Abstract
With the advent of Industry 5.0 (I5.0), healthcare is undergoing a profound transformation, integrating human capabilities with advanced technologies to promote a patient-centered, efficient, and empathetic healthcare ecosystem. This study aims to examine the effects of Industry 5.0 on healthcare, emphasizing the synergy between human experience and technology. To this end, 6 specific objectives were found, which were answered in the results through an empirical study based on interviews with 11 healthcare professionals. This article thus outlines strategic and policy guidelines for the integration of I5.0 in healthcare, advocating policy-driven change, and contributes to the literature by offering a solid theoretical basis on I5.0 and its impact on the healthcare sector.
1. Introduction
As we enter a new era defined by Industry 5.0 (I5.0), we witness a symbiosis between human capabilities and technological innovations, reshaping the healthcare ecosystem on an unprecedented scale [1,2]. The importance of this topic lies in its ability to radically transform not just the existing healthcare systems but also to fundamentally reinvent the healthcare model [1,3]. As mentioned by Gomathi and Mishra [4], “Industry 5.0 is predicted to revolutionize the healthcare sector”.
This way, the concept of “Industry 5.0” is gaining traction as a model that blends technology, machinery, and human input, being an evolution of Industry 4.0. This approach (I5.0) is increasingly relevant to the healthcare industry as well, where it is known as “Healthcare 5.0”. It introduces a paradigm where technology not only supports but amplifies human competence, promoting unprecedented collaboration between doctors, patients, and machines. In this context, Healthcare 5.0 leverages advanced technologies to transform patient care, healthcare services, technologists, and the overall patient experience, bringing significant benefits to the healthcare sector [2,3,4,5,6].
The I5.0 revolution advocates for the actualization of sustainable practices and the harmonization of technology with human values and is viewed as a progressive stride toward fulfilling sustainable development goals [5,7]. The Sustainable Development Goals are “an integrated framework of human, social, and environmental development objectives that include 17 goals” [8]. I5.0 in healthcare carries the transformative potential to advance the Sustainable Development Goals (SDGs), especially SDG 3, which focuses on ensuring healthy lives and promoting well-being for all ages [9]. By integrating smart technologies, I5.0 can revolutionize patient care, making health services more accessible and personalized, thereby directly contributing to the goal’s fulfillment [1]. The ripple effects of such advancements also help in achieving SDG 8, as I5.0 technologies can create new job opportunities and promote sustained, inclusive economic growth within the different sectors, among which the healthcare sector is included [9,10]. The impact of I5.0 on health within the framework of SDG9 is addressed through an emphasis on collaboration between technologies and trends aimed at digital transformation. I5.0 represents a concept that promotes cooperation between humans and machines, improving production efficiency through effective means. This advancement supports innovation and product development in the medical sector, enabling new manufacturing opportunities through advanced technologies such as the Internet of Things (IoT), ensuring data exchange and connectivity [9]. Concurrently, the potential of I5.0 to empower local healthcare provision aligns with SDG 11, fostering the development of sustainable cities and communities through improved health infrastructure and services, reducing healthcare disparities, and enhancing services in both urban and rural areas [9]. The implementation of I5.0 could be a cornerstone in supporting and elevating global health standards, echoing the core principles of these interconnected SDGs.
Central to the success of I5.0 in healthcare is the advancement of digital literacy [1,6], robust hardware and infrastructure [4], and seamless connectivity. These elements are fundamental in realizing sophisticated telemedicine services and continuous health monitoring systems, which enable direct digital communication between patients and doctors [11], overcome geographical barriers, and enhance specialist care accessibility, particularly in remote areas [1,11].
I5.0 synergizes the technological advancements of Industry 4.0 with human expertise to enhance communication, cooperation, and the capabilities of the workforce rather than replace it. It focuses on creating inclusive digital health solutions, ensuring accessibility, affordability, and cultural sensitivity by engaging a broad range of stakeholders in their development [4,12].
The healthcare profession is on the cusp of a transformative evolution with I5.0, where the synergy between human expertise and advanced technologies will expand traditional roles. This integration will not only improve patient outcomes through personalized care but also optimize healthcare delivery, marking a new era of innovation and quality in patient care, with professionals at the helm steering toward a more responsive, informed, and technologically integrated healthcare system. For healthcare professionals, healthcare 5.0 will represent empowerment through the integration of technology as a complement to their expertise, not as a replacement, thereby enhancing their capabilities and allowing them to provide better care without being overshadowed by the technology they use [3,6,13,14].
In the transformative landscape of I5.0, Generation Z, born between the mid-1990s and early 2010s, is inherently equipped to embrace the digitalization of healthcare. Known as “digital natives” [15], they are poised to become pivotal agents of change within this new era. This generation, as part of the healthcare workforce, is not content with technical fulfillment alone; they seek roles that make a social impact, resonate with their adeptness in digital environments, and align with their innovative spirit. They aspire to positions that provide opportunities for growth and learning, and they are eager to make significant contributions to the advancement of patient care [4,15,16,17]. As beneficiaries of healthcare services, they advocate for experiences that are not just technologically enriched but also highly personalized, accessible, and seamlessly integrated with digital platforms [17]. Their innate digital fluency and fresh outlook are crucial for bridging the gap between conventional healthcare practices and the evolving dynamics of I5.0, thus shaping the future of healthcare in a manner that is both revolutionary and grounded in their unique worldview.
This study is propelled by the imperative to understand the integration of disruptive technologies from I5.0 into healthcare and to navigate the evolving landscape that is reshaping efficiency, personalization, and the humanization of care [3,4]. In doing so, it seeks to chart the largely unexplored terrain of this transition, pinpointing the challenges and opportunities that lie within. Such an analysis is not only timely but critical, given the swift progression of change and the pressing need for health systems that are both resilient and adaptable—capable of meeting current demands while also forecasting and sculpting the future of medical care and patient well-being. The central inquiry of this article, informed by the observation of Sharma et al. [1] that “scholarly works on I5.0 are still in the infancy phase”, is to answer the question: “What is the impact of I5.0 on the healthcare sector?”, thereby contributing to a foundational understanding that will guide future innovation and strategy.
Our research, driven by the continuous need for R&D (Research and Development), as emphasized by Popov et al. [18], intends to guide healthcare professionals, policymakers, and technology innovators, proposing an interdisciplinary approach to mindfully integrate emerging technologies in a manner that respects and uplifts human dignity at the heart of healthcare.
2. Theoretical Background
2.1. I5.0 in Healthcare
2.1.1. Industry 1.0 to Industry 5.0
The journey from Industry 1.0 to 5.0 marks the remarkable evolution of our manufacturing systems and the role of labor within them. The First Industrial Revolution, denoted as Industry 1.0, sparked a significant shift from agrarian societies to industrial powerhouses, beginning in the 18th century. With pioneering technologies like the steam engine, sewing machines, steelmaking, and railroads, this era catalyzed the move from agriculture to industrialization. These innovations not only redefined the production landscape but also paved the way for societal transformation, setting the foundations for subsequent industrial revolutions that would continue to leverage new energy sources and technological advancements to further reshape the economic and social fabric of societies [19].
The Second Industrial Revolution, also known as the Technological Revolution, marked a period of major industrial expansion, especially in the late 19th century. It was characterized by significant advancements in steel production, the widespread use of electric power, and the invention of the assembly line, which transformed manufacturing processes. The introduction of electricity not only enabled more extensive work hours but also led to the development of new industries and technologies, knitting disparate regions into interconnected economic units, a step toward globalization [19,20,21].
The Third Industrial Revolution, occurring in the late 20th century, brought about the digital age, heralding the rise of electronics and information technology. This revolution transformed industries with automation and computerization, shifting the focus from analog to digital technologies. It introduced a new era of digital communication, changing the nature of work and leading to the development of the Internet, which has had a profound impact on global communication and information sharing [19,20,21].
The use of computers and robots began to replace more repetitive and manual tasks, heralding an era of digital manufacturing. This digital revolution continued to evolve into Industry 4.0, which integrated cyber–physical systems and the IoT, leading to smart factories with decentralized decision-making processes.
Industry 4.0 was presented for the first time at the Hannover Fair in 2011, being the symbol of the Fourth Industrial Revolution [22]. This concept is not only widely used to increase the company’s level of productivity but also to help organizations create innovation to stay competitive in the market [23] by using digital technologies to connect the physical and cybernetic environments [24].
Now, as we transition into I5.0, the focus shifts toward a human-centric model of production. According to Xu et al. [25], I5.0 represents a significant departure from its predecessors by prioritizing societal goals and the well-being of workers. It acknowledges the value of human skills and seeks to enhance, rather than replace, these capabilities with smart automation. Gomathi and Mishra [4] emphasize that I5.0 merges the technical efficiencies of Industry 4.0 with the creativity and problem-solving abilities of humans, aiming to foster symbiotic relationships between workers and machines. But, as X. Xu et al. [25] mentioned, “I5.0 is not a chronological continuation of, or an alternative to, the existing Industry 4.0 paradigm”.
Additionally, I5.0 promises to transform various sectors beyond health, including education, manufacturing, agriculture, and services. In education, I5.0 promotes an educational transformation, emphasizing the need for a transdisciplinary approach, preparing students for advanced human–machine interactions, addressing the pillars of sustainability, and focusing on the development of human-centered solutions. In addition, technology encourages personalized and interactive teaching [26]. In manufacturing, I5.0 integrates various technologies to transform workers into “super workers”, using ergonomic and worker-friendly stations, thus enhancing the mass customization of products [27]. Ruiz-de-la-Torre-Acha et al. [28] mention a shift from efficiency-oriented to value-oriented production, thus contributing to achieving the SDGs in the production sector. In agriculture, there has been an introduction of digitized and automated systems, where AI and cloud computing can be used for remote monitoring. This technological advance aims to make agriculture highly productive and sustainable, addressing challenges such as the need to increase agricultural production by 70% by 2050 to meet the demand of the world’s population, thus aligning with the UN’s SDGs, specifically SDG 2 (“zero hunger”) [29]. In services, it promotes personalization and efficiency, improving the customer experience and optimizing operations. Several benefits of introducing I5.0 are mentioned, including increased and improved collaboration between humans and machines, user focus and user-oriented design, improved decision making, customized and efficient manufacturing solutions, and continuous innovation. However, it also faces several challenges, such as technological complexity, the need to adapt to new jobs and acquire skills, financial implications, and the risk of technological obsolescence [6,26,27,29,30,31,32].
Furthermore, I5.0’s potential impact on healthcare is profound. Pang et al. [12] suggest that by leveraging digital health solutions that are accessible, affordable, and culturally sensitive, I5.0 could address long-standing equity issues within healthcare. By actively involving a diverse array of stakeholders in the development and implementation of these solutions, I5.0 stands to democratize healthcare, making it more participatory and patient-centric. This inclusive approach to technology development could ensure that advancements in healthcare delivery truly benefit all members of society.
Figure 1 illustrates the evolution from Industry 1.0 to Industry 5.0.
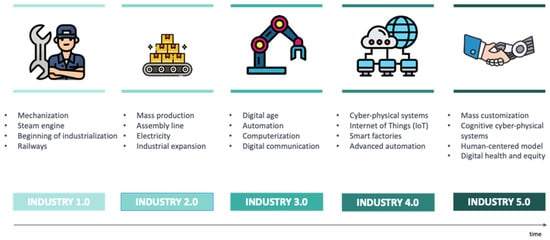
Figure 1.
Evolution from Industry 1.0 to Industry 5.0.
2.1.2. Healthcare 1.0 to Healthcare 5.0
Healthcare 1.0, from 1970 to 1990 [33], represents the traditional model of direct patient–clinician encounters, a practice that has been the foundation of healthcare for centuries, where clinicians rely on empirical evidence and their expertise for testing, diagnosis, and prescribing treatment [34]. The principal objective was “quality treatment and patient’s survivability” [35].
This model, prevalent before the digital age, involved manual record-keeping on paper, which, although widely used, presented challenges in privacy and meeting the growing demands of healthcare services due to an expanding population [36]. Despite its limitations, the face-to-face Healthcare 1.0 model has been a resilient practice in medical care [19]. As the population and demand for quality services increased, the model faced challenges in scalability and maintaining enough trained healthcare workers [19,34].
Healthcare 2.0, evolving during the early 20th century from 1991 to 2005 [37], marked a significant shift toward industrialization in healthcare, integrating new medical equipment and digital technologies for enhanced patient care [14]. Healthcare 2.0 represents the integration of advanced medical devices and digital technology into care delivery, marked by the industrialization of the healthcare sector and a focus on the value chain for end-to-end service coverage [35]. Also, our research indicates a paradigm where healthcare is characterized by increased home visits, a reduction in diagnostic testing, a narrower scope of disease knowledge, and a minimized reliance on pharmaceutical interventions [38].
This period saw the introduction of e-health, the adoption of electronic-based medical devices, and the early stage of digital technology for patient tracking and imaging, significantly improving diagnosis, treatment, and healthcare efficiency [36,39]. The era was characterized by a transition from traditional face-to-face services to a more electronically facilitated healthcare environment, leveraging the power of electricity and technology in Industry 2.0 [34].
Healthcare 3.0 emerged in 2006 and lasted until 2015 as a paradigm characterized by automation and advanced information systems, transforming healthcare through the introduction of Electronic Health Records (EHRs) and enabling more efficient care and remote healthcare capabilities [19]. This period saw artificial intelligence (AI) and digital technologies, like IoT and cloud computing, being integrated to address the challenges of data security and meet the rising demand for quality healthcare services [36]. EHRs became crucial for managing patient data and supporting the healthcare system’s efficiency, cost-effectiveness, and ability to cope with larger patient populations [34,39].
“Health 4.0 heralds the conversion of traditional health care approaches in light of a patient-centered perspective”, Moumtzoglou states in [40]. Healthcare 4.0, which ran from 2016 to 2019 [37], is aligned with the digitalization era, focusing on unique business models, mass personalization, and proactive healthcare. This revolution parallels Industry 4.0, transforming healthcare into a cyber–physical system integrated with IoT, Radio Frequency Identification (RFID), wearables, and medical robots, all supported by cloud computing, big data, and AI for smarter, interconnected healthcare delivery. This integration enables proactive treatments and personalized medicine, enhancing patient-centered care [19,35,41].
Further advancing the healthcare industry, Healthcare 4.0 introduces real-time customization of healthcare through technologies such as big data, IoT, and cloud computing. It encapsulates the notion of delivering real-time personalized healthcare to patients, physicians, and caregivers. Amidst growing medical innovation, this healthcare revolution raises both immense possibilities and significant challenges, reshaping healthcare delivery on a global scale [42,43].
Healthcare 5.0, which has lasted since 2020 [37], prioritizes personalization and customer-centric models, aiming for lifelong partnerships and improved well-being. It integrates I5.0 technologies, such as IoT, AI, and big data, to advance healthcare sustainability, reduce costs, and enhance patient outcomes. Emphasizing human-centric services, it seeks to balance service quality, cost, and benefits, addressing the satisfaction of patients, healthcare workers, and providers. Despite progress, continued development in technology and cooperation among international stakeholders is essential to fully realize Healthcare 5.0’s potential [4,34,35,36].
Building upon Healthcare 5.0’s foundation, the future can comprise a system where technology and human touch converge to offer a holistic approach to patient wellness. This will not only manage illnesses but also foster overall well-being, with a focus on preventive care. As mentioned by Hamood Alsamhi et al. [44], “Healthcare 5.0, …, seeks to create an environment that is personalized, preventive, predictive, participatory, and purpose-driven”. By harnessing advanced analytics and patient data, Healthcare 5.0 aims to predict health trends and understand patients’ needs and preferences, transforming the patient experience in line with what they need [4].
Also, as a potential future aspect of this revolution, the impact of different payment methods to reduce disparities in healthcare access across various social groups is a topic currently under exploration [45].
Figure 2 illustrates the evolution from Healthcare 1.0 to Healthcare 5.0.
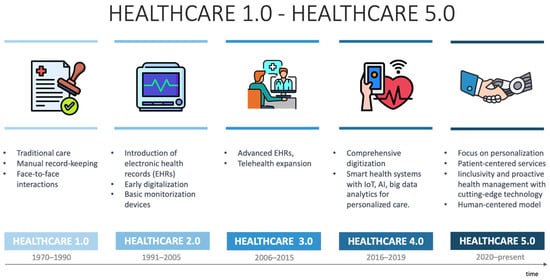
Figure 2.
Evolution from Healthcare 1.0 to Healthcare 5.0.
The evolution of healthcare over the last 5 decades has seen significant changes, with Healthcare 1.0 from 1970 to 1990, Healthcare 2.0 from 1991 to 2005, Healthcare 3.0 from 2006 to 2015, Healthcare 4.0 from 2016 to 2019, and Healthcare 5.0 from 2020 to the present, each phase being progressively shorter, indicating an acceleration in healthcare innovation and paradigm shifts. An important contribution to the rapid evolution of the digital eras is the transition from a paradigm in which information was viewed in a limited way to a digital paradigm in which it is easier to access information. This progress is marked by the development and growth of computers, which have evolved from mainframes to minicomputers and then to personal computers, culminating in the portability of iPads, making it easier for people to access information.
2.1.3. Concept Principles Applied to Health
The transition from Industry 4.0 to 5.0 in healthcare marks a shift from pure technology-driven solutions to a value-driven paradigm that centers on human well-being. This evolution embraces digitalization not just for efficiency but also for societal goals, leveraging advanced technologies like bio-inspired systems and sustainable energy solutions. It heralds a new era where the digitization of health services goes hand in hand with ethical responsibility and the betterment of patient care [4,25].
Table 1 outlines key concepts of I5.0 in healthcare.

Table 1.
Concept principles: I5.0 in Healthcare.
2.1.4. Different Terminologies for the Concept of I5.0 in Healthcare
As previously mentioned, technological evolution has reshaped various sectors, and healthcare is no exception. With the advent of I5.0, we are witnessing a significant transformation in this field, characterized by the integration of advanced technologies and personalization of patient care. In this context, terms such as “Healthcare 5.0” and “Hospital 5.0” emerge as designations that reflect the fusion of human care and technological innovations. Table 2 presents some concepts related to I5.0 in the healthcare sector.

Table 2.
Different terminologies: I5.0 in healthcare.
3. Objectives and Methods
3.1. Aims and Goals
As mentioned above, the main objective of this study is to answer the question: “What is the impact of I5.0 on the healthcare sector?” (Q1).
To answer this question, it is important to know that this new approach of I5.0 is not merely a continuation of Industry 4.0 but an effort to place human beings at the center of innovation, leveraging the impact of technology to improve quality of life, social responsibility, and sustainability [51]. For healthcare professionals, this means embracing new technologies and social innovations that can radically transform healthcare delivery. Therefore, understanding the level of knowledge of these professionals is crucial to assess the healthcare sector’s readiness to embrace these transformations and effectively apply the principles of I5.0 in clinical practice and decision making. Thus, this study will investigate the extent of healthcare professionals’ knowledge and awareness of I5.0 principles, raising the following research sub-question: “What is the level of knowledge and awareness among healthcare professionals regarding the principles of I5.0?”(Q1.1).
It is also crucial to understand emerging technological trends and how they can be applied to improve healthcare services due to the paradigm shift that Industry 4.0 is bringing to healthcare. This shift includes the use of a wide range of modern technologies, such as artificial intelligence, the Internet of Things, machine learning, and big data, among others. These technologies are providing greater user comfort through proactive interventions in the early detection and treatment of various diseases, preparing the sector to move toward I5.0. It is essential to understand these trends to guide and prepare the healthcare sector for an I5.0-ready healthcare system [4,18]. In this way, a research sub-question arises, “What are the emerging technological trends and how can they be applied to improve healthcare services?” (Q1.2) to help understand which technological trends are emerging and how they can be applied to improve health services.
Investigating the main challenges and barriers preventing the implementation of I5.0 in the healthcare sector is a critical inquiry. As Sharma et al. [1] suggest, the barriers that impede the adoption of I5.0 have not yet been fully explored. Understanding these impediments is crucial as they represent the unseen hurdles that healthcare professionals and institutions must overcome to leverage the benefits of I5.0. Furthermore, Gomathi and Mishra [4] imply that despite the challenges in adopting I5.0, it is essential to surmount them, underscoring the importance of identifying these obstacles. Recognizing and addressing these challenges is necessary to facilitate a smooth transition to the advanced, technology-driven paradigms of I5.0, which promise to enhance the efficiency, effectiveness, and personalization of healthcare services. It is therefore crucial to understand the barriers to adopting I5.0 in the health sector. Thus, another research sub-question emerges: “What are the main challenges and barriers preventing the implementation of I5.0 in the health sector?”(Q1.3).
Understanding how the adoption of I5.0 can alter healthcare delivery is critical as it moves us toward more efficient, proactive, and personalized care. I5.0 could address equity issues in health by ensuring digital health solutions are accessible, affordable, and culturally sensitive, as Pang et al. [12] suggest. Additionally, as noted by Gomathi and Mishra [4], grasping the changes brought by I5.0 is vital for progressing toward innovative technologies that enhance patient experience and well-being. As mentioned by Hamood Alsamhi et al. [44], “Healthcare 5.0, …, seeks to create an environment that is personalized, preventive, predictive, participatory, and purpose-driven”, suggesting a paradigm shift with a focus on health promotion.
In the modern digital era, individuals have a dual role as both producers and beneficiaries of data. This dual functionality enhances their capacity to be more informed and engaged in their health decisions, supporting a shift toward health promotion and preventive care models that align with the growing emphasis on patient engagement and empowerment in healthcare. [41,52]. Therefore, it is important to ask and understand the following: “How can healthcare be changed by adopting I5.0?”(Q1.4).
Investigating how I5.0 might alter the healthcare labor market is crucial, as indicated by Pang et al. [12], who emphasize the need to prepare students for the “new worlds of work they will be entering”, suggesting a significant shift in the job market. As Ong et al. [53] highlight, there is a growing demand for a new class of digital healthcare professionals equipped with skills to navigate digital healthcare strategies, develop and understand software, and manage technical issues such as computer crashes and malware, all while safely employing digital healthcare technology. Moreover, I5.0 aims to provide humans with more rewarding and fulfilling jobs, according to Gomathi and Mishra [4], enhancing job satisfaction. Understanding these changes is pivotal since the successful integration of this new industrial era hinges on the ability of healthcare professionals to adeptly use advanced technologies, posing a considerable challenge to the implementation of I5.0 within healthcare, as also noted by Gomathi and Mishra [4]. From the literature, it was concluded that it would be necessary to understand the following: “How could I5.0 change the job market in the health sector?” (Q1.5).
For effective adoption of I5.0 in healthcare, governance and management strategies must encompass collaboration between people, industry, business, and government, as highlighted by Popov et al. [18]. Similar to the transition to Industry 4.0, I5.0 will require significant investment from government agencies, as noted by Xu et al. [25]. Furthermore, the successful implementation of Healthcare 5.0 hinges on the cooperative efforts of healthcare professionals, business stakeholders, and policymakers, as mentioned by Gomathi and Mishra [4]. Examining the referenced literature has led to the recognition that it is imperative to understand the following: “What governance and management strategies are needed for effective adoption of I5.0 in the health sector?” (Q1.6).
In this way, six objectives emerged, which will be the subject of empirical analysis in the results.
3.2. Methods and Sample
To achieve the proposed objectives and understand how different stakeholders perceive the impact of I5.0 on healthcare, we adopted a bifurcated methodological approach. Firstly, we conducted semi-structured interviews with healthcare professionals. These interviews were designed to capture perceptions, personal experiences, and qualitative assessments of knowledge and expectations related to I5.0. Each specific objective of the study was addressed by a set of questions during the interviews, allowing for an in-depth investigation of the subject. Preliminary, the script of the interviews was tested by 2 health professionals who helped to identify areas of great interest or concern that warranted more detailed investigation, thus enabling feedback to be obtained on the questions that made it possible to improve them. At the end, the script was presented to the interviewees. The terminology used in the script, in ethical terms, was validated by people in the field. This methodology ensures that each study objective is explored, providing a comprehensive and balanced view of the impact of I5.0 on healthcare.
3.2.1. Data Collection Procedures
As previously mentioned, a qualitative approach was adopted for data collection, involving semi-structured interviews with various health sector professionals, including doctors, nurses, health managers, informaticists, and technologists. These interviews (audio-recorded) were conducted in January 2024, following pre-designed questions structured in line with the six specific objectives mentioned in Section 3.1, resulting in an interview script with eleven questions, in addition to those that anonymously characterized the interviewee (see Table 3). Before conducting the interviews, participants’ consent was obtained, ensuring confidentiality and anonymity.

Table 3.
Methodology: interview questions and goal-mapping.
3.2.2. Data Analysis Methods
The data collected necessitated the use of qualitative analysis methods. This involved conducting a thematic-categorical content analysis of the transcribed interviews. This analysis technique is designed to extract meanings from texts that pertain to a specific phenomenon being studied. To accomplish this, we adhered to the standard stages of content analysis. These stages include (i) organizing the material and establishing pre-analysis procedures, (ii) identifying emerging categories through textual interpretation in the exploration phase, and (iii) processing and interpreting the results of the established categories. The interviews were double-checked and analyzed to ensure that the conclusions drawn were valid.
3.2.3. Sample Characterization
To accomplish the aforementioned objectives, a total of 11 interviews were conducted with healthcare professionals. The profiles of the healthcare professionals who actively participated in these interviews are detailed in Table 4, including their respective professions, employment settings (public/private), and age range.

Table 4.
Profile of the health professionals interviewed.
The initial sampling approach was one of convenience, followed by the recommended snowball method to ensure a broad spectrum of participants for the interviews. This number of interviews allowed us to explore the concepts comprehensively while ensuring that the data analysis was manageable. We noticed a point of saturation in the responses from the last interviews, with no new information to add compared to previous collections. The selection also reflects a deliberate effort to cover a broad spectrum of ages, functions, and institutional types in the healthcare sector, thus providing a balanced view that captures the heterogeneity of the workforce. By including a range of ages and roles, from nurses and pharmacists to doctors and other healthcare specialists, this study aims to understand the different impacts and perceptions of I5.0 at different stages of professional development and institutional contexts. This approach mitigates the risk of bias toward specific groups, thus increasing the validity and reliability of the research results.
The sample includes a range of healthcare professionals: nurses, doctors, pharmacists, physiotherapists, diagnostic technicians, electromedical technicians, psychiatrists, medical surgeons, and physician teachers. These individuals are employed across both public and private sectors, with the following breakdown: 60% of the professionals are from the public sector, and 40% are affiliated with the private sector. The age distribution of the professionals is varied, with 5/11 being in the 30–40 age group. This suggests a deliberate effort to include a diverse group of healthcare workers with different specialties and sectors, as well as a range of age groups to potentially gather a wide array of insights and perspectives.
4. Results and Discussion
The obtained results of the interviews were categorized into six sections, each aligning with the six specific questions mentioned in the section before.
4.1. Healthcare Professionals’ Knowledge and Awareness of I5.0
Concerning healthcare professionals’ knowledge of I5.0 and awareness of the issue, the findings show a varied level of awareness, from familiarity with concepts like human-technology collaboration for enhanced sustainability and safety to a complete lack of knowledge. This variation seems independent of age, suggesting that I5.0 training should be tailored to varying experience levels. Some professionals recognize the value I5.0 brings to healthcare, citing the potential for improved efficiency and quality through man–machine collaboration, as mentioned by various authors [3,6,13,14]. Yet, the apparent unawareness of I5.0 among many indicates an educational gap that could hinder the adoption of advanced, human-centered technologies. In a nutshell, the results reveal that while some healthcare professionals are at the forefront of understanding I5.0 and its health implications, others are still at the beginning of this journey. The disparity in knowledge suggests the need for more comprehensive awareness and training programs that can prepare all healthcare professionals for the transformations that I5.0 is starting to bring to the sector.
4.2. Technological Trends and Their Applicability in Health
Concerning trends in emerging technologies and their applicability in healthcare, we sought to find out from the interviewees what their perception was of the impact of emerging technologies on the practice of their tasks and on the practice of patient care.
The findings show that many respondents, 9 out of 11, view technology to enhance efficiency and improve the precision and personalization of medical treatments, as mentioned by Gomathi and Mishra [4]. This enhancement is one of the most highlighted benefits, alongside the expansion of healthcare access, which is seen to extend health services to remote areas, as was also stated by Faruqui [11] and Sharma et al. [1]. However, unique concerns are mentioned by only one participant, such as the reduction in direct contact, thus impacting the human aspect of healthcare provision. This may be attributed to their specialization in physiotherapy, a field where personal interaction is paramount.
Additionally, inequity in access to technology is a substantial concern, as it could worsen healthcare disparities among socioeconomically disadvantaged groups, contrary to what Kasinathan et al. [9] suggest. Although not mentioned by a significant number of professionals, it is a topic that may not yet have reached widespread awareness. Markowitz et al.’s [45] study introduced the idea that a single-payer system could be a strategy to alleviate disparities in access to healthcare between different economic classes. Aligned with democratic values, such a system would promote equity by offering everyone the same quality of healthcare, regardless of their economic class. This is essential in a context like the US, where the current healthcare system perpetuates a divide between those who have and those who do not have access to high-quality healthcare.
Table 5 summarizes the main opinions of the interviewees on this subject.

Table 5.
Perspectives on technology in health.
In exploring the trends of emerging technologies and their application in healthcare, we delved into the respondents’ insights on the implementation of these technologies in clinical practice and patient care within their respective areas of expertise.
In analyzing the responses, several key conclusions emerge regarding the implementation of emerging technologies in healthcare. A subset of respondents emphasized the importance of patient-centered and gradual implementation, highlighting the need to tailor technology to the individual needs of patients and maintain their involvement in care decisions, as stated by Gomathi and Mishra [4]. Another consensus exists around the need for multidisciplinary collaboration in clinical development, ensuring that new technologies are needs-driven and clinician-led, as highlighted by Popov et al. [18]. Additionally, the necessity for adequate training and robust infrastructure is stressed, ensuring that healthcare professionals are equipped to integrate new technologies effectively, as also noted by Ong et al. [53] and Gomathi and Mishra [4]. Lastly, there is an acknowledgment of the need for continuous feedback and improvement mechanisms, signifying a recognition that healthcare technology must evolve responsively to remain beneficial and relevant. Thus, the following findings emerged from the analysis of the interviewer’s answers:
- The importance of accurate records and quick access: There is a consensus on the need for precise and easily accessible digital records, as well as the use of telemedicine for remote consultations and monitoring (E1). This points to a trend of digitization and remote access as fundamental components in modernizing patient care.
- Gradual and patient-centered implementation: The implementation of technologies should be gradual and tailored to the specific needs of patients (E2, E4, E11). This allows for a better assessment of needs and technology adaptation, ensuring that the patient remains at the center of care. “For example, while an AI-based system can provide valuable insights, the final decision should always be made together with the patient, considering their preferences and values.” (E11).
- Needs-driven clinical development: From the outset, technologies should be designed to meet the real needs of clinical practice and be led by qualified healthcare professionals (E10). Additionally, it is mentioned that “the implementation process should involve multidisciplinary collaboration between healthcare professionals and IT professionals is essential to optimize the use of these technologies in healthcare delivery” (E8).
- Training and integration are keys to success: Healthcare professionals need proper training to effectively use emerging technologies (E6, E8). Integrating these technologies into existing systems and interdisciplinary collaboration is essential to optimize their use in patient care. Before implementing new technologies, it is necessary to assess needs, train all healthcare professionals in their use, and establish rigorous data-management protocols (E9).
- Legal and security challenges with technologies: The integration of artificial intelligence into healthcare systems faces significant obstacles related to legal and security issues, especially regarding access to sensitive data (E7).
- Robust infrastructure and data privacy policies: Effective implementation requires robust technological infrastructure and well-established data privacy and security policies (E8).
- Ongoing evaluation and implementation science: Ongoing evaluation of technology implementation is crucial, and the use of implementation science methodologies can help measure the real impact of technologies on patient health (E8).
- Continuous feedback and improvement: The importance of continuous feedback and continuous improvement is emphasized, suggesting an iterative and responsive development model for technology in healthcare (E9).
4.3. Challenges and Barriers to Implementing I5.0
In the quest to harness the transformative potential of I5.0 in healthcare, it is imperative to understand the obstacles that stand in the way of integrating these advanced technological approaches, as pointed out by Sharma et al. [1].
Healthcare professionals identify several significant barriers to the implementation of emerging technologies. A considerable number of respondents also highlight resistance to change, signaling a need for enhanced digital literacy among both patients and healthcare providers and emphasizing the necessity of targeted training programs [6]. Privacy and security concerns are prevalent, reflecting apprehension about the safeguarding of sensitive data within new technological systems, in line with the observations of Mbunge et al. [36]. Financial constraints are frequently mentioned, indicating a pressing concern about the high costs and substantial investments required for technology infrastructure, as highlighted by Tóth et al. [31]. Also, the rapid obsolescence of technologies is mentioned by professionals and is also highlighted in the literature [31].
Although there is widespread concern among professionals about the lack of interoperability standards in healthcare, the truth is that there are established standards, such as Health Level 7 (HL7), which appeared in 1987 and has evolved from v2 to v3 and Clinical Document Architecture (CDA). The Fast Healthcare Interoperable Resource (FHIR) is also currently in use [54,55].
While not as widely noted, ethical, legal, and sustainability considerations are acknowledged, suggesting an awareness of the complex, multifaceted nature of technology adoption in the healthcare sector and reflecting the viewpoint of [4,25]. These insights collectively underscore the need for a holistic strategy that addresses financial, educational, technical, and ethical aspects to facilitate the successful integration of healthcare technologies.
The following table (Table 6) presents the main insights drawn from the interviews.

Table 6.
Barriers to implementing I5.0 in Healthcare.
4.4. The Evolution of Healthcare Delivery
Regarding the progression of healthcare, we aimed to explore with professionals how I5.0 principles are reinforcing the shift in the patient’s role from a passive recipient to an active collaborator in managing their health.
The data reveal a consensus among healthcare professionals on the impact of I5.0 in transitioning patients from passive recipients to active participants in their health management, in agreement with the statements of Chi et al. [34] and Garg and Sinth [47]. The majority (E6, E11, E1, E2) recognize the role of personalized information and monitoring technologies in this shift. The empowerment of patients through technology and education is a recurring theme (E1, E2, E5) (as highlighted by Afferni et al. [41] and Teixeira et al. [52]), albeit with the caveat of ensuring professional support for correct information interpretation (E5). While the opportunities of I5.0 in enhancing healthcare efficiency are highlighted (E9, E10), as pointed out by Haleem and Javaid [3], the need for structured health policies and societal changes to support this evolution is also acknowledged (E8), pointing to a multi-dimensional approach required for the effective integration of these new principles.
- The active role of the patient in I5.0 healthcare: The emergence of I5.0 in healthcare is redefining the traditionally passive role of patients, transforming them into active agents in the prevention and management of their health. “I5.0 in healthcare strengthens the role of the patient by providing access to personalized information and continuous health monitoring” (E6), signaling a shift toward a more preventative and patient-centered system where customization and technology are key (E11).
- Personalization and technology, the dynamic duo: The personalization of care is one of the most transformative aspects of I5.0. Tools like “applications that monitor the patient in real-time, with AI able to give indications based on the analysis of the patient’s clinical data” (E1) are enabling real-time health monitoring. These technologies not only improve treatment adherence but also “assist in the self-monitoring of disease signs and symptoms” (E2), which is vital in the management of chronic conditions.
- Patient empowerment, education, and decision making: The concept of “empowerment” is crucial in the era of I5.0. “Holding each individual accountable for their own physical and mental health” (E1) is a step toward autonomy and informed decision making. Patient education is paramount, and access to specialized information is necessary for active and conscious participation. However, it is imperative to have “the accompaniment of a specialized professional” (E5) to ensure the correct interpretation of information.
- Challenges and opportunities in implementation: Transitioning to a proactive, patient-centered health model presents challenges. “But we can’t always control what patients will understand on the other side” (E4), highlighting the variability in patient comprehension of information. On the other hand, I5.0 offers a significant opportunity to improve the healthcare system’s efficiency and reduce costs, “allowing for an improvement in quality of life and at the same time substantially reducing the costs incurred by medical assistance” (E9).
- Toward an integrated healthcare system: Developing an integrated and personalized healthcare system is a goal of I5.0. It is increasingly “perceptible a desire and beginning of the realization of a greater focus on preventive medicine” (E8). However, this trend is still in its infancy and somewhat “disorganized,” often driven by technological “hypes” such as wearable monitoring technologies rather than by comprehensive health policies. To solidify this shift, “healthcare services need to be organized in a way that promotes more personalized care, greater interaction with healthcare professionals, and access to quality health information” (E8). The establishment of comprehensive health policies and societal changes are necessary to contribute to these paradigm shifts.
“The integration of I5.0 principles empower patients with tools, information, and all the support to make their own decisions” (E9), shaping a future where the patient’s role is more significant than ever. This evolution is seen as essential for the advancement of healthcare in the future, with a consensus among professionals that “it is one of the most promising aspects of the application in health” (E10). To realize the full potential of this promise, however, “there is a need for the development of health policies and societal changes that also contribute to these paradigm changes” (E8).
4.5. Forecasting Workforce Shifts in the Emerging Market Landscape
As we have explored so far, we have already seen that the advance of I5.0 promises to revolutionize the way health services are provided. However, changes of such magnitude raise fundamental questions about the preparedness and adaptability of healthcare professionals. These results will be explored and discussed in more detail in the following subsections (Section 4.5.1, Section 4.5.2 and Section 4.5.3).
4.5.1. Preparing and Sensitizing Professionals for I5.0
The interviews indicate that, while some healthcare professionals are aware of and preparing for I5.0, there is a considerable journey ahead. Comprehensive preparation, including not only technical training but also awareness of the possibilities offered by human-technology collaboration, is fundamental for a successful transition. The responses can be summarized in the following topics:
- Challenges and resistance: Many professionals emphasized the overall lack of readiness among their colleagues for the paradigm shift, with the fear of job loss due to automation being a prominent concern (E1, E2). Additionally, the lack of digital health literacy (E3) and resistance to changing established routines (E5) were identified as significant barriers. Readiness for I5.0 was also perceived to vary considerably depending on the sector and region (E6), with some professionals questioning if they will ever feel fully prepared for such a change (E7).
- Paths for awareness and preparation: The interviews suggest that addressing these challenges requires a multifaceted strategy for raising awareness and preparing healthcare professionals. Education and training in the areas at the intersection of digital technology and healthcare were highlighted as crucial (E10), as well as the implementation of training programs by employers (E6). Additionally, sensitizing professionals to the advantages of new technological tools (E1), demonstrating how technology can improve healthcare delivery (E2), and creating new job opportunities (E6, E11) are essential steps to take. Huang et al. also mentioned this topic in their studies [32].
- The role of education and innovation: The paradigm shift requires substantial investments in education and effective engagement of professionals who understand both technology and patient care (E8, E9). It is emphasized that, in addition to technical preparation, cultivating an open mindset to harness the opportunities presented by emerging technologies, such as “reducing the burden on healthcare systems” (E3), is crucial.
4.5.2. Developing New Skills for I5.0
Based on the previous responses, it can be concluded that professionals are not adequately prepared for this paradigm shift, with some interviewed professionals emphasizing the need for training to initiate this paradigm shift. Therefore, the analysis of the data points to a recognized need for a diverse set of competencies among healthcare professionals to navigate the transition to I5.0. Technical skills such as digital literacy are the most frequently cited (E1, E5, E6, E8, E11), as reported by Ong et al. [53], underlining the importance of technology proficiency in the new healthcare paradigm. The widespread introduction of technology into the health system has an impact not only on the way clinical practice operates but also on the practice of health teaching itself. Specific mentions of cybersecurity and data-management skills (E1, E6) and artificial intelligence (E6, E10) further highlight the technical acumen required. Behavioral competencies like critical thinking (E2, E8, E9, E11) and communication skills (E8, E10) are also identified as crucial for adapting to rapid technological changes and maintaining effective patient communication.
Moreover, the emphasis on patient-centric skills by respondents (E3, E9, E2, E9) suggests a strong recognition of the importance of maintaining a focus on personalized care in the midst of technological advancements, following the assertion of Pang et al. [12]. The acknowledgment of continuous learning and innovation competencies by a single professional (E10) for various management and creative skills underscores the smaller but significant recognition of the need for ongoing development and leadership abilities to effectively manage the integration of new technologies and innovative practices within the healthcare sector.
Table 7 summarizes the skills mentioned by health professionals.

Table 7.
Competencies required of professionals.
4.5.3. Generation Z and the Transformation of the Health Paradigm
As previously seen, the preparation and awareness of healthcare professionals for the paradigm shift to I5.0 are crucial to ensure that technology is effectively utilized to enhance patient well-being. This necessitates not only investments in education but also an open mindset to embrace the opportunities presented by emerging technologies. But are the newer generations more open to change?
Generation Z’s entry into the healthcare workforce could pivot the sector from curative to preventive care, leveraging their digital savvy within the context of I5.0, as specified by Kustono [17]. However, while they are digitally inclined, Generation Z requires the development of true digital competency for health prevention (E10). Their approach to health, influenced by various socio-economic factors, suggests that broader disparities must be addressed to ensure equitable access to preventive care (E2, E4).
Incorporating Generation Z into the healthcare system may ease the financial strain on services like the National Health Service (NHS) by cutting down on chronic illness and the need for complex treatments (E1). However, a digitized healthcare model risks diminishing personal patient care (E5) and may clash with Generation Z’s preference for immediate results, challenging the adoption of preventive measures (E10).
Generation Z advocates for a comprehensive health perspective that integrates physical, mental, and emotional well-being, which could enhance patient care and incorporate a balance between technology and personalization (E8). Nevertheless, transforming healthcare goes beyond just one generation; it calls for suitable health policies, structural reforms, and measures to address social inequalities (E7, E9). In essence, the impact of Generation Z on healthcare will depend on a collaborative effort to foster digital skills, implement policy innovations, and promote reforms for a more effective, sustainable, and equitable healthcare system.
4.6. Strategies for I5.0 Adoption in Healthcare
In this section of the article, which focuses on the management strategies and governmental actions needed to integrate I5.0 into the healthcare system, it is important to recognize that the dynamics of this integration are driven primarily by healthcare policy and not by the professionals at work. The successful implementation of Healthcare 5.0 hinges on the cooperative efforts of healthcare professionals, business stakeholders, and policymakers, as mentioned by Gomathi and Mishra [4]. The previous section (Section 4.3) has illuminated the challenges of adopting I5.0; it is now essential to direct our discussion toward the institutional management strategies considered effective in overcoming these obstacles.
4.6.1. Management Strategies
Regarding the strategic approaches healthcare institutions can adopt to navigate the complexities of the new industrial revolution, it is essential that the integration of advanced technologies and practices not only enhances healthcare delivery but also aligns with the overarching goals of health policy and the evolving landscape of patient care.
Promoting a culture of innovation and continuous training is the most frequently cited strategic approach for managing the transition to I5.0 in healthcare, with mentions by three professionals (E1, E5, E10). This suggests a widespread recognition of the need for ongoing education and adaptability within the healthcare workforce. On the other hand, strategies like understanding the profiles of users and professionals for inclusive technology integration (as mentioned by Gomathi and Mishra [4] and Pang et al. [12]), developing political strategies, and providing information on new technologies were each mentioned by only one professional (E2, E3, E4, respectively), pointing to these areas as potentially under-recognized or niche concerns. This distribution of responses might reflect the immediate perceived needs and the differing levels of urgency assigned to various strategies, with training and innovation taking precedence in the current climate as the most direct ways to influence and prepare for upcoming changes. Moreover, the input from a psychiatrist (E7) on the importance of acknowledging the limitations of current technological models likely stems from the unique challenges in mental healthcare, where technology has yet to fully meet the nuanced demands of patient treatment and interaction.
The management strategies highlighted by the healthcare professionals are as follows:
- Develop a strategic vision aligned with new technologies (E1);
- Promote a culture of innovation and encourage continuous training (E1, E5, E10);
- Create an institutional culture open to innovation, reducing centralization and vertical hierarchies based on small, agile, and well-connected groups (E10, E11);
- Encourage change among collaborators (E1, E11);
- Involve all stakeholders in the transformation process, including patients, health professionals, and political decision makers (E1, E11) and promote interdisciplinary collaboration (E6, E8, E9);
- Emphasize data security as an organizational priority (E1, E6, E9);
- Implement monitoring systems that support strategic decisions and increase efficiency (E1);
- Understand the profile of users and professionals to integrate technology inclusively (E2);
- Develop political strategies to drive changes in the sector (E3);
- Provide information and clarification about new technological tools (E4);
- Facilitate the collaboration of workers with reward strategies (E5);
- Adopt committed leadership and comprehensive training (E6);
- Implement an incremental approach with pilot projects (E6);
- Perform continuous assessment of the impact in terms of health outcomes (E6, E8);
- Keep people informed about the limitations of current technological models (E7).
4.6.2. Governance Strategies
The health professionals interviewed emphasized the importance of strategic government policies as an initial step for the transition to I5.0 in the healthcare sector, in addition to organizational initiatives.
In the strategic planning for the transition to I5.0 within healthcare, the analysis highlights that the most emphasized element is training and professional development, with five professionals (E1, E6, E8, E9, E11) advocating for skill-updating programs. This emphasis indicates a broad agreement on the critical role of equipping healthcare workers with the necessary expertise to navigate the changes introduced by I5.0. Financial stimuli and incentives are also frequently mentioned (E1, E5, E6, E8), pointing to the importance placed on motivating healthcare professionals and supporting technological advancements.
Conversely, certain strategies such as the expansion of 5G infrastructure and the assurance of efficient information systems (as pointed out by Sharma et al. [1]), while seen as essential, are mentioned less frequently, noted by two and three professionals, respectively. The promotion of equitable access and universality is highlighted by four professionals (E1, E2, E9, E11), indicating a strong awareness of the need to address accessibility and inclusivity in the digital transformation of healthcare, as mentioned by Gomathi and Mishra [4] and Pang et al. [12]. Regulatory support and the fostering of innovation receive attention, suggesting that creating a conducive environment for continuous improvement is a recognized need, though not as prominently as training and incentives.
The strategic actions identified by them are listed below:
- Financial Stimuli and Incentives (E1, E5, E6, E8): Implementation of financial incentives and rewards for objectives to motivate healthcare professionals and support the development and adoption of new technologies.
- Training and Skilling (E1, E6, E8, E9, E11): Development of programs to update healthcare professionals’ skills, ensuring they are prepared for the demands of I5.0.
- Expansion of 5G Infrastructure (E1, E3): Investment in the construction and improvement of a robust, nationwide 5G infrastructure essential for supporting telemedicine and other emerging technologies.
- Assurance of Efficient Information Systems (E1, E4, E7): Implementation and maintenance of secure and efficient healthcare information systems, allowing more agile and safer data management.
- Establishment of Quality and Safety Standards (E1): Definition of strict standards to ensure safety in the implementation of new technologies.
- Promotion of Equitable Access and Universality (E1, E2, E9, E11): Implementation of policies that ensure equal access to healthcare and promote digital inclusion, especially in remote areas. Further, implementation of actions to reduce disparities in access to these technologies and ensure their use by a larger number of people.
- Integration and Intersectoral Collaboration (E8): Promotion of collaborations between the public sector, private sector, academia, and industry to drive innovations and efficiency in the healthcare sector.
- Regulatory Clarity and Support for Innovation (E6, E11): Establishment of clear regulations and constant support for innovation, including public–private partnerships and incentives for startups.
- Digitalization and Population Education (E4, E9): Investments in digital infrastructure and education programs to familiarize the population with digital health and maximize the benefits of technological innovations.
- Focus on Value-Based Health (E10): Encouragement of a value-based approach, emphasizing the efficient measurement of outcomes and resources in the healthcare sector.
5. Reflection on the Results in the Light of a SWOT Analysis
To discuss the integration of I5.0 in healthcare, a SWOT analysis was conducted, assessing the Strengths, Weaknesses, Opportunities, and Threats associated with this integration to identify proactive management strategies.
I5.0 in healthcare promises to personalize care and improve efficiency through innovative tools, AI, and automation (strengths). These advancements aim to enhance service quality and adapt to individual patient needs. Yet, the transition is challenged by a lack of professional understanding, infrastructure limitations, and training deficits. Access inequality and resource management also pose issues (weaknesses).
Opportunities lie in addressing the needs of an aging population and capitalizing on technological R&D, with potential government support and the tech-savvy Generation Z driving progress. However, threats include data privacy concerns, access disparities, the possibility of technological obsolescence, economic limits, and potential job displacement due to automation.
SWOT analysis will help identify management strategies to meet the challenges of integrating I5.0 into healthcare, exploit the opportunities it offers, and minimize the threats to its success. This way, this analysis allows leaders to develop more effective strategies, make informed decisions, and identify areas that need improvement or adjustment. As mentioned by Selvam et al. [46], “This is just the tip of the iceberg, as there are more advancements to come in the near future in this avenue”.
Figure 3 presents an illustration of SWOT analysis.
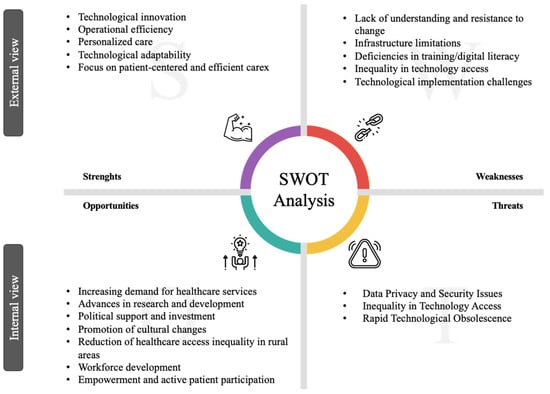
Figure 3.
SWOT analysis of the integration of I5.0 in healthcare.
6. Final Remarks
6.1. Conclusions
This article offers a comprehensive overview of the current landscape of I5.0 within the healthcare sector. It delves into the technological advancements identified by Gomathi and Mishra [4] as pivotal for equipping the healthcare industry for a transition to an I5.0-aligned system. This study also addresses the challenges in adopting I5.0 in healthcare settings, highlighting unexplored areas, as pointed out by Sharma et al. [1]. Furthermore, it underscores the importance, as emphasized by Gomathi and Mishra [4], of understanding the transformative impact of I5.0 to foster innovation and improve patient care and welfare. This article also embarks on an exploratory journey, guided by insights from Pang et al. [12], into the potential reshaping of the healthcare workforce due to I5.0 innovations. Finally, it proposes actionable strategies and policy recommendations for the successful integration of I5.0 in healthcare, aligning with the perspectives of Mbunge et al. [36] on the imperative need for such advancements in the sector.
I5.0 ushers in a dynamic change in healthcare, from traditional methods to personalized, technology-driven care. This new paradigm improves the relationship between patient and healthcare professional, moving from hierarchical to collaborative, and changes treatment from standardized to individualized, integrating technology. Despite the technological basis, care remains human, focusing on personalization, efficiency, and empathy. The transition faces obstacles such as resistance from professionals, but the digital fluency of Generation Z and management and government strategies will help adopt new practices. Policies that support digital literacy among professionals, equitable access to technology, and the development of telemedicine are key to a smoother transformation. This change, symbolized by a bridge in Figure 4, marks the progress from resistance to innovation, pointing to a future of resilient and flexible healthcare. Technology and I5.0 are not the solution to all issues; it is essential to implement practices in the social sphere and raise awareness among government bodies of the need to create mechanisms and solutions to help mitigate the problem. In conclusion, it can be stated that one of the most significant transitions in Health 5.0 is the shift from an emphasis on sickness to wellness.
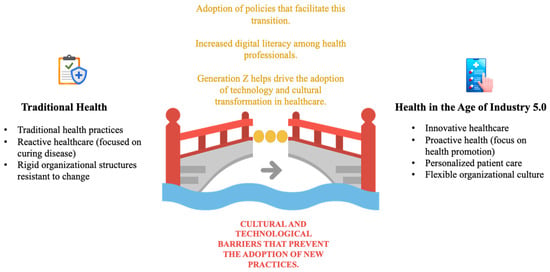
Figure 4.
The gap between traditional healthcare and I5.0 innovations.
6.2. Contributions and Implications
- Practical Implications for Healthcare Professionals and Policymakers: This study provides practical recommendations related to management strategies and governmental actions required to effectively integrate I5.0 into the healthcare system. It recognizes that the driving force behind this integration is primarily shaped by healthcare policies rather than by active professionals in the field. We hope that this article catalyzes in-depth and comprehensive discussions on these matters, promoting reflection and action. Moreover, this article disseminates the potential of technology in healthcare to catalyze new practices that may be driven by technologies, some of which are still possibly unknown. In addition, it can help alert clinicians and patients to focus on promoting health rather than treating disease. Furthermore, this document can contribute in a way that may influence what could become the next era of healthcare.
- Theoretical Implications: This study also significantly contributes to the literature by offering a solid theoretical foundation regarding I5.0 and its impact on the healthcare sector. It describes I5.0 as an approach that prioritizes humans at the forefront of innovation, harnessing technology’s potential to enhance quality of life, promote social responsibility, and strengthen sustainability. Also, this work enriches the discussion on this topic and shows some trends in this area.
6.3. Limitations and Future Work
- Limitations of the Study: It is important to acknowledge that this study has certain limitations. Firstly, the research was based on a limited number of interviews, which may impact the representativeness of the results. Additionally, the interviews were conducted within a specific healthcare context, which may limit the generalizability of the findings to other areas within the healthcare sector. Furthermore, the qualitative nature of the interviews may have introduced selection bias, as interviewees may have varied perspectives and experiences. In addition, we would like to note that quantitative analyses based on interviews possibly entail biases arising from the interviewer’s familiarity with the topic discussed. Therefore, it is essential to consider these limitations when interpreting the results of this study.
- Future Work: For future research in this area, there are several promising directions to explore. Firstly, as mentioned earlier, it is crucial to expand the number of interviews and include a variety of participants to gain a more comprehensive insight into healthcare professionals’ perceptions of I5.0. Additionally, future studies can focus on conducting more detailed analyses of inclusion issues and how I5.0 technologies can be applied to promote equality in access to healthcare services. In line with this, the critical importance of the Social Determinants of Health and the significant role they play in shaping the future of healthcare is recognized. Although this aspect was not explored in the present study, we intend to address it in detail as a central line of research in our future work. This additional research will allow us to better understand how socioeconomic, environmental, and cultural factors influence health and how health systems can evolve to respond to these determinants more effectively, promoting inclusion and equitable access to healthcare. Another relevant research area is the assessment of healthcare professionals’ training needs and the development of specific training programs. Moreover, collaboration with stakeholders such as healthcare government agencies and professional associations can be explored to establish guidelines and policies that support the successful implementation of I5.0 in the healthcare sector. Furthermore, we intend, as part of future work, to address a literature review highlighting previous studies on the impact of I5.0 on healthcare or similar impacts in other sectors, to enrich the context of our current study, as well as establish a clear link between the principles of I 5.0 and how they can contribute to achieving the SDGs in healthcare. Finally, we would like to note that, recognizing the importance of patient-centered care, future work will aim to capture the experiences, expectations, and satisfaction levels of patients receiving healthcare services in the evolving scenario of I5.0. This two-stage approach will allow us to build a more holistic view of the healthcare ecosystem and its players. These research directions can significantly contribute to advancing our understanding and application of I5.0 in the field of healthcare.
Author Contributions
Conceptualization, J.B.-R.; methodology, J.B.-R. and L.T.; validation, L.T.; formal analysis, J.B.-R. and L.T.; writing—original draft preparation, J.B.-R.; writing—review and editing, J.B.-R. and L.T.; supervision, L.T.; funding acquisition, J.B.-R. and L.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the Institute of Electronics and Informatics Engineering of Aveiro (UIDB/00127/2020), funded by national funds through the FCT—Foundation for Science and Technology (FCT).
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to private issues.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Sharma, M.; Sehrawat, R.; Luthra, S.; Daim, T.; Bakry, D. Moving towards Industry 5.0 in the Pharmaceutical Manufacturing Sector: Challenges and Solutions for Germany. IEEE Trans. Eng. Manag. 2022; early access. [Google Scholar] [CrossRef]
- Ozkeser, B. Lean Innovation Approach in Industry 5.0. Technology, Engineering & Mathematics (EPSTEM). 2018, Volume 2. Available online: www.isres.org (accessed on 18 January 2024).
- Haleem, A.; Javaid, M. Industry 5.0 and its expected applications in medical field. Curr. Med. Res. Pract. 2019, 9, 167–169. [Google Scholar] [CrossRef]
- Gomathi, L.; Mishra, A.K. Industry 5.0 for Healthcare 5.0: Opportunities, Challenges and Future Research Possibilities. In Proceedings of the IEEE—7th International Conference on Trends in Electronics and Informatics (ICOEI), Tirunelveli, India, 11–13 April 2023. [Google Scholar]
- Sindhwani, R.; Afridi, S.; Kumar, A.; Banaitis, A.; Luthra, S.; Singh, P.L. Can industry 5.0 revolutionize the wave of resilience and social value creation? A multi-criteria framework to analyze enablers. Technol. Soc. 2022, 68, 101887. [Google Scholar] [CrossRef]
- Adel, A. Future of industry 5.0 in society: Human-centric solutions, challenges and prospective research areas. J. Cloud Comput. 2022, 11, 40. [Google Scholar] [CrossRef] [PubMed]
- Renda, A.; Schwaag Serger, S.; Tataj, D.; Morlet, A.; Isaksson, D.; Martins, F.; Mir Roca, M.; Hidalgo, C.; Huang, A.; Dixson-Declève, S.; et al. Industry 5.0, a Transformative Vision for Europe: Governing Systemic Transformations towards a Sustainable Industry. 2022. Available online: https://op.europa.eu/en/web/eu-law-and-publications/publication-detail/-/publication/38a2fa08-728e-11ec-9136-01aa75ed71a1 (accessed on 18 December 2023).
- Moyer, J.D.; Hedden, S. Are we on the right path to achieve the sustainable development goals? World Dev. 2020, 127, 104749. [Google Scholar] [CrossRef]
- Kasinathan, P.; Pugazhendhi, R.; Elavarasan, R.M.; Ramachandaramurthy, V.K.; Ramanathan, V.; Subramanian, S.; Kumar, S.; Nandhagopal, K.; Raghavan, R.R.V.; Rangasamy, S.; et al. Realization of Sustainable Development Goals with Disruptive Technologies by Integrating Industry 5.0, Society 5.0, Smart Cities and Villages. Sustainability 2022, 14, 15285. [Google Scholar] [CrossRef]
- Ghobakhloo, M.; Iranmanesh, M.; Morales, M.E.; Nilashi, M.; Amran, A. Actions and approaches for enabling Industry 5.0-driven sustainable industrial transformation: A strategy roadmap. Corp. Soc. Responsib. Environ. Manag. 2023, 30, 1473–1494. [Google Scholar] [CrossRef]
- Faruqui, U. Survey Paper: Future Service in Industry 5.0. J. Sist. Cerdas 2019, 2, 67–79. [Google Scholar] [CrossRef]
- Pang, T.Y.; Lee, T.K.; Murshed, M. Towards a New Paradigm for Digital Health Training and Education in Australia: Exploring the Implication of the Fifth Industrial Revolution. Appl. Sci. 2023, 13, 6854. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M. Industry 5.0 and its applications in orthopaedics. J. Clin. Orthop. Trauma 2019, 10, 807–808. [Google Scholar] [CrossRef]
- Ahmad, K.A.B.; Khujamatov, H.; Akhmedov, N.; Bajuri, M.Y.; Ahmad, M.N.; Ahmadian, A. Emerging trends and evolutions for smart city healthcare systems. Sustain. Cities Soc. 2022, 80, 103695. [Google Scholar] [CrossRef]
- Benítez-Márquez, M.D.; Sánchez-Teba, E.M.; Bermúdez-González, G.; Núñez-Rydman, E.S. Generation Z within the Workforce and in the Workplace: A Bibliometric Analysis. Front. Psychol. 2022, 12, 736820. [Google Scholar] [CrossRef] [PubMed]
- Kreacic, A.; Romeo, J.; Luong, S.; Uribe, L.; Lasater-Wille, A.; Costa, E. What Business Needs To Know About The Generation Changing Everything Click. 2023. Available online: https://www.oliverwymanforum.com/global-consumer-sentiment/a-gen-z.html (accessed on 18 January 2024).
- Kustono, D. Sharpening Public Health’s Goals and Tools in Currently Global Issue. In Proceedings of the International Conference on Sports Science and Health (ICSSH 2022); Atlantis Press International: Dordrecht, The Netherlands, 2022; pp. 189–197. [Google Scholar] [CrossRef]
- Popov, V.V.; Kudryavtseva, E.V.; Katiyar, N.K.; Shishkin, A.; Stepanov, S.I.; Goel, S. Industry 4.0 and Digitalisation in Healthcare. Materials 2022, 15, 2140. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Carayon, P. Health Care 4.0: A vision for smart and connected health care. IISE Trans. Healthc. Syst. Eng. 2021, 11, 171–180. [Google Scholar] [CrossRef]
- Ávila-Gutiérrez, M.J.; de Miranda, S.S.F.; Aguayo-González, F. Occupational Safety and Health 5.0—A Model for Multilevel Strategic Deployment Aligned with the Sustainable Development Goals of Agenda 2030. Sustainability 2022, 14, 6741. [Google Scholar] [CrossRef]
- Ali, M.A.; Irfan, M.S.; Khan, T.; Khalid, M.Y.; Umer, R. Graphene nanoparticles as data generating digital materials in industry 4.0. Sci. Rep. 2023, 13, 4945. [Google Scholar] [CrossRef] [PubMed]
- Da Xu, L.; Xu, E.L.; Li, L. Industry 4.0: State of the art and future trends. Int. J. Prod. Res. 2018, 56, 2941–2962. [Google Scholar] [CrossRef]
- Sarbu, M. The impact of industry 4.0 on innovation performance: Insights from German manufacturing and service firms. Technovation 2021, 113, 102415. [Google Scholar] [CrossRef]
- da Silva, L.; Soltovski, R.; Pontes, J.; Treinta, F.; Leitão, P.; Mosconi, E.; de Resende, L.; Yoshino, R. Human resources management 4.0: Literature review and trends. Comput. Ind. Eng. 2022, 168, 108111. [Google Scholar] [CrossRef]
- Xu, X.; Lu, Y.; Vogel-Heuser, B.; Wang, L. Industry 4.0 and Industry 5.0—Inception, conception and perception. J. Manuf. Syst. 2021, 61, 530–535. [Google Scholar] [CrossRef]
- Ruppert, T.; Darányi, A.; Medvegy, T.; Csereklei, D.; Abonyi, J. Demonstration Laboratory of Industry 4.0 Retrofitting and Operator 4.0 Solutions: Education towards Industry 5.0. Sensors 2023, 23, 283. [Google Scholar] [CrossRef]
- John, K.K.; Adarsh, S.N.; Pattali, V. Workers to super workers: A brief discussion on important technologies for industry 5.0 manufacturing systems. AIP Conf. Proc. 2020, 2311, 070025. [Google Scholar] [CrossRef]
- Ruiz-de-la-Torre-Acha, A.; Guevara-Ramirez, W.; Río-Belver, R.M.; Borregan-Alvarado, J. Industry 5.0. The Road to Sustainability. In Lecture Notes in Networks and Systems; Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2023; pp. 247–257. [Google Scholar] [CrossRef]
- Martos, V.; Ahmad, A.; Cartujo, P.; Ordoñez, J. Ensuring agricultural sustainability through remote sensing in the era of agriculture 5.0. Appl. Sci. 2021, 11, 5911. [Google Scholar] [CrossRef]
- Maddikunta, P.K.R.; Pham, Q.-V.; Prabadevi, B.; Deepa, N.; Dev, K.; Gadekallu, T.R.; Ruby, R.; Liyanage, M. Industry 5.0: A survey on enabling technologies and potential applications. J. Ind. Inf. Integr. 2022, 26, 100257. [Google Scholar] [CrossRef]
- Tóth, A.; Nagy, L.; Kennedy, R.; Bohuš, B.; Abonyi, J.; Ruppert, T. The human-centric Industry 5.0 collaboration architecture. MethodsX 2023, 11, 102260. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Wang, B.; Li, X.; Zheng, P.; Mourtzis, D.; Wang, L. Industry 5.0 and Society 5.0—Comparison, complementation and co-evolution. J. Manuf. Syst. 2022, 64, 424–428. [Google Scholar] [CrossRef]
- Jain, R.; Gupta, M.; Nayyar, A.; Sharma, N. Adoption of fog computing in healthcare 4.0. In Signals and Communication Technology; Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2021; pp. 3–36. [Google Scholar] [CrossRef]
- Chi, H.R.; de Fátima Domingues, M.; Zhu, H.; Li, C.; Kojima, K.; Radwan, A. Healthcare 5.0: In the Perspective of Consumer Internet-of-Things-Based Fog/Cloud Computing. IEEE Trans. Consum. Electron. 2023, 69, 745–755. [Google Scholar] [CrossRef]
- Wazid, M.; Das, A.K.; Mohd, N.; Park, Y. Healthcare 5.0 Security Framework: Applications, Issues and Future Research Directions. IEEE Access 2022, 10, 129429–129442. [Google Scholar] [CrossRef]
- Mbunge, E.; Muchemwa, B.; Jiyane, S.; Batani, J. Sensors and healthcare 5.0: Transformative shift in virtual care through emerging digital health technologies. Glob. Health J. 2021, 5, 169–177. [Google Scholar] [CrossRef]
- Natarajan, R.; Lokesh, G.H.; Flammini, F.; Premkumar, A.; Venkatesan, V.K.; Gupta, S.K. A Novel Framework on Security and Energy Enhancement Based on Internet of Medical Things for Healthcare 5.0. Infrastructures 2023, 8, 22. [Google Scholar] [CrossRef]
- Van De Belt, T.H.; Engelen, L.J.L.P.G.; Berben, S.A.A.; Schoonhoven, L. Definition of health 2.0 and medicine 2.0: A systematic review. J. Med. Internet Res. 2010, 12, e18. [Google Scholar] [CrossRef]
- Bhavin, M.; Tanwar, S.; Sharma, N.; Tyagi, S.; Kumar, N. Blockchain and quantum blind signature-based hybrid scheme for healthcare 5.0 applications. J. Inf. Secur. Appl. 2021, 56, 102673. [Google Scholar] [CrossRef]
- Ciasullo, M.V.; Orciuoli, F.; Douglas, A.; Palumbo, R. Putting Health 4.0 at the service of Society 5.0: Exploratory insights from a pilot study. Socio-Econ. Plan. Sci. 2022, 80, 101163. [Google Scholar] [CrossRef]
- Afferni, P.; Merone, M.; Soda, P. Hospital 4.0 and Its Innovation in Methodologies and Technologies. In Proceedings of the 2018 IEEE 31st International Symposium on Computer-Based Medical Systems (CBMS), Karlstad, Sweden, 18–21 June 2018; pp. 333–338. [Google Scholar] [CrossRef]
- Gupta, A.; Singh, A. Healthcare 4.0: Recent advancements and futuristic research directions. Wirel. Pers. Commun. 2023, 129, 933–952. [Google Scholar] [CrossRef] [PubMed]
- Tortorella, G.L.; Fogliatto, F.S.; Vergara, A.M.C.; Vassolo, R.; Sawhney, R. Healthcare 4.0: Trends, challenges and research directions. Prod. Plan. Control 2020, 31, 1245–1260. [Google Scholar] [CrossRef]
- Alsamhi, S.H.; Hawbani, A.; Shvetsov, A.V.; Kumar, S. Advancing Pandemic Preparedness in Healthcare 5.0: A Survey of Federated Learning Applications. Adv. Hum.-Comput. Interact. 2023, 2023, 9992393. [Google Scholar] [CrossRef]
- Markowitz, W.; McLeod-Sordjan, R. Values-Based Foundation for a U.S. Single Payer Health System Model. Front. Sociol. 2021, 6, 627560. [Google Scholar] [CrossRef] [PubMed]
- Selvam, A.; Aggarwal, T.; Mukherjee, M.; Verma, Y.K. Humans and robots: Friends of the future? A bird’s eye view of biomanufacturing industry 5.0. Biotechnol. Adv. 2023, 68, 108237. [Google Scholar] [CrossRef]
- Garg, J.; Singh, A.K. the Use of Digital Healthcare Systems To Predict Diseases. Asia Pac. J. Health Manag. 2023, 18, 267–274. [Google Scholar] [CrossRef]
- Nahavandi, S. Industry 5.0-a human-centric solution. Sustainability 2019, 11, 4371. [Google Scholar] [CrossRef]
- Rehman, M.U.; Andargoli, A.E.; Pousti, H. Healthcare 4.0: Trends, Challenges and Benefits. In Proceedings of the Australasian Conference on Information Systems, Perth, Australia, 9–11 December 2019. [Google Scholar]
- Gauttier, S. Hospital 5.0: Enhancing nurses with the use of wearables. In Proceedings of the 32nd International BCS Human. Computer Interaction Conference, HCI 2018, Belfast, UK, 4–6 July 2018; BCS Learning and Development Ltd.: Swindon, UK, 2018. [Google Scholar] [CrossRef]
- Carayannis, E.G.; Morawska-Jancelewicz, J. The Futures of Europe: Society 5.0 and Industry 5.0 as Driving Forces of Future Universities. J. Knowl. Econ. 2022, 13, 3445–3471. [Google Scholar] [CrossRef]
- Teixeira, L.; Cardoso, I.; Sá, J.O.E.; Madeira, F. Are Health Information Systems Ready for the Digital Transformation in Portugal? Challenges and Future Perspectives. Healthcare 2023, 11, 712. [Google Scholar] [CrossRef]
- Ong, J.; Parchment, V.; Zheng, X. Effective regulation of digital health technologies. J. R. Soc. Med. 2018, 111, 439–443. [Google Scholar] [CrossRef]
- Vorisek, C.N.; Lehne, M.; Klopfenstein, S.A.I.; Mayer, P.J.; Bartschke, A.; Haese, T.; Thun, S. Fast Healthcare Interoperability Resources (FHIR) for Interoperability in Health Research: Systematic Review. JMIR Med. Inform. 2022, 10, e35724. [Google Scholar] [CrossRef]
- Gulden, C.; Blasini, R.; Nassirian, A.; Stein, A.; Altun, F.B.; Kirchner, M.; Prokosch, H.-U.; Boeker, M. Prototypical clinical trial registry based on fast healthcare interoperability resources (FHIR): Design and implementation study. JMIR Med. Inform. 2021, 9, e20470. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).