Spray-Dried Serum for Inhaled Antiviral Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Anti-SARS-CoV-2 Antiserum, Neat and Purified
2.2. Excipients and Buffers
2.3. Powder Preparation of BSA and Serum by Spray- and Freeze-Drying
2.3.1. Spray-Drying of Neat Serum and Purified Serum in Trehalose Formulations at Increasing Protein-to-Excipient Ratio
2.3.2. Freeze Drying of Bovine Serum Albumin (BSA) in Single-Component and Binary Formulations
2.3.3. Spray Drying of Neat Serum and Purified Serum in Selected Binary Formulations
2.4. Powder Characterization
2.4.1. Dynamic Light Scattering (DLS)
2.4.2. Scanning Electron Microscopy (SEM)
2.4.3. Particle Size Distribution by Laser Diffraction
2.4.4. Size Exclusion Chromatography (SEC)
2.4.5. Dynamic Angle of Repose
2.4.6. Thermogravimetric Analysis (TGA)
2.4.7. In Vitro Aerodynamic Performance Assessment
2.4.8. Anti-Spike Protein (SARS-CoV-2) Enzyme-Linked Immunosorbent Assay (ELISA)
2.5. Statistical Analysis
3. Results
3.1. Selection of the Protein-to-Excipient Ratio and Formulations for Spray Drying
3.2. Spray Drying of Neat Serum and Purified Serum in Selected Binary Formulation
3.2.1. Flowability and Relative Moisture Content
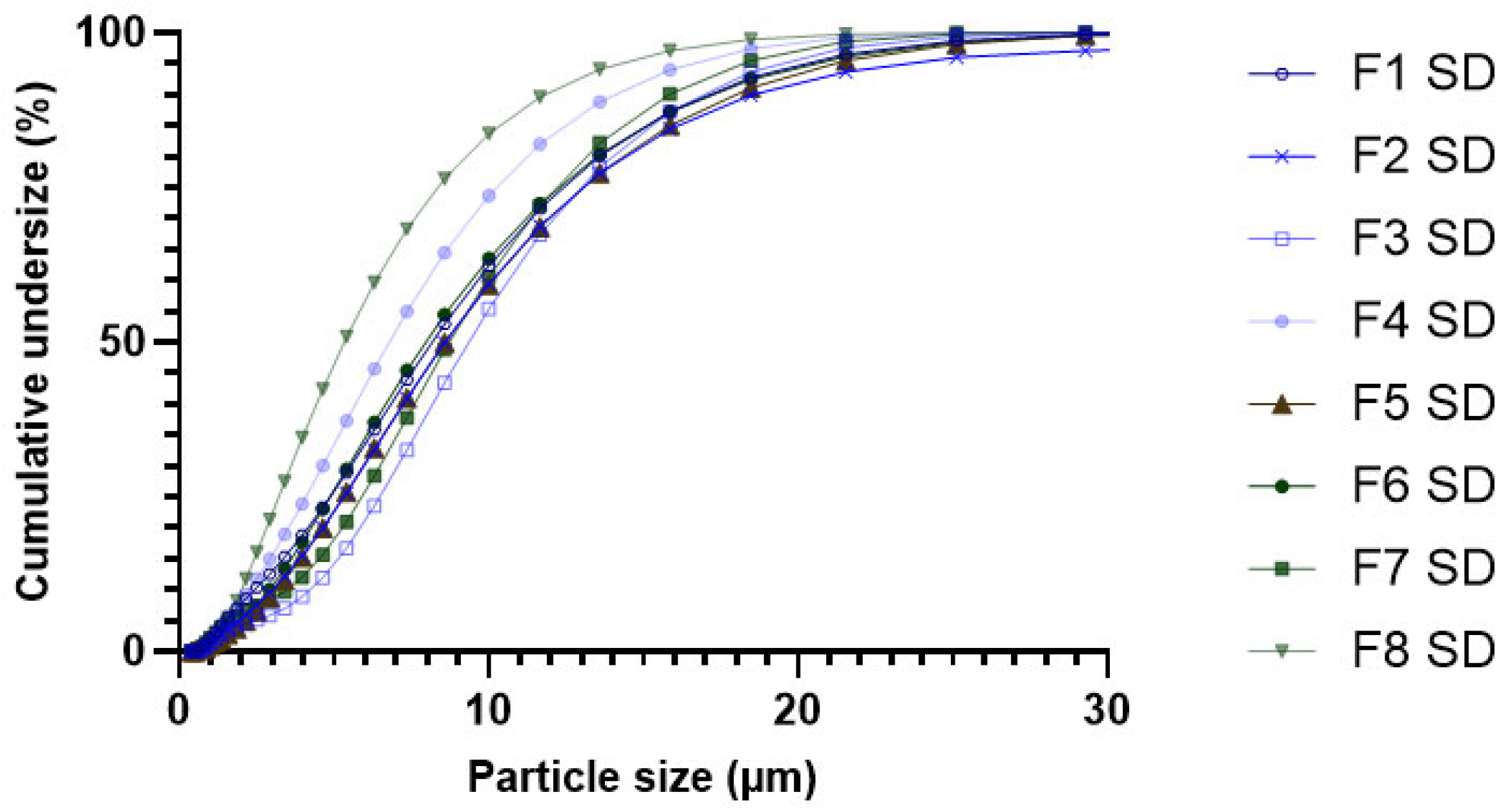
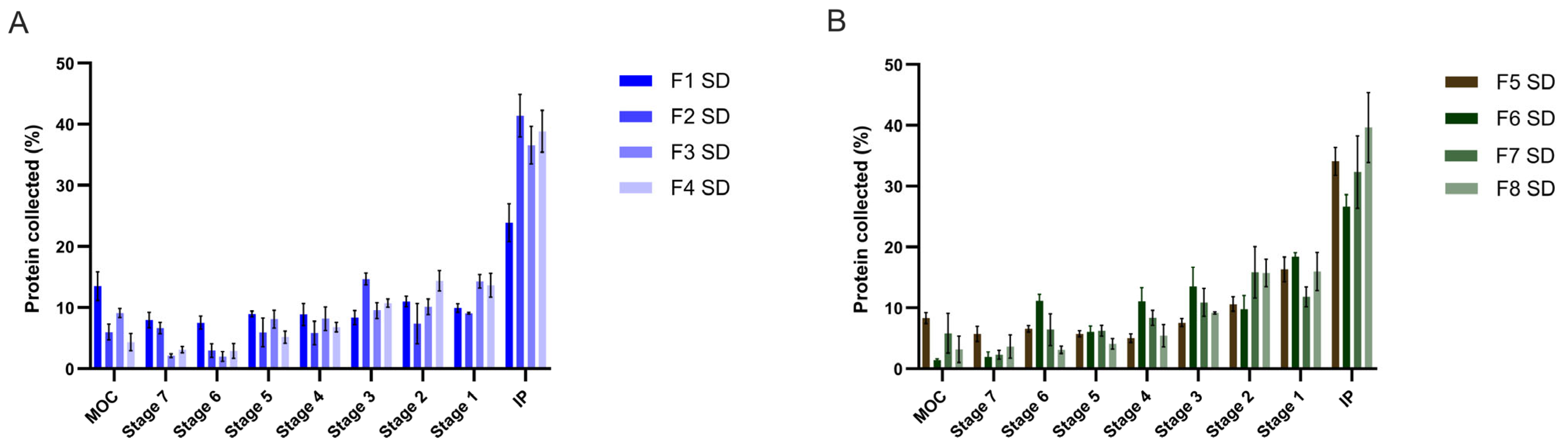
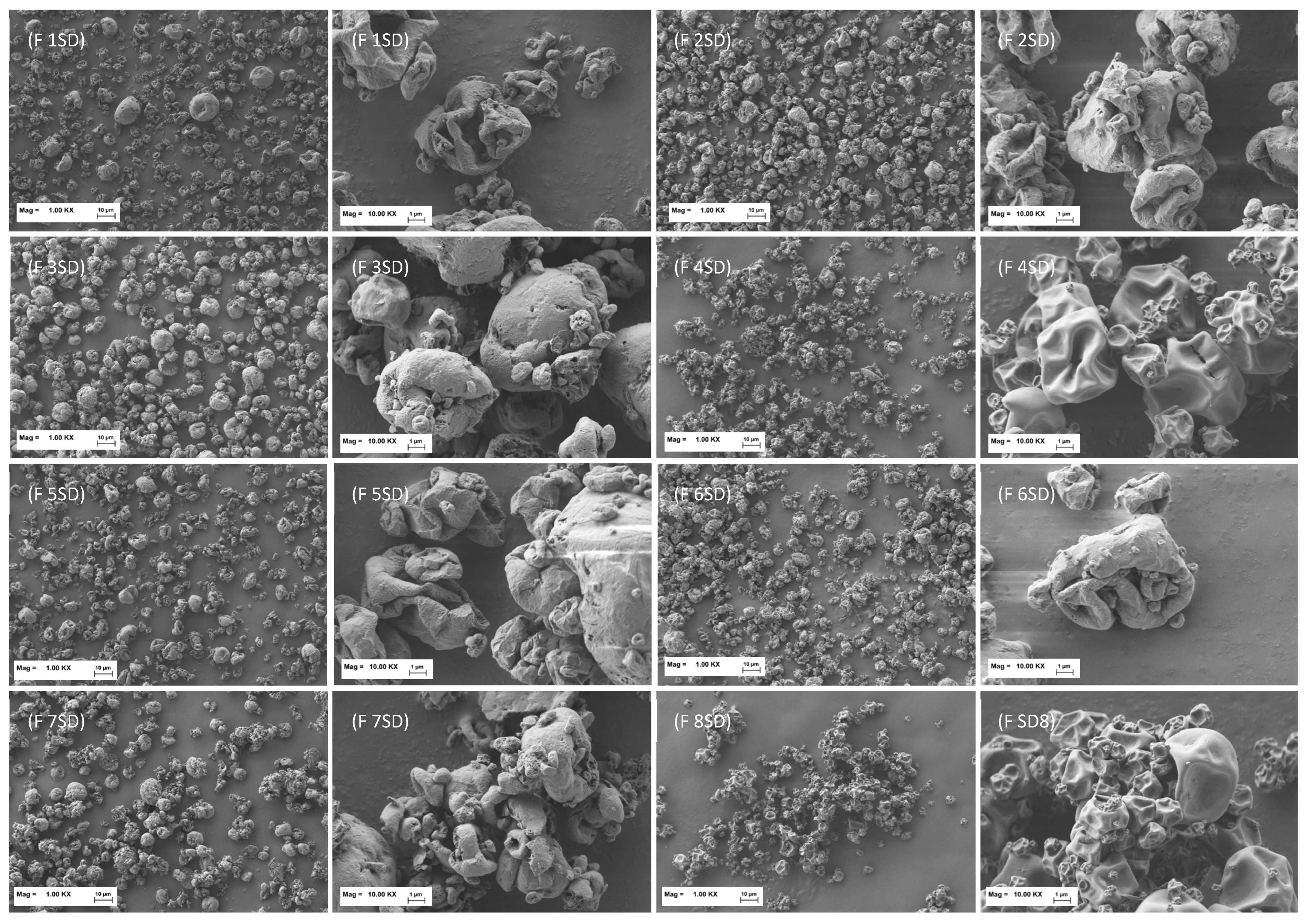
3.2.2. Particle Size Distribution (PSD), Aerodynamic Behavior and Morphology of Spray-Dried Formulations
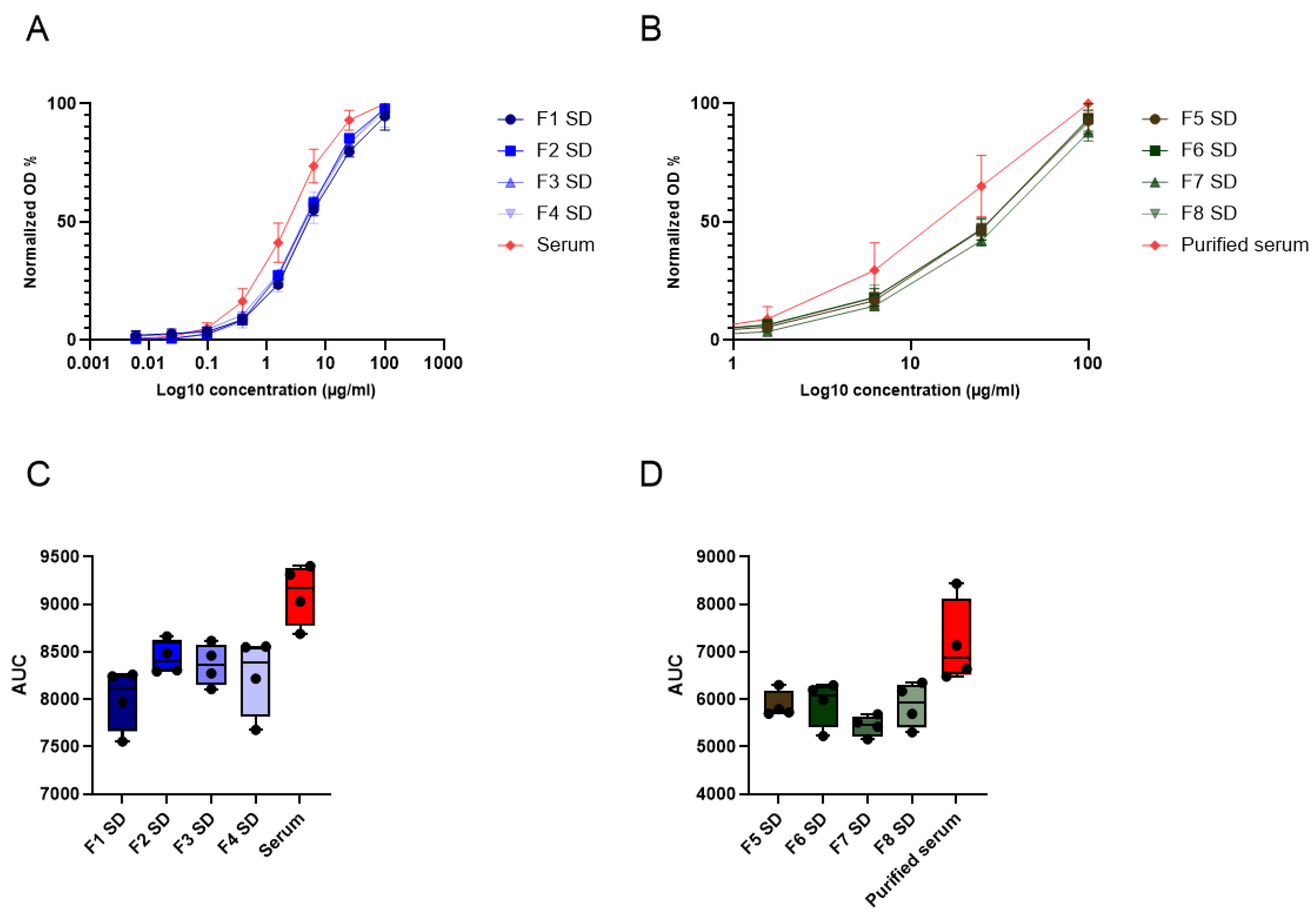
3.2.3. Particle Size, Residual Protein Activity and Estimated Pulmonary Activity of Spray-Dried Serum Proteins
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boon, H.; Meinders, A.-J.; van Hannen, E.J.; Tersmette, M.; Schaftenaar, E. Comparative analysis of mortality in patients admitted with an infection with influenza A/B virus, respiratory syncytial virus, rhinovirus, metapneumovirus or SARS-CoV-2. Influenza Other Respir. Viruses 2024, 18, e13237. [Google Scholar] [CrossRef] [PubMed]
- Sungnak, W.; Huang, N.; Becavin, C.; Berg, M.; Queen, R.; Litvinukova, M.; Talavera-Lopez, C.; Maatz, H.; Reichart, D.; Sampaziotis, F.; et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat. Med. 2020, 26, 681–687. [Google Scholar] [CrossRef]
- Morens, D.M.; Taubenberger, J.K.; Fauci, A.S. Rethinking next-generation vaccines for coronaviruses, influenzaviruses, and other respiratory viruses. Cell Host Microbe 2023, 31, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Kalil, A.C.; Thomas, P.G. Influenza virus-related critical illness: Pathophysiology and epidemiology. Crit. Care Lond. Engl. 2019, 23, 258. [Google Scholar] [CrossRef]
- Chaefer, I.-M.; Padera, R.F.; Solomon, I.H.; Kanjilal, S.; Hammer, M.M.; Hornick, J.L.; Sholl, L.M. In situ detection of SARS-CoV-2 in lungs and airways of patients with COVID-19. Mod. Pathol. 2020, 33, 2104–2114. [Google Scholar] [CrossRef] [PubMed]
- Shaibie, N.A.; Mohammad Faizal, N.D.F.; Buang, F.; Srichana, T.; Mohd Amin, M.C.I. Inhaled biologics for respiratory diseases: Clinical potential and emerging technologies. Drug Deliv. Transl. Res. 2025, 15, 4098–4114. [Google Scholar] [CrossRef]
- Chow, M.Y.T.; Pan, H.W.; Seow, H.C.; Lam, J.K.W. Inhalable neutralizing antibodies—Promising approach to combating respiratory viral infections. Trends Pharmacol. Sci. 2023, 44, 85–97. [Google Scholar] [CrossRef]
- Parray, H.A.; Shukla, S.; Perween, R.; Khatri, R.; Shrivastava, T.; Singh, V.; Murugavelu, P.; Ahmed, S.; Samal, S.; Sharma, C.; et al. Inhalation monoclonal antibody therapy: A new way to treat and manage respiratory infections. Appl. Microbiol. Biotechnol. 2021, 105, 6315–6332. [Google Scholar] [CrossRef]
- Chakraborty, C.; Sharma, A.R.; Bhattacharya, M.; Lee, S.-S. A Detailed Overview of Immune Escape, Antibody Escape, Partial Vaccine Escape of SARS-CoV-2 and Their Emerging Variants With Escape Mutations. Front. Immunol. 2022, 13, 801522. [Google Scholar] [CrossRef]
- Struble, E.B.; Rawson, J.M.O.; Stantchev, T.; Scott, D.; Shapiro, M.A. Uses and Challenges of Antiviral Polyclonal and Monoclonal Antibody Therapies. Pharmaceutics 2023, 15, 1538. [Google Scholar] [CrossRef]
- Jacque, E.; Chottin, C.; Laubreton, D.; Nogre, M.; Ferret, C.; de Marcos, S.; Baptista, L.; Drajac, C.; Mondon, P.; De Romeuf, C.; et al. Hyper-Enriched Anti-RSV Immunoglobulins Nasally Administered: A Promising Approach for Respiratory Syncytial Virus Prophylaxis. Front. Immunol. 2021, 12, 683902. [Google Scholar] [CrossRef]
- Imsuwansri, T.; Jongthitinon, T.; Pojdoung, N.; Meesiripan, N.; Sakarin, S.; Boonkrai, C.; Wongtangprasert, T.; Phakham, T.; Audomsun, T.; Attakitbancha, C.; et al. Assessment of safety and intranasal neutralizing antibodies of HPMC-based human anti-SARS-CoV-2 IgG1 nasal spray in healthy volunteers. Sci. Rep. 2023, 13, 15648. [Google Scholar] [CrossRef]
- Omidian, H.; Nokhodchi, A.; Babanejad, N. Dry Powder Inhalers for Delivery of Synthetic Biomolecules. Pharmaceuticals 2025, 18, 175. [Google Scholar] [CrossRef] [PubMed]
- Chang, R.Y.K.; Chan, H.-K. Advancements in Particle Engineering for Inhalation Delivery of Small Molecules and Biotherapeutics. Pharm. Res. 2022, 39, 3047–3061. [Google Scholar] [CrossRef] [PubMed]
- Shetty, N.; Cipolla, D.; Park, H.; Zhou, Q.T. Physical stability of dry powder inhaler formulations. Expert Opin. Drug Deliv. 2020, 17, 77–96. [Google Scholar] [CrossRef]
- Xu, H.; Sahakijpijarn, S.; Moon, C.; Emig, C.J.; Mena, M.; Henry, S.J.; Vitug, A.; Ventura, C.J.; Kuehl, P.J.; Revelli, D.; et al. Inhalable dry powders of a monoclonal antibody against SARS-CoV-2 virus made by thin-film freeze-drying. Int. J. Pharm. 2024, 662, 124511. [Google Scholar] [CrossRef] [PubMed]
- Seow, H.C.; Cai, J.-P.; Pan, H.W.; Luo, C.; Wen, K.; Situ, J.; Wang, K.; Cao, H.; Leung, S.W.; Yuan, S.; et al. Neutralisation of SARS-CoV-2 by monoclonal antibody through dual targeting powder formulation. J. Control. Release 2023, 358, 128–141. [Google Scholar] [CrossRef]
- Chang, L.L.; Shepherd, D.; Sun, J.; Ouellette, D.; Grant, K.L.; Tang, X.C.; Pikal, M.J. Mechanism of protein stabilization by sugars during freeze-drying and storage: Native structure preservation, specific interaction, and/or immobilization in a glassy matrix? J. Pharm. Sci. 2005, 94, 1427–1444. [Google Scholar] [CrossRef]
- Pinto, J.T.; Faulhammer, E.; Dieplinger, J.; Dekner, M.; Makert, C.; Nieder, M.; Paudel, A. Progress in spray-drying of protein pharmaceuticals: Literature analysis of trends in formulation and process attributes. Dry Technol. 2021, 39, 1415–1446. [Google Scholar] [CrossRef]
- Mensink, M.A.; Frijlink, H.W.; van der Voort Maarschalk, K.; Hinrichs, W.L.J. How sugars protect proteins in the solid state and during drying (review): Mechanisms of stabilization in relation to stress conditions. Eur. J. Pharm. Biopharm. 2017, 114, 288–295. [Google Scholar] [CrossRef]
- Mensink, M.A.; Van Bockstal, P.-J.; Pieters, S.; De Meyer, L.; Frijlink, H.W.; van der Voort Maarschalk, K.; Hinrichs, W.L.; De Beer, T. In-line near infrared spectroscopy during freeze-drying as a tool to measure efficiency of hydrogen bond formation between protein and sugar, predictive of protein storage stability. Int. J. Pharm. 2015, 496, 792–800. [Google Scholar] [CrossRef] [PubMed]
- Ramezani, V.; Vatanara, A.; Seyedabadi, M.; Nabi Meibodi, M.; Fanaei, H. Application of cyclodextrins in antibody microparticles: Potentials for antibody protection in spray drying. Drug Dev. Ind. Pharm. 2017, 43, 1103–1111. [Google Scholar] [CrossRef]
- Ramezani, V.; Vatanara, A.; Najafabadi, A.R.; Shokrgozar, M.A.; Khabiri, A.; Seyedabadi, M. A comparative study on the physicochemical and biological stability of IgG1 and monoclonal antibodies during spray drying process. Daru J. Fac. Pharm. Tehran Univ. Med. Sci. 2014, 22, 31. [Google Scholar] [CrossRef]
- Serno, T.; Geidobler, R.; Winter, G. Protein stabilization by cyclodextrins in the liquid and dried state. Adv. Drug Deliv. Rev. 2011, 63, 1086–1106. [Google Scholar] [CrossRef]
- Ajmera, A.; Scherließ, R. Stabilisation of proteins via mixtures of amino acids during spray drying. Int. J. Pharm. 2014, 463, 98–107. [Google Scholar] [CrossRef]
- Alhajj, N.; O’Reilly, N.J.; Cathcart, H. Leucine as an excipient in spray dried powder for inhalation. Drug Discov. Today. 2021, 26, 2384–2396. [Google Scholar] [CrossRef]
- Mutukuri, T.T.; Ling, J.; Du, Y.; Su, Y.; Zhou, Q.T. Effect of Buffer Salts on Physical Stability of Lyophilized and Spray-Dried Protein Formulations Containing Bovine Serum Albumin and Trehalose. Pharm. Res. 2023, 40, 1355–1371. [Google Scholar] [CrossRef]
- Bianchera, A.; Donofrio, G.; Sonvico, F.; Bettini, R. Dry powder formulations of hyperimmune serum. Drug Deliv. Transl. Res. 2025, 15, 1330–1341. [Google Scholar] [CrossRef] [PubMed]
- Bosquillon, C.; Lombry, C.; Préat, V.; Vanbever, R. Influence of formulation excipients and physical characteristics of inhalation dry powders on their aerosolization performance. J. Control. Release 2001, 70, 329–339. [Google Scholar] [CrossRef] [PubMed]
- Nouraei, M.S.; Faghihi, H.; Najafabadi, A.R.; Zadeh, A.H.M.; Darabi, M.; Vatanara, A. Human Serum Albumin, a Suitable Candidate to Stabilize Freeze-Dried IgG in Combination with Trehalose: Central Composite Design. AAPS PharmSciTech 2019, 20, 327. [Google Scholar] [CrossRef]
- Ko, S.K.; Björkengren, G.; Berner, C.; Winter, G.; Harris, P.; Peters, G.H.J. Combining Molecular Dynamics Simulations and Biophysical Characterization to Investigate Protein-Specific Excipient Effects on Reteplase during Freeze Drying. Pharmaceutics 2023, 15, 1854. [Google Scholar] [CrossRef]
- Technical Note: ANCFGAMSULF 0511. Available online: https://documents.thermofisher.com/TFS-Assets/LED/Product-Bulletins/D01821~.pdf (accessed on 6 September 2025).
- Jena, S.; Krishna Kumar, N.S.; Aksan, A.; Suryanarayanan, R. Stability of lyophilized albumin formulations: Role of excipient crystallinity and molecular mobility. Int. J. Pharm. 2019, 569, 118568. [Google Scholar] [CrossRef]
- Lo Presti, K.; Jégo, M.; Frieß, W. “The More, the Better?”: The Impact of Sugar-to-Protein Molar Ratio in Freeze-Dried Monoclonal Antibody Formulations on Protein Stability. Mol. Pharm. 2024, 21, 6484–6490. [Google Scholar] [CrossRef]
- Jachimska, B.; Pajor, A. Physico-chemical characterization of bovine serum albumin in solution and as deposited on surfaces. Bioelectrochemistry 2012, 87, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Protein Sizing with Differential Dynamic Microscopy|Macromolecules. Available online: https://pubs.acs.org/doi/10.1021/acs.macromol.3c00782 (accessed on 28 September 2025).
- Stetefeld, J.; McKenna, S.A.; Patel, T.R. Dynamic light scattering: A practical guide and applications in biomedical sciences. Biophys. Rev. 2016, 8, 409–427. [Google Scholar] [CrossRef]
- Molodenskiy, D.; Shirshin, E.; Tikhonova, T.; Gruzinov, A.; Peters, G.; Spinozzi, F. Thermally induced conformational changes and protein–protein interactions of bovine serum albumin in aqueous solution under different pH and ionic strengths as revealed by SAXS measurements. Phys. Chem. Chem. Phys. 2017, 19, 17143–17155. [Google Scholar] [CrossRef]
- Pan, H.W.; Guo, J.; Zhu, L.; Leung, S.W.S.; Zhang, C.; Lam, J.K.W. Enhanced powder dispersion of dual-excipient spray-dried powder formulations of a monoclonal antibody and its fragment for local treatment of severe asthma. Int. J. Pharm. 2023, 644, 123272. [Google Scholar] [CrossRef] [PubMed]
- Gislefoss, R.E.; Lauritzen, M.; Langseth, H.; Mørkrid, L. Effect of multiple freeze-thaw cycles on selected biochemical serum components. Clin Chem. Lab. Med. CCLM 2017, 55, 967–973. [Google Scholar] [CrossRef]
- Mangal, S.; Meiser, F.; Tan, G.; Gengenbach, T.; Denman, J.; Rowles, M.R.; Larson, I.; Morton, D.A. Relationship between surface concentration of l-leucine and bulk powder properties in spray dried formulations. Eur. J. Pharm. Biopharm. 2015, 94, 160–169. [Google Scholar] [CrossRef]
- Li, L.; Sun, S.; Parumasivam, T.; Denman, J.A.; Gengenbach, T.; Tang, P.; Mao, S.; Chan, H.-K. l-Leucine as an excipient against moisture on in vitro aerosolization performances of highly hygroscopic spray-dried powders. Eur. J. Pharm. Biopharm. 2016, 102, 132–141. [Google Scholar] [CrossRef]
- You, Y.; Zhao, M.; Liu, G.; Tang, X. Physical characteristics and aerosolization performance of insulin dry powders for inhalation prepared by a spray drying method. J. Pharm. Pharmacol. 2007, 59, 927–934. [Google Scholar] [CrossRef] [PubMed]
- Emery, E.; Oliver, J.; Pugsley, T.; Sharma, J.; Zhou, J. Flowability of moist pharmaceutical powders. Powder Technol. 2009, 189, 409–415. [Google Scholar] [CrossRef]
- Sandler, N.; Reiche, K.; Heinämäki, J.; Yliruusi, J. Effect of Moisture on Powder Flow Properties of Theophylline. Pharmaceutics 2010, 2, 275–290. [Google Scholar] [CrossRef]
- Geethambika, S.B.; Veerendrasimha, V.S.H.; Prakash, A.K.; Pasagadi, A.S.; Franklin, M.E.E.; Ambrose, R.P.K.; Pushpadass, H.A. Effect of moisture content on physical and flow properties of milk-millet powders. J. Food Process Eng. 2023, 46, e14198. [Google Scholar] [CrossRef]
- Dieplinger, J.; Pinto, J.T.; Dekner, M.; Brachtl, G.; Paudel, A. Impact of Different Saccharides on the In-Process Stability of a Protein Drug During Evaporative Drying: From Sessile Droplet Drying to Lab-Scale Spray Drying. Pharm. Res. 2023, 40, 1283–1298. [Google Scholar] [CrossRef]
- Encinas-Basurto, D.; FAcosta, M.; Babu Eedara, B.; RFineman, J.; MBlack, S.; MMansour, H. Design and comprehensive characterization of dry powder inhalation aerosols of simvastatin DPPC/DPPG lung surfactant-mimic nanoparticles/microparticles for pulmonary nanomedicine. RSC Adv. 2024, 14, 29413–29427. [Google Scholar] [CrossRef]
- Sou, T.; Orlando, L.; McIntosh, M.P.; Kaminskas, L.M.; Morton, D.A.V. Investigating the interactions of amino acid components on a mannitol-based spray-dried powder formulation for pulmonary delivery: A design of experiment approach. Int. J. Pharm. 2011, 421, 220–229. [Google Scholar] [CrossRef]
- Ahmed, S.; Mansour, M.; Ishak, R.A.H.; Mortada, N.D. Customizable resveratrol spray-dried micro-composites for inhalation as a promising contender for treatment of idiopathic pulmonary fibrosis. Int. J. Pharm. 2023, 642, 123117. [Google Scholar] [CrossRef]
- Laube, B.; Janssens, H.; de Jongh, F.; Devadason, S.; Dhand, R.; Diot, P.; Everard, M.; Horvath, I.; Navalesi, P.; Voshaar, T.; et al. What the pulmonary specialist should know about the new inhalation therapies. Eur. Respir. J. 2011, 37, 1308–1417. [Google Scholar] [CrossRef]
- Zhang, L.; Tong, Z.; Zhang, Y.; Yu, A. Numerical study on the deposition distribution and mechanism of inhaled drug particles in various regions of the realistic inhaler-airway model. Powder Technol. 2025, 449, 120402. [Google Scholar] [CrossRef]
- Hofmann, W. Modelling inhaled particle deposition in the human lung—A review. J. Aerosol. Sci. 2011, 42, 693–724. [Google Scholar] [CrossRef]
- Chew, N.Y.K.; Chan, H.-K. Use of Solid Corrugated Particles to Enhance Powder Aerosol Performance. Pharm. Res. 2001, 18, 1570–1577. [Google Scholar] [CrossRef] [PubMed]
- Emami, F.; Vatanara, A.; Park, E.J.; Na, D.H. Drying Technologies for the Stability and Bioavailability of Biopharmaceuticals. Pharmaceutics 2018, 10, 131. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Mocking-Bode, H.C.M.; Van Den Hoek, I.A.F.; Theunissen, M.; Voudouris, P.; Meinders, M.B.J.; Sagis, L.M. The impact of heating and freeze or spray drying on the interface and foam stabilising properties of pea protein extracts: Explained by aggregation and protein composition. Food Hydrocoll. 2022, 133, 107913. [Google Scholar] [CrossRef]
- Burgess, D.J.; Ponsart, S. β-Glucuronidase activity following complex coacervation and spray drying microencapsulation. J. Microencapsul 1998, 15, 569–579. [Google Scholar] [CrossRef]
- Jain, K.; Salamat-Miller, N.; Taylor, K. Freeze–thaw characterization process to minimize aggregation and enable drug product manufacturing of protein based therapeutics. Sci. Rep. 2021, 11, 11332. [Google Scholar] [CrossRef]
| Formulation | Proteins | Trehalose Conc. (mg/mL) | Solid Content Conc. (mg/mL) | Protein/Excipient Ratio |
|---|---|---|---|---|
| A | Neat serum | 3.5 | 5 | 1:2.3 |
| B | Neat serum | 8.5 | 10 | 1:5.7 |
| C | Neat serum | 18.5 | 20 | 1:12.3 |
| D | Neat serum | 28.5 | 30 | 1:19 |
| E | Purified serum | 3.5 | 5 | 1:2.3 |
| F | Purified serum | 8.5 | 10 | 1:5.7 |
| G | Purified serum | 18.5 | 20 | 1:12.3 |
| H | Purified serum | 28.5 | 30 | 1:19 |
| Formulation | Excipients | Solvent | Moisture Content (% w/w) | Main Peak Size (nm) | Intensity of Peak (%) |
|---|---|---|---|---|---|
| 1 FD | Trehalose | KP 25 mM | 7.0 ± 3.6 | 9.33 ± 0.47 | 52.1 ± 5.3 |
| 2 FD | Trehalose | Water | 5.2 ± 0.7 | 9.22 ± 0.64 | 47.3 ± 3.5 |
| 3 FD | Mannitol | KP 25 mM | 6.1 ± 1.7 | 10.04 ± 22.27 | 51.4 ± 1.6 |
| 4 FD | Mannitol | Water | 2.9 ± 0.7 | 8.44 ± 0.52 | 61.7 ± 4.9 |
| 5 FD | HPβCD | KP 25 mM | 5.3 ± 0.2 | 8.70 ± 0.41 | 52.0 ± 7.5 |
| 6 FD | HPβCD | Water | 7.4 ± 1.2 | 9.09 ± 0.26 | 52.4 ± 4.2 |
| 7 FD | Phenylalanine | Water | 12.3 | 8.93 ± 0.72 | 71.6 ± 14.3 |
| 8 FD | L-arginine | KP 25 mM | 10.8 ± 2.0 | 9.11 ± 0.32 | 55.2 ± 4.6 |
| 9 FD | L-arginine | Water | 5.3 ± 0.6 | 8.93 ± 0.34 | 72.6 ± 10.5 |
| 10 FD | L-leucine | KP 25 mM | 6.4 ± 2.5 | 9.45 ± 0.28 | 55.1 ± 9.7 |
| 11 FD | L-leucine | Water | 3.1 ± 0.0 | 8.89 ± 0.29 | 59.8 ± 6.2 |
| 12 FD | Glycine | KP 25 mM | 6.4 ± 0.9 | 8.62 ± 0.86 | 59.2 ± 10.4 |
| 13 FD | Glycine | Water | 3.6 ± 0.5 | 8.82 ± 0.45 | 55.4 ± 7.0 |
| 14 FD | Trehalose/ L-phenylalanine | Water | 6.1 ± 0.9 | 9.93 ± 0.94 | 48.6 ± 7.1 |
| 15 FD | Trehalose/L-arginine | KP 25 mM | 22.0 ± 18.8 | 9.87 ± 2.08 | 60.5 ± 17.7 |
| 16 FD | Trehalose/L-arginine | Water | 5.4 ± 0.4 | 9.67 ± 0.38 | 80.0 ± 2.6 |
| 17 FD | Trehalose/L-leucine | KP 25 mM | 5.3 ± 2.8 | 10.42 ± 1.58 | 61.9 ± 12.7 |
| 18 FD | Trehalose/L-leucine | Water | 4.4 ± 0.3 | 10.29 ± 1.31 | 86.3 ± 6.2 |
| 19 FD | Trehalose/Glycine | KP 25 mM | 9.6 ± 2.3 | 10.48 ± 0.83 | 77.9 ± 2.6 |
| 20 FD | Trehalose/Glycine | Water | 7.9 | 7.97 ± 1.20 | 41.3 ± 4.3 |
| 21 FD | Mannitol/ L-phenylalanine | Water | 2.3 ± 0.9 | 7.46 ± 0.86 | 55.9 ± 1.4 |
| 22 FD | Mannitol/L-arginine | KP 25 mM | 13.5 | 11.85 ± 2.63 | 15.0 ± 1.8 |
| 23 FD | Mannitol/L-arginine | Water | 3.3 ± 0.5 | 8.61 ± 0.61 | 75.6 ± 1.0 |
| 24 FD | Mannitol/L-leucine | KP 25 mM | 5.8 ± 3.9 | 8.16 ± 1.54 | 31.3 ± 19.7 |
| 25 FD | Mannitol/L-leucine | Water | 3.9 ± 1.3 | 8.72 ± 0.14 | 61.1 ± 2.8 |
| 26 FD | Mannitol/Glycine | KP 25 mM | 9.1 ± 1.9 | 9.26 ± 0.93 | 45.8 ± 13.0 |
| 27 FD | Mannitol/Glycine | Water | 3.3 ± 1.4 | 9.18 ± 0.30 | 76.0 ± 4.3 |
| 28 FD | HPβCD/ L-phenylalanine | Water | 6.1 ± 0.9 | 11.84 ± 1.90 | 64.3 ± 13.3 |
| 29 FD | HPβCD/L-arginine | KP 25 mM | 6.6 ± 5.2 | 9.17 ± 0.74 | 53.3 ± 4.4 |
| 30 FD | HPβCD/L-arginine | Water | 5.1 ± 1.1 | 9.33 ± 0.32 | 55.7 ± 7.4 |
| 31 FD | HPβCD/L-leucine | KP 25 mM | 5.9 ± 5.0 | 10.80 ± 0.59 | 86.1 ± 2.0 |
| 32 FD | HPβCD/L-leucine | Water | 4.2 ± 1.6 | 13.11 ± 0.36 | 86.3 ± 2.8 |
| 33 FD | HPβCD/Glycine | KP 25 mM | 9.8 ± 0.3 | 11.70 ± 0.48 | 82.8 ± 0.6 |
| 34 FD | HPβCD/Glycine | Water | 7.4 ± 3.0 | 9.85 ± 0.89 | 59.4 ± 14.6 |
| Main Peak | Secondary Peak | |||||
|---|---|---|---|---|---|---|
| Sample | Moisture Content (% w/w) | Z-Average (d.nm) | Size (nm) | Intensity (%) | Size (nm) | Intensity (%) |
| Neat serum | - | 79.5 ± 1.4 | 144.0 ± 33.9 | 90.8 ± 2.4 | 12.5 ± 0.6 | 7.1 ± 0.7 |
| 16 S-FD | 6.76 | 141.3 ± 0.5 | 217.1 ± 11.5 | 96.6 ± 1.5 | 8.4 ± 0.0 | 2.0 ± 0.0 |
| 18 S-FD | 5.25 | 85.9 ± 0.2 | 149.7 ± 25.8 | 92.8 ± 3.0 | 13.5 ± 1.0 | 8.0 ± 1.4 |
| 19 S-FD | 9.10 | 126.7 ± 3.9 | 226.9 ± 63.2 | 85.8 ± 19.7 | 46.9 ± 52.1 | 18.9 ± 23.1 |
| 23 S-FD | 7.51 | 138.7 ± 6.9 | 199.2 ± 12.9 | 95.8 ± 4.4 | 15.6 ± 0.0 | 5.6 ± 0.0 |
| 27 S-FD | 5.41 | 114.1 ± 3.1 | 170.0 ± 6.8 | 95.3 ± 5.1 | 15.7 ± 16.1 | 4.7 ± 5.1 |
| 31 S-FD | 6.67 | 93.2 ± 2.3 | 141.7 ± 5.6 | 93.0 ± 0.7 | 13.8 ± 1.4 | 6.0 ± 0.3 |
| 32 S-FD | 4.95 | 84.1 ± 3.4 | 129.8 ± 6.8 | 92.5 ± 1.9 | 15.3 ± 2.3 | 7.2 ± 1.6 |
| 33 S-FD | 9.59 | 102.8 ± 1.6 | 152.6 ± 10.3 | 94.8 ± 3.4 | 10.0 ± 8.8 | 3.6 ± 3.1 |
| Formulation Nr. | Proteins | Excipients | Solvent | % Process Yield |
|---|---|---|---|---|
| 1 SD | Neat serum | HPβCD/L-leucine | Water | 77.5 |
| 2 SD | Neat serum | HPβCD/L-leucine | KP 25 mM | 79.6 |
| 3 SD | Neat serum | Trehalose/L-leucine | Water | 76.4 |
| 4 SD | Neat serum | HPβCD/Glycine | KP 25 mM | 43.1 |
| 5 SD | Purified serum | HPβCD/L-leucine | Water | 78.2 |
| 6 SD | Purified serum | HPβCD/L-leucine | KP 25 mM | 79.9 |
| 7 SD | Purified serum | Trehalose/L-leucine | Water | 69.7 |
| 8 SD | Purified serum | HPβCD/Glycine | KP 25 mM | 81.4 |
| Formulation Nr. | Dynamic Angle of Repose (°) | Flowability | Relative Moisture Content (% w/w) |
|---|---|---|---|
| 1 SD | 37.10 ± 0.28 | Fair | 2.61 |
| 2 SD | 39.16 ± 0.26 | Fair | 4.32 |
| 3 SD | 42.53 ± 0.59 | Passable | 3.3 |
| 4 SD | 48.09 ± 0.75 | Poor | 5.68 |
| 5 SD | 50.76 ± 0.66 | Poor | 2.52 |
| 6 SD | 45.55 ± 0.78 | Passable–Poor | 3.43 |
| 7 SD | 51.49 ± 0.49 | Poor | 2.95 |
| 8 SD | 28.68 ± 0.40 | Excellent | 6.29 |
| Formulation Nr. | DV10 | DV50 | DV90 | Span |
|---|---|---|---|---|
| 1 SD | 2.43 | 8.16 | 17.01 | 1.78 |
| 2 SD | 3.02 | 8.58 | 18.52 | 1.80 |
| 3 SD | 4.25 | 9.34 | 16.81 | 1.34 |
| 4 SD | 2.27 | 6.78 | 13.99 | 1.73 |
| 5 SD | 3.15 | 8.59 | 17.90 | 1.72 |
| 6 SD | 2.93 | 7.96 | 17.11 | 1.78 |
| 7 SD | 3.49 | 8.71 | 15.81 | 1.41 |
| 8 SD | 2.01 | 5.33 | 11.79 | 1.83 |
| Formulation | MMAD (μm) | GSD | FPF% | RF% | ||||
|---|---|---|---|---|---|---|---|---|
| Mean ± sd | CI 95% | Mean ± sd | CI 95% | Mean ± sd | CI 95% | Mean ± sd | CI 95% | |
| 1 SD | 1.69 ± 0.29 | 0.97–2.41 | 4.46 ± 0.90 | 2.22–6.70 | 77.3 ± 0.5 | 76.1–78.6 | 58.9 ± 2.6 | 52.5–65.4 |
| 2 SD | 5.05 ± 0.39 | 4.10–6.00 | 2.89 ± 0.03 | 2.81–2.96 | 69.0 ± 0.9 | 66.7–71.3 | 39.3 ± 0.1 | 39.0–39.6 |
| 3 SD | 3.06 ± 0.12 | 2.77–3.36 | 4.40 ± 0.37 | 3.48–5.32 | 73.8 ± 1.0 | 71.5–76.4 | 48.4 ± 3.1 | 40.8–56.0 |
| 4 SD | 4.09 ± 0.50 | 2.85–5.33 | 3.61 ± 0.28 | 2.92–4.23 | 71.2 ± 1.4 | 67.7–74.7 | 43.4 ± 1.9 | 38.7–48.1 |
| 5 SD | 2.96 ± 0.54 | 1.62–4.30 | 8.83 ± 0.32 | 8.05–9.63 | 72.7 ± 1.3 | 68.9–76.5 | 47.6 ± 1.6 | 44.8–50.5 |
| 6 SD | 3.28 ± 0.16 | 2.87–3.69 | 3.66 ± 0.77 | 1.75–5.56 | 74.0 ± 1.0 | 71.5–76.5 | 54.8 ± 2.0 | 49.8–59.9 |
| 7 SD | 3.36 ± 0.34 | 2.51–4.21 | 3.81 ± 0.15 | 3.43–4.18 | 73.1 ± 1.1 | 70.5–75.7 | 50.7 ± 1.9 | 45.9–55.6 |
| 8 SD | 4.90 ± 0.75 | 3.05–6.75 | 4.81 ± 1.23 | 1.76–7.87 | 69.4 ± 2.1 | 64.1–74.5 | 39.8 ± 2.3 | 33.9–45.7 |
| MMAD (μm) | FPF% | RF% | ||||
|---|---|---|---|---|---|---|
| Pair | p-Value | Significance | p-Value | Significance | p-Value | Significance |
| 1 SD vs. 5 SD | 0.0369 | * | 0.0067 | ** | 0.0001 | *** |
| 2 SD vs. 6 SD | 0.0024 | ** | 0.0034 | ** | <0.0001 | *** |
| 3 SD vs. 7 SD | 0.9864 | ns | 0.9955 | ns | 0.8646 | ns |
| 4 SD vs. 8 SD | 0.3477 | ns | 0.6276 | ns | 0.4328 | ns |
| Main Peak | Secondary Peak | ||||
|---|---|---|---|---|---|
| Sample | Z-Average (d.nm) | Size (nm) | Intensity (%) | Size (nm) | Intensity (%) |
| Neat serum | 221.67 ± 13.03 | 381.17 ± 29.94 | 79.13 ± 5.20 | 82.79 ± 18.57 | 18.43 ± 5.50 |
| F1 SD | 108.27 ± 6.29 | 190.10 ± 9.41 | 78.70 ± 11.82 | 31.60 ± 18.65 | 17.97 ± 13.60 |
| F2 SD | 85.45 ± 1.51 | 189.77 ± 62.04 | 86.03 ± 6.56 | 22.90 ± 9.54 | 13.00 ± 6.68 |
| F3 SD | 115.03 ± 2.45 | 105.25 ± 37.33 | 55.70 ± 9.86 | 22.35 ± 8.46 | 11.83 ± 6.39 |
| F4 SD | 144.13 ± 3.47 | 204.73 ± 8.21 | 89.73 ± 2.26 | 30.58 ± 8.08 | 5.67 ± 0.64 |
| Purified serum | 242.97 ± 4.94 | 388.07 ± 24.45 | 85.97 ± 2.84 | 61.54 ± 9.06 | 13.23 ± 1.62 |
| F5 SD | 126.87 ± 4.96 | 281.00 ± 65.11 | 82.80 ± 20.33 | 52.22 ± 48.27 | 20.70 ± 20.65 |
| F6 SD | 112.87 ± 0.91 | 194.87 ± 15.21 | 89.43 ± 7.92 | 22.76 ± 16.67 | 8.30 ± 7.80 |
| F7 SD | 103.83 ± 0.60 | 199.87 ± 46.30 | 82.97 ± 20.35 | 38.32 ± 38.17 | 20.75 ± 24.11 |
| F8 SD | 154.97 ± 3.03 | 234.07 ± 17.18 | 94.20 ± 3.86 | 30.32 ± 13.85 | 7.25 ± 2.76 |
| Formulation Nr. | AUC | Residual Activity % | Pulmonary Activity % |
|---|---|---|---|
| 1 SD | 8009 ± 329 | 87.9 ± 3.6 | 68.0 ± 2.6 |
| 2 SD | 8438 ± 173 | 92.6 ± 1.9 | 63.9 ± 1.4 |
| 3 SD | 8364 ± 220 | 91.8 ± 2.4 | 67.8 ± 1.8 |
| 4 SD | 8250 ± 412 | 90.6 ± 4.5 | 64.5 ± 3.1 |
| 5 SD | 5879 ± 283 | 82.0 ± 4.0 | 59.6 ± 2.8 |
| 6 SD | 5927 ± 484 | 82.6 ± 6.7 | 61.1 ± 4.6 |
| 7 SD | 5444 ± 219 | 75.9 ± 3.1 | 55.5 ± 2.1 |
| 8 SD | 5882 ± 473 | 82.0 ± 6.6 | 56.9 ± 4.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Germani, S.; Polichetti, M.; Garrapa, V.; Trevisi, G.; Füner, J.; Bettini, R. Spray-Dried Serum for Inhaled Antiviral Therapy. Pharmaceutics 2025, 17, 1518. https://doi.org/10.3390/pharmaceutics17121518
Germani S, Polichetti M, Garrapa V, Trevisi G, Füner J, Bettini R. Spray-Dried Serum for Inhaled Antiviral Therapy. Pharmaceutics. 2025; 17(12):1518. https://doi.org/10.3390/pharmaceutics17121518
Chicago/Turabian StyleGermani, Saveria, Miriam Polichetti, Valentina Garrapa, Giovanna Trevisi, Jonas Füner, and Ruggero Bettini. 2025. "Spray-Dried Serum for Inhaled Antiviral Therapy" Pharmaceutics 17, no. 12: 1518. https://doi.org/10.3390/pharmaceutics17121518
APA StyleGermani, S., Polichetti, M., Garrapa, V., Trevisi, G., Füner, J., & Bettini, R. (2025). Spray-Dried Serum for Inhaled Antiviral Therapy. Pharmaceutics, 17(12), 1518. https://doi.org/10.3390/pharmaceutics17121518








