Engineering Neurotoxin-Functionalized Exosomes for Targeted Delivery to the Peripheral Nervous System
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Cell Culture
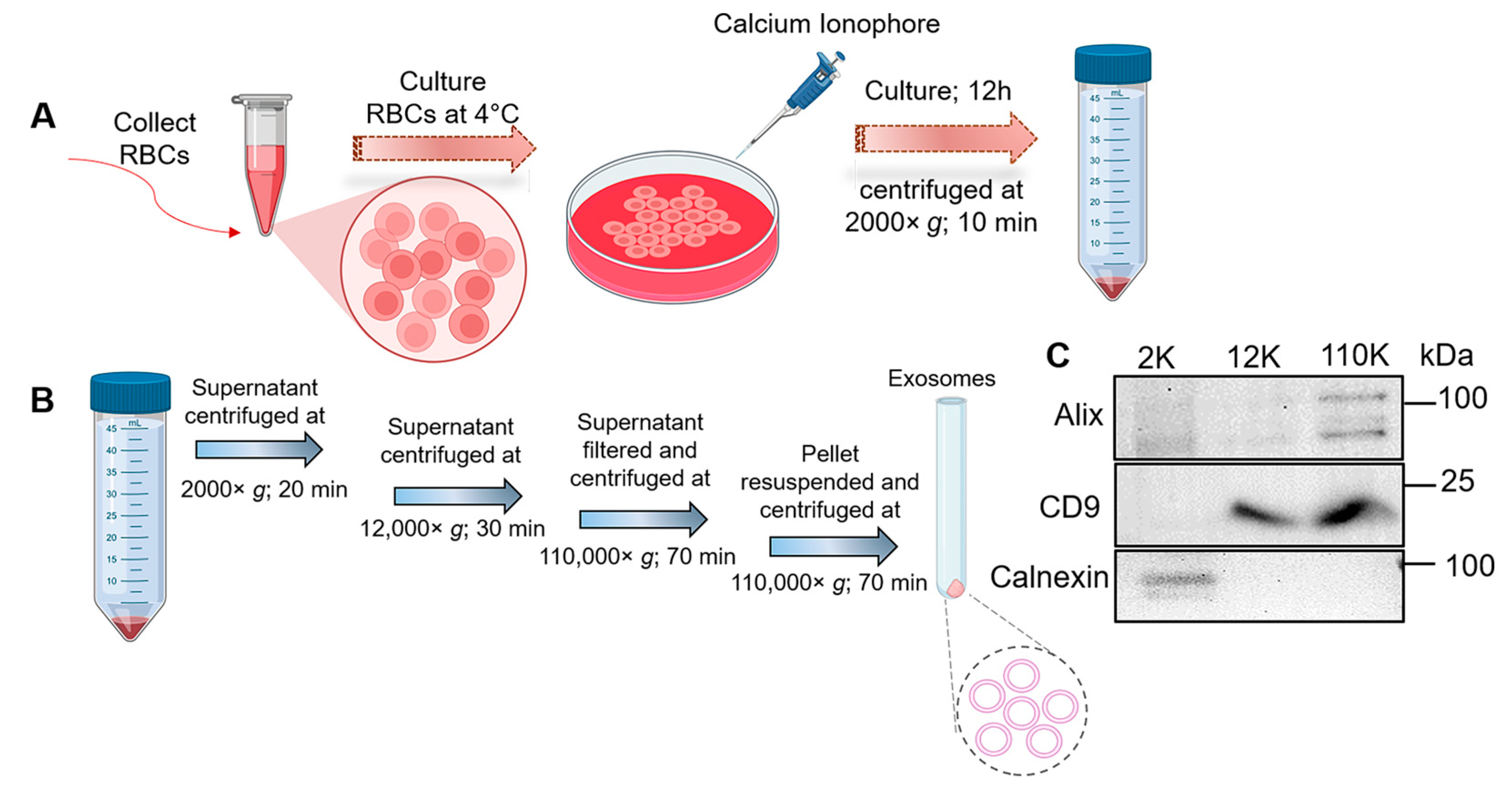
2.3. Exo Isolation and Purification
2.4. Characterization of Exos
Western Blot
2.5. Conjugation of TTC-Fragment and Exo Surface Labeling
2.6. Staining of Exos with Lipophilic Dye
2.7. Uptake of TTC-Targeted and Unmodified Exos in Cells
2.8. Semi-Quantitative Imaging Analysis of CLSM Images
2.9. Animal Experiment Design and Treatment
2.10. Imaging and Bio-Distribution of Exos In Vivo
2.11. Immunofluorescent (IF) Staining and CLSM Imaging of Tissues
2.12. Statistical Analysis
3. Results
3.1. Isolation and Characterization of RBC-Derived Exos
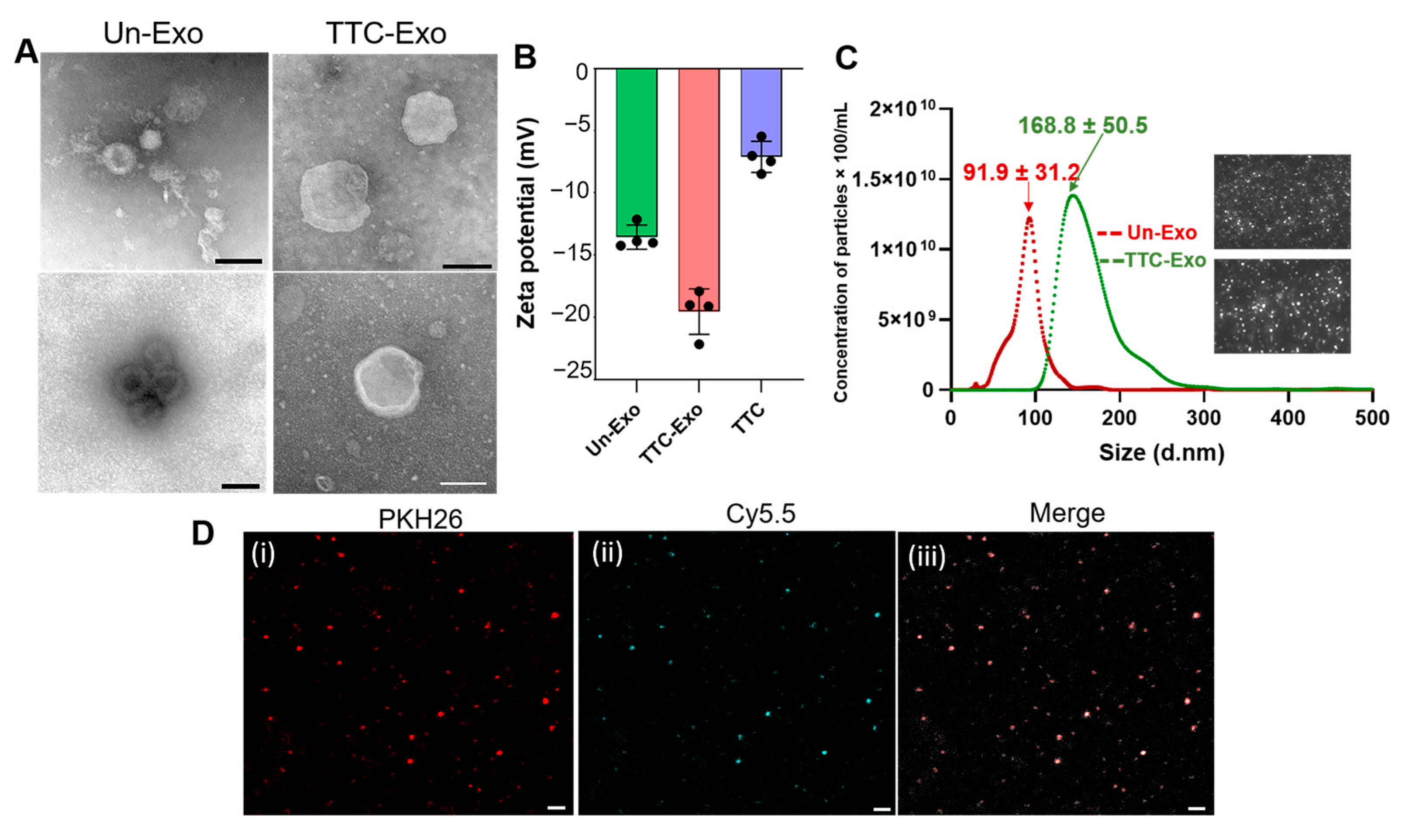
3.2. Design and Synthesis of TTC-Exo Targeted Delivery System for PNS
3.3. Characterization of TTC-Exo and Un-Exo
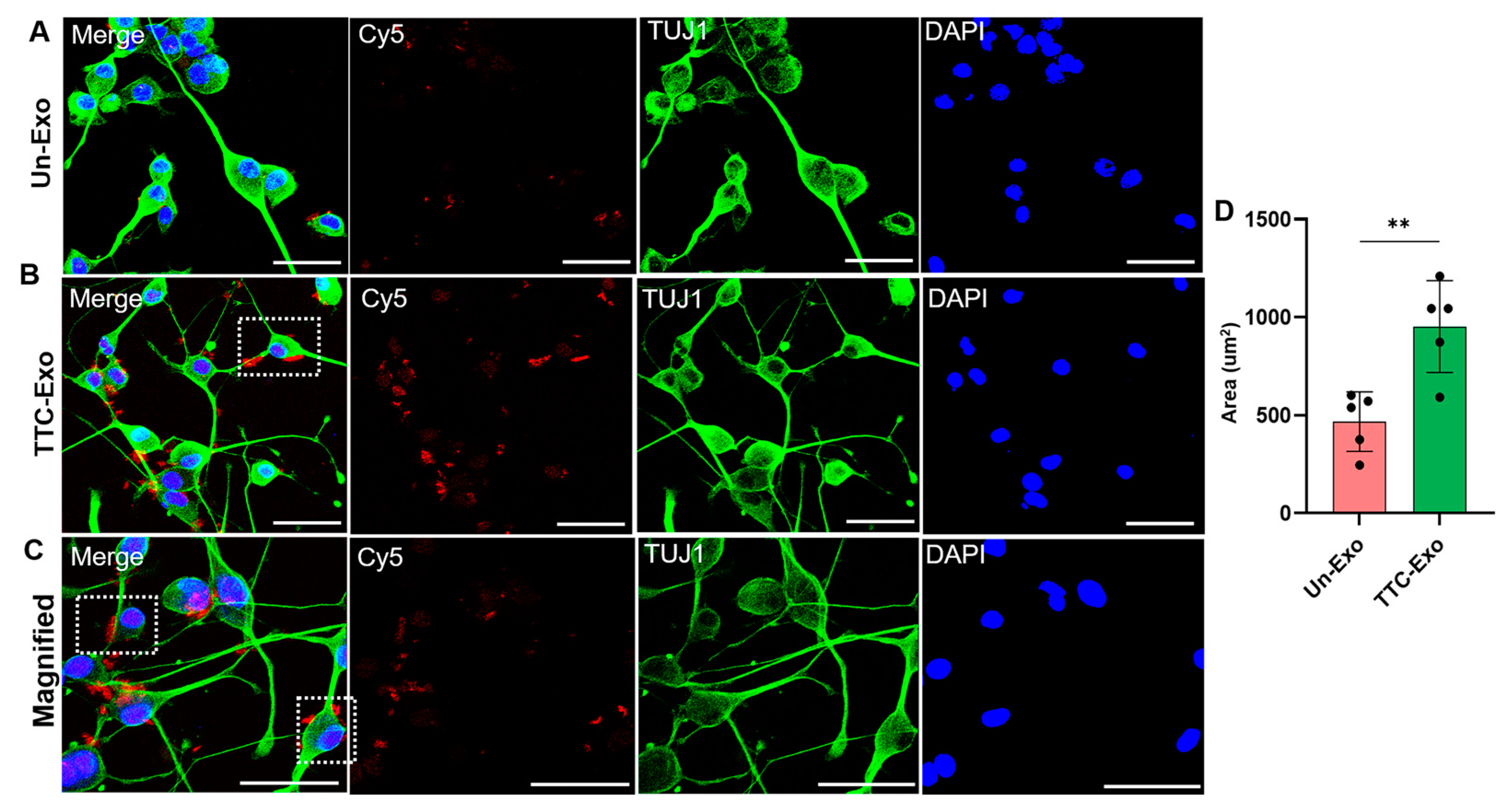
3.4. Uptake of Un-Exo and TTC-Exo in Neuro-2a Cells
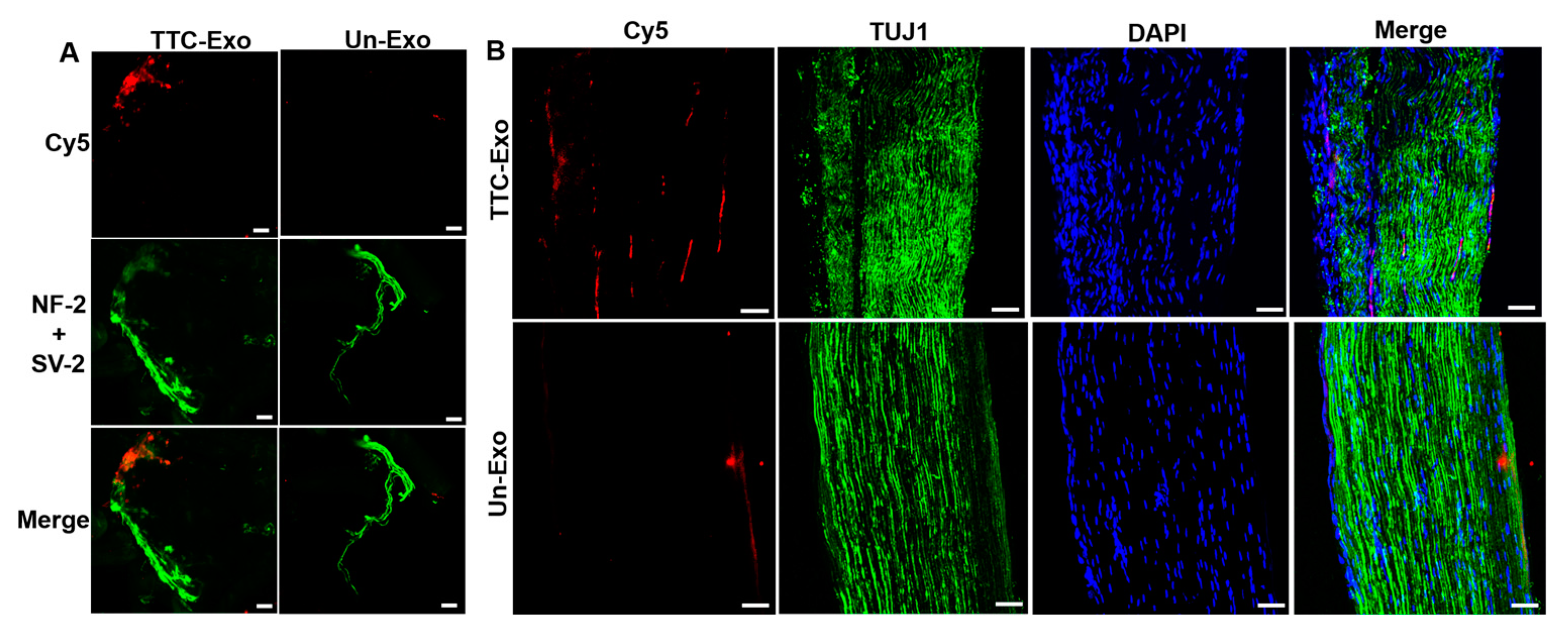
3.5. Modification of Exos with the TTC-Fragment Improves Transport into the PNS in a Mice Model
3.6. IF Images of Muscle and Nerve Tissues Show Localization of TTC-Exo in PNS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hanewinckel, R.; van Oijen, M.; Ikram, M.A.; van Doorn, P.A. The epidemiology and risk factors of chronic polyneuropathy. Eur. J. Epidemiol. 2016, 31, 5–20. [Google Scholar] [CrossRef] [PubMed]
- Bouche, P. Neuropathy of the elderly. Rev. Neurol. 2020, 176, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.L.; Rivlin, M.; Graham, J.G.; Beredjiklian, P.K. Peripheral nerve injury, scarring, and recovery. Connect. Tissue Res. 2019, 60, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Silver, S.; Ledford, C.C.; Vogel, K.J.; Arnold, J.J. Peripheral Nerve Entrapment and Injury in the Upper Extremity. Am. Fam. Physician 2021, 103, 275–285. [Google Scholar] [PubMed]
- Spallone, V.; Lacerenza, M.; Rossi, A.; Sicuteri, R.; Marchettini, P. Painful diabetic polyneuropathy: Approach to diagnosis and management. Clin. J. Pain. 2012, 28, 726–743. [Google Scholar] [CrossRef] [PubMed]
- Windebank, A.J.; Grisold, W. Chemotherapy-induced neuropathy. J. Peripher. Nerv. Syst. 2008, 13, 27–46. [Google Scholar] [CrossRef] [PubMed]
- Bilbao, J.M.; Schmidt, R.E. Infectious Diseases Causing Neuropathy. In Biopsy Diagnosis of Peripheral Neuropathy; Bilbao, J.M., Schmidt, R.E., Eds.; Springer International Publishing: Cham, Switzerland, 2015; pp. 209–224. [Google Scholar]
- Hehir, M.K., 2nd; Logigian, E.L. Infectious neuropathies. Contin. Lifelong Learn. Neurol. 2014, 20, 1274–1292. [Google Scholar] [CrossRef] [PubMed]
- Morrison, B.; Chaudhry, V. Medication, toxic, and vitamin-related neuropathies. Contin. Lifelong Learn. Neurol. 2012, 18, 139–160. [Google Scholar] [CrossRef]
- Hanewinckel, R.; Ikram, M.A.; Van Doorn, P.A. Peripheral neuropathies. Handb. Clin. Neurol. 2016, 138, 263–282. [Google Scholar] [CrossRef]
- Azhary, H.; Farooq, M.U.; Bhanushali, M.; Majid, A.; Kassab, M.Y. Peripheral neuropathy: Differential diagnosis and management. Am. Fam. Physician 2010, 81, 887–892. [Google Scholar]
- Cavalli, E.; Mammana, S.; Nicoletti, F.; Bramanti, P.; Mazzon, E. The neuropathic pain: An overview of the current treatment and future therapeutic approaches. Int. J. Immunopathol. Pharmacol. 2019, 33, 2058738419838383. [Google Scholar] [CrossRef] [PubMed]
- Finnerup, N.B.; Attal, N.; Haroutounian, S.; McNicol, E.; Baron, R.; Dworkin, R.H.; Gilron, I.; Haanpää, M.; Hansson, P.; Jensen, T.S.; et al. Pharmacotherapy for neuropathic pain in adults: A systematic review and meta-analysis. Lancet Neurol. 2015, 14, 162–173. [Google Scholar] [CrossRef]
- McGregor, C.E.; English, A.W. The Role of BDNF in Peripheral Nerve Regeneration: Activity-Dependent Treatments and Val66Met. Front. Cell. Neurosci. 2019, 12, 522. [Google Scholar] [CrossRef]
- Li, R.; Li, D.-h.; Zhang, H.-y.; Wang, J.; Li, X.-k.; Xiao, J. Growth factors-based therapeutic strategies and their underlying signaling mechanisms for peripheral nerve regeneration. Acta Pharmacol. Sin. 2020, 41, 1289–1300. [Google Scholar] [CrossRef] [PubMed]
- Cui, Q. Actions of neurotrophic factors and their signaling pathways in neuronal survival and axonal regeneration. Mol. Neurobiol. 2006, 33, 155–179. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Song, L.; Li, Y.; Guo, J.; Huang, S.; Du, S.; Li, W.; Cao, R.; Cui, S. Neurotrophin-3 promotes peripheral nerve regeneration by maintaining a repair state of Schwann cells after chronic denervation via the TrkC/ERK/c-Jun pathway. J. Transl. Med. 2023, 21, 733. [Google Scholar] [CrossRef] [PubMed]
- Goss, J.R. The therapeutic potential of gene transfer for the treatment of peripheral neuropathies. Expert. Rev. Mol. Med. 2007, 9, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Glorioso, J.C.; Mata, M.; Fink, D.J. Therapeutic gene transfer to the nervous system using viral vectors. J. Neurovirol. 2003, 9, 165–172. [Google Scholar] [CrossRef]
- Lopes, C.D.; Oliveira, H.; Estevão, I.; Pires, L.R.; Pêgo, A.P. In vivo targeted gene delivery to peripheral neurons mediated by neurotropic poly(ethylene imine)-based nanoparticles. Int. J. Nanomed. 2016, 11, 2675–2683. [Google Scholar] [CrossRef]
- Saragovi, H.U.; Gehring, K. Development of pharmacological agents for targeting neurotrophins and their receptors. Trends Pharmacol. Sci. 2000, 21, 93–98. [Google Scholar] [CrossRef]
- Lopes, C.D.F.; Gonçalves, N.P.; Gomes, C.P.; Saraiva, M.J.; Pêgo, A.P. BDNF gene delivery mediated by neuron-targeted nanoparticles is neuroprotective in peripheral nerve injury. Biomaterials 2017, 121, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Kanda, T. Biology of the blood-nerve barrier and its alteration in immune mediated neuropathies. J. Neurol. Neurosurg. Psychiatry 2013, 84, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Rechthand, E.; Smith, Q.R.; Rapoport, S.I. Transfer of nonelectrolytes from blood into peripheral nerve endoneurium. Am. J. Physiol.-Heart Circ. Physiol. 1987, 252, H1175–H1182. [Google Scholar] [CrossRef]
- Liu, H.; Chen, Y.; Huang, L.; Sun, X.; Fu, T.; Wu, S.; Zhu, X.; Zhen, W.; Liu, J.; Lu, G.; et al. Drug Distribution into Peripheral Nerve. J. Pharmacol. Exp. Ther. 2018, 365, 336–345. [Google Scholar] [CrossRef] [PubMed]
- Shankarappa, S.A.; Tsui, J.H.; Kim, K.N.; Reznor, G.; Dohlman, J.C.; Langer, R.; Kohane, D.S. Prolonged nerve blockade delays the onset of neuropathic pain. Proc. Natl. Acad. Sci. USA 2012, 109, 17555–17560. [Google Scholar] [CrossRef] [PubMed]
- Langert, K.A.; Brey, E.M. Strategies for Targeted Delivery to the Peripheral Nerve. Front. Neurosci. 2018, 12, 887. [Google Scholar] [CrossRef] [PubMed]
- Rayner, M.L.D.; Healy, J.; Phillips, J.B. Drug Therapies for Peripheral Nerve Injuries. In Peripheral Nerve Tissue Engineering and Regeneration; Phillips, J.B., Hercher, D., Hausner, T., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 437–463. [Google Scholar]
- Park, I.K.; Lasiene, J.; Chou, S.H.; Horner, P.J.; Pun, S.H. Neuron-specific delivery of nucleic acids mediated by Tet1-modified poly(ethylenimine). J. Gene Med. 2007, 9, 691–702. [Google Scholar] [CrossRef]
- Chu, D.S.; Schellinger, J.G.; Bocek, M.J.; Johnson, R.N.; Pun, S.H. Optimization of Tet1 ligand density in HPMA-co-oligolysine copolymers for targeted neuronal gene delivery. Biomaterials 2013, 34, 9632–9637. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, W.; Johnston, A.H.; Newman, T.A.; Pyykkö, I.; Zou, J. Targeted delivery of Tet1 peptide functionalized polymersomes to the rat cochlear nerve. Int. J. Nanomed. 2012, 7, 1015–1022. [Google Scholar] [CrossRef]
- Lee, S.; Ashizawa, A.T.; Kim, K.S.; Falk, D.J.; Notterpek, L. Liposomes to target peripheral neurons and Schwann cells. PLoS ONE 2013, 8, e78724. [Google Scholar] [CrossRef]
- Chiangjong, W.; Netsirisawan, P.; Hongeng, S.; Chutipongtanate, S. Red Blood Cell Extracellular Vesicle-Based Drug Delivery: Challenges and Opportunities. Front. Med. 2021, 8, 761362. [Google Scholar] [CrossRef] [PubMed]
- Cheng, K.; Kalluri, R. Guidelines for clinical translation and commercialization of extracellular vesicles and exosomes based therapeutics. Extracell. Vesicle 2023, 2, 100029. [Google Scholar] [CrossRef]
- Usman, W.M.; Pham, T.C.; Kwok, Y.Y.; Vu, L.T.; Ma, V.; Peng, B.; Chan, Y.S.; Wei, L.; Chin, S.M.; Azad, A.; et al. Efficient RNA drug delivery using red blood cell extracellular vesicles. Nat. Commun. 2018, 9, 2359. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Kundrat, L.; Pishesha, N.; Bilate, A.; Theile, C.; Maruyama, T.; Dougan, S.K.; Ploegh, H.L.; Lodish, H.F. Engineered red blood cells as carriers for systemic delivery of a wide array of functional probes. Proc. Natl. Acad. Sci. USA 2014, 111, 10131–10136. [Google Scholar] [CrossRef]
- Smyth, T.; Petrova, K.; Payton, N.M.; Persaud, I.; Redzic, J.S.; Graner, M.W.; Smith-Jones, P.; Anchordoquy, T.J. Surface Functionalization of Exosomes Using Click Chemistry. Bioconjugate Chem. 2014, 25, 1777–1784. [Google Scholar] [CrossRef]
- Rumsby, M.G.; Trotter, J.; Allan, D.; Michell, R.H. Recovery of membrane micro-vesicles from human erythrocytes stored for transfusion: A mechanism for the erythrocyte discocyte-to-spherocyte shape transformation. Biochem. Soc. Trans. 1977, 5, 126–128. [Google Scholar] [CrossRef]
- Akbari, A.; Nazari-Khanamiri, F.; Ahmadi, M.; Shoaran, M.; Rezaie, J. Engineered Exosomes for Tumor-Targeted Drug Delivery: A Focus on Genetic and Chemical Functionalization. Pharmaceutics 2022, 15, 66. [Google Scholar] [CrossRef] [PubMed]
- Lencer, W.I.; Tsai, B. The intracellular voyage of cholera toxin: Going retro. Trends Biochem. Sci. 2003, 28, 639–645. [Google Scholar] [CrossRef]
- Surana, S.; Tosolini, A.P.; Meyer, I.F.G.; Fellows, A.D.; Novoselov, S.S.; Schiavo, G. The travel diaries of tetanus and botulinum neurotoxins. Toxicon 2018, 147, 58–67. [Google Scholar] [CrossRef]
- Liu, B.; Kong, Y.; Shi, W.; Kuss, M.; Liao, K.; Hu, G.; Xiao, P.; Sankarasubramanian, J.; Guda, C.; Wang, X.; et al. Exosomes derived from differentiated human ADMSC with the Schwann cell phenotype modulate peripheral nerve-related cellular functions. Bioact. Mater. 2022, 14, 61–75. [Google Scholar] [CrossRef]
- Tian, T.; Hui-Xin, Z.; Chun-Peng, H.; Song, F.; Yan-Liang, Z.; Cui, Q.; Ning-Ping, H.; Zhong-Dang, X.; Zu-Hong, L.; Bakhos, A.T.; et al. Surface functionalized exosomes as targeted drug delivery vehicles for cerebral ischemia therapy. Biomaterials 2018, 150, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.B.; Ly, T.B.; Wesseling, M.C.; Hittinger, M.; Torge, A.; Devitt, A.; Perrie, Y.; Bernhardt, I. Characterization of Microvesicles Released from Human Red Blood Cells. Cell Physiol. Biochem. 2016, 38, 1085–1099. [Google Scholar] [CrossRef] [PubMed]
- Duly, A.M.P.; Kao, F.C.L.; Teo, W.S.; Kavallaris, M. βIII-Tubulin Gene Regulation in Health and Disease. Front. Cell Dev. Biol. 2022, 10, 851542. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.J.; Kennedy, Z.; Wang, Y.; Lu, Y.; Cefaliello, C.; Uyan, Ö.; Song, C.Q.; Godinho, B.M.C.; Xu, Z.; Rusckowski, M.; et al. Imaging Net Retrograde Axonal Transport In Vivo: A Physiological Biomarker. Ann. Neurol. 2022, 91, 716–729. [Google Scholar] [CrossRef] [PubMed]
- Toivonen, J.M.; Oliván, S.; Osta, R. Tetanus toxin C-fragment: The courier and the cure? Toxins 2010, 2, 2622–2644. [Google Scholar] [CrossRef] [PubMed]
- Hussain, G.; Wang, J.; Rasul, A.; Anwar, H.; Qasim, M.; Zafar, S.; Aziz, N.; Razzaq, A.; Hussain, R.; de Aguilar, J.G.; et al. Current Status of Therapeutic Approaches against Peripheral Nerve Injuries: A Detailed Story from Injury to Recovery. Int. J. Biol. Sci. 2020, 16, 116–134. [Google Scholar] [CrossRef]
- Townsend, S.A.; Evrony, G.D.; Gu, F.X.; Schulz, M.P.; Brown, R.H.; Langer, R. Tetanus toxin C fragment-conjugated nanoparticles for targeted drug delivery to neurons. Biomaterials 2007, 28, 5176–5184. [Google Scholar] [CrossRef]
- Chen, C.; Fu, Z.; Kim, J.J.P.; Barbieri, J.T.; Baldwin, M.R. Gangliosides as High Affinity Receptors for Tetanus Neurotoxin. J. Biol. Chem. 2009, 284, 26569–26577. [Google Scholar] [CrossRef]
- Montecucco, C.; Rossetto, O.; Schiavo, G. Presynaptic receptor arrays for clostridial neurotoxins. Trends Microbiol. 2004, 12, 442–446. [Google Scholar] [CrossRef]
- Schmieg, N.; Menendez, G.; Schiavo, G.; Terenzio, M. Signalling endosomes in axonal transport: Travel updates on the molecular highway. Semin. Cell Dev. Biol. 2014, 27, 32–43. [Google Scholar] [CrossRef]
- Bayart, C.; Mularoni, A.; Hemmani, N.; Kerachni, S.; Jose, J.; Gouet, P.; Paladino, J.; Le Borgne, M. Tetanus Toxin Fragment C: Structure, Drug Discovery Research and Production. Pharmaceuticals 2022, 15, 756. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Mukhopadhyay, C.D. Exosome as drug delivery system: Current advancements. Extracell. Vesicle 2024, 3, 100032. [Google Scholar] [CrossRef]
- Putzu, G.A.; Figarella-Branger, D.; Bouvier-Labit, C.; Liprandi, A.; Bianco, N.; Pellissier, J.F. Immunohistochemical localization of cytokines, C5b-9 and ICAM-1 in peripheral nerve of Guillain-Barré syndrome. J. Neurol. Sci. 2000, 174, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Langert, K.A.; Von Zee, C.L.; Stubbs, E.B., Jr. Tumour necrosis factor α enhances CCL2 and ICAM-1 expression in peripheral nerve microvascular endoneurial endothelial cells. ASN Neuro 2013, 5, e00104. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Chittasupho, C.; Duangrat, C.; Siahaan, T.J.; Berkland, C. PLGA nanoparticle--peptide conjugate effectively targets intercellular cell-adhesion molecule-1. Bioconjug Chem. 2008, 19, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Fan, B.; Li, C.; Szalad, A.; Wang, L.; Pan, W.; Zhang, R.; Chopp, M.; Zhang, Z.G.; Liu, X.S. Mesenchymal stromal cell-derived exosomes ameliorate peripheral neuropathy in a mouse model of diabetes. Diabetologia 2020, 63, 431–443. [Google Scholar] [CrossRef]
- Fan, B.; Chopp, M.; Zhang, Z.G.; Liu, X.S. Treatment of diabetic peripheral neuropathy with engineered mesenchymal stromal cell-derived exosomes enriched with microRNA-146a provide amplified therapeutic efficacy. Exp. Neurol. 2021, 341, 113694. [Google Scholar] [CrossRef]
- Kalvala, A.K.; Bagde, A.; Arthur, P.; Kulkarni, T.; Bhattacharya, S.; Surapaneni, S.; Patel, N.K.; Nimma, R.; Gebeyehu, A.; Kommineni, N.; et al. Cannabidiol-Loaded Extracellular Vesicles from Human Umbilical Cord Mesenchymal Stem Cells Alleviate Paclitaxel-Induced Peripheral Neuropathy. Pharmaceutics 2023, 15, 554. [Google Scholar] [CrossRef]
- Bercsenyi, K.; Schmieg, N.; Bryson, J.B.; Wallace, M.; Caccin, P.; Golding, M.; Zanotti, G.; Greensmith, L.; Nischt, R.; Schiavo, G. Nidogens are therapeutic targets for the prevention of tetanus. Science 2014, 346, 1118–1123. [Google Scholar] [CrossRef]
- Ma, S.-R.; Xia, H.-F.; Gong, P.; Yu, Z.-L. Red Blood Cell-Derived Extracellular Vesicles: An Overview of Current Research Progress, Challenges, and Opportunities. Biomedicines 2023, 11, 2798. [Google Scholar] [CrossRef]
- Liu, W.-z.; Ma, Z.-j.; Kang, X.-w. Current status and outlook of advances in exosome isolation. Anal. Bioanal. Chem. 2022, 414, 7123–7141. [Google Scholar] [CrossRef] [PubMed]
- Sidhom, K.; Obi, P.O.; Saleem, A. A Review of Exosomal Isolation Methods: Is Size Exclusion Chromatography the Best Option? Int. J. Mol. Sci. 2020, 21, 6466. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Kim, E.H.; Kwak, G.; Chi, S.G.; Kim, S.H.; Yang, Y. Exosomes: Cell-Derived Nanoplatforms for the Delivery of Cancer Therapeutics. Int. J. Mol. Sci. 2020, 22, 14. [Google Scholar] [CrossRef] [PubMed]
- Mehryab, F.; Rabbani, S.; Shahhosseini, S.; Shekari, F.; Fatahi, Y.; Baharvand, H.; Haeri, A. Exosomes as a next-generation drug delivery system: An update on drug loading approaches, characterization, and clinical application challenges. Acta Biomater. 2020, 113, 42–62. [Google Scholar] [CrossRef]
- Yin, Y.; Han, X.; Li, C.; Sun, T.; Li, K.; Liu, X.; Liu, M. The status of industrialization and development of exosomes as a drug delivery system: A review. Front. Pharmacol. 2022, 13, 961127. [Google Scholar] [CrossRef]
- Hussen, B.M.; Faraj, G.S.H.; Rasul, M.F.; Hidayat, H.J.; Salihi, A.; Baniahmad, A.; Taheri, M.; Ghafouri-Frad, S. Strategies to overcome the main challenges of the use of exosomes as drug carrier for cancer therapy. Cancer Cell Int. 2022, 22, 323. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krishnan, M.A.; Alimi, O.A.; Pan, T.; Kuss, M.; Korade, Z.; Hu, G.; Liu, B.; Duan, B. Engineering Neurotoxin-Functionalized Exosomes for Targeted Delivery to the Peripheral Nervous System. Pharmaceutics 2024, 16, 102. https://doi.org/10.3390/pharmaceutics16010102
Krishnan MA, Alimi OA, Pan T, Kuss M, Korade Z, Hu G, Liu B, Duan B. Engineering Neurotoxin-Functionalized Exosomes for Targeted Delivery to the Peripheral Nervous System. Pharmaceutics. 2024; 16(1):102. https://doi.org/10.3390/pharmaceutics16010102
Chicago/Turabian StyleKrishnan, Mena Asha, Olawale A. Alimi, Tianshu Pan, Mitchell Kuss, Zeljka Korade, Guoku Hu, Bo Liu, and Bin Duan. 2024. "Engineering Neurotoxin-Functionalized Exosomes for Targeted Delivery to the Peripheral Nervous System" Pharmaceutics 16, no. 1: 102. https://doi.org/10.3390/pharmaceutics16010102
APA StyleKrishnan, M. A., Alimi, O. A., Pan, T., Kuss, M., Korade, Z., Hu, G., Liu, B., & Duan, B. (2024). Engineering Neurotoxin-Functionalized Exosomes for Targeted Delivery to the Peripheral Nervous System. Pharmaceutics, 16(1), 102. https://doi.org/10.3390/pharmaceutics16010102






