1. Introduction
Breast cancer remains the most frequently diagnosed malignancy among women in the United States, accounting for approximately 30% of all new female cancer cases annually [
1]. Nearly 10–20% of patients lack estrogen, progesterone, or HER2 receptors and are classified as TNBC [
2]. TNBC has been identified as a more aggressive subtype with earlier metastasis and overall poorer prognosis compared to other breast cancer subtypes [
3]. Standard treatments for TNBC are limited to conventional chemotherapy and surgery. However, chemotherapy is often short-lived in its effectiveness due to rapid development of drug resistance [
4]. This therapeutic gap has driven the search for repurposing clinically approved, off-patent drugs with latent anticancer activity.
DSF, originally approved by the FDA as an alcohol-aversion medication, has shown promise in cancer treatment [
5]. Upon administration, DSF is rapidly metabolized into diethyldithiocarbamate (DDC), which chelates Cu
2+ to form a complex [Cu(DDC)
2]. This complex exhibits cytotoxicity by elevating reactive oxygen species (ROS) and inhibiting proteasome function, offering a potential mechanism to overcome drug resistance in cancer cells [
2,
3]. However, clinical application of DSF has been limited by poor drug stability, rapid systemic metabolism, and limited plasma half-life [
6,
7], while direct use of [Cu(DDC)
2] is impractical due to extremely low solubility (<0.5 ng/mL) [
8]. These challenges underscore the need for a robust, stable, and bioavailable delivery system for [Cu(DDC)
2].
Recent studies have further shown that DSF/Cu co-treatment may induce ICD in breast cancer cells [
9], suggesting a promising new avenue for the treatment of TNBC through immunotherapy. ICD is a regulated type of cell death that activates an adaptive immune response in immunocompetent hosts [
10]. Cytotoxic chemotherapies such as doxorubicin and oxaliplatin trigger ICD by promoting endoplasmic reticulum (ER) stress and releasing damage-associated molecular patterns (DAMPs) [
11]. These DAMPs include CRT, ATP, and high-mobility group box-1 (HMGB1), which act, respectively, as “eat me”, “find me”, and immunostimulatory signals, facilitating dendritic cell maturation and antigen presentation [
12,
13,
14,
15]. While DSF/Cu has been shown to promote ICD, it remained unclear whether the pre-formed [Cu(DDC)
2] complex, particularly when delivered via NP, can elicit a comparable immunogenic response.
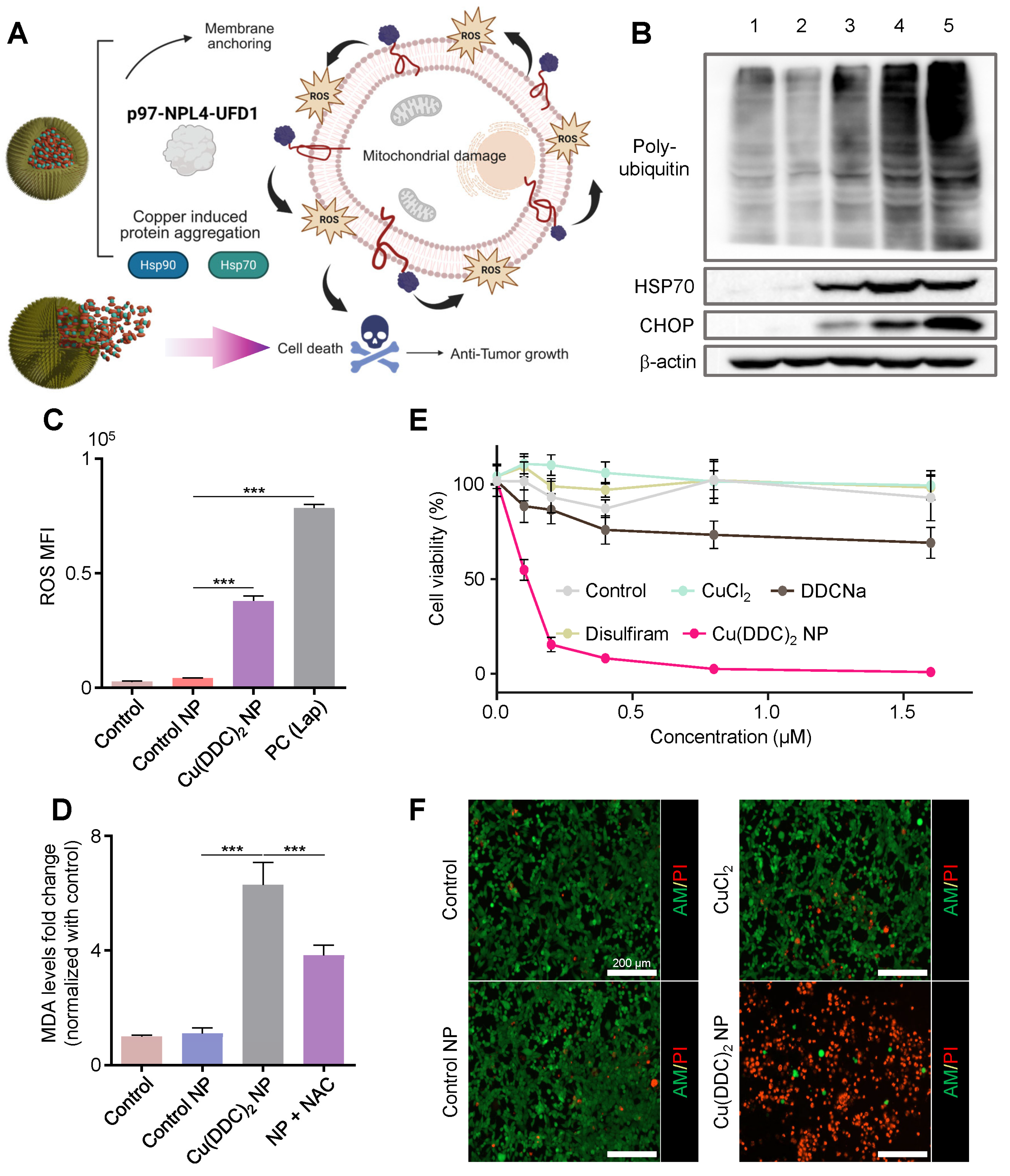
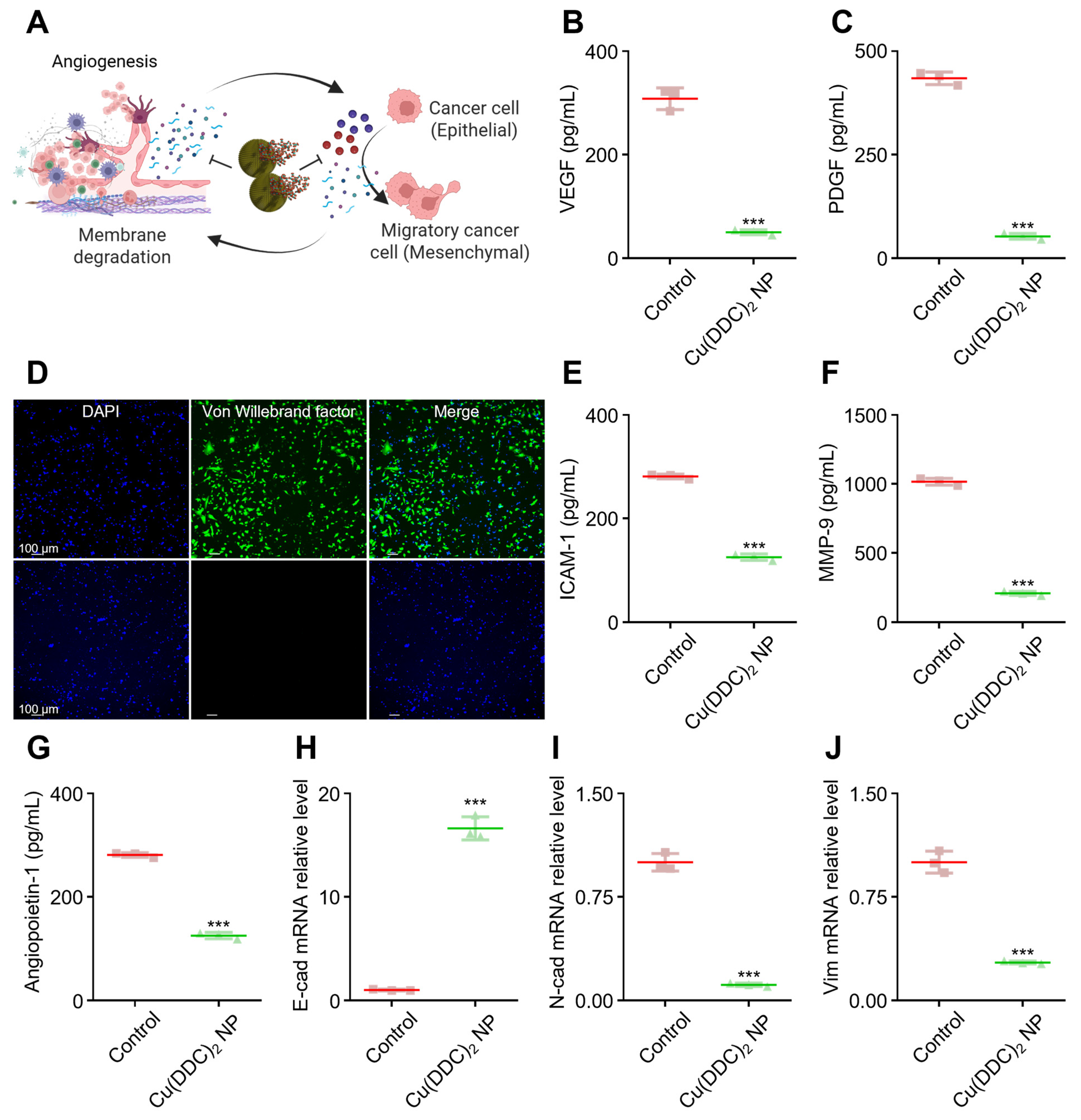
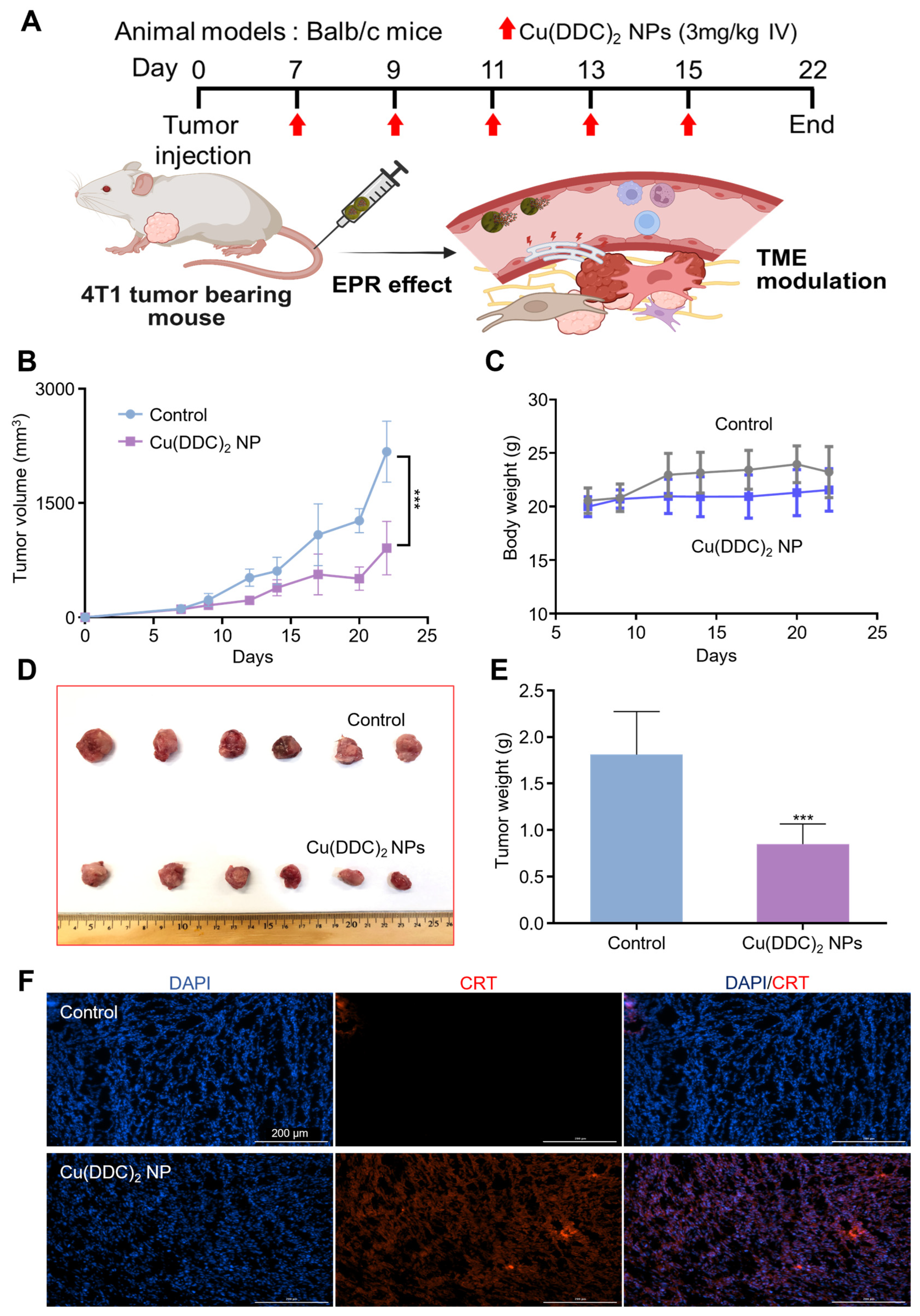
Herein, we developed amphiphilic dendrimer-capped [Cu(DDC)2] NP to overcome the delivery obstacles and enhance the therapy’s efficacy against TNBC. Encapsulation of [Cu(DDC)2] within a dendritic amphiphilic carrier improves its solubility and serum stability, circumvents the rapid metabolism of DSF, and eliminates the need for in vivo copper supplementation, collectively enabling sustained systemic levels of the active complex. To optimize the NP formulation, we synthesized a library of amphiphilic PEGylated lysine-based dendrimers and identified PEG5k-Lys4-Cholic Acid8 (PLCA8) as the optimal stabilizer based on its high drug loading capacity and colloidal stability. Using this optimized PLCA8/[Cu(DDC)2] formulation, we demonstrated potent in vitro cytotoxicity against TNBC cells at sub-micromolar IC50 concentrations. Importantly, the NP induced hallmark features of ICD, including surface CRT exposure and extracellular ATP release. Beyond their cytotoxic activity, PLCA8/[Cu(DDC)2] NP also modulated the tumor microenvironment by downregulating MMP-3 and MMP-9, and key angiogenic and mesenchymal markers such as VEGF, N-cadherin, and vimentin, thereby suppressing angiogenesis and metastatic potential. In vivo studies further demonstrated that PLCA8/[Cu(DDC)2] NP effectively suppressed tumor progression in a TNBC mouse model following a single systemic administration, without requiring adjunctive chemotherapy or radiotherapy. These findings demonstrate the potential of this strategy to enhance and broaden anticancer efficacy by integrating targeted cytotoxicity with immune activation, offering a promising avenue for the development of next-generation immunomodulatory nanotherapeutics against TNBC.
2. Materials and Methods
2.1. Materials
Methoxy PEG Amine HCl salt (PEG5K-NH2, Cat. # M-NH2HCl-5000) was purchased from JenKem Technology (Plano, TX, USA). Nα,ε-Bis-Fmoc-L-lysine, Nα,im-Bis-Fmoc-L-histidine, and N,N’-Diisopropylethylamine (DIEA) were obtained from Chem-Impex International, Inc. (Wood Dale, IL, USA). Fmoc-D-His(Boc)-OH was purchased from BACHEM, and cholic acid was obtained from Beantown Chemical. 1-Hydroxybenzotriazole hydrate (HOBt) was purchased from Sigma-Aldrich (St. Louis, MO, USA), and N,N’-Diisopropylcarbodiimide (DIC) was purchased from Alfa Aesar (MA). All other general chemicals and reagents were obtained from VWR. ELISA kits for IL-12 and IL-1β were purchased from R&D Systems (Minneapolis, MN, USA), and the HMGB1 ELISA kit was obtained from Arigo Biolaboratories (Zhubei City, Taiwan). The following cell lines were used in this study: 4T1 mouse mammary carcinoma cell line (ATCC), U937-DC-SIGN (CRL-2539, ATCC), primary CD8+ cytotoxic T cells (PCS-800-017™, ATCC), THP-1 Dual™ NF-κB/IRF reporter cells (CRL-3253™, ATCC), and DC2.4 mouse dendritic cell line (immortalized; Cat. # SCC142, Sigma-Aldrich (St. Louis, MO, USA)).
2.2. PEG-Lysine Dendrimer
The PEG
5K-Lysine dendrimer was synthesized via stepwise peptide coupling process starting from MeO-PEG-NH
2·HCl [
16]. PEG
5K-NH
2 (1 g, 0.2 mmol), Fmoc-Lys(Fmoc)-OH (236.4 mg, 0.4 mmol), DIC (75 μL, 0.48 mmol), HOBt (64.8 mg, 0.48 mmol), and DIEA (175 μL, 1 mmol) were dissolved in DMF (25 mL) and stirred at room temperature for 3 h. Completion of the coupling reaction was confirmed by the Kaiser test: yellow indicated the completed reaction with no free amino groups, while a blue color indicated the presence of unreacted amino groups. The reaction mixture was poured into cold diethyl ether (100 mL), and the precipitate was collected by centrifugation, washed with cold ether (3 × 75 mL), and dried under vacuum. Fmoc groups were removed by treatment with 20% piperidine in DMF (
v/
v 1:4, 50 mL), and the deprotected products were precipitated and washed with cold ether. This coupling and deprotection process was repeated twice with Fmoc-Lys(Fmoc)-OH to generate the final PEG-lysine-dendrimer structure. After the final deprotection, NHS-Cholic acid was conjugated to the terminal amino groups of the lysine residues to yield PLCA8. The product was further purified by dialysis with deionized water for 2 days and lyophilized to obtain the white powder. The chemical structure and degree of substitution of PLCA8 were confirmed by
1H NMR (DMSO-d
6) (
Figure S1).
2.3. Preparation of NP
The [Cu(DDC)
2] NP was prepared with SMILE technology as described in the previous report [
17]. In brief, the stabilizer was dissolved in dichloromethane. The dichloromethane was removed by a rotavapor, and the resulting film was dispersed in deionized water. Then, DDC-Na and CuCl
2 were dissolved in the aqueous solution containing 1% (
w/
v) stabilizer to form a DDC-Na solution and a CuCl
2 solution. [Cu(DDC)
2] NP was formed by mixing DDC-Na solution and CuCl
2 solution and vortexing for 1 min. To remove large aggregation, the forming [Cu(DDC)
2] NP was centrifuged at 10,000 rpm (6700×
g) for 10 min and filtered through a 0.45 µm membrane.
2.4. Characterization of NP
DLS (Zetasizer Nano ZS, Malvern, UK) was used to determine the particle size of [Cu(DDC)2] NP. The morphology and elemental compositions of NP were characterized by FESEM using JBM-7000F (JEOL, Tokyo, Japan), equipped with an EDX detector. The concentration of [Cu(DDC)2] NP was estimated by a UV spectrometer (Nanodrop 2000, Thermo Scientific, Waltham, MA, USA) at 435 nm. The [Cu(DDC)2] concentration was calculated by a standard curve generated with various [Cu(DDC)2] concentrations. To determine the stability of [Cu(DDC)2] NP. The NP was incubated with 10% fetal bovine serum (FBS) at 37 °C, and the particle size and concentration were examined at different time points. The loading efficiency of [Cu(DDC)2] NP was calculated by the following equation: Loading efficiency (%) = (real drug concentration/theoretical drug concentration) × 100%.
The encapsulated [Cu(DDC)
2] concentration was quantified by UV–Vis spectroscopy at 435 nm after complete nanoparticle disruption in DMSO. As shown in
Figure S2A, the PLCA8 polymer matrix displayed negligible absorbance at this wavelength, indicating minimal background interference. The calibration curve for {Cu(DDC)
2] in DMSO followed the linear regression equation y = 0.02989x + 0.003463 with R
2 = 0.9994 (
Figure S2B). Free drug was removed by centrifugation prior to measurement, and the remaining pellet was redispersed in DMSO for analysis. Results are reported as mean ± SD (
n = 3 technical replicates).
2.5. Cell Viability Assay
4T1 murine breast cancer cells were cultured in a medium composed of RPMI-1640 (Corning) with 10% FBS and 1% antibiotic-antimycotic. Cells were cultured at 37 °C in a humidified atmosphere containing 5% CO2. Cells were seeded into a 96-well plate at a density of 5000 cells/well and incubated overnight. Followed by treating the cells with a series of different concentrations of [Cu(DDC)2] NP diluted in a cell culture medium for 48 h, cytotoxicity was determined with the MTT assay. The absorbance was determined with a microplate spectrophotometer. The IC50 was calculated with GraphPad software based on a dose–response curve. Due to the poor aqueous solubility of [Cu(DDC)2], the free compound was first dissolved in DMSO to prepare a stock solution and diluted in cell culture medium immediately before use (final DMSO ≤ 0.1%). The nanoparticle suspensions were diluted in the same medium to match the molar [Cu(DDC)2] concentrations used for free-drug treatments, ensuring equivalent [Cu(DDC)2] exposure across groups.
2.6. Calcein-AM and PI Staining
Cells were seeded at a density of 5000 cells per well in a 96-well plate overnight. This was followed by treating cells with different compounds for 24 h and then staining them with a solution composed of Calcein-AM and PI in pH 7.4 PBS. Cell samples were analyzed with a Cytation 5 Cell Imaging Multi-Mode Reader. Viable and dead cells can be identified by the green fluorescence (live) and the red fluorescence (dead), respectively.
2.7. HMGB1 Detection
4T1 cells were seeded at a density of 1 × 105 cells per well in a 12-well plate. After incubation overnight, the cells were treated with different test agents for 18 h. Then, the cells were washed with cold PBS twice, fixed with 4% paraformaldehyde for 20 min, and permeabilized with 0.1% Triton X-100 for 10 min. Next, cells were incubated with primary HMGB1 antibody (3935S, Cell signaling) for 1 h and followed by incubating with FITC-conjugated secondary antibody for 1 h. Finally, the cells were stained with DAPI and examined by microscope (NIKON, Tokyo, Japan). The releasing level of HMGB1 were quantified from culture supernatants collected from wells seeded at equal initial cell densities and treated under identical conditions. Samples were not normalized to cell number because equal plating and comparable viability across groups ensured equivalent total cell input. The concentrations of HMGB1 in supernatants were measured using HMGB1 ELISA Kit according to the manufacturer’s instructions.
2.8. Calreticulin (CRT) Detection
4T1 breast cancer cells were seeded at a density of 1 × 105 cells per well in a 12-well plate. After being incubated overnight, the cells were treated with different agents for 12 h. Then, cells were harvested by 0.25% trypsin, washed with PBS (0.5% BSA) three times. Cells were incubated with anti-CRT (ab2907, Abcam, Cambridge, UK) primary antibodies for 1 h at RT and the FITC labeled secondary antibodies with for 1 h at RT. The FITC (green) fluorescence intensity in each sample was detected and quantified by flow cytometry (BD Accuri C6, San Jose, CA, USA).
2.9. ROS Evaluation
Intracellular ROS levels were measured using the DCFH-DA fluorescence assay. Briefly, cells were seeded in a 24-well plate at a density of 50,000 cells per well. After treatment with the indicated formulations, cells were incubated with 5 µM DCFH-DA in serum-free medium at 37 °C for 30–45 min. Following incubation, cells were washed with PBS to remove excess dye. The fluorescence intensity was measured using a Cytation 5 Cell Imaging Multi-Mode Reader (Agilent Technologies, Santa Clara, CA, USA) with excitation at 485 nm and emission at 535 nm.
2.10. ATP Detection
The level of extracellular ATP was determined with an ATP determination assay (A22066, Thermo Scientific, Waltham, MA, USA) according to the manufacturer’s instructions. In brief, 4T1 breast cancer cells were seeded at a density of 1 × 104 cells per well in a 96-well plate. After being incubated overnight, the cells were treated with different agents for 12 h. Then, the conditioned medium was collected and examined with the ATP determination kit. The luminescence was measured using GloMax 96 Microplate Luminometer (Promega Corporation, Madison, WI, USA).
2.11. Anti-Angiogenesis Evaluation
To evaluate the effect of NP on angiogenesis, the mouse endothelial cell line BEND3 was selected as the detection model. The control group consisted of a co-culture of 5000 cancer cells, 5000 BEND3 cells, and 5000 macrophages. For the [Cu(DDC)2] treatment group, cells were incubated with [Cu(DDC)2] for 6 h. After treatment, the NP was removed, and the cells were further incubated for an additional 18 h. Following incubation, culture supernatants were collected and analyzed using ELISA to quantify levels of mouse VEGF-A, MMP-3, MMP-9, sICAM-1, and ANGPT1. Commercial ELISA kits (Abcam, Cambridge, UK) were used according to the manufacturers’ protocols. Specifically, mouse VEGF-A was measured using the Mouse VEGF-A ELISA Kit (Abcam, Cambridge, UK, Cat# ab100751), MMP-3 using the Mouse MMP-3 ELISA Kit (Abcam, Cambridge, UK, Cat# ab100731), MMP-9 using the Mouse MMP-9 ELISA Kit (Abcam, Cambridge, UK, Cat# ab100610), and sICAM-1 using the Mouse ICAM-1 ELISA Kit (Abcam, Cambridge, UK, Cat# ab100688). Mouse ANGPT1 levels were quantified using the Mouse ANGPT1/Angiopoietin-1 Sandwich ELISA Kit (LSBio, Seattle, WA, USA, Cat# LS-F31477). For each assay, a standard curve was generated by serial dilution of the corresponding recombinant mouse protein. Sample concentrations were calculated by interpolating the absorbance values measured at 450 nm against the respective standard curves.
Immunofluorescence staining for MMP-3 was performed using a mouse monoclonal anti-MMP-3 antibody (purchased from Abcam, Cambridge, UK, Cat# ab53015), followed by incubation with an appropriate fluorophore-conjugated anti-mouse secondary antibody. Cells or tissue sections were fixed, permeabilized, and blocked prior to antibody incubation, following standard immunofluorescence protocols.
2.12. Western Blot
Mouse 4T1 cancer cells were seeded in a 6-well plate at a cell density of 4 × 105 cells/well. After incubating the cells overnight, the cells were treated with different agents. After 6 h of incubation, cell lysates were prepared using lysis buffer. The cell lysates were separated using sodium dodecyl sulfate-polyacrylamide gel electrophoresis and transferred to membranes for Western blot analysis. Membranes were probed with one of the following primary antibodies: anti-HSP70 (Enzo, Farmingdale, NY, USA, 1:4000), anti-ubiquitin (Cell Signaling, Danvers, MA, USA, 1:1000), anti-CHOP (Proteintech, Rosemont, IL, USA, 1:1000), anti-b-actin (Cell Signaling, Danvers, MA, USA, 1:2000) followed by detection by horseradish peroxidase-conjugated secondary antibodies: goat anti-rabbit IgG-HRP (Cell Signaling, Danvers, MA, USA), anti-mouse IgG-HRP (Santa Cruz, Dallas, TX, USA). After removing secondary antibodies, the membranes were washed with TBS-T (TBS with 0.1% Tween 20). Then, membranes were visualized by an ECL (32209, Thermo Scientific, Waltham, MA, USA) detection reagent and imaged using a Western Blot imaging system (c600, Azure, Dublin, CA, USA).
2.13. In Vivo Tumor Growth Inhibition Study
Balb/c mice (female, 7 weeks) were purchased from the Jackson Laboratory (Bar Harbor, ME, USA). The orthotopic breast tumor animal models were established by injecting 4T1 cells (2 × 10
6 cells) into the first mammary fat pad of the Balb/c mice. Treatments were initiated when the tumors reached an average volume of 100 mm
3. Tumor size (mm
3) = [width (mm)
2× length (mm)] × 1/2. Mice were randomly divided into two groups (6 mice per group) and were given an intravenous injection of [Cu(DDC)
2] NP and 10% (
w/
v) PLCA8 polymer in PBS (control). [Cu(DDC)
2] NP was administered intravenously at 3 mg/kg, calculated based on the total Cu(DDC)
2 complex, on days 7, 9, 11, 13, and 15 post-tumor inoculation. The group size and dosage were selected to ensure adequate statistical power and to account for potential animal loss during the study, consistent with prior Cu-based nanoparticle studies employing comparable sample sizes [
18]. Body weight and tumor volume were measured and recorded. The mice were euthanized, and the weight of the collected tumors was determined at the end of the experiment. All animal procedures were approved and conducted in accordance with the guidelines of Auburn University’s Institutional Animal Care and Use Committee (protocol #2022-3824).
2.14. Immune Cells Co-Culture Experiment
The 4T1 breast cancer cells were seeded in 12-well plates at a cell density of 5 × 104 cells/well and incubated overnight. Cells were treated with different agents for 12 h, and BMDCs were added after the removing of treatment agents in each well. After co-culture for 48 h, the maturation of DCs was examined by determining the concentration of IL-12 and IL-1b in the conditioned cell culture medium with ELISA. Additionally, the levels of CD80, CD86, and CD11c were determined with standard IF protocol. The activated T cells were evaluated with the secretion of Granzyme B, Perforin, and IFN-γ. Those molecules were determined by ELISA kits.
2.15. Caspase-3 Activity
Caspase-3 was quantified using a colorimetric DEVD-pNA assay (Abs 405 nm). Cells were seeded at 3 × 104 per well in 96-well plates and treated with [Cu(DDC)2] NP; staurosporine (1 µM, 4 h) served as the positive control. After treatment, cells were lysed on ice with lysis buffer for 15 min and clarified by brief centrifugation. Equal volumes of lysate and DEVD substrate were mixed and incubated for 60 min at 37 °C, and signals were read as absorbance at 405 nm for DEVD-pNA.
2.16. Statistical Analysis
Data were analyzed by GraphPad Prism 10.4.1 using the unpaired t-test or ANOVA analysis.
4. Discussion
The rational engineering of metal–organic nanotherapeutics offers an opportunity to overcome long-standing challenges in drug delivery and cancer treatment. Selecting an appropriate stabilizer is essential for achieving high encapsulation efficiency and NP stability [
20]. By applying the SMILE approach, we successfully formulated [Cu(DDC)
2] NP using an amphiphilic PLCA8 with cholic acid moieties. PLCA8 provided critical nanoscale stabilization through enhanced hydrophobic interactions, achieving near-complete encapsulation efficiency (~100%) and excellent serum stability. In contrast, dendrimers with fewer cholic acids or different hydrophobic groups, such as PLCA2 or PEG-lysine-histidine variants, failed to maintain NP integrity under physiological conditions. These findings demonstrate that dendrimer architecture, particularly the degree and nature of hydrophobic conjugation, plays a decisive role in coordinating stable metal–drug complexation at high loading, a recurring challenge in nanomedicine. To support clinical translation, the manufacturability and pharmacokinetic behavior of the NP formulation were critically evaluated. Batch-to-batch reproducibility was confirmed across three independent syntheses of the polymers including PLCA8, showing consistent physicochemical characteristics with minimal variation in yield (±5%). The [Cu(DDC)
2] NP maintained a consistent particle size and exhibited stable surface charge with low variability.
In vitro studies confirmed that [Cu(DDC)
2] NP exhibited high potency against TNBC cells, with a notably low IC
50 value. Treatment with [Cu(DDC)
2] NP induced marked oxidative stress and ER stress in these cells. Mechanistically, [Cu(DDC)
2] is known to inhibit the NPL4-p97 segregase complex, a key regulator of ERAD [
21]. This inhibition impairs proteostasis by preventing the clearance of misfolded and polyubiquitinated proteins, leading to sustained ER stress and proteotoxic accumulation [
22,
23]. When coupled with excessive ROS generation, these stressors can push tumor cells into a non-apoptotic form of cell death known as paraptosis, a mechanism previously observed in other cancer models treated with [Cu(DDC)
2]. Our in vitro studies in TNBC cells revealed hallmark features of this disruption, including the buildup of polyubiquitinated proteins and upregulation of HSP70 and CHOP, markers associated with the unfolded protein response. Concurrently, the NP triggered pronounced oxidative stress, as evidenced by increased ROS and lipid peroxidation (MDA production). These stress signals are consistent with a paraptosis-like form of cell death, characterized by ER dilation and vacuolization rather than caspase-dependent apoptosis [
24]. This is particularly advantageous for TNBC, where apoptosis resistance limits the efficacy of many standard chemotherapies.
Beyond direct cytotoxicity, [Cu(DDC)
2] NP effectively induced ICD, a feature rarely achieved by small-molecule therapies alone. We observed three canonical hallmarks of ICD: translocation of CRT to the tumor cell surface, ATP release, and HMGB1 secretion [
25]. These DAMPs are critical for activating DCs and priming anti-tumor immunity. Indeed, bone marrow-derived DCs co-cultured with [Cu(DDC)
2]-treated tumor cells showed robust upregulation of CD80 and CD86, confirming functional maturation [
8]. This translated downstream into adaptive immune activation, evidenced by increased IL-12 secretion, elevated IFN-γ production by T cells, and significant upregulation of Granzyme B and Perforin, two cytolytic effectors essential for CTL-mediated killing [
26]. The abrogation of IFN-γ by ROS scavenger NAC highlights the mechanistic link between oxidative stress and immune activation. These findings suggest that [Cu(DDC)
2] NPs serve not only as chemotoxic agents but also as immune adjuvants capable of overcoming tumor immune evasion.
Importantly, the therapeutic efficacy extended beyond immune modulation. [Cu(DDC)
2] NP inhibited EMT and angiogenesis, two characteristic features of metastatic progression. Treated tumors displayed increased E-cadherin expression with concomitant suppression of N-cadherin and vimentin, indicating MET reprogramming [
24]. Additionally, key pro-angiogenic and pro-metastatic mediators, including VEGF, PDGF, angiopoietin-1, MMP-3, and MMP-9, were downregulated following treatment [
25,
26]. These effects suggest that [Cu(DDC)
2] NP disrupted the tumor–stroma crosstalk and prevented vascular remodeling and ECM degradation necessary for metastatic dissemination. Such microenvironmental modulation likely synergizes with ICD-induced immune activation to produce a durable anti-tumor response. Consistent with our previous investigations, the dose range used in this study aligns well with the established safety limits for copper-containing therapeutics, supporting its translational feasibility.
Taken together, the [Cu(DDC)
2] NP platform developed here exemplifies a rationally designed, multifunctional therapeutic that couples drug repurposing with advanced materials engineering. The convergence of proteotoxic stress, ICD induction, EMT suppression, and immune reprogramming within a single formulation highlights the therapeutic versatility of this system for treating aggressive, immune-cold tumors such as TNBC (
Figure 6).