Management of Phantom Limb Pain through Thalamotomy of the Centro-Median Nucleus
Abstract
:1. Introduction
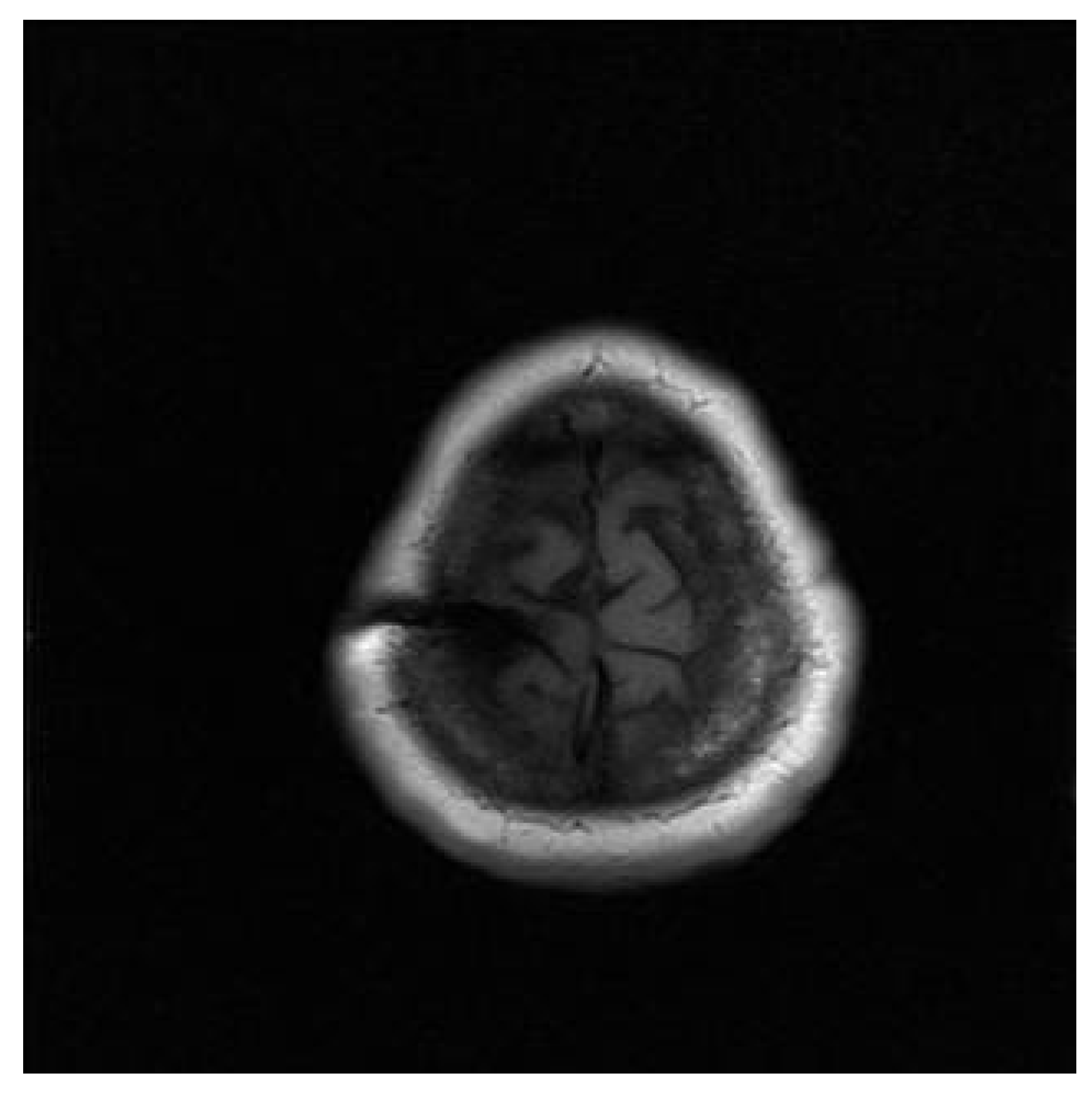
2. Case Presentation
Surgical Technique
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sherman, R.A.; Sherman, C.J.; Parker, L. Chronic Phantom and Stump Pain among American Veterans: Results of a Survey. Pain 1984, 18, 83–95. [Google Scholar] [CrossRef]
- Hsu, E.; Cohen, S.P. Postamputation Pain: Epidemiology, Mechanisms, and Treatment. J. Pain Res. 2013, 6, 121–136. [Google Scholar] [CrossRef] [Green Version]
- Ephraim, P.L.; Wegener, S.T.; MacKenzie, E.J.; Dillingham, T.R.; Pezzin, L.E. Phantom Pain, Residual Limb Pain, and Back Pain in Amputees: Results of a National Survey. Arch. Phys. Med. Rehabil. 2005, 86, 1910–1919. [Google Scholar] [CrossRef] [PubMed]
- Harahap, Z.C.S.; Amin, M.M.; Effendy, E. Phantom Pain Limb: A Case Report in a Soldier—Theory and Therapy. Open Access Maced. J. Med. Sci. 2019, 7, 2691–2694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinstein, S.M. Phantom Limb Pain And Related Disorders. Neurol. Clin. 1998, 16, 919–935. [Google Scholar] [CrossRef]
- Rudy, T.E.; Lieber, S.J.; Boston, J.R.; Gourley, L.M.; Baysal, E. Psychosocial Predictors of Physical Performance in Disabled Individuals with Chronic Pain. Clin. J. Pain 2003, 19, 18–30. [Google Scholar] [CrossRef] [PubMed]
- Splavski, B.; Rotim, K.; Boop, F.A.; Gienapp, A.J.; Arnautović, K.I. Ambroise Paré: His Contribution to the Future Advancement of Neurosurgery and the Hardships of His Times Affecting His Life and Brilliant Career. World Neurosurg. 2020, 134, 233–239. [Google Scholar] [CrossRef]
- Intiso, D.; Basciani, M.; Santamato, A.; Intiso, M.; Di Rienzo, F. Botulinum Toxin Type A for the Treatment of Neuropathic Pain in Neuro-Rehabilitation. Toxins 2015, 7, 2454–2480. [Google Scholar] [CrossRef] [Green Version]
- Kline, D.G. Silas Weir Mitchell and “The Strange Case of George Dedlow”. Neurosurg. Focus 2016, 41, E5. [Google Scholar] [CrossRef]
- Klifto, K.M.; Dellon, A.L. Silas Weir Mitchell, MD, LLD, FRC: Neurological Evaluation and Rehabilitation of the Injured Upper Extremity. Hand 2021, 16, 128–133. [Google Scholar] [CrossRef] [Green Version]
- Srivastava, D. Chronic Post-Amputation Pain: Peri-Operative Management—Review. Br. J. Pain 2017, 11, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Buchheit, T.; Van de Ven, T.; Hsia, H.-L.J.; McDuffie, M.; MacLeod, D.B.; White, W.; Chamessian, A.; Keefe, F.J.; Buckenmaier, C.T.; Shaw, A.D. Pain Phenotypes and Associated Clinical Risk Factors Following Traumatic Amputation: Results from Veterans Integrated Pain Evaluation Research (VIPER). Pain Med. 2016, 17, 149–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chahine, L.; Kanazi, G. Phantom Limb Syndrome: A Review. Middle East. J. Anaesthesiol. 2007, 19, 345–355. [Google Scholar] [PubMed]
- Dijkstra, P.U.; Geertzen, J.H.B.; Stewart, R.; van der Schans, C.P. Phantom Pain and Risk Factors: A Multivariate Analysis. J. Pain Symptom Manag. 2002, 24, 578–585. [Google Scholar] [CrossRef]
- Flor, H.; Elbert, T.; Knecht, S.; Wienbruch, C.; Pantev, C.; Birbaumer, N.; Larbig, W.; Taub, E. Phantom-Limb Pain as a Perceptual Correlate of Cortical Reorganization Following Arm Amputation. Nature 1995, 375, 482–484. [Google Scholar] [CrossRef]
- Collins, K.L.; Russell, H.G.; Schumacher, P.J.; Robinson-Freeman, K.E.; O’Conor, E.C.; Gibney, K.D.; Yambem, O.; Dykes, R.W.; Waters, R.S.; Tsao, J.W. A Review of Current Theories and Treatments for Phantom Limb Pain. J. Clin. Investig. 2018, 128, 2168–2176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sherman, R.A.; Sherman, C.J.; Gall, N.G. A Survey of Current Phantom Limb Pain Treatment in the United States. Pain 1980, 8, 85–99. [Google Scholar] [CrossRef]
- Makin, T.R.; Flor, H. Brain (Re)Organisation Following Amputation: Implications for Phantom Limb Pain. Neuroimage 2020, 218, 116943. [Google Scholar] [CrossRef]
- Makin, T.R.; Scholz, J.; Henderson Slater, D.; Johansen-Berg, H.; Tracey, I. Reassessing Cortical Reorganization in the Primary Sensorimotor Cortex Following Arm Amputation. Brain 2015, 138, 2140–2146. [Google Scholar] [CrossRef] [Green Version]
- Flor, H.; Nikolajsen, L.; Staehelin Jensen, T. Phantom Limb Pain: A Case of Maladaptive CNS Plasticity? Nat. Rev. Neurosci. 2006, 7, 873–881. [Google Scholar] [CrossRef]
- Flor, H. Phantom-Limb Pain: Characteristics, Causes, and Treatment. Lancet Neurol. 2002, 1, 182–189. [Google Scholar] [CrossRef]
- Bittar, R.G.; Otero, S.; Carter, H.; Aziz, T.Z. Deep Brain Stimulation for Phantom Limb Pain. J. Clin. Neurosci. 2005, 12, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Jerath, R.; Crawford, M.W.; Jensen, M. Etiology of Phantom Limb Syndrome: Insights from a 3D Default Space Consciousness Model. Med. Hypotheses 2015, 85, 153–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Subedi, B.; Grossberg, G.T. Phantom Limb Pain: Mechanisms and Treatment Approaches. Pain Res. Treat. 2011, 2011, 864605. [Google Scholar] [CrossRef]
- Aydemir, K.; Demir, Y.; Güzelküçük, Ü.; Tezel, K.; Yilmaz, B. Ultrasound Findings of Young and Traumatic Amputees with Lower Extremity Residual Limb Pain in Turkey. Am. J. Phys. Med. Rehabil. 2017, 96, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Borghi, B.; D’Addabbo, M.; White, P.F.; Gallerani, P.; Toccaceli, L.; Raffaeli, W.; Tognù, A.; Fabbri, N.; Mercuri, M. The Use of Prolonged Peripheral Neural Blockade after Lower Extremity Amputation: The Effect on Symptoms Associated with Phantom Limb Syndrome. Anesth. Analg. 2010, 111, 1308–1315. [Google Scholar] [CrossRef]
- Wu, H.; Sultana, R.; Taylor, K.B.; Szabo, A. A Prospective Randomized Double-Blinded Pilot Study to Examine the Effect of Botulinum Toxin Type A Injection versus Lidocaine/Depomedrol Injection on Residual and Phantom Limb Pain: Initial Report. Clin. J. Pain 2012, 28, 108–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levendoglu, F.; Ogün, C.O.; Ozerbil, O.; Ogün, T.C.; Ugurlu, H. Gabapentin Is a First Line Drug for the Treatment of Neuropathic Pain in Spinal Cord Injury. Spine 2004, 29, 743–751. [Google Scholar] [CrossRef]
- Moore, A.; Derry, S.; Wiffen, P. Gabapentin for Chronic Neuropathic Pain. JAMA 2018, 319, 818–819. [Google Scholar] [CrossRef]
- Alviar, M.J.M.; Hale, T.; Lim-Dungca, M. Pharmacologic Interventions for Treating Phantom Limb Pain. Cochrane Database Syst. Rev. 2016, 2016, CD006380. [Google Scholar] [CrossRef]
- Vaso, A.; Adahan, H.-M.; Gjika, A.; Zahaj, S.; Zhurda, T.; Vyshka, G.; Devor, M. Peripheral Nervous System Origin of Phantom Limb Pain. Pain 2014, 155, 1384–1391. [Google Scholar] [CrossRef]
- Hou, S.; Kemp, K.; Grabois, M. A Systematic Evaluation of Burst Spinal Cord Stimulation for Chronic Back and Limb Pain. Neuromodulation 2016, 19, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Deer, T.R.; Mekhail, N.; Provenzano, D.; Pope, J.; Krames, E.; Leong, M.; Levy, R.M.; Abejon, D.; Buchser, E.; Burton, A.; et al. The Appropriate Use of Neurostimulation of the Spinal Cord and Peripheral Nervous System for the Treatment of Chronic Pain and Ischemic Diseases: The Neuromodulation Appropriateness Consensus Committee. Neuromodulation 2014, 17, 515–550. [Google Scholar] [CrossRef] [PubMed]
- Krushelnytskyy, M.D.; Carlstrom, L.P.; Klassen, B.T.; Lundstrom, B.N.; Paek, S.B.; Lavrov, I.A.; Stead, S.M.; Sandroni, P.; Lee, K.H. Chronic Subdural Cortical Stimulation for Phantom Limb Pain: Report of a Series of Two Cases. Acta Neurochir. 2019, 161, 925–934. [Google Scholar] [CrossRef] [PubMed]
- Sokal, P.; Harat, M.; Zieliński, P.; Furtak, J.; Paczkowski, D.; Rusinek, M. Motor Cortex Stimulation in Patients with Chronic Central Pain. Adv. Clin. Exp. Med. 2015, 24, 289–296. [Google Scholar] [CrossRef] [Green Version]
- Cárdenas, K.; Aranda, M. Psychotherapies for the Treatment of Phantom Limb Pain. Rev. Colomb Psiquiatr. 2017, 46, 178–186. [Google Scholar] [CrossRef]
- Barbin, J.; Seetha, V.; Casillas, J.M.; Paysant, J.; Pérennou, D. The Effects of Mirror Therapy on Pain and Motor Control of Phantom Limb in Amputees: A Systematic Review. Ann. Phys. Rehabil. Med. 2016, 59, 270–275. [Google Scholar] [CrossRef]
- Niizuma, H.; Kwak, R.; Ikeda, S.; Ohyama, H.; Suzuki, J.; Saso, S. FoIIow-Up Results of Centromedian Thalamotomy for Central Pain. Stereotact. Funct. Neurosurg. 1982, 45, 324–325. [Google Scholar] [CrossRef]
- Urgosik, D.; Liscak, R. Medial Gamma Knife Thalamotomy for Intractable Pain. J. Neurosurg. 2018, 129, 72–76. [Google Scholar] [CrossRef]
- Franzini, A.; Rossini, Z.; Moosa, S.; Tropeano, M.P.; Milani, D.; Attuati, L.; Clerici, E.; Navarria, P.; Pessina, F.; Picozzi, P. Medial Thalamotomy Using Stereotactic Radiosurgery for Intractable Pain: A Systematic Review. Neurosurg. Rev. 2021, 1–10. [Google Scholar] [CrossRef]
- Prantl, L.; Schreml, S.; Heine, N.; Eisenmann-Klein, M.; Angele, P. Surgical Treatment of Chronic Phantom Limb Sensation and Limb Pain after Lower Limb Amputation. Plast Reconstr. Surg. 2006, 118, 1562–1572. [Google Scholar] [CrossRef] [PubMed]
- Deer, T.R.; Stewart, C.D. Complications of Spinal Cord Stimulation: Identification, Treatment, and Prevention. Pain Med. 2008, 9, S93–S101. [Google Scholar] [CrossRef]
- Smith, Y.; Raju, D.; Nanda, B.; Pare, J.-F.; Galvan, A.; Wichmann, T. The Thalamostriatal Systems: Anatomical and Functional Organization in Normal and Parkinsonian States. Brain Res. Bull. 2009, 78, 60–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez de la Torre, R.A.; Rodríguez Hernández, J.J.; Al-Ramadan, A.; Gharaibeh, A. Management of Phantom Limb Pain through Thalamotomy of the Centro-Median Nucleus. Neurol. Int. 2021, 13, 587-593. https://doi.org/10.3390/neurolint13040058
Pérez de la Torre RA, Rodríguez Hernández JJ, Al-Ramadan A, Gharaibeh A. Management of Phantom Limb Pain through Thalamotomy of the Centro-Median Nucleus. Neurology International. 2021; 13(4):587-593. https://doi.org/10.3390/neurolint13040058
Chicago/Turabian StylePérez de la Torre, Ramiro A., Job J. Rodríguez Hernández, Ali Al-Ramadan, and Abeer Gharaibeh. 2021. "Management of Phantom Limb Pain through Thalamotomy of the Centro-Median Nucleus" Neurology International 13, no. 4: 587-593. https://doi.org/10.3390/neurolint13040058
APA StylePérez de la Torre, R. A., Rodríguez Hernández, J. J., Al-Ramadan, A., & Gharaibeh, A. (2021). Management of Phantom Limb Pain through Thalamotomy of the Centro-Median Nucleus. Neurology International, 13(4), 587-593. https://doi.org/10.3390/neurolint13040058





