1. Introduction
The World Health Organization’s (WHO) recommended Directly Observed Treatment Short-courses (DOTS) strategy promotes de-centralized care and effective management of the tuberculosis (TB) control program, including training and supervision of healthcare providers [
1]. Among other challenges of the healthcare systems in low and middle-income countries, poor quality, insufficient quantity, and partial distribution of the healthcare providers are significant concerns mentioned in the WHO Global Plan to Stop TB 2006–2015 [
2,
3]. In addition, it is usually acknowledged that building the capacity of human resource is crucial for TB control efforts [
4]. Recognizing the need of human resource capacity building, the Global Fund to Fight AIDS, Tuberculosis, and Malaria provided 16 million training episodes to healthcare providers (HCPs), which is almost ten times higher the number of HCPs training episodes given in 2005 [
5]. In the past, most of the TB care and prevention focus remained on the coverage of services. However, current data trends show that there is a need to think about expansion of TB care services, thereby emphasizing quality of care, both in private and public sectors [
6,
7]. Evidence indicated that improved training and continuous supportive supervision can improve providers’ skills for TB case management, hence resulting in better treatment adherence [
8]. It is also known that quality of training is directly associated with quality of TB care and treatment outcome. Additionally, knowledge deficiency in healthcare providers can result in a delayed or missed diagnosis [
9]. Hence, troubling the overall efforts of the TB control program.
Training is considered as an agent of change and lectures are the most common, simple, and low-cost method used in training programs in classroom settings [
10]. However, disengagement of participants, likelihood of forgetting, and one-way communication are common issues associated with this method [
11]. Therefore, importance of blended education is emphasized where two or more methods are used to impart training (e.g., multimedia course, seminar, and e-learning). Studies suggest that a combination of face-to-face training along with e-learning methods has generated better results [
12]. An increasingly popular method, e-Learning, is a training method where trainer and trainee are not required to be co-located and technological capabilities (tools, technology, equipment) connect them together [
13]. For these reasons, e-Learning or e-Training approaches have gained immense importance, especially when healthcare providers have limited time available, different work shifts, and high turnover rate in developing countries. Virtual reality (VR) is a methodology that has successfully been applied to the learning process and it can help to improve the traditional teaching methods. VR’s adoption in the learning process allows participants to have intuitive understanding of what they learn [
14].
Three-dimensional (3D) virtual worlds and graphical environments, such as Second Life (
http://secondlife.com/) and Sansar (
https://www.sansar.com/), offer a number of unique edutainment affordances and opportunities (edutainment is education enhanced by entertainment and game-like elements, also known as ‘serious gaming’); for example, realistic immersion, visualization, and simulation, exploratory learning and training, networking and collaboration (in multi-player environments). Kamel Boulos et al.’s [
15,
16] reviews of the subject toured some of the early medical and public, environmental, and occupational health examples in Second Life and highlighted the potentials of 3D virtual worlds in medical and health education. Serious gaming engages the learner through various game elements and challenges involving positive competition with other learners (or players), such as game points, badges, achievements, and leader boards.
However, virtual environments are different from digital games and simulations [
17]. The use of game elements and metaphors is currently a wide practice across several domains to improve the design of non-game elements (e.g., virtual environment) and processes, helping create outcomes that enhance user engagement [
18]. This process is usually called gamification and is successfully being used to create education support and motivation promotion systems, elicitation, digital inclusion, and social platforms and health applications, among others. In the domain of medicine, digital games are presented as simulations, virtual environments, and alternate reality games [
19,
20]. The present state of literature, pertinent to digital games in medical education, is not conclusive in regard to definition of its constituent elements [
17].
Considering the nature of the medical profession, medical practice is given a pivotal importance, hence the majority of the games-based education and training programs concentrate on the procedural skills (e.g., for surgery) to improve patient safety and to offer competency-based learning [
21]. This method of learning is cost-effective in providing virtual experience to learners through a variety of clinical scenarios, hence they are able to assess themselves by negative or positive outcome of the clinical procedure [
22] in a safe environment without any fear of being judged and becoming a risk to patient safety [
23].
The current cumulative evidence in the research literature regarding the effectiveness of serious games in a healthcare professionals’ education is mixed. This could be partially explained by the wide variability in their design and presentation (on mobile, desktop, and dedicated game console platforms) across different studies, prompting Maheu-Cadotte et al. [
24] to conduct a new systematic review to “identify, appraise, and synthesize the best available evidence regarding the effectiveness of serious games and the impact of game design on engagement and educational outcomes of healthcare professionals”. Evaluations are crucial to determine whether training programs were effective or not [
25] (Habicht et al., 1999). This can be done by systematic assessment of the intended learning outcomes of training activities, and by measuring if it has resulted in improved job performance or not [
26]. In one cluster randomized controlled trial, no significant improvement was observed in treatment outcome of TB patients as a result of an 18-h long participatory training program for clinic staff [
27]. After the success of flight simulations, use of virtual reality was first proposed by Satava [
28] in the medical field for the purpose of gaining surgical skills. Virtual reality is based on creating virtual environments that allow users to interact with a 3-dimensional computerized world. The virtual environment consists of a humanoid ‘avatar’ as well as real life objects to make it look more realistic. User can take any avatar and can interact with objects, people, and scene through joystick or mouse. The VR technology utilizes the concepts of immersion and interactivity.
The use of technological solutions to improve health care is a constant and growing reality. Management of the patient´s vital statistics, anamnesis, risk factors, and information related to the communication between the patient and the healthcare organization are the focus of a solution proposed by Conte et al. [
29], with the main purpose being to present a platform to coordinate the whole clinical data and management within a common framework. Mobile apps, for their frequent use in daily lives of citizens, are also being used for e-learning and e-training purposes. An example is provided by Fonsa et al. [
30] that provides medical practitioners with a mobile app to use in e-training in imaging diagnosis, allowing them to perform measurements on those images, which represent an important component of healthcare personnel training.
In this paper, we start by presenting the context of what has been the approach so far to the education of medical practitioners (MPs) in the Public Private Mix (PPM) model of the Pakistan’s National TB Control Program. Based on the learning from the previously applied methods, we designed a survey that we gave to randomly selected MPs with the purpose of evaluating their experience with previous methodology and predisposition to enroll in a new program with a new approach. Based on the obtained results, we describe the requirements and architecture for an e-training platform that will be composed of 5 phases to allow MPs to have access to all the necessary information that will support them in provision of quality TB care. The proposed solution makes use of a virtual reality environment as well as gamification concepts to improve motivation and efficiency in the learning process. This paper also presents the User Experience UX) prototype for the first phase of the entire e-training platform.
3. Findings of Feedback and Readiness Survey
The questionnaire-based survey had the participation of 27 general practitioners that completed the survey with a 66% response rate. Average age of participating MPs was 44 years with an average of 15 years of medical practice experience in a primary healthcare setting.
A great degree of variation is found in the MPs’ assessment of a facilitator’s knowledge about a subject and gave an average score of 7.4 with a range 0 to 10. Similarly, a comparable level of variation was also found in the ratings of MPs for their satisfaction with the quality of training provided to them at the time of induction (i.e., mean score was 7 and range was 3 to 10). One respondent suggested improvement in a training facilitation role and said that:
“Facilitator should engage all participants and provide training in such a way that all participants understand it easily”.
In total, 44% of the MPs (n = 12) were discouraged with the length of the course and found it increasingly difficult to participate in 6-h long daily sessions for three days. More than half (n = 16) found it practically difficult to attend three days of training. Only 6 MPs were comfortable with a classroom-based training arrangement. One of the MPs explained his experience as:
“daily requirement for participation in training should be of two hours, because it becomes increasingly difficult to participate in long training sessions and shutting down clinical practice during that time”.
Another MP referred that “Basic (induction) training should be arranged in classroom-based settings while refresher trainings can be arranged at a clinic, because in basic training more time and concentration is required which one will not be able to assign due to patient load”.
One MP provided a suggestion on changing the training approach and said that “Overall quality of training was good; however, refresher sessions should be conducted on a regular basis with use of pre- and post-test to assess change in knowledge”.
Other suggestions included a scenario-based feedback session, manifestation and management of high-risk groups, and a session on behavior change communication strategies.
All of the MPs use mobile phone or computer for gaining medical knowledge either on a daily basis (n = 20) or occasionally (n = 7). However, all the MPs agreed that technology and need-based training modules will work better for them. Almost all of the MPs (n = 24) think that training provided at their clinic is more feasible and all the MPs (n = 27) liked the idea of an in-App quiz to assess learning outcomes. Further, 26 MPs thought that learning through game will improve their engagement and they identified different learning needs, such as diagnosis for TB (n = 7), treatment protocol (n = 10), and case management (n = 10). Twenty-four of the participating MPs thought that game scores from participating MPs will have a motivational effect, however, one MP said:
“I will not be comfortable to share my scores in game as my colleagues may develop a negative perception about me, however, I also think that it can motivate you to participate if you are performing well and you know that others will see your scores”.
One MP, having 65 years of age, said:
“In this mature age, we are generally afraid of technology related things because of our age, but I think whenever I overcame this fear in the past, I received great benefit from the use of technology. So, I think a technology-based training solution is a need of time and we should eliminate our fears pertaining to technology”.
All the participating MPs expressed their interest in prototype testing and liked the idea of accrediting this training course with the Pakistan Medical and Dental Council (a regulatory authority in Pakistan). Further, 80% of the MPs think that technology-based training methodology is better than classroom-based training methodology.
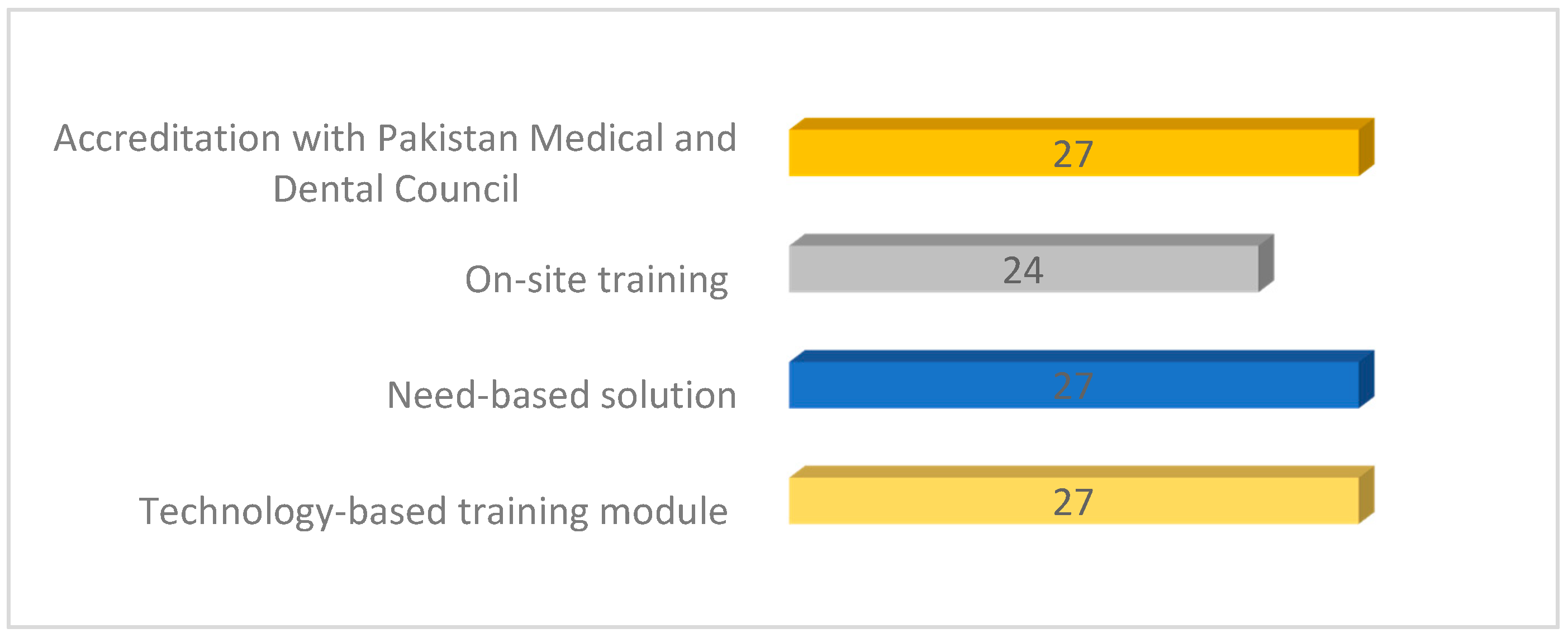
Figure 1 shows the four main aspects and major conclusions we were able to obtain from the survey and that are fundamental to the rest of this work.
4. Requirement Analysis
Taking into account the past experience of classroom-based training for the MPs, standardization in the practice of TB care and prevention services is yet to be achieved, which highlights potential concern for patient safety. Developing and testing an innovative approach or tool is highly needed to improve the current performance of the TB control program. Therefore, based on the survey results we described above, we propose to develop an immersive 3-dimensional environment of a typical clinical set-up to disseminate technical knowledge in an interactive manner. A virtual clinic will include display of TB-specific medical equipment and supplies along with general equipment. Head-mounted virtual reality devices, along with joysticks will be used for this purpose. On-site, on-demand, competency-based learning (beginner and expert levels), in-app quizzes for learning assessment or certification, and course accreditation from relevant authorities are key characteristics of the proposed concept or technology. To guide the content development of an e-training module, we have identified five key learning areas which are identified below:
Identification of Presumptive TB Case
Diagnosis Process
Intensive Phase of Treatment
Continuation Phase of Treatment
Treatment Outcome
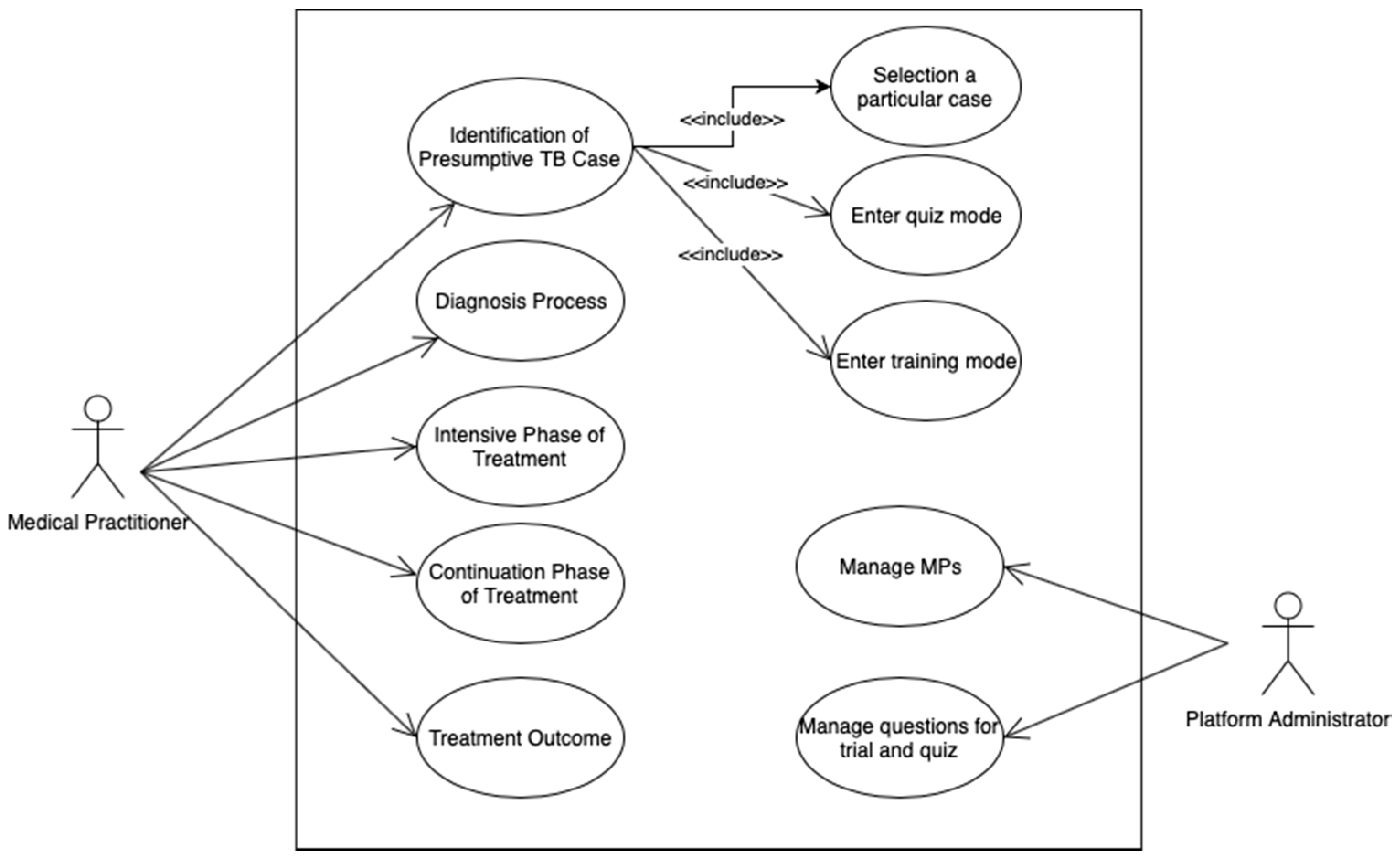
Figure 2 illustrates a Use Case Diagram with the main use cases for the two actors that are part of the system, the medical practitioner and platform administrator. The medical practitioner will have access to the five modules previously identified, each one representing a use case for him. The first use case, which we will focus on in detail in the rest of the paper, has other associated use cases that encompass selection of a particular case to work on, quiz mode, and training mode. The administrator has two use cases associated that allows him to manage medical practitioners and questions that can be used both for training and quiz mode.
The first learning area—and use case for the medical practitioner—corresponds to the first step in tuberculosis process of care, which is identification of a TB presumptive case. A list of simulated patients, also known as standardized patients, will allow user or trainee to select any particular case (e.g., pregnant lady, child, a regular smoker, diabetic patient, etc.). The recommended process of TB care will be shown in the virtual environment, which will be representative of the typical clinical set-up of primary and private healthcare settings, and users will be allowed to interact with it through joystick and audio-visual arrangements. A series of questions or steps will be displayed in a recommended sequence to identify a typical TB presumptive case. If the user chooses a wrong step or option, then recommended care guidelines will be displayed or narrated to facilitate the user’s learning. Clinical assessment of the presenting case will lead into referral of presumptive cases for the appropriate diagnostic test. At each step, users will be guided through the recommended process of care and common error in the clinical practice.
The diagnosis process involves implementation of recommended diagnostic algorithms. The user will have to choose the appropriate diagnostic test from a list of tests in a sequential manner. The interpretation of test results and further actions will then ensure correct and timely diagnosis, which is critically important for TB control efforts and patient safety. After the patient is diagnosed, an intensive phase of TB treatment is commenced that accounts for the measures of clinical importance, such as body weight. Correct dosage, side effect management, contact screening, and infection control measures are important aspects of the intensive phase. At the junction of initial phase and continuation phase, a laboratory test and its interpretation are important for treatment effectiveness. Once the intensive phase is completed, the continuation phase of TB treatment is started. Technically, this phase is similar to the intensive phase, with differences of treatment regimen and follow up laboratory tests. At the culmination of the continuation phase, declaring treatment outcomes becomes important because it involves consideration of various treatment-related indicators. It includes decisions regarding the termination of anti-TB drugs if treatment of a recommended period is completed. However, in the case of treatment interruptions or a non-standardized treatment regimen, a different outcome may occur, such as the patient may die or be declared as loss-to-follow-up or treatment failure.
In addition to five distinct learning areas, counselling, recording and reporting, patient safety, treatment compliance, and side effects management are important cross-cutting themes. These are important for achieving desirable treatment outcomes and for meaningful efforts towards breaking the chain of transmission, preventing relapse, and stopping the progression of disease severity.
5. Solution Proposal and Specification
In this section, we introduce the architecture proposed for this system and refer to the main actors and modules that compose the architecture. Moreover, we explain the general behavior of the platform, make some considerations regarding the user experience, present the detail of the first learning area, and end this section with a reference on how gamification elements will be incorporated as a motivational factor.
5.1. Architecture
Our proposed system architecture for developing a platform to facilitate e-training to MPs is presented in
Figure 2.
As depicted in
Figure 3, the system architecture encompasses MPs, patients, and a frontend application. MPs are the main actors in this system as the e-training platform is meant for their use, in order to promote their capacity to identify and treat TB cases. Patients are indirect actors of the system, as the purpose of the platform is to provide them better care when they are assisted by MPs. The frontend is the point of access MPs have to interact with the e-training solution, which can be accessed via a web browser, smartphone, or tablet. The frontend will interact via a data layer (REST web services) with a set of processes (logic layer) that support each one of the phases identified in the requirement analysis.
5.2. General Behavior
The e-training platform, named Dr. DOTS (after Directly Observed Treatment Short Courses), will require a login for each MP, which is approved by the administrator of the platform, before having access to the contents. There are two training programs: inception training and refresher training. The first time the MP uses the platform, he is automatically assigned with an inception training program that is characterized by the mandatory need of performing levels by sequence, to require that all knowledge has been learned. MPs can ask to join the refresher training after they successfully finish the inception training. The refresher training allows MPs to visualize and train specific levels and content, without having to follow any sequence. The main purpose is for MPs to train a specific content, depending on their needs.
5.3. Considerations on the User Experience
As users interact with products, systems, or services, their level of satisfaction or frustration establishes the quality of the User Experience (UX). Based on positive or negative responses and perceptions resulting from handling the product, system, or service, the UX is also determined by the number of steps and participants involved in the process. Also, understanding the UX involves understanding potential users’ priorities and needs, so they can be met through the implementation of credible solutions. This is determined through use by parameters such as functionality, performance, attributes, interactivity, and function features [
32]. Hence, to accomplish a pleasurable successful experience, it is fundamental to analyze the properties and aspects that may trigger positive responses, including the actions performed by the user, the surrounding space, and the product, service, or system in question. Therefore, the UX is not about how the service or product works internally, but how it operates externally, as users interact with such a service or product. Oriented by functionality, product design must therefore encompass product performance according to user expectations, characterized by users’ perceptions, emotions, references, and behaviors throughout the various stages of use. According to Roto et al. [
33], the User Experience process has properties and characteristics to follow, namely the context of use has physical aspects (surrounding environment, external noises, task to perform (purpose, time, importance of use) and socio-cultural factors (rules, beliefs, fashion, language). Users visualize the system engineering but are free to handle and control it. It is also argued by some authors that systems must allow user control in order to fit the user experience parameters. Therefore, user experience relies on the concept of usability. Usability translates the attributes defining the user friendliness of the interface. The term usability also regards methods to improve the ease-of-use during the design process [
34]. Usability empowers the creation of transparent interfaces so as not to hinder the process, allowing the user to control the environment during the interaction instead of becoming an obstacle. In the present context of research, usability may be simply understood as ensuring that something will work well, as defined by Stephen Krug [
35]. Usability relies on three concepts: effectiveness, efficiency, and satisfaction [
36]. Effectiveness relates to objective analysis and the possible level of accuracy achieved. Efficiency is the ratio of effectiveness and the amount of allocated resources. Satisfaction is established by the comfort and product acceptability by the users. This may be determined through subjective methods or goals. Interaction is apprehended by the use of or experience with other products. Therefore, the products that are used intuitively are those with similar characteristics to those developed earlier. The relevant past experience is thus transferred among products and probably also between settings. Hence, performance is affected by the level of familiarity of the user with similar technologies [
37]. This explains why good visual design is structured according to classical models and rationalization standards that have been present in societies since early stages. An important part of the user interface Graphic Design is the graphical presentation, including the layout, colors, icon design, and text fonts. Visual elements allow manipulation to achieve various emphases, modifiable by visual communication techniques, corresponding to the purpose of a message [
38]. Much of the interaction objects are limited by edges (i.e., lines) which are quite significant to assure the lightness of such objects. This occurs through the simple nature of the strokes and proposed clearance between edges and texts displayed on the screen, such as names, titles, headers, and labels, among others [
39]. Concerning the development of the platform logo, it was inspired by the prospective users (Medical Practitioners, MP), choosing as the main symbol the stethoscope (
Figure 4). However, after the development of the first proposal, the team members decided to incorporate signs of technological aspects, suggesting the introduction of 3-D glasses and some more detail to the image of the doctor. It was also suggested the lowering of the round side of the stethoscope, to replace the ‘o’ in Dots, as shown in
Figure 5.
However, the second proposal triggered some discussion regarding the color of the skin and hair of the avatar. It was decided to adopt the first solution, a color stain producing the silhouette of a human being, in this case a doctor. The final logo is presented in
Figure 6, the result of this long process. Concerning color, red was the first suggestion, but due to the sharp contrast, the compromise was a punctual use of red over the dominant grey color, creating visual tuning. The typeface family chosen for this process was Helvetica Neue. It coexists harmoniously with our own logo and allows full readability of the text, complemented with the Bold and Light versions. The product development was centered on the human being, a process beginning with users and their needs instead of starting with technology. The logo targets mainly the user, his characteristics and capabilities, and targets meeting his expectations, habits, and levels of recognition. Finally, the logo definition allowed the layout definition and subsequently all other visual elements.
5.4. Detailed Analysis of Phase 1
At this point, we have defined the behavior, functionalities, and UX prototypes for phase 1 corresponding to the Identification of a Presumptive TB Case, as introduced in
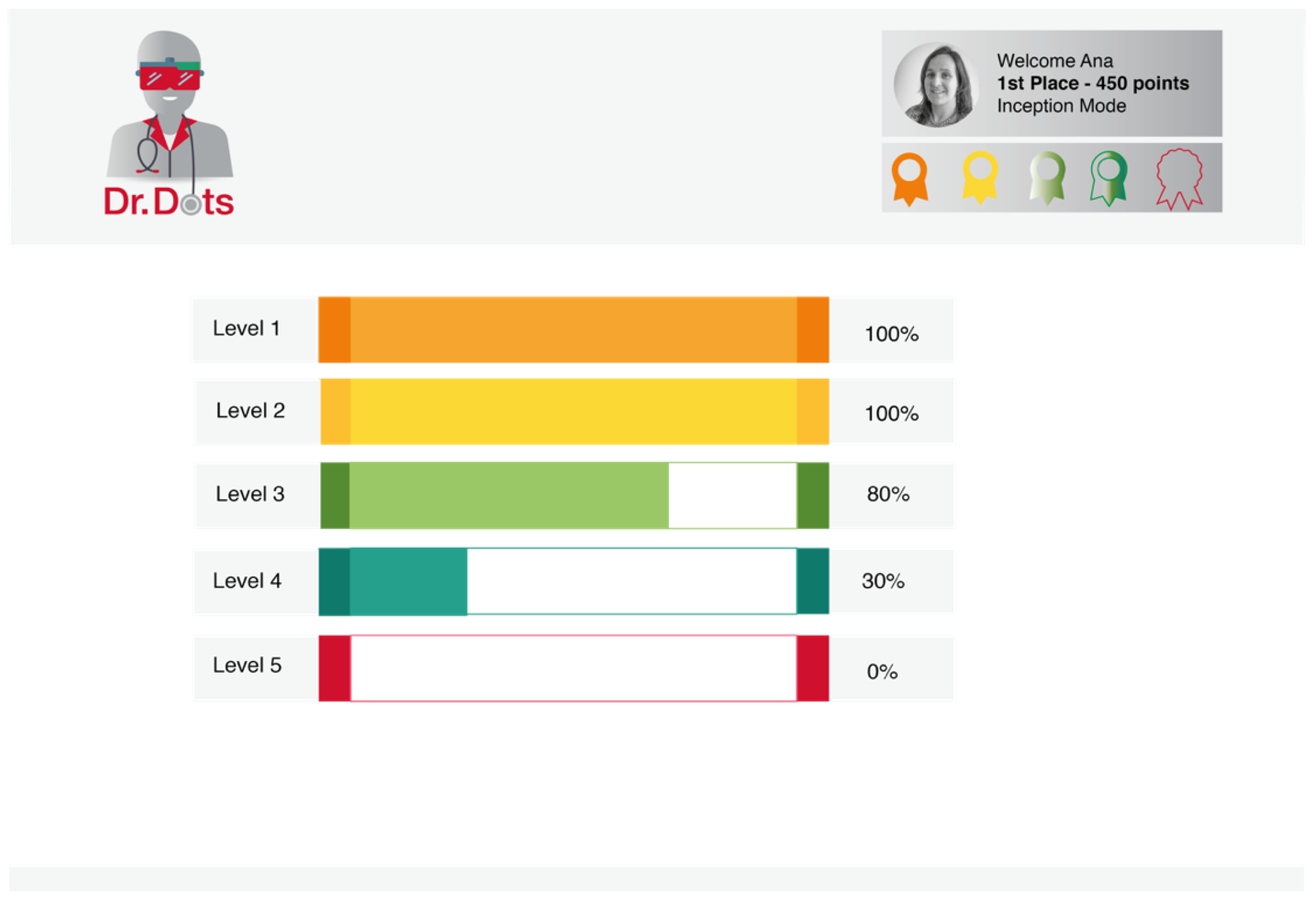
Section 4. Gamification strategies will be incorporated in this platform as a learning motivating factor. Leader boards, badges, scores, levels, progress bars, and rewards are some of the game elements that will be used throughout the e-training platform.
The first screen (shown in
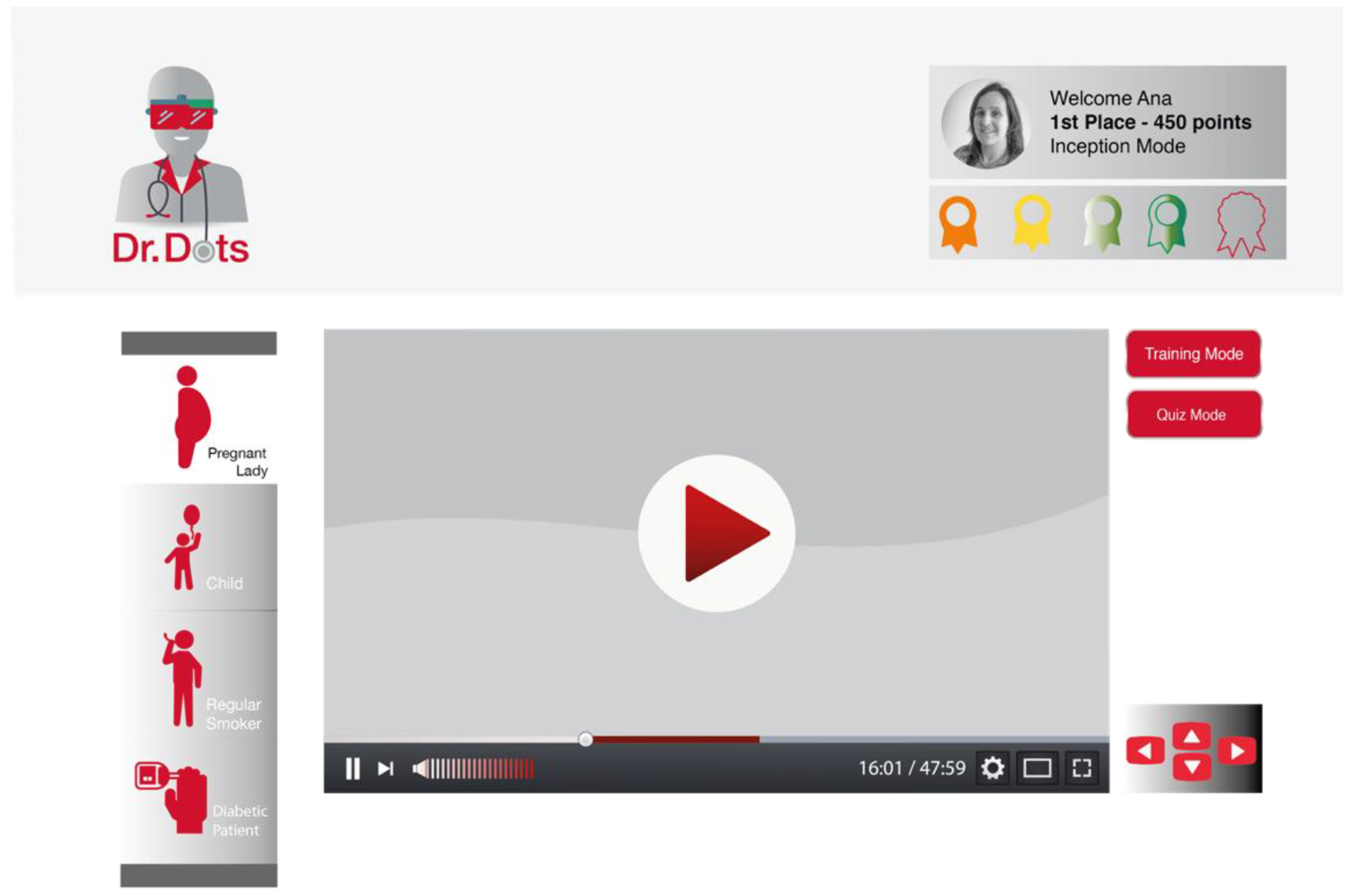
Figure 7), after the MP logs in, presents the user with the five different levels of the game, corresponding to the five key learning areas identified in the requirements. Each of the levels has an associated progress bar that shows the MP’s progress on that level. The MP can see their current registration type on the platform (inception or refresher), and according to that, they will be able to choose the specific content they want, or else they have to continue in the proposed sequence. At the top of the page, the MP can see his current classification (position and points earned) within the global leader board and the badge he has earned so far. In case of inception training, the MP can also see the percentage of completion of the entire training; in case of refresher training, the MP can see the last module taken in the e-training platform. When entering level 1, the MP is taken to a screen where he can choose the type of case he wants to practice (see
Figure 8). Some examples include a pregnant lady, child, regular smoker, or diabetic patient. After choosing one presumptive case, a virtual environment is shown with a 3D image that can be explored by the MP using the keyboard or joystick.
Each presumptive case has a training and a quiz mode. In training mode, the MP can select a question and answer to it. In case he fails to answer a question correctly, the MP is presented with a detailed explanation, so he can understand what was wrong with his selection.
5.5. Points and Level Progression
This e-training platform will use a point-based scoring system that will include accumulation of points as MP makes progress through learning areas. As stated earlier, the first time the user will be auto-assigned the inception training module and the MP will have to take all courses (corresponds to five learning areas) in sequence. Difficulty level also increases with later levels; therefore, each learning area will be assigned different points based on the difficulty level. For availing on-demand learning, which is only possible after inception training is completed, MP will be identified by the system as refresher training user. Since, different points are assigned to different learning areas therefore corresponding points of on-demand training will be added to MP’s personal scoreboard and based on points earned MP will be given rank within leader board. However, positions on leader boards will be determined as a result of combined scores of quiz marks (learning assessment) and points earned (learning) after completing one or more learning areas or levels.
6. Discussion
The solution we presented represents the design of an e-training platform and presents underlying logic, which was formed on the basis of Mercy Corps’ implementation experience coupled with MP feedback. Our e-training platform offers an on-site, on-demand, technology-enabled, interactive, accredited, and competency-based learning solution. These learning strategies were used to promote meaningful engagement and to achieve learning outcomes that are reflected by active, interactive, reflective, and authentic learning [
40]. Further, e-learning courses are advantageous because of the convenience and flexibility they offer to their users, hence permits them to undertake their working, personal, and family commitments [
41].
In most of the technology-based educational systems, information is usually presented in a static manner, resulting in less engagement and activity [
42]. Recently, personalized services have gained enormous attention because of the ability to address diverse information or learning needs of the users [
43]. Considering this, our e-training platform offers competency-based learning, which takes into account learners’ goals, existing knowledge, and their experience.
Our e-training platform gives an opportunity to the medical practitioner to see how fellow practitioners are making progress with learning, and they will also have opportunity to interact with a technical person or trainer to receive further assistance on any matter of their interest. It is noted that lack of interaction with a trainer and fellow practitioners is a disadvantage of e-learning courses [
41]. Additionally, without interaction, users or learners miss the opportunity to receive instant feedback [
44]. However, such issues are likely to be resolved with the use of blended learning, also known as hybrid e-training, which utilizes a combination of learning methods [
45], where cornerstone is a dependency, to promote a lifelong learning and knowledge society [
46].
In addition to hybrid e-training, the role of the trainer should also be carefully addressed in an e-learning environment which is not significantly different from trainer’s role in the traditional environments. However, new roles and competencies are to be developed to maximize learning outcomes in new environments [
47]. Therefore, our e-training platform does not eliminate the role of the trainer, and uses learning strategies (e.g., gamification, on-site, etc.) to achieve training goals. The game element is used to promote interactivity by providing system-generated instant responses and feedback. When the user is in learning mode and in assessment mode, the system will not generate prompts. However, in later stages of development and based on the actual usage data, our e-training platform will estimate the learner’s ability through item response theory [
48], and based on that a personalized and adaptive post-test scenario can be presented for better learning.