Abstract
The severity of Parkinson’s disease (PD) is developed by multifactorial factors. Falls can worsen disease severity. We previously found that frontal assessment battery (FAB) score was associated with a higher risk of future falls. This eight-year follow-up study aimed to verify whether factors including low FAB score can be the risk of PD progression based on the Hoehn and Yahr scale. In total, 95 patients were initially enrolled in this research and 45 were included in the final follow-up. Then, the cohort was classified into patients with and without disease progression, defined by upgrade of Hoehn-Yahr stage. Differences in clinical characteristics between patients with disease progression and those without were evaluated using the Mann–Whitney U test. Eighteen independent variables were evaluated via a univariate logistic regression analysis. Of the 45 patients enrolled, 32 had disease progression and 13 had no progression. Age (p = 0.033), BFI score (p = 0.003), Zung self-rating depression (p = 0.011), and anxiety scale (p = 0.026) were significantly increased in patients who had disease progression than those with no disease progression. On multivariate logistic regression analysis, brief fatigue inventory (BFI) score (OR = 1.048, p = 0.045, 95% CI = 1.001–1.098) was significantly related to disease progression. All BFI subscores related to general fatigue. Fatigue could predict the progression of motor dysfunction severity over a longitudinal duration in patients with PD with disease progression, having declining physical and mental fatigue.
1. Introduction
Disease severity of Parkinson’s disease (PD) is developed by multifactorial factors. Falls can worsen disease severity. We previously found that slow gait with freezing is associated with a risk for future falls, as assessed using our originally designed, sudden narrowed path [1]. During the two-year course, this cohort had a lower frontal assessment battery (FAB) score, which was closely correlated with slow gait with freezing, and it could be a predictor of a higher risk of falling in 30 patients with Hoehn and Yahr stage III PD [2]. To determine the risk of future falls, we have previously investigated 100 patients with PD, including this cohort. Results showed that the low FAB score and a history of falls within the last six months were associated with a higher risk of future falls [3]. This finding can give rise to an open question of whether factors including low FAB score can be predictors of PD severity during a longitudinal follow-up period. We assessed 100 patients during an eight-year follow-up to determine the predictors of PD progression.
2. Methods
Methods used in the present study were the same as our previous study [3]. This study included 100 consecutive patients who fulfilled the UK PD Society Brain Bank criteria [4]. In addition, no patient had the following conditions: possible or probable multiple system atrophy per the Gilman criteria [5] and progressive supranuclear palsy per the National Institute of Neurologic Disorders and Stroke-SPSP diagnostic criteria [6]. No patient had any other form of parkinsonism, such as vascular parkinsonism, large vessel disease, infarction, or tumors on magnetic resonance imaging and evidence of psychosis, epilepsy, a history of stroke, transient ischemic attacks, uncompensated heart failure, severe pulmonary problems, or a history of surgical intervention like deep brain stimulation surgery. All patients could follow our instructions. All patients were evaluated upon enrollment using the following scales: scores on parts I, II, III, and IV of the unified Parkinson’s disease rating scale (UPDRS) [7], Hoehn-Yahr stage [8], mini-mental status examination (MMSE), FAB, brief fatigue inventory (BFI) [9], Zung self-rating depression and anxiety scales, Parkinson’s disease sleep scale (PDSS), and Tinetti balance and gait assessment [10]. The history of falls during the preceding 6 months was ascertained at enrollment. The daily dose of antiparkinsonian medications was converted into the equivalent dose of levodopa per previous studies [3,11,12]. Disease progression was defined by upgrade of Hoehn-Yahr stage for 8 years.
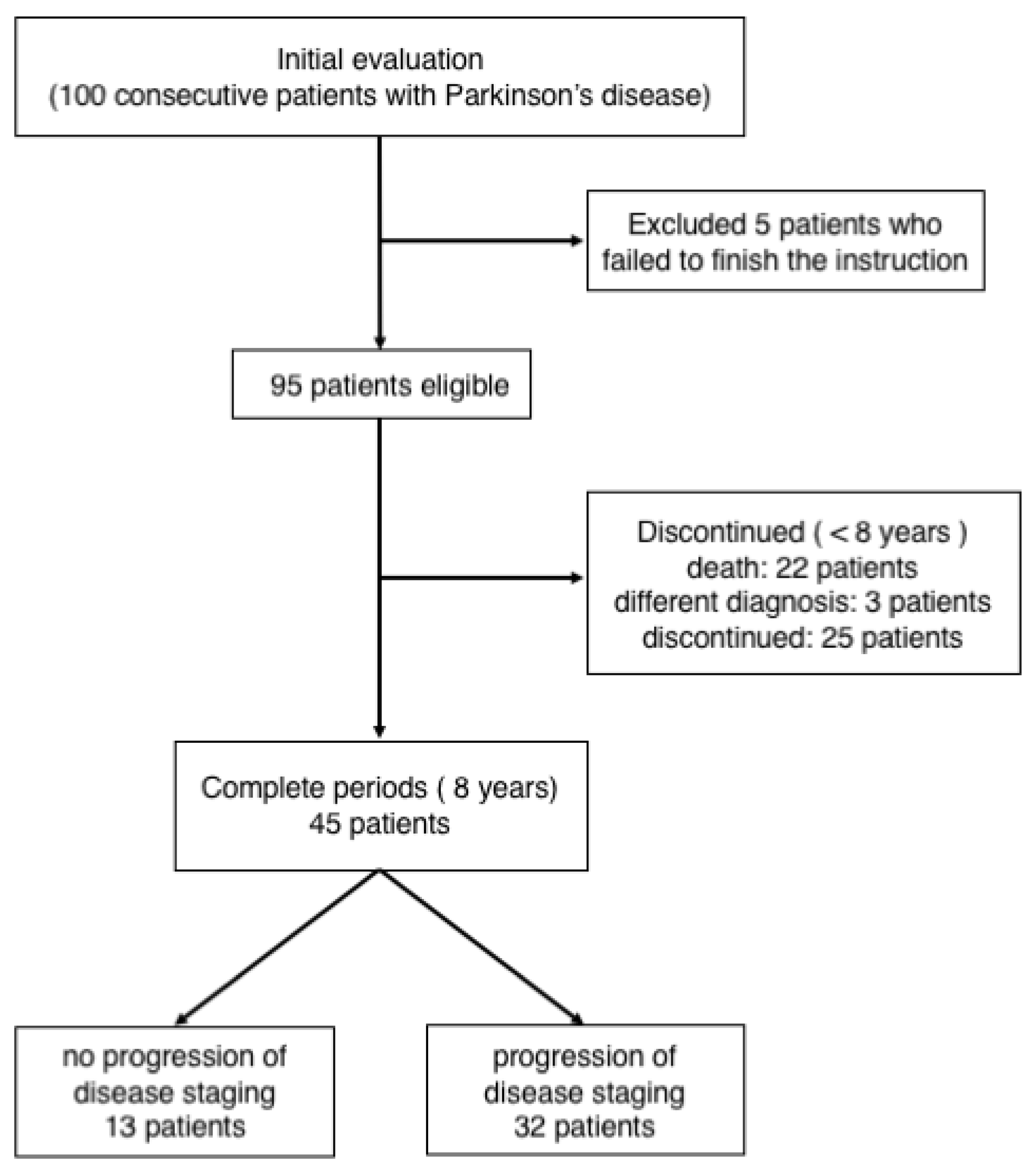
All the 95 patients with PD (Figure 1) registered for the study. These patients visited our hospital every 1–3 months during the 8-year follow-up. During the follow-up, 22 patients died, and 25 patients who required hospitalization and were transferred to other hospitals or did not return to our hospital were excluded from the study. In addition, three patients were eventually diagnosed as having other diseases (normal pressure hydrocephalus in one and progressive supranuclear palsy–parkinsonism in two). The remaining 45 patients were included in data analysis. The study protocol was approved by the Medical Ethics Committee of Nara Medical University.
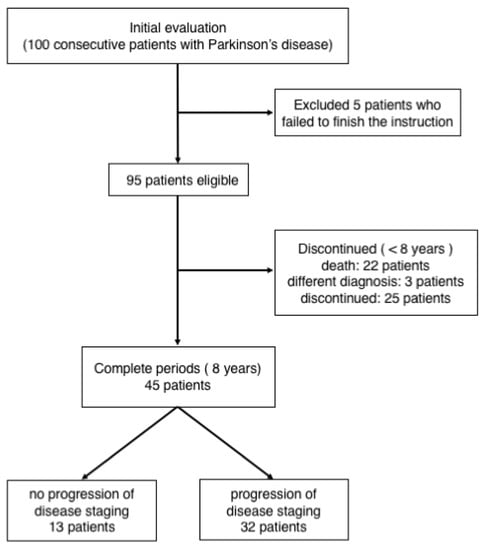
Figure 1.
Patient selection procedure.
Statistical Analysis
The statistical significance of differences in clinical characteristics between patients with and without disease progression defined by a change of Hoehn-Yahr stage was evaluated using the Mann–Whitney test. The disease progression was coded as objective variable (present = 1). Overall, the following 18 independent variables were evaluated using univariate logistic regression analysis: age, gender (men = 1), disease duration, levodopa equivalent dose, UPDRS total score, UPDRS part I, UPDRS part II, UPDRS part III, UPDRS part IV, Tinetti balance, Tinetti gait, MMSE, FAB, BFI, Zung self-rating depression scale, Zung self-rating anxiety scale, summed score of items on PDSS that were rated from good to bad sleep, and history of falls (absent = 0, present = 1). Variables that were significantly related to disease progression (p < 0.05) were entered into multivariate logistic regression analysis using forced entry. Odds ratios (OR) and 95% confidence intervals (CI) were calculated. In addition, the correlations of each variable were evaluated using Spearman’s rank correlation test. The SPSS software (version 18) was used for statistical analysis.
3. Results
Of the 45 patients enrolled, 32 had disease progression and 13 had no progression (Table 1). Age (p = 0.033), BFI score (p = 0.003), Zung self-rating depression (p = 0.011), and anxiety scale (p = 0.026) were significantly increased in patients who had disease progression than those with no disease progression (Table 2). On univariate analysis, BFI score (OR = 1.057, p = 0.008, 95% CI = 1.015–1.102), Zung self-rating depression score (OR = 1.148, p = 0.017, 95% CI = 1.025–1.285), and anxiety scale (OR = 1.143, p = 0.036, 95% CI = 1.009–1.295) were significantly related to disease progression (Table 3). The results of multivariate logistic regression analysis showed that fatigue (as measured by BFI score) significantly increased the risk of disease progression (OR = 1.048, p = 0.045, 95% CI = 1.001–1.098). All BFI subscores related to general fatigue (p < 0.001), mood (p = 0.014), walking ability (p = 0.014), normal work (p = 0.002), interpersonal relationships (p = 0.015), and enjoyment of life (p = 0.013) were significantly higher in patients with disease progression (Table 4). The baseline characteristics between patients who were included in and those who dropped out from the study are shown in Table 5.

Table 1.
Hoehn-Yahr stage of subjects with Parkinson’s disease in our study.

Table 2.
Basic characteristics of subjects with Parkinson’s disease in our study.

Table 3.
Independent predictive variables for disease progression defined by an upgrade of Hoehn-Yahr stage.

Table 4.
Comparative subscores of Brief Fatigue Inventory of patients with PD with and without disease progression defined by an upgrade of Hoehn-Yahr stage.

Table 5.
Baseline characteristics between patients with Parkinson’s disease who were included in and those who dropped out from the study.
4. Discussion
The present study showed that patients with disease progression measured by Hoehn-Yahr stage have higher fatigue scores than those without progression. Therefore, fatigue was a significant predictor for disease progression.
Fatigue has an estimated prevalence of 50% in patients with PD [13] and is an intrinsic symptom derived from the pathobiological mechanism of the disease [13,14], being presence even before the onset of motor symptoms [15,16,17]. Fatigue tends to persist over the disease course and worsens with disease progression [18]. Notably, in PD, fatigue was noted to be related to striatal dopamine deficiency and an imbalance between both dopaminergic and serotonergic neurotransmitters [14]. Typically, in PD, the serotonergic function reduces in the basal ganglia and limbic structures, and this finding is possibly associated with fatigue [14]. A pathological process of PD might probably arise from the olfactory bulb and spread toward the limbic areas, potentially causing fatigue [13]. In addition, another process might arise from the dorsal vagal nucleus and ascend to the substantia nigra, causing the degeneration of the nigrostriatal dopaminergic system [19]. These pathological processes can increase the severity of both motor symptoms and fatigue. Most studies have yielded conflicting results regarding the correlation between fatigue and PD progression [13,14]. Most studies revealed that fatigue did not correlate with motor disability, but 13 cross-sectional studies demonstrated that fatigue was associated with a higher Hoehn-Yahr stage [13]. A meta-analysis revealed that patients with fatigue had Hoehn-Yahr state 0.33 points higher than those without fatigue [13]. Moreover, compared to PD patients without fatigue, patients with PD and fatigue exhibited more muscle fatigability during a finger-tapping task [20] and low-level leisure physical activity [21]. Therefore, a correlation seems to exist between fatigue and PD progression.
Notably, there are limited number of longitudinal studies that investigated the association between motor progression and fatigue. One study compared the non-motor symptoms and motor severity at baseline and two years later and observed no significant differences in fatigue levels obtained using a semi-structured 12-domain interview between patients with stable versus worsened Hoehn-Yahr stage [22]. However, the PD cohort of this study was similar to that of the PRIMO study, with the cross-sectional PRIMO study revealing fatigue severity increased with the Hoehn-Yahr stage progression [18]. Another study with a design similar to ours evaluated motor severity and non-motor symptoms of patients with PD at baseline, and after two years to determine a predictor for the motor progression based on Movement Disorders Society (MDS)-UPDRS scale [23]. Fatigue, assessed by the Fatigue Severity Scale, was found to increase the risk for MDS-UPDRS part 3 score progression, thereby indicating that subjective fatigue severity score could predict motor function in PD. This study was mentioned as the first study to have focused on the association between fatigue and motor function. Another prospective study tried to determine demographic and clinical properties associated with change in fatigue severity scale score, but could not detect any motor dysfunction progression based on UPDRS score or Hoehn-Yahr stage [24]. The reason for this finding could be that the follow-up period of one year was too short, and patients with fatigue were given higher doses of dopaminergic medications during follow-up. The dopaminergic medication doses are typically increased with motor dysfunction progression; therefore, the finding might indirectly suggest an association between fatigue and Hoehn-Yahr stage.
The pathogenesis of fatigue is unknown. Serotonin is closely associated with fatigue in chronic fatigue syndrome [25,26]. In patients with PD, the postmortem brain tissue has pathologically revealed degeneration of both dopaminergic and serotonergic neurons [27,28]. PET studies using markers of dopamine storage capacity and serotonin transporter in PD patients with fatigue have revealed serotonergic denervation in the basal ganglia and the limbic structures compared with non-fatigued patients [29]. Furthermore, serotonergic neurons, instead of the dopaminergic neurons, are known to produce dopamine with the progression of PD, especially in patients with dyskinesia. Therefore, dopaminergic and serotonergic neurons are closely related to PD. The spread of a neuropathological process toward basal ganglia and limbic structures closely associated with dopaminergic and serotonergic neurons could contribute to dysfunction of prefrontal-basal ganglia loops causing fatigue [30,31]. A higher degree of subjective fatigue severity could reflect the widespread presence of α-synuclein, which influences the progression of motor dysfunction.
The critical distinction between the subjective perception of fatigue and performance fatigability can help understand the fatigue of neurological illness [32]. The former involves homeostatic and psychological factors, with hypothalamic lesion and frontal dysfunction in PD [14,33]. On the other hand, the latter involves peripheral and central factors. Measuring quadriceps performance in PD revealed a strong negative correlation between central activation deficits and quadriceps strength, thereby suggesting the absence of muscle fatigue [34]. Nevertheless, central fatigue involves both physical and mental components, and several physiological mechanisms were hypothesized to cause dysfunction of frontal striothalamocortical loops and imbalance among various neurotransmitters [14]. The present study documented decreased scores on all BFI subscales, including physical and mental fatigue components, which might indicate that fatigue is influenced by interactions among these factors, specifically central fatigue is considered to be highly influenced by psychological factors [14].
The present study demonstrates an association between fatigue and motor dysfunction severity as previously documented in patients with a longer follow up than previous studies [18,23]. We recognize some limitations of the study. Indeed, a specific Parkinson’s fatigue scale was not used. Also, knowledge about the relationship between fatigue and depression can be better evaluated using the quick inventory of depressive symptomatology [35] or the Hamilton depression scales [36] compared with the Zung self-rating depression score, which was used in the current study. Another limitation was the small number of patients who did not demonstrate progression in motor staging.
In conclusion, fatigue could predict the progression of motor dysfunction severity over a longitudinal duration in PD patients with disease progression, having declining physical and mental fatigue.
Author Contributions
H.K. was responsible for the overall study design, and wrote the manuscript. H.K. contributed to the acquisition of data, and to analysis and interpretation of the data. H.K. and K.S. contributed to drafting and critical revision of part of the submitted materials. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study protocol was approved by the Medical Ethics Committee of Nara Medical University (No. 2710, 10 July 2020).
Informed Consent Statement
We obtained the consent of patients via opt out (http://www.nara-med-u.ac.jp/~neu/first.htm, accessed on 20 July 2020). We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Data Availability Statement
The data that support the findings of this study are openly available in this article and available from the corresponding author upon reasonable.
Acknowledgments
Thanks to neurologists for regularly seeing the patients and giving the patient information to H. Kataoka.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kataoka, H.; Tanaka, N.; Eng, M.; Saeki, K.; Kiriyama, T.; Eura, N.; Ikeda, M.; Izumi, T.; Kitauti, T.; Furiya, Y.; et al. Risk of Falling in Parkinson’s Disease at the Hoehn-Yahr Stage III. Eur. Neurol. 2011, 66, 298–304. [Google Scholar] [CrossRef]
- Kataoka, H.; Tanaka, N.; Saeki, K.; Kiriyama, T.; Ueno, S. Low frontal assessment battery score as a risk factor for falling in patients with Hoehn-Yahr Stage III Parkinson’s disease: A 2-year prospective study. Eur. Neurol. 2014, 71, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, H.; Ueno, S. Low FAB Score as a Predictor of Future Falling in Patients with Parkinson’s Disease: A 2.5-year Pro-spective Study. J. Neurol. 2015, 262, 2049–2055. [Google Scholar] [CrossRef]
- Hughes, A.J.; Daniel, S.E.; Kilford, L.; Lees, A.J. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: A clini-co-pathological study of 100 cases. J. Neurol. Neurosurg. Psychiatry 1992, 55, 181–184. [Google Scholar] [CrossRef]
- Gilman, S.; Low, P.; Quinn, N.; Albanese, A.; Ben-Shlomo, Y.; Fowler, C.; Kaufmann, H.; Klockgether, T.; Lang, A.; Lantos, P.; et al. Consensus statement on the diagnosis of multiple system atrophy. J. Neurol. Sci. 1999, 163, 94–98. [Google Scholar] [CrossRef]
- Litvan, I.; Agid, Y.; Calne, D.; Campbell, G.; Dubois, B.; Duvoisin, R.C.; Goetz, C.G.; Golbe, L.I.; Grafman, J.; Growdon, J.H.; et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): Report of the NINDS-SPSP international workshop. Neurology 1996, 47, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fahn, S.; Elton, R.; Members of UPDRS Development Committee. Unified Parkinson’s Disease Rating Scale. In Recent Development in Parkinson’s Disease; Fahn, S., Marsden, C.D., Caine, D.B., Goldstein, M., Eds.; Macmillan Health Care Information: Florham Park, NJ, USA, 1987; Volume 2, pp. 153–163, 293–304. [Google Scholar]
- Hoehn, M.M.; Yahn, M.D. Parkinsonism: Onset, progression and mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, T.R.; Wang, X.S.; Cleeland, C.S.; Morrissey, M.; Johnson, B.A.; Wendt, J.K.; Huber, S.L. The Rapid Assessment of Fatigue Severity in Cancer Patients: Use of the Brief Fatigue Inventory. Cancer 1999, 85, 1186–1196. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk Factors for Falls among Elderly Persons Living in the Community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef]
- Minguez-Castellanos, A.; Escamilla-Sevilla, F.; Katati, M.J.; Martin-Linares, J.M.; Meersmans, M.; Ortega-Moreno, A.; Arjona, V. Different patterns of medication change after subthalamic or pallidal stimulation for Parkinson’s disease: Target related effect or selection bias? J. Neurol. Neurosurg. Psychiatry 2005, 76, 34–39. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schindehütte, J.; Trenkwalder, C. “Atypical anti-psychotics” are substances of choice in treating drug-induced psychosis (DP) in Parkinson’s disease (PD). Clin. Neurol. Neurosurg. 2007, 109, 188–191. [Google Scholar] [CrossRef] [PubMed]
- Siciliano, M.; Trojano, L.; Santangelo, G.; De Micco, R.; Tedeschi, G.; Tessitore, A. Fatigue in Parkinson’s Disease: A System-atic Review and Meta-Analysis. Mov. Disord. 2018, 33, 1712–1723. [Google Scholar] [CrossRef] [PubMed]
- Kostić, V.S.; Tomić, A.; Ječmenica-Lukić, M. The Pathophysiology of Fatigue in Parkinson’s Disease and Its Pragmatic Man-agement. Mov. Disord. Clin. Pract. 2016, 3, 323–330. [Google Scholar] [CrossRef]
- Valko, P.O.; Waldvogel, D.; Weller, M.; Bassetti, C.L.; Held, U.; Baumann, C.R. Fatigue and excessive daytime sleepiness in idiopathic Parkinson’s disease differently correlate with motor symptoms, depression and dopaminergic treatment. Eur. J. Neurol. 2010, 17, 1428–1436. [Google Scholar] [CrossRef] [PubMed]
- Schifitto, G.; Friedman, J.H.; Oakes, D.; Shulman, L.; Comella, C.L.; Marek, K.; Fahn, S.; The Parkinson Study Group ELLDOPA Investigators. Fatigue in levodopa-naive subjects with Parkinson disease. Neurology 2008, 71, 481–485. [Google Scholar] [CrossRef]
- Schrag, A.; Horsfall, L.; Walters, K.; Noyce, A.; Petersen, I. Prediagnostic presentations of Parkinson’s disease in primary care: A case-control study. Lancet. Neurol. 2015, 14, 57–64. [Google Scholar] [CrossRef]
- Barone, P.; Antonini, A.; Colosimo, C.; Colosimo, C.; Marconi, R.; Morgante, L.; Avarello, T.P.; Bottacchi, E.; Cannas, A.; Ceravolo, G.; et al. The PRIAMO study: A multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov. Disord. 2009, 24, 1641–1649. [Google Scholar] [CrossRef]
- Braak, H.; Del Tredici, K.; Rüb, U.; de Vos, R.A.; Steur, E.N.J.; Braak, E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging 2003, 24, 197–211. [Google Scholar] [CrossRef]
- Lou, J.S.; Kearns, G.; Benice, T.; Oken, B.; Sexton, G.; Nutt, J. Levodopa Improves Physical Fatigue in Parkinson’s Disease: A Double-Blind, Placebo-Controlled, Crossover Study. Mov. Disord. 2003, 18, 1108–1114. [Google Scholar] [CrossRef]
- Garber, C.E.; Friedman, J.H. Effects of fatigue on physical activity and function in patients with Parkinson’s dis-ease. Neurology 2003, 43, 1119–1124. [Google Scholar] [CrossRef]
- Antonini, A.; Barone, P.; Marconi, R.; Morgante, L.; Zappulla, S.; Pontieri, F.E.; Ramat, S.; Ceravolo, M.G.; Meco, G.; Cicarelli, G.; et al. The progression of non-motor symptoms in Parkinson’s disease and their contribution to motor disability and quality of life. J. Neurol. 2012, 259, 2621–2631. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.X.; Guo, M.R.; Li, G.; Zhang, B. Association Between Fatigue and Motor Progression in Parkinson’s Disease in South-ern Chinese. Neurol. Sci. 2020, 41, 161–164. [Google Scholar] [CrossRef] [PubMed]
- Ongre, S.O.; Larsen, J.P.; Tysnes, O.B.; Herlofson, K. Fatigue in Early Parkinson’s Disease: The Norwegian ParkWest Study. Eur. J. Neurol. 2017, 24, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, S.; Ouchi, Y.; Onoe, H.; Yoshikawa, E.; Tsukada, H.; Takahashi, H.; Iwase, M.; Yamaguti, K.; Kuratsune, H.; Watanabe, Y. Reduction of serotonin transporters of patients with chronic fatigue syndrome. NeuroReport 2004, 15, 2571–2574. [Google Scholar] [CrossRef] [PubMed]
- Cleare, A.J.; Messa, C.; Rabiner, E.A.; Grasby, P.M. Brain 5-HT1A receptor binding in chronic fatigue syndrome measured using positron emission tomography and [11C]WAY-100635. Biol. Psychiatry 2005, 57, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Halliday, G.M.; Blumbergs, P.C.; Cotton, R.G.; Blessing, W.W.; Geffen, L.B. Loss of brainstem serotonin- and substance P-containing neurons in Parkinson’s disease. Brain. Res. 1990, 510, 104–107. [Google Scholar] [CrossRef]
- Hillarp, N.A.; Fuxe, K.; Dahlström, A. Demonstration and mapping of central neurons containing dopamine, noradrenaline, and 5-hydroxytryptamine and their reactions to psychopharmaca. Pharmacol. Rev. 1966, 18, 727–741. [Google Scholar]
- Pavese, N.; Metta, V.; Bose, S.K.; Chaudhuri, K.R.; Brooks, D.J. Fatigue in Parkinson’s disease is linked to striatal and limbic serotonergic dysfunction. Brain 2010, 133, 3434–3443. [Google Scholar] [CrossRef]
- Titova, N.; Qamar, M.A.; Chaudhuri, K.R. The nonmotor features of Parkinson’s disease. Int. Rev. Neurobiol. 2017, 132, 33–54. [Google Scholar]
- Marras, C.; Chaudhuri, K.R. Nonmotor features of Parkinson’s disease subtypes. Mov. Disord. 2016, 31, 1095–1102. [Google Scholar] [CrossRef]
- Kluger, B.M.; Krupp, L.B.; Enoka, R.M. Fatigue and fatigability in neurologic illnesses: Proposal for a unified taxono-my. Neurology 2013, 80, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Langston, J.W.; Forno, L.S. The hypothalamus in parkinson disease. Ann. Neurol. 1978, 3, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Stevens-Lapsley, J.; Kluger, B.M.; Schenkman, M. Quadriceps muscle weakness, activation deficits, and fatigue with Parkin-son disease. Neurorehabil. Neural. Repair. 2012, 26, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Koretz, D.; Merikangas, K.R.; Rush, A.J.; Walters, E.E.; Wang, P.S. National Comorbidity Survey Replication. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003, 229, 3095–3105. [Google Scholar] [CrossRef]
- Hedlund, J.L.; Viewig, B.W. The Hamilton rating scale for depression: A comprehensive review. J. Oper. Psychiatry 1979, 10, 149–165. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).