercises with coordination exercises in motor proficiency. | The intervention group improved in running speed, agility, balance, two-way coordination, strength, upper extremity coordination, response speed, motor–visual control, upper extremity agility and general fine and gross motor skills. |
| 23. | Fong et al., 2016, (2nd), [39] | 3 months, 2 sessions per week for 90 min each time | ADHD, Dyslexia, suspected ASD | Task-specific balance training in the form of functional movement in the form of an FMT program (two-legged balance on foam with electromyographic biofeedback, balance with one foot on the ground (alternate leg), walking in a straight line with raised heels, two-legged bounce, balance on a ball while the person is walking. | In general, task-specific balance training was found to marginally improve body–sensory function and somewhat improve the balance performance of children with DCD. Specifically, the FMT group showed greater improvements than the control group in the body–sensory ratio in 3 and 6 months, but within-group changes were not significant. The balance performance of the FMT group was significantly better than that of the control group in 3 and 6 months. |
| 24. | Damanpak and Sabzi, 2022, [33] | 8 weeks, 3 sessions per week, 45–60 min each session | It was not reported | Kinetic games to improve executive functions (coordination, balance, fine and gross mobility, perception, sensory–motor exercises). | Improvement in the executive functions of the intervention group, specifically the skills of attention, organization, inhibition, planning and decision-making. |
| 25. | Maharaj and Lallie, 2016, [30] | 8 weeks, 30 min per week | It was not reported | Intervention program with an emphasis on gross mobility exercises: trunk stability, strengthening, balance and coordination exercises (target throwing ball exercises with an emphasis on strength and coordination, mimicking sensory integration exercises). | Improvement in gross motor function. Improvement in M-ABC and DCDQ score. Some teachers’ ratings of the children’s motor skills were lower than those of the children’s parents. |
| 26. | Ma et al. (2018), [26] | 12 weeks, 1 session each week, 60 min each time and home physical activities 7 times per week | ADHD, ASD, Dyslexia | Taekwondo training intervention for skeletal development and motor performance (balance control and eye–hand coordination training. Mostly kicking and striking techniques were used). | Overall improvement in the skeletal development of the TKD group in the movement time of EHC (eye–hand coordination) in children with DCD. (1) Skeletal growth improved in both groups over time (the TKD group had a significant delay in skeletal growth at baseline compared to the control group). (2) Improvements in MABC scores were also observed in both groups over time. (3) Only the TKD group had a significant improvement in EHC (eye–hand coordination) movement time at 3 and 6 months. Both groups had general improvements in gross and fine motor skills over time (this may also be due to the maturation factor). In terms of static standing balance performance, surprisingly, neither group showed significant improvement over time. For motor performance, the factor of maturation may be more responsible. |
| 27. | Kane and Staples (2014), [25] | 7 weeks, 2 h each session, 3 times per week | ADHD, anxiety, in-toeing, low birth weight, premature birth, speech delay, average intellectual disability, delay in language expression, possible autism, apraxia of speech, abnormal brain development, epilepsy. | Group program of gross motor skills with an emphasis on the participation of parents in the performance of their children’s motor skills and physical activity (multidisciplinary program; aerobic and strength exercises and practice skills directly related to each child’s goals). | Positive effects on mobility. Parents’ satisfaction and perception of their child’s performance also improved. The majority of children also reported improved performance, at least on the targets. On average, moderate to vigorous physical activity improved by 10 min per day, although these gains were not significant. Time spent in sedentary activities was unchanged. |
| 28. | Jahanbakhsh et al., 2020, [37] | 8 weeks, 3 times per week, 45 min each time | It was not reported | Task-specific balance training in single-task and dual-task conditions for balance performance. (1) Single-task conditions: children had to maintain their balance while standing on one leg and maintain their balance while walking. (2) Dual-task conditions: similar to the single-task group program, with the exception that the children also had to perform cognitive tasks such as counting numbers. | Improvement in both groups’ static and dynamic balance, with the dual-task group having more improvement and the results remaining even two months after the program had been completed. Therefore, a dual-task training program that focuses on balance and cognitive tasks may improve children’s static and dynamic balance skills more than single-task training. |
| 29. | Kordi et al., 2016, [51] | 12 weeks, 2 sessions per week, 60 min each session | It was not reported | Program strength exercises for the improvement in static and dynamic balance. | Significant increase in muscle strength of children with DCD and improvement in their static balance performance. Exercises had no significant effect on dynamic balance. |
| 30. | Noordstar et al., 2017, [52] | 12 weeks, 1 time per week for 30 min | It was not reported | (1) Motor intervention (ball exercises, basketball), (2) motor intervention (ball exercises, basketball) | No differences were found between the intervention group and the care-as-usual group. The children improved their motor performance and increased their perceived athletic ability, their global self-esteem and perceived motor ability. The improvement was maintained at the repeat measurement 3 months after the intervention. |
| 31. | Caçola et al., 2016, [53] | 10 weeks, 1 time per week for 60 min | It was not reported | Group A: Task-oriented training. Group B: Basic motor skills training. | The children improved their motor skills after both programs, but: (1) After Program A, they showed higher anxiety and lower levels of enjoyment, even though parents noted an improvement in functioning rate and a decrease in peer problems. (2) After Program B, children’s anxiety levels decreased and parents noticed better control of their movements. |
| 32. | Mohamma et al., 2018, [44] | 8 weeks, 1 time per week | Depression, Anxiety disorder | Aerobic rhythmic training intervention program. | Improvement in motor skills of the intervention group, and a significant reduction in the levels of anxiety and depression of the intervention group. The intervention was fun and enjoyable for the participants of the intervention group. |
| 33. | Tamplain et al., 2020, [32] | 10 weeks, 1 time per week for 60 min | ADHD, Dyslexia, Dysgraphia, Obsessive Compulsive Disorder (OCD), Sensory Processing Disorder. | Collaborative motor exercises, motor coordination exercises, gross mobility exercises, fine motor improvement exercises, trunk stabilization exercises, and dynamic balance exercises. | Improvement in dynamic stabilization and trunk control and improvement in static and dynamic balance. |
| 34. | Zolghadr et al., 2019, [45] | 12 weeks, 3 times per week | It was not reported | Static and dynamic balance exercises. | Improvement in neuromuscular and bilateral coordination of the intervention group |
| 35. | Rezaei et al., 2016, [38] | 8 weeks, 3 times per week for 45 min | It was not reported | Static and dynamic balance exercises. | Significant improvement in the accuracy of bilateral upper extremity coordination in the intervention group and improvement in attention and concentration in the intervention group. |
| 36. | Norouzi et al., 2021, [54] | 4 weeks, 2 times per week for 40 min | It was not reported | Bilateral coordination exercises with QET (Quiet Eye Training) or TT (Traditional Training: flexions and extensions in in-phase and antiphase movements of the upper limbs). | Significant improvement in the accuracy of bilateral upper extremity coordination of children in the Quiet Eye intervention group compared to the Traditional Training intervention. |
| 37. | Liu et al., 2018, [38] | 3 weekly sessions | Neurological disabilities, motor disability. | Exercises on an ergometric stationary bike. | Improving endurance and reducing fatigue in adolescents with ADHD and increasing metabolic rate. Greater fatigue was observed during sessions in adolescents with DCD, which is useful for creating interventions for people with DCD. |
| 38. | Monastiridi et al., 2021, [55] | 12 weeks, 3 times per week For 60 min | It was not reported | Functional training program for core stabilization/strengthening (core, balance, strengthening exercises). | Significant improvements in motor performance, static and dynamic balance, abdominal muscle strength and endurance, and lower back and hamstring flexibility. Improvement in Body Mass Index (BMR), quality of life and functionality in the intervention group. |
| 39. | Wood et al., 2017, [56] | 4 weeks, 1 time per week for 60 min | It was not reported | (1) Quiet Eye Training group: focus on a target position before throwing, and observe the ball before serving. (2) Technical Training group: video instructions on throwing and serving phases. | Improving eye control and coordination of throwing and passing the ball in the QET (Quiet Eye Training) Group. Improving self-confidence, social skills and disposition for physical activity in the QET group. |
| 40. | Alagesan et al., 2020, [39] | 8 weeks, 3 times per week | Anxiety Disorder | Aerobic training (brisk walking, skipping rope, running, jogging, aerobic dance, hide and seek, walking). | Improving the quality of life, academic results, physical activity and functionality of people with DCD. Reduction in the increased level of anxiety of people with Anxiety Disorder. |
5. Case Control
5.1. First Case Control
5.2. Second Case Control
6. Conclusions, Discussion
6.1. Teaching Instructions and Educational Applications
6.2. Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hession, C.E.; Law Smith, M.J.; Watterson, D.; Oxley, N.; Murphy, B.A. The impact of equine therapy and an audio-visual approach emphasizing rhythm and beat perception in children with developmental coordination disorder. J. Altern. Complement. Med. 2019, 25, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Pérez, A.; Vicente-Nicolás, G.; Valero-García, A.V. Music, body movement, and dance intervention program for children with developmental coordination disorder. Psychol. Music 2020, 49, 1215–1225. [Google Scholar] [CrossRef]
- Ludyga, S.; Pühse, U.; Gerber, M.; Kamijo, K. How children with neurodevelopmental disorders can benefit from the neurocognitive effects of exercise. Neurosci. Biobehav. Rev. 2021, 127, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Ku, B. The effects of motor skill interventions on motor skills in children with developmental disabilities: A literature review. Asian J. Kinesiol. 2020, 22, 11–22. Available online: https://www.ajkinesiol.org/journal/view.php?number=481 (accessed on 8 October 2022). [CrossRef]
- Sung, M.C.; Ku, B.; Leung, W.; MacDonald, M. The effect of physical activity interventions on executive function among people with neurodevelopmental disorders: A meta-analysis. J. Autism Dev. Disord. 2021, 52, 1030–1050. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Du, W.; Ke, L.; Wang, Y.; Hua, J.; Duan, W.; Barnett, A.L. The prenatal, postnatal, neonatal, and family environmental risk factors for Developmental Coordination Disorder: A study with a national representative sample. Res. Dev. Disabil. 2020, 104, 1–9. Available online: https://www.sciencedirect.com/science/article/pii/S0891422220301293?via%3Dihub (accessed on 8 October 2022). [CrossRef]
- Dewey, D.; Bernier, F.P. The concept of atypical brain development in developmental coordination disorder (DCD)—A New Look. Curr. Dev. Disord. Rep. 2016, 3, 161–169. [Google Scholar] [CrossRef]
- Lee, D.; Psotta, R.; Vagaja, M. Motor skills interventions in children with developmental coordination disorder: A review study. Eur. J. Adapt. Phys. Act. 2016, 9, 20–29. [Google Scholar] [CrossRef]
- Τan, J.; Siafarikas, A.; Hands, B.; McIntyre, F.; Hart, N.; Rantalainen, T.; Chivers, P. Impact of a multimodal exercise program on tibial bone health in adolescents with development coordination disorder: An examination of feasibility and potential efficacy. J. Musculoskelet. Neuronal Interact. 2020, 20, 445–471. Available online: https://pubmed.ncbi.nlm.nih.gov/33265073/ (accessed on 31 May 2023).
- Yu, J.; Sit, C.H.; Burnett, A.; Capio, C.M.; Ha, A.S.; Huang, W.Y. Effects of fundamental movement skills training on children with developmental coordination disorder. Adapt. Phys. Act. Q. 2016, 33, 134–155. [Google Scholar] [CrossRef]
- Preston, N.; Magallón, S.; Hill, L.J.; Andrews, E.; Ahern, S.M.; Mon-Williams, M.A. Systematic review of high quality randomized controlled trials investigating motor skill programmes for children with developmental coordination disorder. Clin. Rehabil. 2017, 31, 857–870. [Google Scholar] [CrossRef] [PubMed]
- Engel, A.C.; Broderick, C.R.; van Doorn, N.; Hardy, L.L.; Parmenter, B.J. Exploring the relationship between fundamental motor skill interventions and physical activity levels in children: A systematic review and meta-analysis. Sport. Med. 2018, 8, 1845–1857. [Google Scholar] [CrossRef] [PubMed]
- Miyahara, M.; Lagisz, M.; Nakagawa, S.; Henderson, S.E. A narrative meta-review of a series of systematic and meta-analytic reviews on the intervention outcome for children with developmental co-ordination disorder. Child Care Health Dev. 2017, 43, 733–742. [Google Scholar] [CrossRef]
- Smits-Engelsman, B.; Vinçon, S.; Blank, R.; Quadrado, V.H.; Polatajko, H.; Wilson, P.H. Evaluating the evidence for motor-based interventions in developmental coordination disorder: A systematic review and meta-analysis. Res. Dev. Disabil. 2018, 74, 72–102. [Google Scholar] [CrossRef] [PubMed]
- Giagazoglou, P.; Sidiropoulou, M.; Mitsiou, M.; Arabatzi, F.; Kellis, E. Can balance trampoline training promote motor coordination and balance performance in children with developmental coordination disorder? Res. Dev. Disabil. 2015, 36, 13–19. [Google Scholar] [CrossRef]
- Kuijpers, R.; Smulders, E.; Groen, B.; Weerdesteyn, V.; van der Sanden, N. Task-oriented treadmill training improves gait adaptability in children with Developmental Coordination Disorder. Gait Posture 2019, 73, 58. [Google Scholar] [CrossRef]
- Cameron, K.L.; Albesher, R.A.; McGinley, J.L.; Allison, K.; Cheong, J.L.Y.; Spittle, A.J. Movement-based interventions for preschool-age children with, or at risk of, motor impairment: A systematic review. Dev. Med. Child Neurol. 2020, 62, 290–296. [Google Scholar] [CrossRef]
- Kim, M.J.; Choi, J.S. A systematic review of developmental coordination disorders in South Korea: Evaluation and intervention. J. Korean Soc. Sens. Integr. Ther. 2021, 19, 69–82. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 89, 105906. Available online: https://www.bmj.com/content/bmj/372/bmj.n71.full.pdf (accessed on 29 March 2021).
- Cresswell, J.; Cresswell, D. Research Design Qualitative, Quantitative and Mixed Methods Approaches; Propompos: Athens, Greece, 2019; p. 64. ISBN 97861895036508. (In Greek) [Google Scholar]
- Papanastasiou, K. Methodology of Educational Research; Theo Press LTD: Nicosia, Cyprus, 1996; p. 18. ISBN 9963-8176-0-2. (In Greek) [Google Scholar]
- De Milander, M.; Coetzee, F.F.; Venter, A. Perceptual-motor intervention for developmental coordination disorder in Grade 1 children. South Afr. J. Res. Sport Phys. Educ. Recreat. 2015, 37, 15–32. [Google Scholar]
- Saidmamatov, O.; Raximov, Q.; Rodrigues, P.; Vasconcelos, O. A ten-week motor skills training program increases motor competence in children with developmental coordination disorder. Children 2021, 8, 1147. [Google Scholar] [CrossRef]
- Navarro-Patón, R.; Martín-Ayala, J.L.; Martí González, M.; Hernández, A.; Mecías-Calvo, M. Effect of a 6-week physical education intervention on motor competence in pre-school children with developmental coordination disorder. J. Clin. Med. 2021, 10, 1936. [Google Scholar] [CrossRef] [PubMed]
- Saidmamatov, O.; Ozodovich, R.Q. Improving the motor skills of children with developmental coordination disorder. J. La Edusci. 2021, 2, 1–5. [Google Scholar] [CrossRef]
- Kane, K.J.; Staples, K.L. A group motor skills program for children with coordination difficulties: Effect on fundamental movement skills and physical activity participation. Phys. Occup. Ther. Pediatr. 2014, 36, 28–45. [Google Scholar] [CrossRef] [PubMed]
- Ma, A.W.W.; Fong, S.S.M.; Guo, X.; Liu, K.P.Y.; Fong, D.Y.T.; Bae, Y.H.; Yuen, L.; Cheng, Y.T.Y.; Tsang, W.W.N. Adapted Taekwondo training for prepubertal children with developmental coordination disorder: A randomized, controlled trial. Sci. Rep. 2018, 8, 10330. [Google Scholar] [CrossRef]
- Balayi, E.; Sedaghati, P. The effect of combined core stability and coordination exercises on the motor skills of intellectual disability with DCD. Phys. Treat. Specif. Phys. Ther. J. 2021, 11, 249–260. [Google Scholar] [CrossRef]
- Hashemi, A.; Sheikh, M.; Hemayat-Talab, R. The effect of regular exercise on motor function in children with developmental coordination disorder. Int. J. Sport Stud. 2016, 6, 254–260. [Google Scholar]
- Heus, I.; Weezenberg, D.; Severijnen, S.; Vliet Vlieland, T.; van der Holst, M. Measuring treatment outcome in children with developmental coordination disorder; responsiveness of six outcome measures. Disabil. Rehabil. 2020, 44, 1023–1034. [Google Scholar] [CrossRef]
- Maharaj, S.S.; Lallie, R. Does a physiotherapy programme of gross motor training influence motor function and activities of daily living in children presenting with developmental coordination disorder? S. Afr. J. Physiother. 2016, 72, a304. [Google Scholar] [CrossRef]
- Zwicker, J.G.; Rehal, H.; Sodhi, S.; Karkling, M.; Paul, A.; Hilliard, M.; Jarus, T. Effectiveness of a summer camp intervention for children with developmental coordination disorder. Phys. Occup. Ther. Pediatr. 2014, 35, 163–177. [Google Scholar] [CrossRef]
- Tamplain, P.; Sherrod, G.M.; Fuchs, C.; Miller, H.L. Preliminary improvements in dynamic postural control after a group-based intervention program for children with developmental coordination disorder: A brief report. Dev. Neurorehabilit. 2021, 24, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Damanpak, S.; Sabzi, H.A. The effect of selected motor games on executive functions of children with developmental coordination disorders. Int. J. Pediatr. 2022, 10, 15449–15459. [Google Scholar] [CrossRef]
- Dannenbaum, E.; Bégin, C.L.; Daigneault-Bourgeois, L.; Kwon Pak Yin, N.; Laferrière-Trudeau, C.; Mazer, B.; Moreau, V.; Salvo, L.; Villeneuve, M.; Lamontagne, A. Feasibility and preliminary effects of a 1-week vestibular rehabilitation day camp in children with developmental coordination disorder. Phys. Occup. Ther. Pediatr. 2021, 42, 62–79. [Google Scholar] [CrossRef] [PubMed]
- Farhat, F.; Hsairi, I.; Baati, H.; Smits-Engelsman, B.; Masmoudi, K.; Mchirgui, R.; Triki, C.; Moalla, W. The effect of a motor skills training program in the improvement of practiced and non-practiced tasks performance in children with developmental coordination disorder (DCD). Hum. Mov. Sci. 2016, 46, 10–22. [Google Scholar] [CrossRef]
- Fong, S.S.; Guo, X.; Cheng, Y.T.; Liu, K.P.; Tsang, W.W.; Yam, T.T.; Chung, L.M.; Macfarlane, D.J. A Novel balance training program for children with developmental coordination disorder. Medicine 2016, 95, e3492. [Google Scholar] [CrossRef]
- Jahanbakhsh, H.; Sohrabi, M.; Saberi Kakhki, A.; Khodashenas, E. The effect of task-specific balance training program in dual-task and single-task conditions on balance performance in children with developmental coordination disorder. Acta Gymnica 2020, 50, 28–37. [Google Scholar] [CrossRef]
- Liu, F.; Morris, M.; Hicklen, L.; Izadi, H.; Dawes, H. The impact of high and low-intensity exercise in adolescents with movement impairment. PLoS ONE 2018, 13, e0195944. [Google Scholar] [CrossRef]
- Alagesan, B.; Akahaya, J.; Rajameena, R.; Brite Saghaya Rayna, A. Effect of aerobic exercise training on anxiety in children with developmental coordination disorder. Biomedicine 2021, 40, 535–538. [Google Scholar] [CrossRef]
- Mohammadi Oranghi, B.; Yaali, R.; Shahrzad, N. The effect of eight weeks aerobic rhythmic exercises with music on motor proficiency, anxiety and depression in children with developmental coordination disorder. Mot. Behav. 2018, 9, 57–70. [Google Scholar] [CrossRef]
- Zolghadr, H.; Sedaghati, P.; Daneshmandi, H. The effect of selected balance/corrective exercises on the balance performance of mentally-retarded students with developmental coordination disorder. Phys. Treat. Specif. Phys. Ther. J. 2019, 9, 23–30. [Google Scholar] [CrossRef]
- Sit, C.H.; Yu, J.J.; Wong, S.H.; Capio, C.M.; Masters, R. A school-based physical activity intervention for children with developmental coordination disorder: A randomized controlled trial. Res. Dev. Disabil. 2019, 89, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Rahman Gholhaki, M.; Molanorozi, K.; Ghasemi, A. The effect of selected motor program on neuropsychological variability and motor function at children with developmental coordination disorder. Int. J. Mot. Control Learn. 2021, 3, 33–45. [Google Scholar] [CrossRef]
- Miyahara, M. Physical Literacy as a Framework of assessment and intervention for children and youth with developmental coordination disorder: A narrative critical review of conventional practice and proposal for future directions. Int. J. Environ. Res. Public Health 2020, 12, 4313. [Google Scholar] [CrossRef]
- Monastiridi, S.; Katartzi, E.; Kourtessis, T.; Vlachopoulos, S. A core stabilization program improves motor performance and health-related quality of life in adolescents with motor difficulties. Health Fit. J. Can. 2021, 14, 3–24. [Google Scholar] [CrossRef]
- Farhat, F.; Masmoudi, K.; Hsairi, I.; Smits-Engelsman, B.C.M.; Mchirgui, R.; Triki, C.; Moalla, W. The effects of 8 weeks of motor skill training on cardiorespiratory fitness and endurance performance in children with developmental coordination disorder. Appl. Physiol. Nutr. Metab. 2015, 45, 1269–1278. [Google Scholar] [CrossRef]
- Cheng, Y.T.; Wong, T.K.; Tsang, W.W.; Schooling, C.M.; Fong, S.S.; Fong, D.Y.; Gao, Y.; Chung, J.W. Neuromuscular training for children with developmental coordination disorder. Medicine 2019, 98, e17946. [Google Scholar] [CrossRef]
- Kordi, H.; Sohrabi, M.; Saberi Kakhki, A.; Attarzadeh Hossini, S.R. The effect of strength training based on process approach intervention on balance of children with developmental coordination disorder. Arc. Argent Pediatr. 2016, 114, 526–533. [Google Scholar] [CrossRef]
- Wood, G.; Miles, C.A.; Coyles, G.; Alizadehkhaiyat, O.; Vine, S.J.; Vickers, J.N.; Wilson, M.R. A randomized controlled trial of a group-based gaze training intervention for children with developmental coordination disorder. PLoS ONE 2017, 12, e0171782. [Google Scholar] [CrossRef]
- Noordstar, J.J.; van der Net, J.; Voerman, L.; Helders, P.J.; Jongmans, M.J. The effect of an integrated perceived competence and motor intervention in children with developmental coordination disorder. Res. Dev. Disabil. 2017, 60, 162–175. [Google Scholar] [CrossRef] [PubMed]
- Rezaei, S.; Arabameri, E.; Sohrabi, M. Examination of the impact of an eight-week exclusive exercise on the balance of children with developmental coordination disorders. Sci. J. Rehabil. Med. 2016, 5, 57–64. [Google Scholar] [CrossRef]
- Norouzi Seyed Hosseini, R.; Norouzi, E.; Soleymani, M. Effects of quiet eye training on performance of bimanual coordination in children with DCD. Iran. J. Child Neurol. 2021, 15, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Lucas, B.R.; Elliott, E.J.; Coggan, S.; Pinto, R.Z.; Jirikowic, T.; McCoy, S.W.; Latimer, J. Interventions to improve gross motor performance in children with neurodevelopmental disorders: A meta-analysis. BMC Pediatr. 2016, 16, 193. [Google Scholar] [CrossRef] [PubMed]
- Caçola, P.M.; Ibana, M.; Romero, M.; Chuang, J. The effectiveness of a group motor skill intervention program in children with developmental coordination disorder: Program frequency matters. Internet J. Allied Health Sci. Pract. 2016, 14, 4. [Google Scholar] [CrossRef]
- Fong, S.S.; Guo, X.; Cheng, Y.T.; Liu, K.P.; Tsang, W.W.; Yam, T.T.; Chung, L.M.; Macfarlane, D.J. A task-specific balance training improves the sensory organisation of balance control in children with developmental coordination disorder: A randomised controlled trial. Sci. Rep. 2016, 6, 20945. [Google Scholar] [CrossRef]
- Ilana, S.D.O.; Dayana, D.S.O.; Julianna, D.A.G.; Beatriz, M.R.; Silvia, W.S. Effectiveness of motor intervention on children with Developmental Coordination Disorder (DCD): A systematic review. J. Phys. Educ. Sport Manag. 2017, 3, 32–40. [Google Scholar] [CrossRef]
- Yam, T.T.T.; Or, P.P.L.; Ma, A.W.W.; Fong, S.S.M.; Wong, M.S. Effect of kinesio taping on Y-balance test performance and the associated leg muscle activation patterns in children with developmental coordination disorder: A randomized controlled trial. Gait Posture 2019, 68, 388–396. [Google Scholar] [CrossRef]

| Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Participants | Studies for children and adolescents from 4 to 18 years of age with DCD | Studies with adults over 18 years of age |
| Physical Activity Intervention Duration Frequency | Studies with sport activities, martial arts, aerobic exercises, swimming, trampoline, etc. studies on interventions for children with DCD but also with neurodevelopmental disorders (ASD, ADHD, cerebral palsy, mental retardation). | Studies on interventions in children with neurodevelopmental disorders (ASD, ADHD, cerebral palsy, mental retardation) and not refer to DCD. Doctoral theses, postgraduate theses and conference proceedings. |
| Comorbidity | ||
| Outcomes | Assessment positive or negative | Doctoral theses, postgraduate theses and conference proceedings |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaragas, H.; Fragkomichelaki, O.; Geitona, M.; Sofologi, M.; Papantoniou, G.; Sarris, D.; Pliogou, V.; Charmpatsis, C.; Papadimitropoulou, P. The Effects of Physical Activity in Children and Adolescents with Developmental Coordination Disorder. Neurol. Int. 2023, 15, 804-820. https://doi.org/10.3390/neurolint15030051
Zaragas H, Fragkomichelaki O, Geitona M, Sofologi M, Papantoniou G, Sarris D, Pliogou V, Charmpatsis C, Papadimitropoulou P. The Effects of Physical Activity in Children and Adolescents with Developmental Coordination Disorder. Neurology International. 2023; 15(3):804-820. https://doi.org/10.3390/neurolint15030051
Chicago/Turabian StyleZaragas, Harilaos, Olga Fragkomichelaki, Marina Geitona, Maria Sofologi, Georgia Papantoniou, Dimitrios Sarris, Vassiliki Pliogou, Christos Charmpatsis, and Panagoula Papadimitropoulou. 2023. "The Effects of Physical Activity in Children and Adolescents with Developmental Coordination Disorder" Neurology International 15, no. 3: 804-820. https://doi.org/10.3390/neurolint15030051
APA StyleZaragas, H., Fragkomichelaki, O., Geitona, M., Sofologi, M., Papantoniou, G., Sarris, D., Pliogou, V., Charmpatsis, C., & Papadimitropoulou, P. (2023). The Effects of Physical Activity in Children and Adolescents with Developmental Coordination Disorder. Neurology International, 15(3), 804-820. https://doi.org/10.3390/neurolint15030051