Conjugation with Tris Decreases the Risk of Ketoprofen-Induced Mucosal Damage and Reduces Inflammation-Associated Methane Production in a Rat Model of Colitis
Abstract
:1. Introduction
2. Materials and Methods
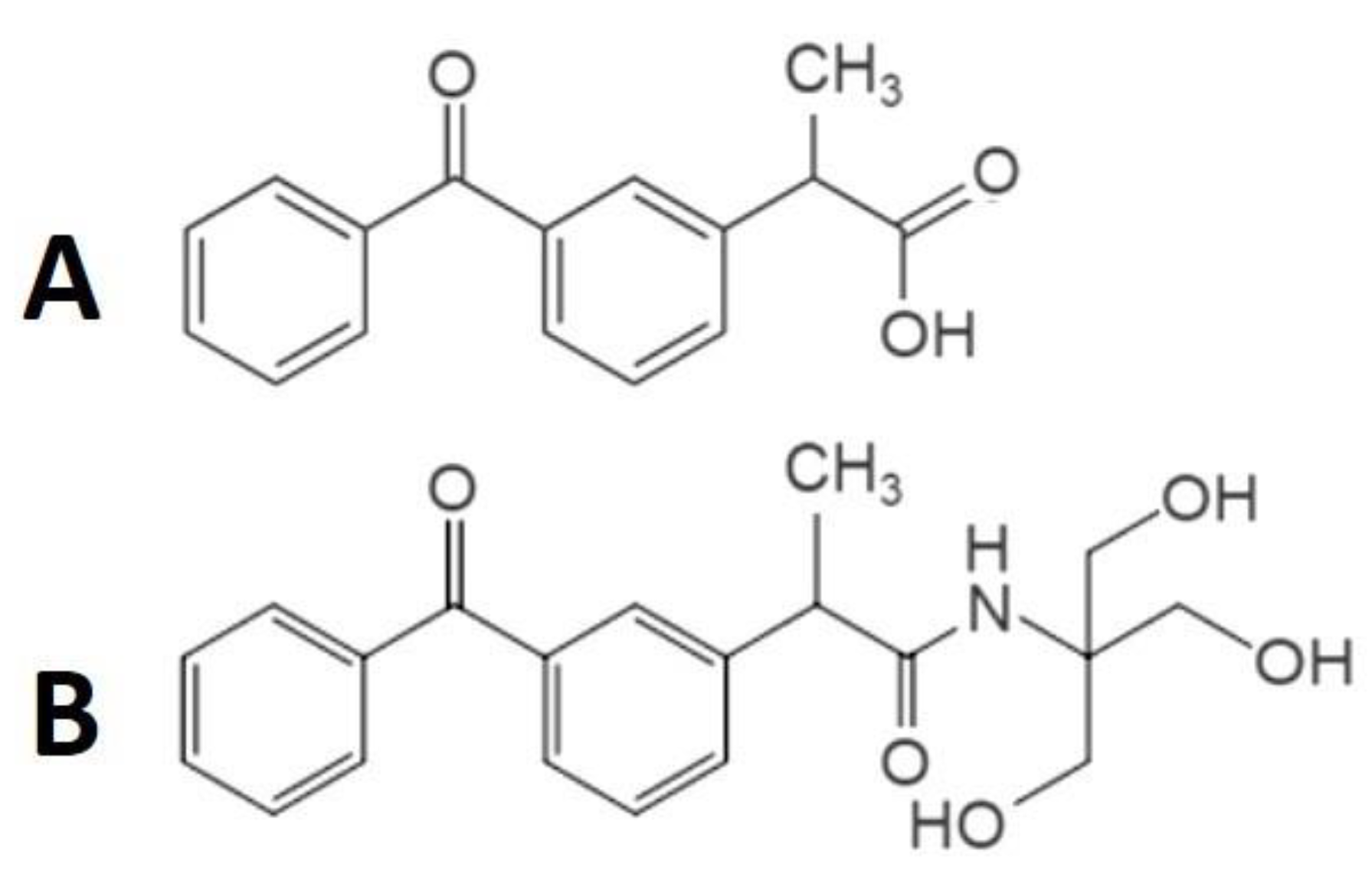
2.1. Chemical Synthesis and Characterisations of Ket-Tris Conjugate
2.2. In Vivo Studies—Animals
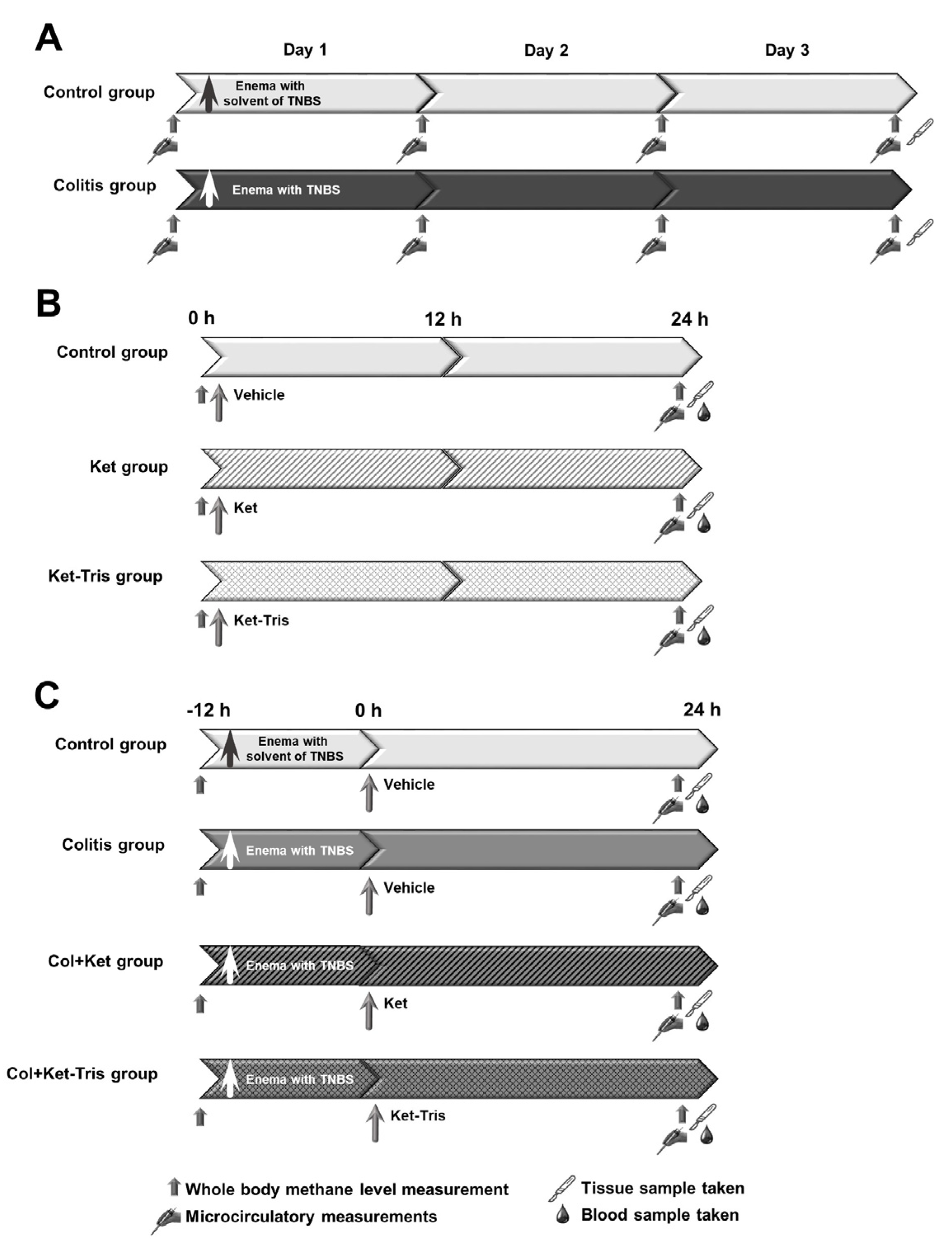
2.3. Experimental Protocol 1
2.4. Experimental Protocol 2
2.5. Experimental Protocol 3
2.6. Direct Measurements on the GI Microcirculation
2.7. In Vivo Detection of Mucosal Damage
2.8. Whole-Body Methane Emissions Measurement
2.9. In Vitro Studies
2.9.1. Tissue Biopsies
2.9.2. Tissue Xanthine Oxidoreductase (XOR) Activity
2.9.3. Tissue Myeloperoxidase (MPO) Activity
2.9.4. Tissue Nitrite/Nitrate (NOx) Levels
2.9.5. Tissue Cytochrome c Oxidase (Cytc) Level
2.9.6. Tissue Malondialdehyde (MDA) Assay
2.9.7. Plasma Tumour Necrosis Factor Alpha (TNF-α) Level
2.10. Statistical Analysis
3. Results
3.1. Study 1
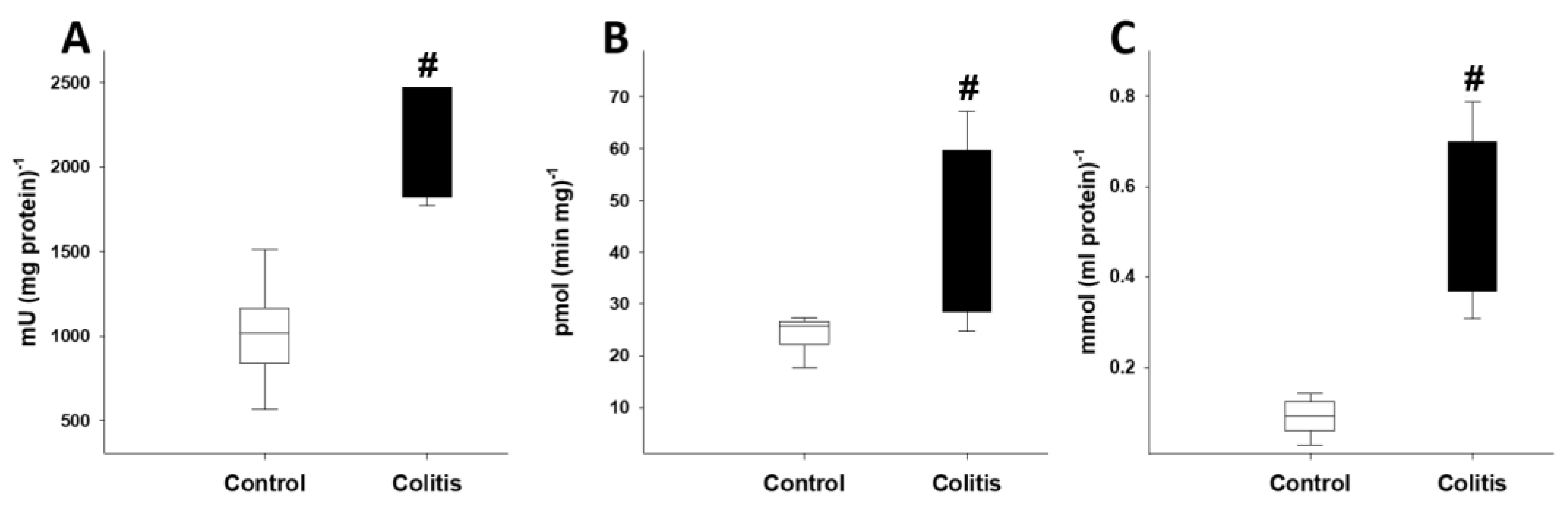
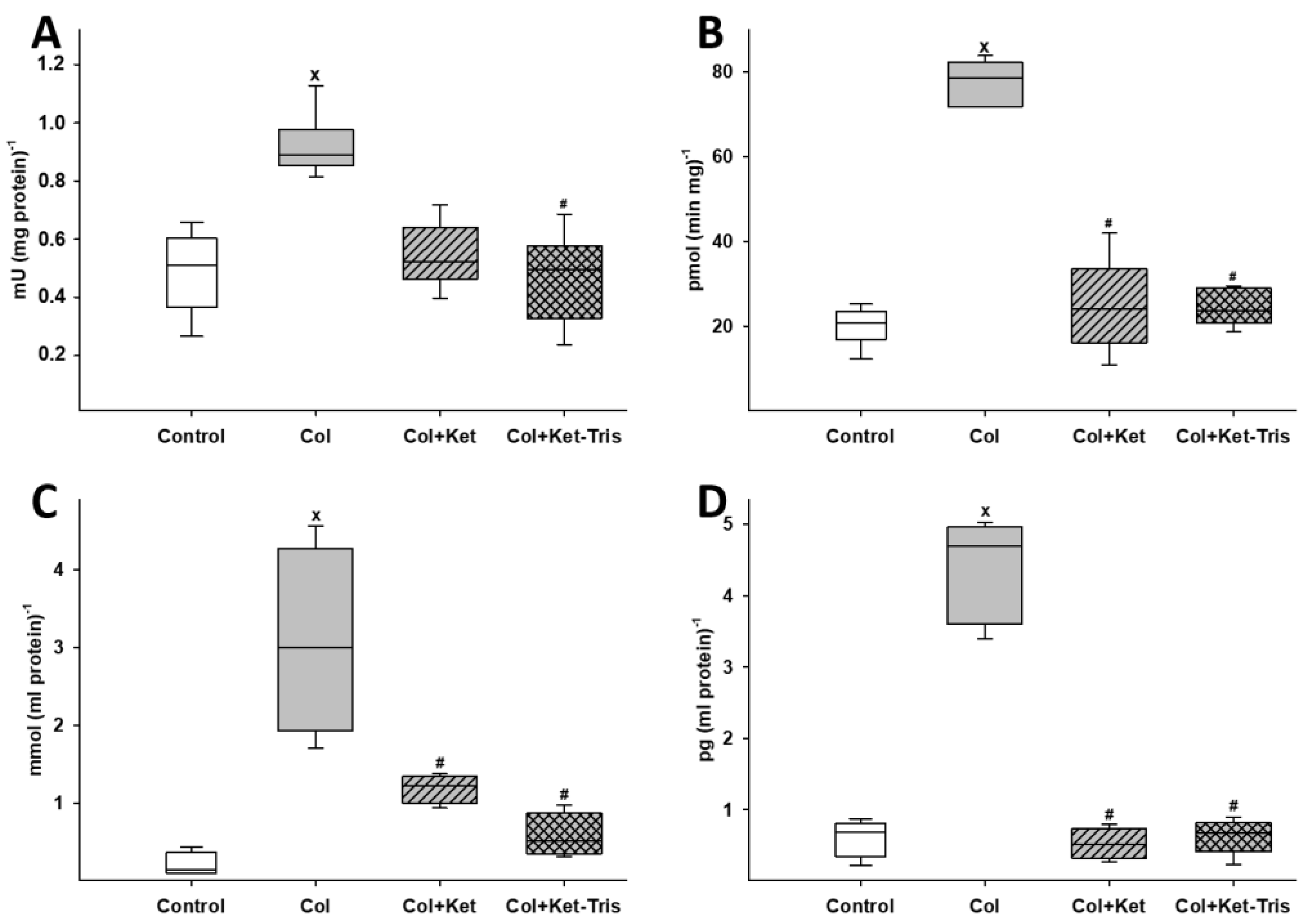
3.1.1. Changes in Inflammatory Mediators after Colitis Induction
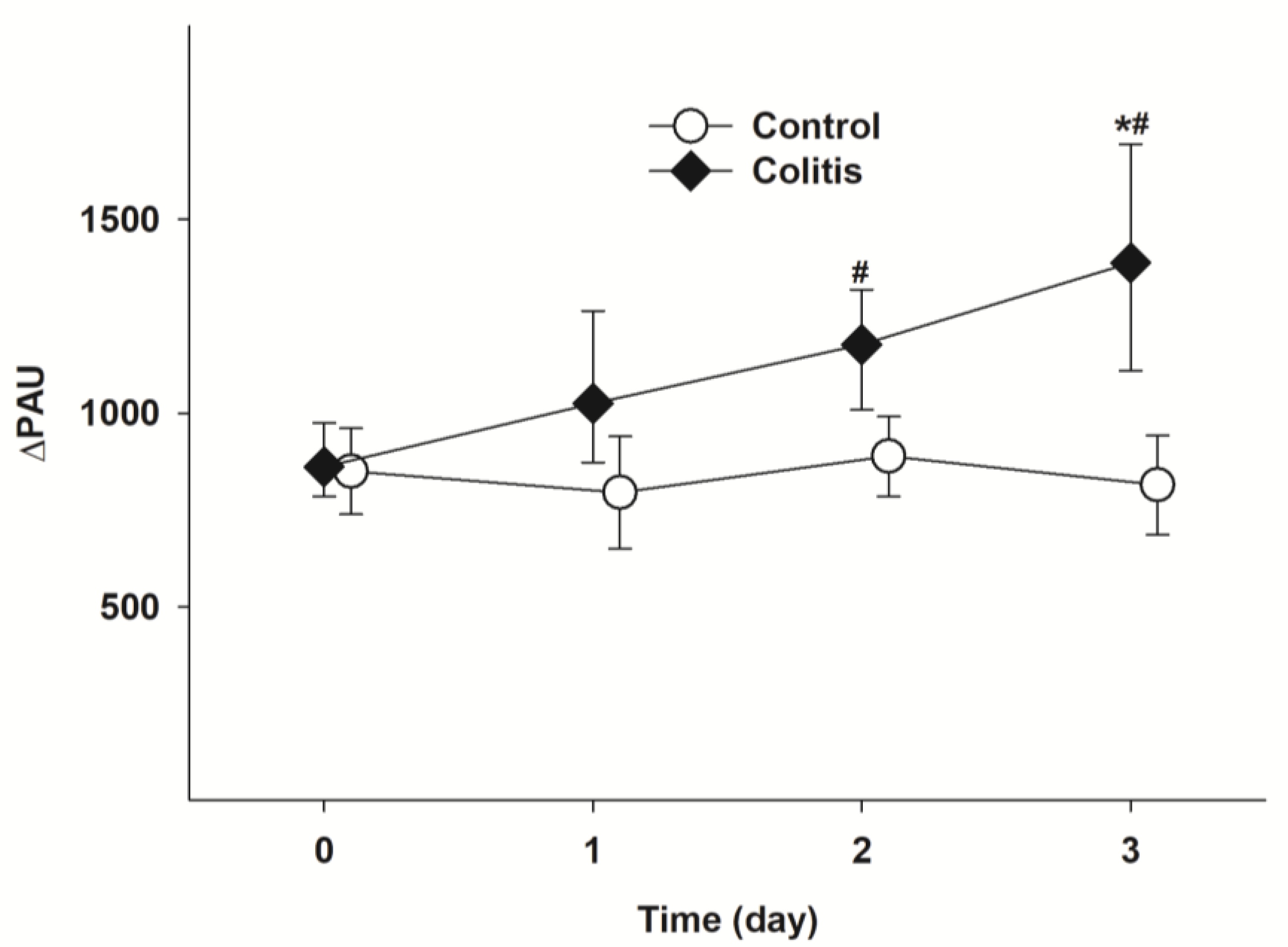
3.1.2. Changes in Microcirculatory Parameters
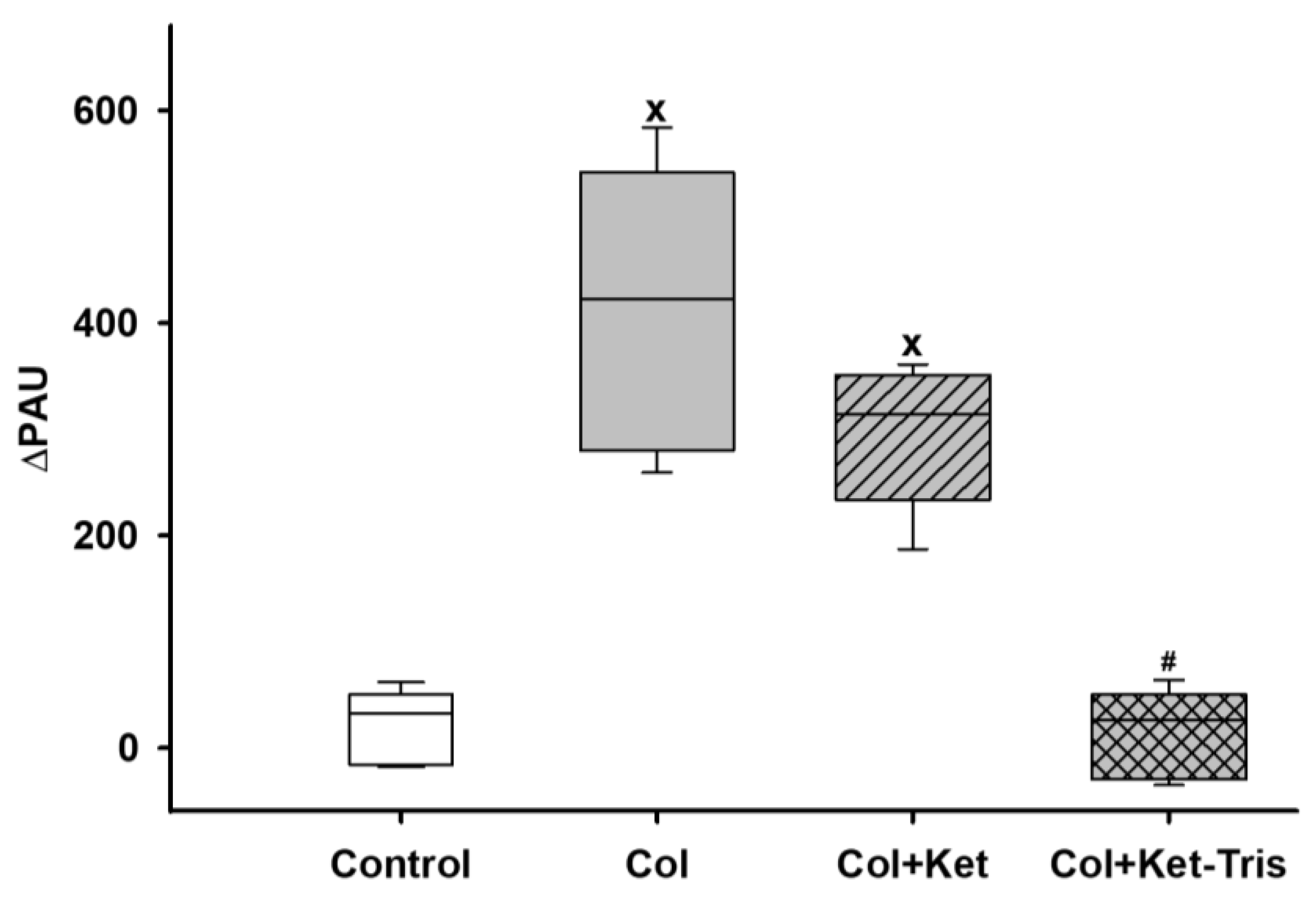
3.1.3. Changes in Whole-Body Methane Emission
3.2. Study 2—Effects of Ket-Tris Conjugate
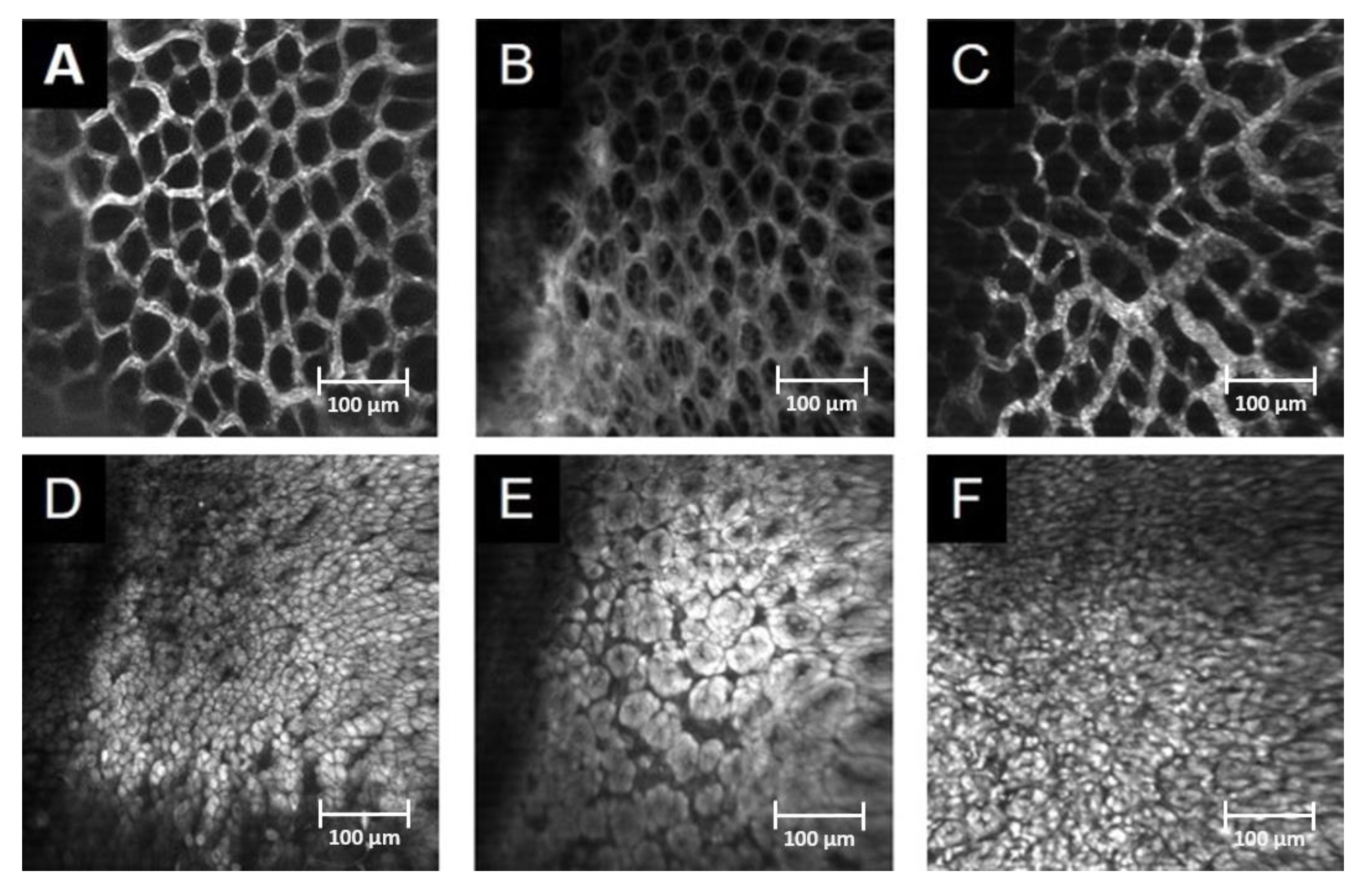
3.2.1. In Vivo Detection of Gastric Mucosal Injury
3.2.2. Changes in Biochemical Parameters
3.2.3. In Vivo Detection of the Microcirculation
3.2.4. Changes in Whole-Body Methane Emission
3.3. Study 3
3.3.1. Changes in Biochemical Factors
3.3.2. In Vivo Detection of Mucosal Damage in the Colon and Serosal Microcirculation with In Vivo Microscopy
3.3.3. Changes in Whole-Body Methane Emissions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wongrakpanich, S.; Wongrakpanich, A.; Melhado, K.; Rangaswami, J. A comprehensive review of non-steroidal anti-inflammatory drug use in the elderly. Aging Dis. 2018, 9, 143–150. [Google Scholar] [CrossRef]
- Bacchi, S.; Palumbo, P.; Sponta, A.; Coppolino, M.F. Clinical pharmacology of non-steroidal anti-inflammatory drugs: A review. Antiinflamm. Antiallergy Agents Med. Chem. 2012, 11, 52–64. [Google Scholar] [CrossRef]
- Lanas, A.; Dumonceau, J.-M.; Hunt, R.H.; Fujishiro, M.; Scheiman, J.M.; Gralnek, I.M.; Campbell, H.E.; Rostom, A.; Villanueva, C.; Sung, J.J.Y. Non-variceal upper gastrointestinal bleeding. Nat. Rev. Dis. Prim. 2018, 4, 18020. [Google Scholar] [CrossRef] [PubMed]
- Varga, G.; Lajkó, N.; Ugocsai, M.; Érces, D.; Horváth, G.; Tóth, G.; Boros, M.; Ghyczy, M. Reduced mucosal side-effects of acetylsalicylic acid after conjugation with tris-hydroxymethyl-aminomethane. Synthesis and biological evaluation of a new anti-inflammatory compound. Eur. J. Pharmacol. 2016, 781, 181–189. [Google Scholar] [CrossRef]
- Varga, G.; Ugocsai, M.; Hartmann, P.; Lajkó, N.; Molnár, R.; Szűcs, S.; Jász, D.K.; Érces, D.; Ghyczy, M.; Tóth, G.; et al. Acetylsalicylic acid-tris-hydroxymethyl-aminomethane reduces colon mucosal damage without causing gastric side effects in a rat model of colitis. Inflammopharmacology 2018, 26, 261–271. [Google Scholar] [CrossRef]
- Kulabas, N.; Set, I.; Aktay, G.; Gürsoy, S.; Danis, Ö.; Ogan, A.; Sag, S.; Erzincan, P.; Helvacioglu, S.; Hamitoglu, M.; et al. Identification of some novel amide conjugates as potent and gastric sparing anti-inflammatory agents: In vitro, in vivo, in silico studies and drug safety evaluation. J. Mol. Struct. 2023, 1285, 135521. [Google Scholar] [CrossRef]
- Kantor, T.G. Ketoprofen: A review of its pharmacologic and clinical properties. Pharmacotherapy 1986, 6, 93–103. [Google Scholar] [CrossRef]
- Lastra, C.A.; Nieto, A.; Martín, M.J.; Cabré, F.; Herrerías, J.M.; Motilva, V. Gastric toxicity of racemic ketoprofen and its enantiomers in rat: Oxygen radical generation and COX-expression. Inflamm. Res. 2002, 51, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Jerussi, T.P.; Caubet, J.F.; McCray, J.E.; Handley, D.A. Clinical endoscopic evaluation of the gastroduodenal tolerance to (R)-ketoprofen, (R)-flurbiprofen, racemic ketoprofen, and paracetamol: A randomized, single-blind, placebo-controlled trial. J. Clin. Pharmacol. 1998, 38, 19S–24S. [Google Scholar] [CrossRef] [PubMed]
- Warner, T.D.; Giuliano, F.; Vojnovic, I.; Bukasa, A.; Mitchell, J.A.; Vane, J.R. Nonsteroid drug selectivities for cyclo-oxygenase-1 rather than cyclo-oxygenase-2 are associated with human gastrointestinal toxicity: A full in vitro analysis. Proc. Natl. Acad. Sci. USA 1999, 96, 7563–7568. [Google Scholar] [CrossRef] [PubMed]
- Boros, M.; Keppler, F. Methane production and bioactivity-A link to oxido-reductive stress. Front. Physiol. 2019, 10, 1244. [Google Scholar] [CrossRef]
- Ghyczy, M.; Torday, C.; Kaszaki, J.; Szabó, A.; Czóbel, M.; Boros, M. Hypoxia-induced generation of methane in mitochondria and eukaryotic cells: An alternative approach to methanogenesis. Cell. Physiol. Biochem. 2008, 21, 251–258. [Google Scholar] [CrossRef]
- Conrad, R. The global methane cycle: Recent advances in understanding the microbial processes involved. Env. Microbiol. Rep. 2009, 1, 285–292. [Google Scholar] [CrossRef]
- Ellermann, J.; Hedderich, R.; Böcher, R.; Thauer, R.K. The final step in methane formation. Investigations with highly purified methyl-CoM reductase (component C) from Methanobacterium thermoautotrophicum (strain marburg). Eur. J. Biochem. 1988, 172, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Boros, M.; Tuboly, E.; Meszaros, A.; Amann, A. The role of methane in mammalian physiology—Is it a gasotransmitter? J. Breath Res. 2015, 9, 014001. [Google Scholar] [CrossRef] [PubMed]
- Dupont, W.D.; Plummer, W.D. Power and sample size calculations: A review and computer program. Control. Clin. Trials 1990, 11, 116–128. [Google Scholar] [CrossRef]
- De Backer, D.; Hollenberg, S.; Boerma, C.; Goedhart, P.; Büchele, G.; Ospina-Tascon, G.; Dobbe, I.; Ince, C. How to evaluate the microcirculation: Report of a round table conference. Crit. Care 2007, 11, R101. [Google Scholar] [CrossRef] [PubMed]
- Kovács, T.; Varga, G.; Érces, D.; Tőkés, T.; Tiszlavicz, L.; Ghyczy, M.; Boros, M.; Kaszaki, J. Dietary phosphatidylcholine supplementation attenuates inflammatory mucosal damage in a rat model of experimental colitis. Shock 2012, 38, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Tuboly, E.; Szabó, A.; Erős, G.; Mohácsi, A.; Szabó, G.; Tengölics, R.; Rákhely, G.; Boros, M. Determination of endogenous methane formation by photoacoustic spectroscopy. J. Breath Res. 2013, 7, 046004. [Google Scholar] [CrossRef]
- Dumitras, D.C.; Petrus, M.; Bratu, A.M.; Popa, C. Applications of near infrared photoacoustic spectroscopy for analysis of human respiration: A review. Molecules 2020, 25, 1728. [Google Scholar] [CrossRef]
- Beckman, J.S.; Parks, D.A.; Pearson, J.D.; Marshall, P.A.; Freeman, B.A. A sensitive fluorometric assay for measuring xanthine dehydrogenase and oxidase in tissues. Free Radic. Biol. Med. 1989, 6, 607–615. [Google Scholar] [CrossRef] [PubMed]
- Kuebler, W.M.; Abels, C.; Schuerer, L.; Goetz, A.E. Measurement of neutrophil content in brain and lung tissue by a modified myeloperoxidase assay. Int. J. Microcirc. Clin. Exp. 1996, 16, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Moshage, H.; Kok, B.; Huizenga, J.R.; Jansen, P.L. Nitrite and nitrate determinations in plasma: A critical evaluation. Clin. Chem. 1995, 41 Pt 1, 892–896. [Google Scholar] [CrossRef]
- Szarka, A.; Horemans, N.; Banhegyi, G.; Asard, H. Facilitated glucose and dehydroascorbate transport in plant mitochondria. Arch. Biochem. Biophys. 2004, 428, 73–80. [Google Scholar] [CrossRef]
- Placer, Z.A.; Cushman, L.L.; Johnson, B.C. Estimation of product of lipid peroxidation (malonyl dialdehyde) in biochemical systems. Anal. Biochem. 1966, 16, 359–364. [Google Scholar] [CrossRef]
- McMahon, S.B.; Dargan, P.; Lanas, A.; Wiffen, P. The burden of musculoskeletal pain and the role of topical non-steroidal anti-inflammatory drugs (NSAIDs) in its treatment. Ten underpinning statements from a global pain faculty. Curr. Med. Res. Opin. 2021, 37, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Kaur, B.; Singh, P. Inflammation: Biochemistry, cellular targets, anti-inflammatory agents and challenges with special emphasis on cyclooxygenase-2. Bioorg. Chem. 2022, 121, 105663. [Google Scholar] [CrossRef]
- Atzeni, F.; Masala, I.F.; Bagnasco, M.; Lanata, L.; Mantelli, F.; Sarzi-Puttini, P. Comparison of efficacy of ketoprofen and ibuprofen in treating pain in patients with rheumatoid arthritis: A systematic review and meta-analysis. Pain Ther. 2021, 10, 577–588. [Google Scholar] [CrossRef]
- Kuczyńska, J.; Nieradko-Iwanicka, B. Future prospects of ketoprofen in improving the safety of the gastric mucosa. Biomed. Pharmacother. 2021, 139, 111608. [Google Scholar] [CrossRef]
- Kumar, M.; Kumar, D.; Kumar, S.; Kumar, A.; Mandal, U.K. A Recent Review on Bio-availability Enhancement of Poorly Water-soluble Drugs by using Bioenhancer and Nanoparticulate Drug Delivery System. Curr. Pharm. Des. 2022, 28, 3212–3224. [Google Scholar] [CrossRef]
- Pergolizzi, J.V.; Breve, F.; Magnusson, P.; LeQuang, J.K.; Varassi, G. Current and emerging COX inhibitors for treating postoperative pain following oral surgery. Expert Opin. Pharm. 2023, 24, 347–358. [Google Scholar] [CrossRef] [PubMed]
- Evans, L.; Spelman, M. The problem of non-compliance with drug therapy. Drugs 1983, 25, 63–76. [Google Scholar] [CrossRef]
- Scheen, A.J.; Giet, D. Non compliance to medical therapy; causes, consequences, solutions. Rev. Med. Liege 2010, 65, 239–245. [Google Scholar] [PubMed]
- Bhandari, S.V.; Bothara, K.G.; Raut, M.K.; Patil, A.A.; Sarkate, A.P.; Mokale, V.J. Design, synthesis and evaluation of antiinflammatory, analgesic and ulcerogenicity studies of novel S-substituted phenacyl-1,3,4-oxadiazole-2-thiol and Schiff bases of diclofenac acid as nonulcerogenic derivatives. Bioorg. Med. Chem. 2008, 16, 1822–1831. [Google Scholar] [CrossRef] [PubMed]
- Ilango, K.; Valentina, P.; Kumar, G.; Dixit, D.; Nilewar, S.; Kathiravan, M.K. Design, Synthesis and QSAR Studies on a series of 2, 5-disubstituted-1,3,4-oxadiazole derivatives of diclofenac and naproxen for analgesic and anti-inflammatory activity. Med. Chem. 2015, 11, 753–763. [Google Scholar] [CrossRef] [PubMed]
- Nose, K.; Nunome, Y.; Kondo, T.; Araki, S.; Tsuda, T. Identification of gas emanated from human skin: Methane, ethylene, and ethane. Anal. Sci. 2005, 21, 625–628. [Google Scholar] [CrossRef]
- Bársony, A.; Vida, N.; Gajda, Á.; Rutai, A.; Mohácsi, Á.; Szabó, A.; Boros, M.; Varga, G.; Érces, D. Methane exhalation can monitor the microcirculatory changes of the intestinal mucosa in a large animal model of hemorrhage and fluid resuscitation. Front. Med. 2020, 7, 567260. [Google Scholar] [CrossRef]
- Keppler, F.; Hamilton, J.T.G.; Brass, M.; Röckmann, T. Methane emissions from terrestrial plants under aerobic conditions. Nature 2006, 439, 187–191. [Google Scholar] [CrossRef]
- Wang, Q.; Alowaifeer, A.; Kerner, P.; Balasubramanian, N.; Patterson, A.; Christian, W.; Tarver, A.; Dore, J.E.; Hatzenpichler, R.; Bothner, B.; et al. Aerobic bacterial methane synthesis. Proc. Natl. Acad. Sci. USA 2021, 118, e2019229118. [Google Scholar] [CrossRef]
- Ghyczy, M.; Torday, C.; Boros, M. Simultaneous generation of methane, carbon dioxide, and carbon monoxide from choline and ascorbic acid-a defensive mechanism against reductive stress? FASEB J. 2003, 17, 1124–1126. [Google Scholar] [CrossRef]
- Liu, C.; Zhang, J. Methane might be made by all living organisms. Nature 2022, 603, 396–397. [Google Scholar] [CrossRef] [PubMed]
- Ernst, L.; Steinfeld, B.; Barayeu, U.; Klintzsch, T.; Kurth, M.; Grimm, D.; Dick, T.P.; Rebelein, J.G.; Bischofs, I.B.; Keppler, F. Methane formation driven by reactive oxygen species across all living organisms. Nature 2022, 603, 482–487. [Google Scholar] [CrossRef] [PubMed]



| Parameters | Control | Ket | Ket-Tris | |
|---|---|---|---|---|
| Tissue damage | Median 25p; 75p | 0.15 0; 0.3 | 5 a 4.12; 5.87 | 0.275 b 0; 0.3 |
| MPO | Median 25p; 75p | 1.7 1.06; 1.85 | 2.4 a 2.16; 2.16 | 1.6 b 1.5; 1.83 |
| XOR | Median 25p; 75p | 18.7 14.9; 27.2 | 41.9 a 33.9; 46.2 | 23.5 b 18.9; 26.1 |
| NOx | Median 25p; 75p | 0.62 0.51; 20 | 1.37 a 1.14; 1.84 | 0.65 b 0.61; 0.68 |
| MDA | Median 25p; 75p | 0.21 0.15; 0.42 | 0.88 a 0.81; 1.38 | 0.35 b 0.29; 0.39 |
| Cytc | Median 25p; 75p | 0.68 0.34; 0.8 | 1.89 a 1.35; 1.95 | 0.67 b 0.53; 0.7 |
| TNF-α | Median 25p; 75p | 3.17 2.7; 3.3 | 4.4 a 3.7; 7.4 | 3.23 b 2.97; 3.55 |
| Parameters | Control | Ket | Ket-Tris | |
|---|---|---|---|---|
| Stomach | Median 25p; 75p | 882 779; 967 | 1084 a 982; 1245 | 763 b 703; 876 |
| Duodenum | Median 25p; 75p | 744 694; 798 | 1084 a 1015; 1229 | 676 b 536; 897 |
| Jejunum | Median 25p; 75p | 762 683; 824 | 1077 a 960; 1267 | 754 b 679; 805 |
| Ileum | Median 25p; 75p | 827 742; 906 | 1012 a 972; 1084 | 781 b 694; 864 |
| Colon | Median 25p; 75p | 946 837; 1034 | 984 754; 1069 | 977 862; 1048 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ugocsai, M.; Bársony, A.; Varga, R.A.; Gajda, Á.; Vida, N.; Lajkó, N.; Rónaszéki, B.; Tóth, G.; Boros, M.; Érces, D.; et al. Conjugation with Tris Decreases the Risk of Ketoprofen-Induced Mucosal Damage and Reduces Inflammation-Associated Methane Production in a Rat Model of Colitis. Pharmaceutics 2023, 15, 2329. https://doi.org/10.3390/pharmaceutics15092329
Ugocsai M, Bársony A, Varga RA, Gajda Á, Vida N, Lajkó N, Rónaszéki B, Tóth G, Boros M, Érces D, et al. Conjugation with Tris Decreases the Risk of Ketoprofen-Induced Mucosal Damage and Reduces Inflammation-Associated Methane Production in a Rat Model of Colitis. Pharmaceutics. 2023; 15(9):2329. https://doi.org/10.3390/pharmaceutics15092329
Chicago/Turabian StyleUgocsai, Melinda, Anett Bársony, Réka Anna Varga, Ámos Gajda, Noémi Vida, Norbert Lajkó, Benedek Rónaszéki, Gábor Tóth, Mihály Boros, Dániel Érces, and et al. 2023. "Conjugation with Tris Decreases the Risk of Ketoprofen-Induced Mucosal Damage and Reduces Inflammation-Associated Methane Production in a Rat Model of Colitis" Pharmaceutics 15, no. 9: 2329. https://doi.org/10.3390/pharmaceutics15092329
APA StyleUgocsai, M., Bársony, A., Varga, R. A., Gajda, Á., Vida, N., Lajkó, N., Rónaszéki, B., Tóth, G., Boros, M., Érces, D., & Varga, G. (2023). Conjugation with Tris Decreases the Risk of Ketoprofen-Induced Mucosal Damage and Reduces Inflammation-Associated Methane Production in a Rat Model of Colitis. Pharmaceutics, 15(9), 2329. https://doi.org/10.3390/pharmaceutics15092329







