Abstract
Disulfiram (DSF) is a thiocarbamate based drug that has been approved for treating alcoholism for over 60 years. Preclinical studies have shown that DSF has anticancer efficacy, and its supplementation with copper (CuII) significantly potentiates the efficacy of DSF. However, the results of clinical trials have not yielded promising results. The elucidation of the anticancer mechanisms of DSF/Cu (II) will be beneficial in repurposing DSF as a new treatment for certain types of cancer. DSF’s anticancer mechanism is primarily due to its generating reactive oxygen species, inhibiting aldehyde dehydrogenase (ALDH) activity inhibition, and decreasing the levels of transcriptional proteins. DSF also shows inhibitory effects in cancer cell proliferation, the self-renewal of cancer stem cells (CSCs), angiogenesis, drug resistance, and suppresses cancer cell metastasis. This review also discusses current drug delivery strategies for DSF alone diethyldithocarbamate (DDC), Cu (II) and DSF/Cu (II), and the efficacious component Diethyldithiocarbamate–copper complex (CuET).
1. Introduction
There has been tremendous progress in the fields of drug discovery, tumor biology, nanomedicine, and targeted drug delivery for improving treatment and patient care, yet cancer remains one of the leading causes of death. The process of discovering new chemical entities and their development into anticancer drugs can be very time consuming and expensive. Drug repurposing via new drug delivery systems is a relatively less time-consuming, simple, and cost-effective strategy in treating many diseases [1,2]. With the advancement of computational and rapid screening technologies, new drug candidates are now available for cancer treatment. However, the efficient delivery of these drugs to cancer tumors still requires novel drug delivery devices and methods [3,4].
Copper stimulates the proliferation and migration of endothelial cells and is required for the secretion of several angiogenic factors by tumor cells [5]. However, copper chelation has been reported to produce a decrease in the secretion of many of these factors [5,6]. Recently, Based on clinical data indicating that elevated serum copper levels associated with many cancer tumors, many copper chelators are being developed and tested in clinical trials in recent years [7]. Although it remains to be determined the mechanism which copper chelation suppresses the growth of endothelial cells and hinders the secretion of angiogenic factors by tumors is not entirely clear, it is has been hypothesized to result from effects on copper-dependent enzymes, transporters, and chaperones [8].
Recently, a novel cell death pathway, distinct from apoptosis, necroptosis, pyroptosis, and ferroptosis, induced by copper, has been identified, and designated as cuproptisis [9]. Cuproptosis is significantly correlated to cellular metabolism and is frequently observed in certain types of cancer that have high levels of aerobic respiration, including melanoma, breast cancer, leukemia, and drug-resistant cancers [10]. Copper ionophores have played a crucial role in the identification of cuproptosis and have been considered as possible anticancer treatments [11,12]. Diethyldithiocarbamate (DDC), an active metabolite of the drug, disulfiram (DSF), has been reported to be a copper ionophore that has in vitro and in vivo efficacy as an anticancer compound. [11].
Disulfiram (DSF,) is a thiocarbamate derivative that has been used to treat alcoholism since 1951 [13]. DSF inhibits the enzyme aldehyde dehydrogenase 1 (ALDH1), which significantly inhibits the biotransformation of ethanol to ethanol at the acetaldehyde stage [14], thereby increasing the levels of ALDH1, which produces various adverse effects following the ingestion of ethanol, decreases or discourage ethanol intake [15]. Interestingly, ALDH1 is present found in cancer cells with stem cell properties, and it catalyzes the oxidation of intracellular aldehydes and produces multidrug resistance [16]. Subsequently, clinical data suggested that DSF had anticancer efficacy [17]. In addition, DSF was shown to regulate the balance of reactive oxygen species (ROS) and glutathione (GSH) [18], inhibit the activity of the ubiquitin proteasome system (UPS) [19], and regulate intracellular signaling [20,21] and the activity of other enzymes, which could play a role in mediating its anticancer efficacy [22,23,24]. Indeed, these mechanisms could induce cancer cell death, decrease the stemness of cancer cells [25], decrease angiogenesis, and overcome drug resistance [26,27].
As mentioned earlier, trace metals are essential for the survival of cancer cells [28,29]. Compared with normal cells, many tumor cells have a 2–3-fold higher concentration of copper [30]. DSF is a potent chelator of copper, and DSF can bio-transform the pro-angiogenic activity of copper to a specific compound that induces cancer cell death [31]. Although DSF has shown promise in both laboratory and animal studies, certain clinical trials with cancer patients have been unsuccessful due to treatment requiring high doses and the expectation partially owing to the rapid biodegradation of the DSF [32,33]. Cu (II) chelation of the primary DSF metabolite, diethyldithiocarbamate (DDC), is crucial for inducing the death of tumor cells [34,35]. The copper-dependent anticancer efficacy of DSF has resulted in an increase in research related to DSF/Cu (II) [36,37]. DSF/Cu (II) has been reported to be efficacious in a variety of cancers, including liver cancer [38], ovarian cancer [39], prostate cancer [25], lung cancer [40], glioblastoma (GBM) [41], and breast cancer [42] (Figure 1). The anticancer efficacy of DSF is most likely due to the bio-transformation of DSF to diethyldithiocarbamate (DDTC), which forms an intracellular copper–DDTC complex (Cu(DDTC)2), which has been shown to be the most efficacious anticancer compound [43]. DSF can induce ferroptosis and cuproptosis in different types of cancer cells [44]. A summary of various clinical trials assessing the efficacy of DSF-based cancer is shown in Table 1. Some clinical trials have investigated the use of DSF for treating solid tumors, with some reporting improved progression-free survival and overall survival, compared the control groups. Adverse effects were generally mild and resolved following a decrease in the dose of DSF. Two single-arm trials in glioblastoma patients showed positive effects, while a randomized controlled trial in NSCLC patients also reported an increase in patient survival [45,46,47]. However, the response to DSF varied among patients, and further in vitro and animal studies are needed to explore the optimal concentration and sensitivity type. Overall, DSF appears safe and effective in prolonging survival in cancer patients [48].
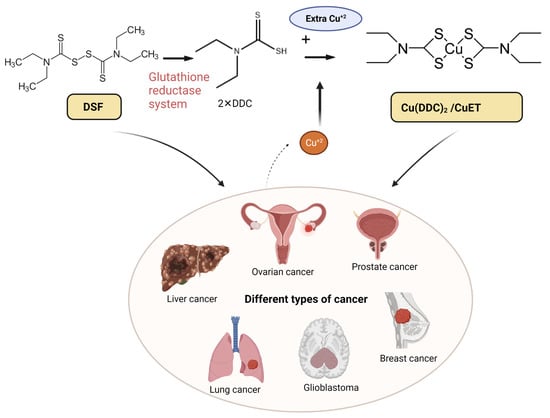
Figure 1.
The chelation mechanism of DSF and Cu (II) and the use of DSF-based therapy for different types of cancer. DSF metabolizes to diethyldithiocarbamate (DDC or ET) via the glutathione reductase system; the active anti-cancer ingredient DDC further chelates with Cu (II) and forms Cu(DDC)2 (aka CuET), which has anti-cancer efficacy. The high dose of DSF alone and low dose of DSF/Cu (II) are effective in various cancers including liver, ovarian, prostate, breast, lung cancer, and glioblastoma (GBM). Created with BioRender.com. accessed on 19 April 2023.

Table 1.
A summary of studies on DSF-based clinical trials (http://clinicaltrials.gov) accessed on 10 April 2023.
2. Anticancer Mechanisms of DSF/Cu (II)
It has been revealed that the anti-cancer mechanism of DSF/Cu (II) may be mediated by the regulation of reactive oxygen species (ROS), enzyme activity regulation, induction of DNA damage, proteasome inhibition, and transcription factors [24] (Figure 2). Additionally, DSF/Cu (II) also exhibits immunomodulatory effects on tumor microenvironment (TME).
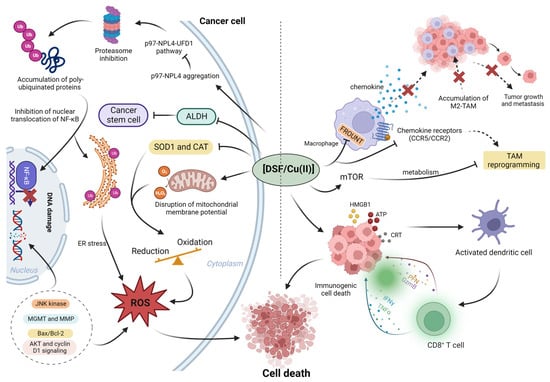
Figure 2.
The summary of roles of DSF/Cu (II) in cancer microenvironment. Left: DSF/Cu (II) inhibits the cancer proteasome activity via p97-NPL4 pathway; in addition, DSF/Cu (II) inhibits cancer-associated ALDH activity and inhibits cancer stem cells (CSCs). In the cancer microenvironment, aberrant enzyme activity, superoxide dismutase 1 (SOD1) and catalase (CAT), results in the elevation of ROS; the higher basal level of ROS benefits cancer proliferation. However, the further increased ROS to exceed cancer tolerance cause cancer death. Right, the DSF/Cu (II) reprograms the tumor-promoting macrophage M2 to anti-tumor type M1. In addition, DSF/Cu (II) transforms the immune-suppressive (cold) tumor microenvironment to the immune-active (hot) microenvironment via the induction of immunogenic cell death (ICD). Created with BioRender.com. accessed on 19 April 2023.
2.1. Disulfiram/Cu with ROS
The effects of ROS on cancer cells has been reported to becontext-dependent [49]. For example, in the initial stage of cancer development, ROS levels are100-fold higher in cancer cells compare to normal cells [22,50]. The increased levels of ROS activates signaling transduction pathways in cancer cells, regulating the activities of redox-sensitive transcription factors [22,50], and facilitating cancer cell survival and proliferation [51,52]. However, in contrast, the excessive ROS that is more than the tolerated limit of cancer can kill the cancer via cell cycle arrest and apoptosis, so the increase in the basal level of ROS in cancer cells will benefit the use of ROS-inducing anti-cancer agents [51,53].
In vitro, 1 μM of DSF was reported to increase the cytotoxic efficacy of cisplatin by increasing the accumulation of ROS [54]. The chelation of DSF with Cu (II)produces a further increase in the production of ROS [42,55,56]. The complex of DSF and Cu (II)has been reported to inhibit the enzyme superoxide dismutase 1 (SOD1), one of the major enzymesthat mitigates oxidative damage in melanoma cells [57]. The inhibition of SOD1 increases the formation of superoxide, thereby increasing oxidative stress [57]. Lipid ROS levels also increased in the presence of Zn (II) and DSF [57,58]. The increased ROS levels were shown to be essential for DSF-induced apoptosis in melanoma cells [42]. The inhibition of Glutathione reductase (GSR) inhibition by DSF disrupts glutathione GSH redox cycling, producing an accumulation of oxidized glutathione (GSSG) and a lower GSH/GSSG ratio, producing an increase in ROS level [59,60].
2.2. Enzyme Inhibition and DNA Damage
As stated earlier in this article, the presence of ALDH is an indicator of cancer stem cell (CSC) activity, which is significantly correlated with tumor progression, metastasis, and drug resistance [61]. Furthermore, the inhibition of the Hedgehog pathway and the proteins Nanog and Oct-4 (the cell stemness transcription factors) result from DSF/Cu (II) decreasing the number of CSCs, thereby inhibiting the proliferation of myeloma cells [62]. DSF inhibits the metastasis of osteosarcoma cells via irreversibly inhibiting ALDH [63,64,65]. DSF suppresses the expression of DNA topoisomerases, DNA methyltransferase, DNA polymerase, and ribonucleotide reductase [66,67]. O6-methylguanine-DNA methyltransferase (MGMT), a unique antimutagenic DNA repair protein [68,69], has been reported to be overexpressed in brain tumors [70]. Disulfiram is a direct inhibitor of MGMT, which greatly increases cancer cell death [71]. Interestingly, DSF also inactivate the enzyme phosphoglycerate dehydrogenase (PHGDH) by covalently reacting with cysteine residues that mediate DNA repair [71,72,73]. DNA damage may also be facilitated by therapeutics- induced ROS generation, which involves the opening of pores in the mitochondria [58,61]. The BRCA1 and BRCA genes are essential for the repair of double-stranded DNA breaks and homologous DNA recombination [74,75]. Individuals who have BRCA mutations are more likely to develop breast cancer comparedto people who undergo no BRCA mutations [74,75], in vitro experiments indicate that the cell viability of BRCA mutant cell lines can also be significantly decreased by DSF/Cu (II) [76].
2.3. The Effect of DSF/Cu (II) on the Activity of the Proteasome System
DSF also exerts anticancer efficacy by the inhibiting of the ubiquitin proteasome system (UPS). The UPS is crucial for the balance of protein metabolism and the normal function of cells [77]. Studies indicate that the proliferation of cancer cells is altered by proteasome inhibition [78]. The 26S proteasome consists of a catalytic 20S core and a 19S regulator, which biodegrades ubiquitinated proteins [79,80]. The active sulfhydryl groups in DSF chelate biological metals such as copper, which subsequently inhibit the 26S proteasome [81]. Importantly, the inhibition of the UPS by DSF/Cu (II), specifically occurs in breast cancer and prostate cancer cells [82] but not in normal cells [81,82]. Recently, a new mechanism of the DDC/Cu (II) complex CuET inhibiting the UPS has been reported to be associated with the proteins p97 and NPL4 [34]. NPL4 contains a Zn finger domain with two zinc fingers, and bivalent metal ions, such as copper, can bind to Zn fingers and cause the aggregation of NPL4 [83]. Furthermore, VCP/p97 interacts with the aggregated NPL4, causing an impairment of the p97-NPL4-UFD1 pathway [34]. All these mechanism consequently block substrate biodegradation, and induce cancer cell death CuETs have been reported to have greater antitumor efficacy than DSF [58,84], as CuET binds NLP4 with a higher affinity than DSF and induces NLP4 aggregation [34]. In addition, DSFalone is a proteasome inhibitor, which means it inhibits the activity of proteasomes, cellular structures responsible for protein degradation, interestingly, DSFalso converts carcinogenic cadmium to a proteasome inhibitor that possesses pro-apoptotic activity in human cancer cells [85]. NF-κB activity has been reported to be associated with the inhibitory activity of DSF on the proteasome [86]. DSF decreases NF-κB activity by blocking proteasome activity [87]. This occurs through the proteasomal cleavage of the protein inhibitor-κB (IκB) [88], which releases the heterodimer p50/p65 from the inhibitory complex, allowing for the translocation of NF-kB to the nucleus, where the regulation of the transcription of certain genes, notably those that mediate inflammation and cell survival happens [87,89]. In vitro, 10 μM of DSF/Cu (II) completely inhibited the chymotrypsin (CT)-like proteasomal activity in glioma stem cells from patients with multiple glioblastoma multiforme [90].
2.4. The Effect on Transcription Factors
DSF form mixed sulfides with sulfhydryl-containing transcription factors (TFs) and prevent the proliferation of melanoma cells [35,91]. NF-kB is a typical TF that mediates the development and progression of cancers [92]. Due to the cysteines in the DNA binding region of NF-kB, DSF affects cancer cells by binding in the DNA binding region of NF-kB and blocking its pro-cancer effects [35,93,94]. The presence of metal ions, such as Cu (II) and Zn (II), increases the formation of mixed sulfides [95]. NF-kB induces the expression of antiapoptotic genes, as indicated by the aberrant activation of NF-kB in many human malignancies [92]. Thus, the inhibition of NF-kB via DSF could increase cancer cell apoptosis [96]. DSF/Cu (II) is efficacious in selectively eradicating leukemia stem cells by simultaneously activating the apoptosis-related cJun N-terminal kinase (JNK) [96].
2.5. The Immunomodulatory Effects on the Tumor Microenvironment (TME)
The tumor microenvironment is a promising target for cancer therapy [97]. M2 tumor-associated macrophages (TAMs) are an important tumor-promoting component in the TME [98]. In vitro, Cu/DSF inhibits M2 TAM recruitment and to reprogram M2 TAMs by regulating the expression of certain chemokines and cytokines [99]. FROUNT (also be known as NUP85), a cytoplasmic protein, interacts with the chemokine receptors CCR2 and CCR5 in macrophages, facilitating the recruitment of TAMs [100]. Furthermore, FROUNT activates the PI3K-Rac-lamellipodium cascade, promoting cancer proliferation [100]. DSF has been reported to inhibit the interaction of FROUNT with CCR2 and CCR5, which decreases tumor associated macrophage (M2) accumulation in the TME, thereby decreasing tumor-promoting properties of tumor associated macrophage [100]. The co-delivery of the compound honokiol and a DSF/Cu (II) complex reprograms M2 TAMs to anti-tumor M1 macrophages and regulates mTOR [41]. In addition, DSF/Cu (II) and CuET induce immunogenic cell death (ICD), as indicated by a significant increase in the expression of damage-associated molecular pattern molecules, such as calreticulin, ATP, and high mobility group box 1 protein, in 4T1 breast cancer [101], colorectal cancer [102,103], and hepatocellular carcinoma [104,105]. The dying cancer cells become an in-situ vaccine that elicit significant immune memory by activating dendritic cells and the CD8 T cell immune response [104,105].
3. The Effect of DSF/Cu (II) on Cancer
In this section, we summarize the effects of DSF/Cu (II) on cancer-associated activities such as unlimited cancer proliferation, the self-renewal activity of cancer stem cells, cancer angiogenesis, and drug resistance (Figure 3).
3.1. DSF/Cu (II) on the Inhibition of Cancer Proliferation
DSF/Cu (II) induces cell death in different cancer cell lines via different mechanisms. In human breast cancer cells, DSF/Cu (II) causes cancer cell apoptosis via increasing Bcl-2 Associated X-protein (Bax, a pro-apoptotic protein) [50]. DSF, at a concentration of 25–50 ng/mL, produces a 4–6-fold increase in apoptosis, and co-incubation with the ROS inhibitory compound N-acetyl-cysteine (NAC) reverses DSF-induced apoptosis, suggesting that DSF-induced apoptosis is associated with an increase in ROS levels [60]. DSF induces the disruption of the mitochondrial membrane potential and cause apoptosis in human melanoma cell lines [60]. Xi et al. reported that DSF/Cu (II) produced significant cytotoxicity and caspase-dependent apoptosis in NSCLC cells [106]. Additionally, DSF produced autophagy-dependent apoptosis [103]. DSF/Cu (II) induced the apoptosis of erbB2-positive breast cancer cells by inhibiting AKT, cyclin D1, and NFκB signaling [107]. In malignant pleural mesothelioma (MPM) cells, DSF/Cu (II) produced apoptosis by activating the proapoptotic stress-activated protein kinases (SAPKs) p38 and JNK1/2, caspase-3. Furthermore, DSF/Cu (II) increased the expression of the apoptosis transducer, cell division cycle, and apoptosis regulator 1 (CARP-1/CCAR1) and sulfatase 1 (SULF1) [108]. The activation of NF-κB mediates cancer proliferation [109] and the DSF/Cu (II) inhibits the activity of NF-κB, thus inhibiting hepatocellular carcinoma (HCC) growth [110].
3.2. DSF/Cu (II) Efficacy in Cancer Stem Cells (CSCs)
CSCs have been reported to mediates cancer angiogenesis and drug resistance [111], so we firstly discuss the functions of DSF/Cu (II) on CSCs, then, in the following two paragraphs, we will discuss the roles of DSF/Cu (II) on angiogenesis and drug resistance. Because of promotions of CSCs on activities including the activation of ABC transporters, such as P-gp [112], and the increase in DNA repair mechanisms [113], CSCs are resistant to conventional anticancer drugs [37]. Furthermore, hypoxia also induces resistance of CSCs to chemotherapy. Numerous studies indicate that the presence of CSCs in patients correlates with poor prognosis [37]. The roles of DSF/Cu (II) on CSCs can be attributed to its activity on the ALDH1 enzyme. The ALDH1 protein family (ALDH1A1, ALDH1A2, and ALDH1A3) enhance the self-renewal, survival, and proliferation of CSCs [114]. ALDH+ CSC phenotypes have a high tumorigenic capacity [115,116]. DSF/Cu (II) significantly decreases MDA-MB-231 breast cancer cell proliferation by decreasing the ALDH+ CSC population [117]. In hepatocellular carcinoma, DSF decreases CSCs by inhibiting the p38 mitogen-activated protein kinase (MAPK) pathway [118]. DSF also inhibits CSCs in ovarian, pancreatic, pulmonary, and hematological cancers [90,119,120].
3.3. DSF/Cu (II) Effects on the Inhibition of Cancer Angiogenesis
Vascular endothelial growth factor (VEGF) is a critical mediator of angiogenesis in cancer cells, and high VEGF levels are positively correlated with poor prognosis [121]. 4HNE, a lipid peroxidation product [122], is involved in angiogenesis [123,124]; and the catabolism of 4HNE is dependent on the cellular levels of glutathione-S-transferases, alcohol dehydrogenases, and ALDHs [125]. The inhibition of ALDH2 by DSF/Cu (II) significantly decreases angiogenesis by inhibiting the hypoxia-inducible factor-1α (HIF-1α)/VEGF signaling cascade [126]. The inhibition of SOD-1 by DSF/Cu (II) induces endothelial cell growth arrest and apoptosis and, thus, exhibits anti-angiogenesis efficacy [127]. DSF/Cu (II) also inhibits tumor angiogenesis by inhibiting the activity of matrix metalloproteinases [128,129]. Copper increases the anti-angiogenic efficacy of DSF via the EGFR/Src/VEGF pathway in gliomas [130]. CSCs were shown to modulate angiogenesis via CSC-secreted VEGF [131]. Moreover, CSCs overexpress CXCR4, whose SDF-1/CXCL12 ligand induces VEGF production via activation of the P13K/AKT signaling pathway [132]. Other CSC-associated factors such as SDF-1/CXCL12 also play roles in the formation of the new blood vessels [133,134]. Thus, the inhibition of DSF/Cu (II) in CSCs decrease angiogenesis.
3.4. DSF/Cu (II) Reverses Drug Resistance
DSF/Cu (II) overcomes drug resistance via targeting the proteasome, epithelial–mesenchymal transition (EMT), P-gp, CSC activity [135,136,137]. By targeting the proteasome, DSF significantly increases the sensitivity of TMZ-resistant brain tumor-initiating cell (BTIC) variants (BT73R and BT206R) to temozolomide (TMZ) [138]. Numerous studies have shown that EMT plays a role in mediating the resistance of cancer cells to certain anticancer drugs, such as paclitaxel in prostate (DU145-TXR) and lung cancer (A549-TXR) [139,140,141]. By downregulating associated proteins such as Vimentin, DSF/Cu (II) inhibits the EMT, which consequently overcomes the paclitaxel resistance of prostate and lung cancer [141]. In addition, DSF/Cu (II) decreases the effects of EMT in breast cancer cells via the regulation of protein kinase (ERK)/NF-κB/Snail pathway [142]. Cancer cells expressing high levels of P-gp exhibit resistance to conventional chemotherapy drugs like doxorubicin and paclitaxel, a phenomenon referred to as multidrug resistance (MDR) [143,144]. However, the metabolite and active anti-cancer compound CuET is not a substrate of P-gp, and thus it is still retained inside of drug resistant cancer cells and increase the likelihood of the drug-resistant cancer cells death [141]. DSF/Cu (II) produce efficacy in osimertinib-resistant NSCLC cells by activating macrophage-mediated innate immunity [40]. It was discovered that the high levels of ABC protein provide the protective mechanism for CSCs to chemotherapeutics [145]. The inhibitory effects of DSF/Cu (II) on the CSCs benefit the overcoming of drug resistance [39]. Another important finding is that Cu(DDC)2 NP is also does not inhibit P-gp activity or expression, thus avoiding the side effects associated with P-gp inhibitors [141].
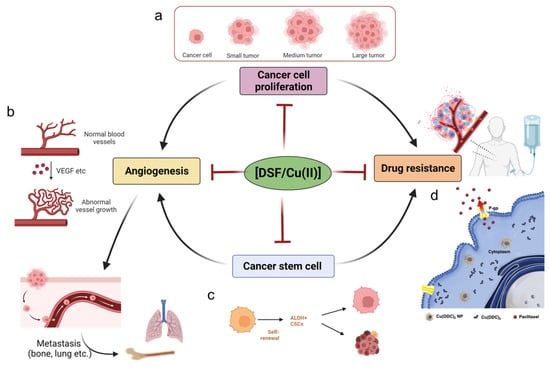
Figure 3.
Cancer cells have unlimited proliferative capacity, and DSF/Cu (II) has been shown anti-proliferation effects towards cancer cells. (a) DSF/Cu (II) inhibits cancer cell proliferation, preventing the transformation of small cancer lesions to large tumors. Created with BioRender.com accessed on 8 May 2023 (b). Angiogenesis is an essential step for cancer metastasis; the VEGF in the cancer microenvironments contributes the massive and abnormal vessels in cancer lesions, and DSF/Cu (II) inhibits the angiogenesis behavior and prevents cancer metastasis to lung and bone, etc., sites. Created with BioRender.com. accessed on 8 May 2023 (c) Cancer stem cells aggravate the angiogenesis and drug resistance of cancer; DSF/Cu (II) inhibits cancer stem cells and thus shown potency in anti-angiogenesis and anti-drug resistance. Created with BioRender.com accessed on 8 May 2023 (d). Drug resistance is a typical phenomenon during the treatment of cancer; novel copper diethyldithiocarbamate nanoparticles can effectively overcome drug-resistant cancers, owing to being non-binding to P-gp and being maintained in the cancer cells. Copyright 2023, Elsevier [141].
4. DSF-Based Therapies for the Treatment of Cancer
Although data from in vitro studies suggested that DSF could be an efficacious anticancer treatment, clinical trials with oral DSF plus Cu (II) in cancer patients have been equivocal [146,147]. The underlying reasons for the poor clinical results include: (1) the instability of DSF in the gastrointestinal environment; (2) the rapid biodegradation of DSF via first-pass metabolism; and (3) low final Cu (II) concentration at the tumor sites [148]. The effective delivery of DSF and Cu (II) to target sites is crucial for maximizing the anticancer efficacy of DSF/Cu (II) and overcoming limitations such as poor solubility, stability, and bioavailability. Recent progress in nanotechnology has facilitated the targeted delivery of DSF, and various types of drug delivery systems based on different nanoparticles have been developed. For instance, polymeric nanoparticles, nanogels, polymer–drug conjugates, liposomes, and dendrimers have been explored as effective carriers for DSF. For instance, DSF-loaded vitamin E-TPGS-modified PEGylated nanostructured lipid carriers have gained significant attention due to their biodegradable and biocompatible properties [149]. Nanogels are composed of nanosized particles that can entrap and release drugs in response to different stimuli, providing a promising strategy for the targeted delivery of DSF [150]. The use of these nanoparticle-based formulations can increase the accumulation of DSF at the target site, thereby reducing the toxic effects on healthy tissues and improving the therapeutic index. Overall, nanotechnology-based strategies have shown promising results in enhancing the anticancer efficacy of DSF and can potentially overcome the limitations associated with conventional DSF-based therapies. Figure 4 explains and summarizes this with some reported examples. Representative examples of the above delivery system are elaborated in the following paragraphs, and additional important investigations are listed in Table 2.
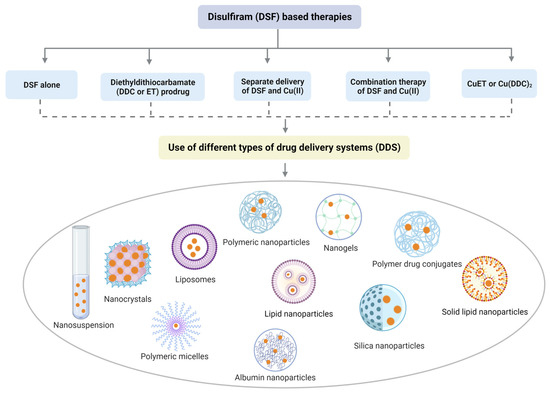
Figure 4.
Divergent nanotechnology and chemical modulation-based formulations to enhance DSF anticancer effects. To sum up, DSF-based nanomedicine includes DSF alone, DDC prodrug delivery system, delivery system for Cu (II) and DSF/Cu (II), and drug delivery system for active component-CuET.

Table 2.
Drug delivery systems of combined DSF/Cu, DSF alone, DDC prodrug, and Cu alone.
4.1. DSF Drug Delivery Systems and DDC Prodrug
To facilitate the use of DSF in breast cancer, Fasehee et al. designed novel poly(lactide-co-glycolide) (PLGA) NPs loaded with DSF, where DSF was released in a sustained manner [187]. In this study, the effect of 0.01 mg/mL DSF-PLGA NPs were evaluated in breast MCF-7 cancer cells, compared to free disulfiram, DSF-PLGA NPs showed more excellent anti-proliferation effects [187]. Cell-penetrating peptides (CPPs) are widely used for the increase in cargo’s cellular uptake [188]. To address non-specific internalization in normal cells, pH-sensitive lipid cell-penetrating peptide nanocapsules (DSF-S-LNCs) were sythesized. With the protective shielding materials (PEG-PGA) modification, the transactivator of transcription (TAT) peptides and drug were preferentially exposed in the acidic tumor microenvironment and exerted anti-HepG 2(Cu-enriched cancer cells) effects at DSF (3 μM) (Figure 5a) [160]. The higher concentrations of ROS (up to 100 μM) in tumors benefit the application of ROS-activatable prodrug. A prodrug of disulfiram (DDC) called DQ has been synthesized [101]. Though DQ will cause cell death with the activation the ROS basal level on cancer cells is still not sufficient for the activation of prodrug. Thus, extra ROS triggered by other therapies is needed [189]. One approach to achieving this is by utilizing copper sulfide (CuS), a photosensitizer of photodynamic therapy (PDT) and photothermal therapy (PTT) and can generate the needed ROS [189]. Hence, we designed a DQ micelle and, meanwhile, used the CuS as the cooper source to generate the final product, Cu (DDC)2 for breast cancer inhibition; in this work, the DQ generated massive DDC with the fuel of ROS induced by the photodynamic effects with CuS. In addition, other products’ quinone methide (QM), released by DQ, consume GSH and, thus, further increase ROS [101,167], The Fenton-like reaction of Cu (II) also contributes ROS. This positive feedback causes the anti-tumor effects of ROS and further increases the release of DQ [101,167], with the additive effects. An excellent in vitro anti-cancer ability was achieved in doses of DQ at 2 μM (Figure 5b). It has been reported that cancer cells overexpress the enzyme γ-glutamyl transferase (GGT) in cancer cells [190]. Recently, a GGT-sensitive DDC prodrug was developed; after being specifically activated by GGT overexpressed by cancer cells, the metabolite of DSF, dithiocarbamate, selectively eliminates GGT-expressing cancer cells [168]. The in vitro anti-tumor efficacy of prodrug is very distinct, ranging from 800 nM in prostate 22 Rv1 cancer lines to over 15 µM in normal prostate PWR-1E cells. Cellular GGT activity was the reason for the obvious difference [168].
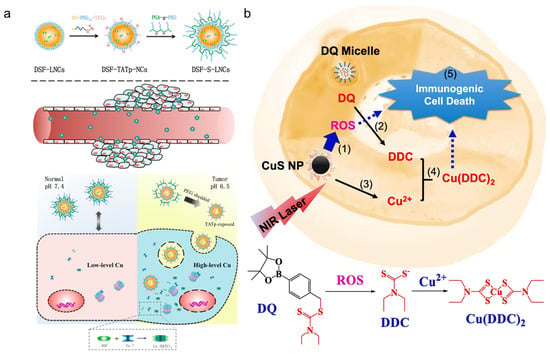
Figure 5.
Typical examples of the DSF delivery system and DDC prodrug: (a) DSF-loaded pH-triggered PEG-shedding TAT peptide-modified lipid nano capsules [160]. Copyright 2015, American Chemical Society. (b) Near-infrared light triggered activation of pro-drug combination cancer therapy and induction of immunogenic cell death, (1) NIR laser + CuS NP treatment increases intracellular ROS. (2) ROS converts DQ prodrug to DDC. (3) CuS NP release Cu (II). (4) DDC and Cu (II) form Cu(DDC)2 active anticancer complex. (5) Cu(DDC)2 chemotherapy and ROS induce immunogenic cell death in cancer cells [101]. Copyright 2015 © 2021 Elsevier B.V.
4.2. Drug Delivery Systems for Cu (II) and DSF/Cu (II)
In clinical trials, DSF is provided orally, but Cu (II) is critical for the efficacy of DSF [191]. It is critical that Cu (II) has a high affinity for its carrier to avoid an insufficient amount of Cu (II) in tumor sites. Liposomes can deliver the hydrophilic and hydrophobic drug [151]. In one study, copper oleate was synthesized and formulated as liposomes. This copper oleate liposome (Cu (OI)2-L) was obtained via alcohol injection and achieved 85% drug loading efficiency. Cu (OI)2-L exhibited a slow-release profile, indicated by >70% retained drug over 8 h incubation. Prolonged circulation time was confirmed in pharmacokinetic studies. Cu (OI)2-L plus DSF nanoparticles showed excellent antitumor efficacy in bearing a hepatoma mice xenograft model [180].
A new technique for breast cancer therapy has been developed using Cu (II)DSF in situ chelation. Cu (II)and DSF are encapsulated separately into PEGylated hollow mesoporous silica nanoparticles (HMSNs). The DSF@PEG/Cu-HMSNs nano system enhances DSF-based chemotherapy without systemic toxicity. It utilizes a tumor-specific pathway involving two mechanisms: pathway I to II and pathway I to III. In pathway I to II, DSF acts as a chelating agent, selectively binding with Cu (II) ions within the tumor site. In pathway I to III, Cu+ ions initiate a Fenton-like reaction with hydrogen peroxide (H2O2) in the tumor microenvironment, generating reactive oxygen species (ROS) for localized cytotoxicity. This combined approach achieves enhanced antitumor efficacy by targeting cancer cells while minimizing harm to healthy tissues (Figure 6a) [174]. Albumin is an FDA-approved material, and BSA was found to be a good carrier for DSF/Cu (II). The regorafenib (Rego) and DSF/Cu co-encapsulation showed potential in reversing multidrug resistance of HCT8/ADR cells. In this work, it was shown that paclitaxel (PTX) showed a slight cytotoxic effect even with 2 µM. However, the potent inhibitory effects were observed in combination therapy (DSF/Cu and Rego), with an IC50 of DSF/Cu about 0.47 µM. Furthermore, modifying the ligand so that it binds to the cancer cell receptor, MD206, decreased the IC50 of DSF/Cu (II) to0.3 µM. In addition, the CD206 was also highly expressed in the tumor-promoting macrophages, so the targeted nanoparticle interacted with 2 sites to produce their anticancer efficacy (“two birds one stone”). (Figure 6b).
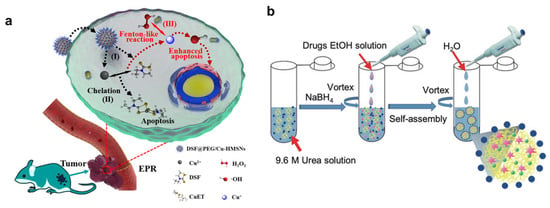
Figure 6.
(a) Schematic illustration: The DSF@PEG/Cu-HMSNs nano system triggers tumor-specific DTC-Cu (II)chelation (pathway I to II) and Cu+-initiated Fenton-like reaction (pathway I to III). This enhances the antitumor efficacy of DSF-based chemotherapy without systemic toxicity. Copyright 2019, American Chemical Society [174]. (b) Schematic illustration of albumin-based dual-targeting biomimetic delivery of Rego and DSF/Cu for cancer therapy. Copyright 2021, Wiley-VCH [192].
4.3. Drug Delivery Systems for CuET
Since CuET was shown to be a pharmacologically active molecule of DSF/Cu (II) [34], research was initiated to deliver CuET to target sites. Recently, a nanoliposomal (LP) CuET formulation was synthesized using ethanol injection as a facile, one-step method that is suitable for large-scale manufacturing [193]. IC50 of LP-CuET on YUMM 1.7 mouse melanoma cells was 91.39 ± 4.98 nM [193]. In 2017, a CuET-loaded liposome was synthesized, and. In 2017, a CuET-loaded liposome was synthesized, the intravenous administration of this formulation produced a 45% decrease of tumor burden in MV-4-11 human biphenotypic B myelomonocytic leukemia xenograft mice model; [182,186]. Although the above-mentioned strategies could be used for CuET delivery, the efficiency of drug loading is not optimal. To overcome the drug loading problem, a stabilized metal ion ligand complex (SMILE) technology was proposed by Chen et al., in which a high CuET drug loading can be achieved [25]. Compared with the traditional thin-film dispersion method, this approach increased drug concentration by over 200-fold. Additionally, the IC50 of Cu (DDC)2 NPs on paclitaxel-resistant prostate cancer cells (DU145-TXR) was only around 100 nM [25]. Subsequently, a scale-up and commercialization 3D-printed microfluidic device was developed to scale the production of CuET [185]. This device could achieve a flow rate of 2 mL/min. Since it is a continuous production device, it can produce around 5000 mg of SMILE nanoparticle drug formulation per day [185] (Figure 7). Delivery strategies, such as the SMILE method, could also be used for the delivery of other metal-based chelators.
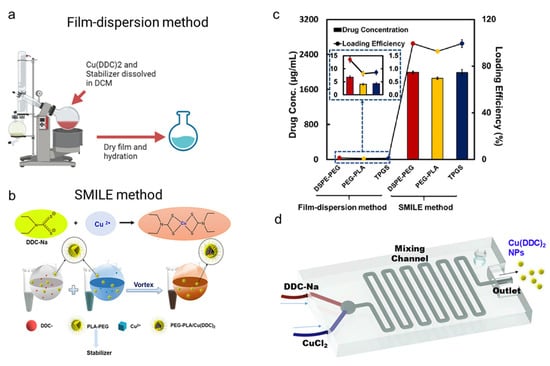
Figure 7.
Schematic comparison of (a) film-dispersion method (Created with BioRender.com) accessed on 8 May 2023 vs. (b) stabilized metal ion ligand complex (SMILE) technology [25]. Copyright © 2018 American Chemical Society. (c) Drug loading efficiency of film-dispersion method and stabilized metal ion ligand complex (SMILE) technology [25]. Copyright © 2018 American Chemical Society. (d) The scale of SMILE technology using a 3D-printed microfluidic device [32]. Copyright © 2019 Elsevier Ltd.
4.4. The Advantages and Disadvantages of Different Drug Delivery Systems
As we have discussed, additional Cu (II) supplementation is needed for DSF alone and DDC prodrug delivery systems. The disadvantages or problems associated with DSF and DDC prodrugs are: (1) the potential mismatch of the pharmacokinetics of DSF or prodrug and Cu (II) in systematic application; (2) difficulties in estimating accurate amounts of additional copper for the DSF and DDC prodrug chelation process in vivo. The major issues for the separate delivery of DSF and Cu are the pharmacokinetic and pharmacodynamic profiles because of the non-simultaneous delivery of two components to the tumor sites. The co-delivery of DSF/Cu (II) is a better strategy due to the synchronous delivery of DSF and Cu (II). However, the loading of drugs requires further improvement. Direct CuET delivery may represent a novel approach that decreases the dose needed and increases the therapeutic index, whereas the unknown effects of the direct use of CuET still need to be addressed (Figure 8).
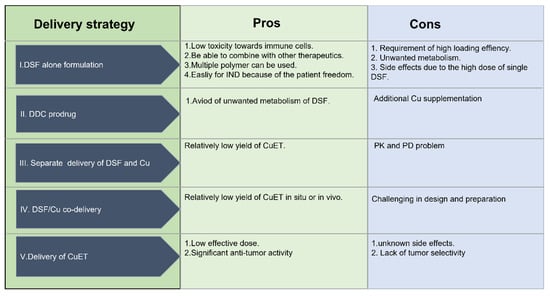
Figure 8.
The pros and cons of the different delivery strategies.
5. Summary and Future Directions
Drug repurposing is a relatively cost-effective and promising strategy for the development of anti-cancer drugs. The in vitro, and preclinical evaluation of investigations of DSF-based delivery systems on cancer applications have dramatically increased in recent years. This review introduces the current targets and formulations of Cu and DSF and its metabolites as anticancer treatments. The effects of DSF/Cu (II) by affecting ROS production, cellular enzymes (e.g., ALDH), transcription factors (e.g., NF-κB), and proteasome activity (e.g., P97/NPL4) reveal the powerful anticancer activity of DSF/Cu (II). In addition, DSF/Cu (II) immunomodulates innate immune response and adaptive immune response; it can be used as a reagent to 1) reprogram macrophages and 2) as a therapeutic adjuvant for immunotherapy.
Although the existing strategies have significantly contributed to the progress of DSF for cancer, some issues still need to be addressed. It is first necessary to determine the precise dose for in vivo studies as high doses of DSF cause side effects such as neuropathic pain. Furthermore, the side effects of CuET remain unknown due to the paucity of studies conducted with CuEt.
In addition, from the delivery perspective, the optimization of physicochemical properties of NPs is critical for decreasing the incidence of side effects and achieving targeted tumor treatment. The “3R” delivery principle is significant for formulation design and optimization. Briefly, 3R defined as effective delivery of multiple drugs to the right place, with the right dose, at the right time. For the right place, the targeting modification or in situ formation of CuET could be helpful in minimizing the amount of off-target drug release. For the right dose, the major concern is the accurate estimation of in vivo usage, but because of the heterogenous properties of different cancer types, the exact amount of drug is difficult to be determined. To ensure accurate dose delivery bya sperate delivery system, analytical methods for determining Cu (II) concentrations at the local regions would be useful. A device that releases a drug at the right time in response to a remote trigger could allow for on-demand drug release.
Although it has been more than half a century since the anti-cancer efficacy of DSF has been discovered, the clinical needs associated with DSF-based treatments have not yet been met. Technological advances, such as organ-on-a-chip or patient-derived organoids may provide an alternative to in vivo or animal studies using in vitro organoids. Finally new tumor-targeting modifications, such as antibodies, nanobodies, aptamers, peptides could increase the delivery of drug to tumors, thus increasing the efficacy and decreasing the incidence and severity of adverse effect.
Cancer chemotherapy-based (pre)clinical trials face significant challenges, including the need to address the reproducibility of research findings. In vitro assays often produce promising results, but in vivo results are frequently disappointing due to the variability of DDC levels in individuals and the heterogeneity of cancer cell lines. Advances in technology, such as the use of organs on a chip, can help to address these challenges by increasing the accuracy of in vitro biological systems. Additionally, there is a need for more rigorous standards and guidelines for conducting (pre)clinical research. This will help ensure that (pre)clinical research can be translated into effective therapies and interventions that benefit patients while minimizing potential risks and ethical concerns.
Author Contributions
Conceptualization: X.K., C.-H.H., C.R.A.J., A.K.T., R.J.B. and P.C.; Funding acquisition: R.J.B. and P.C.; Software: X.K. and S.J.; Supervision: C.R.A.J., A.K.T., R.J.B. and P.C.; Visualization: X.K., S.J., M.A., C.-H.H., R.A., J.S., C.R.A.J., A.K.T., R.J.B. and P.C.; Writing—original draft: X.K., S.J., M.A., C.-H.H., R.A., J.S., C.R.A.J., A.K.T., R.J.B. and P.C.; Writing—review and editing: X.K., C.-H.H., R.A., J.S., C.R.A.J., A.K.T., R.J.B. and P.C. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Institutes of Health (NIH) MIRA R35GM133795 (P. Chen).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Zhang, Z.; Zhou, L.; Xie, N.; Nice, E.C.; Zhang, T.; Cui, Y.; Huang, C. Overcoming cancer therapeutic bottleneck by drug repurposing. Signal Transduct. Target. Ther. 2020, 5, 113. [Google Scholar] [CrossRef] [PubMed]
- Chong, C.R.; Sullivan, D.J. New uses for old drugs. Nature 2007, 448, 645–646. [Google Scholar] [CrossRef] [PubMed]
- Corsello, S.M.; Nagari, R.T.; Spangler, R.D.; Rossen, J.; Kocak, M.; Bryan, J.G.; Humeidi, R.; Peck, D.; Wu, X.; Tang, A.A. Discovering the anticancer potential of non-oncology drugs by systematic viability profiling. Nat. Cancer 2020, 1, 235–248. [Google Scholar] [CrossRef]
- Ma, C.; Peng, Y.; Li, H.; Chen, W. Organ-on-a-chip: A new paradigm for drug development. Trends Pharmacol. Sci. 2021, 42, 119–133. [Google Scholar] [CrossRef]
- Lowndes, S.A.; Harris, A.L. The role of copper in tumour angiogenesis. J. Mammary Gland. Biol. Neoplasia 2005, 10, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Antoniades, V.; Sioga, A.; Dietrich, E.M.; Meditskou, S.; Ekonomou, L.; Antoniades, K. Is copper chelation an effective anti-angiogenic strategy for cancer treatment? Med. Hypotheses 2013, 81, 1159–1163. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhou, M.; Liu, Y.; Si, Z. Cope with copper: From copper linked mechanisms to copper-based clinical cancer therapies. Cancer Lett. 2023, 561, 216157. [Google Scholar] [CrossRef] [PubMed]
- da Silva, D.A.; De Luca, A.; Squitti, R.; Rongioletti, M.; Rossi, L.; Machado, C.M.L.; Cerchiaro, G. Copper in tumors and the use of copper-based compounds in cancer treatment. J. Inorg. Biochem. 2022, 226, 111634. [Google Scholar] [CrossRef]
- Tsvetkov, P.; Coy, S.; Petrova, B.; Dreishpoon, M.; Verma, A.; Abdusamad, M.; Rossen, J.; Joesch-Cohen, L.; Humeidi, R.; Spangler, R.D. Copper induces cell death by targeting lipoylated TCA cycle proteins. Science 2022, 375, 1254–1261. [Google Scholar] [CrossRef]
- Ghosh, P.; Vidal, C.; Dey, S.; Zhang, L. Mitochondria targeting as an effective strategy for cancer therapy. Int. J. Mol. Sci. 2020, 21, 3363. [Google Scholar] [CrossRef]
- Oliveri, V. Selective targeting of cancer cells by copper ionophores: An overview. Front. Mol. Biosci. 2022, 9, 841814. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Yang, Y.; Gao, Y.; He, J. Cuproptosis: Mechanisms and links with cancers. Mol. Cancer 2023, 22, 46. [Google Scholar] [CrossRef] [PubMed]
- Johansson, B. A review of the pharmacokinetics and pharmacodynamics of disulfiram and its metabolites. Acta Psychiatr. Scand. 1992, 86, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Mittal, M.; Bhagwati, S.; Siddiqi, M.I.; Chattopadhyay, N. A critical assessment of the potential of pharmacological modulation of aldehyde dehydrogenases to treat the diseases of bone loss. Eur. J. Pharmacol. 2020, 886, 173541. [Google Scholar] [CrossRef]
- Swift, R.; Davidson, D. Alcohol hangover: Mechanisms and mediators. Alcohol Health Res. World 1998, 22, 54–60. [Google Scholar]
- Yoshida, A.; Hsu, L.C.; Davé, V. Retinal oxidation activity and biological role of human cytosolic aldehyde dehydrogenase. Enzyme 1992, 46, 239–244. [Google Scholar] [CrossRef]
- Lewison, E.F. Spontaneous regression of breast cancer. Natl. Cancer Inst. Monogr. 1976, 44, 23–26. [Google Scholar]
- López-Lázaro, M. Dual role of hydrogen peroxide in cancer: Possible relevance to cancer chemoprevention and therapy. Cancer Lett. 2007, 252, 1–8. [Google Scholar] [CrossRef]
- Schmitt, S.M.; Frezza, M.; Dou, Q.P. New applications of old metal-binding drugs in the treatment of human cancer. Front. Biosci. 2012, 4, 375. [Google Scholar] [CrossRef]
- Wang, W.; McLeod, H.L.; Cassidy, J. Disulfiram-mediated inhibition of NF-κB activity enhances cytotoxicity of 5-fluorouracil in human colorectal cancer cell lines. Int. J. Cancer 2003, 104, 504–511. [Google Scholar] [CrossRef]
- Xu, B.; Shi, P.; Fombon, I.S.; Zhang, Y.; Huang, F.; Wang, W.; Zhou, S. Disulfiram/copper complex activated JNK/c-jun pathway and sensitized cytotoxicity of doxorubicin in doxorubicin resistant leukemia HL60 cells. Blood Cells Mol. Dis. 2011, 47, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Yip, N.C.; Fombon, I.S.; Liu, P.; Brown, S.; Kannappan, V.; Armesilla, A.L.; Xu, B.; Cassidy, J.; Darling, J.L.; Wang, W. Disulfiram modulated ROS–MAPK and NFκB pathways and targeted breast cancer cells with cancer stem cell-like properties. Br. J. Cancer 2011, 104, 1564–1574. [Google Scholar] [CrossRef] [PubMed]
- Roudi, R.; Korourian, A.; Shariftabrizi, A.; Madjd, Z. Differential expression of cancer stem cell markers ALDH1 and CD133 in various lung cancer subtypes. Cancer Investig. 2015, 33, 294–302. [Google Scholar] [CrossRef]
- Koh, H.K.; Seo, S.Y.; Kim, J.H.; Kim, H.J.; Chie, E.K.; Kim, S.-K.; Kim, I.H. Disulfiram, a re-positioned aldehyde dehydrogenase inhibitor, enhances radiosensitivity of human glioblastoma cells in vitro. Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2019, 51, 696–705. [Google Scholar] [CrossRef]
- Chen, W.; Yang, W.; Chen, P.; Huang, Y.; Li, F. Disulfiram copper nanoparticles prepared with a stabilized metal ion ligand complex method for treating drug-resistant prostate cancers. ACS Appl. Mater. Interfaces 2018, 10, 41118–41128. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.-n.; Wang, L.-H.; Li, Y.; Fu, S.-Y.; Xue, X.; Jia, L.-N.; Yuan, X.-Z.; Wang, Y.-T.; Tang, X.; Yang, J.-Y. Targeting ALDH2 with disulfiram/copper reverses the resistance of cancer cells to microtubule inhibitors. Exp. Cell Res. 2018, 362, 72–82. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wang, L.; Cui, W.; Yuan, X.; Lin, L.; Cao, Q.; Wang, N.; Li, Y.; Guo, W.; Zhang, X. Targeting ALDH1A1 by disulfiram/copper complex inhibits non-small cell lung cancer recurrence driven by ALDH-positive cancer stem cells. Oncotarget 2016, 7, 58516–58530. [Google Scholar] [CrossRef] [PubMed]
- Denoyer, D.; Pearson, H.B.; Clatworthy, S.A.S.; Smith, Z.M.; Francis, P.S.; Llanos, R.M.; Volitakis, I.; Phillips, W.A.; Meggyesy, P.M.; Masaldan, S. Copper as a target for prostate cancer therapeutics: Copper-ionophore pharmacology and altering systemic copper distribution. Oncotarget 2016, 7, 37064–37080. [Google Scholar] [CrossRef]
- Orlov, A.P.; Orlova, M.A.; Trofimova, T.P.; Kalmykov, S.N.; Kuznetsov, D.A. The role of zinc and its compounds in leukemia. JBIC J. Biol. Inorg. Chem. 2018, 23, 347–362. [Google Scholar] [CrossRef]
- Gupte, A.; Mumper, R.J. Elevated copper and oxidative stress in cancer cells as a target for cancer treatment. Cancer Treat. Rev. 2009, 35, 32–46. [Google Scholar] [CrossRef]
- Chen, D.; Dou, Q.P. New uses for old copper-binding drugs: Converting the pro-angiogenic copper to a specific cancer cell death inducer. Expert Opin. Ther. Targets 2008, 12, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Jiang, J.; Chen, W.; Yang, W.; Chen, L.; Chen, P.; Shen, J.; Qian, S.; Zhou, T.; Wu, L. Biomimetic metal-organic nanoparticles prepared with a 3D-printed microfluidic device as a novel formulation for disulfiram-based therapy against breast cancer. Appl. Mater. Today 2020, 18, 100492. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Li, X.; Ren, Y.; Zhang, X. Disulfiram: A novel repurposed drug for cancer therapy. Cancer Chemother. Pharmacol. 2021, 87, 159–172. [Google Scholar] [CrossRef]
- Skrott, Z.; Mistrik, M.; Andersen, K.K.; Friis, S.; Majera, D.; Gursky, J.; Ozdian, T.; Bartkova, J.; Turi, Z.; Moudry, P. Alcohol-abuse drug disulfiram targets cancer via p97 segregase adaptor NPL4. Nature 2017, 552, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Brar, S.S.; Grigg, C.; Wilson, K.S.; Holder, W.D., Jr.; Dreau, D.; Austin, C.; Foster, M.; Ghio, A.J.; Whorton, A.R.; Stowell, G.W. Disulfiram inhibits activating transcription factor/cyclic AMP-responsive element binding protein and human melanoma growth in a metal-dependent manner in vitro, in mice and in a patient with metastatic disease. Mol. Cancer Ther. 2004, 3, 1049–1060. [Google Scholar] [CrossRef] [PubMed]
- Wickström, M.; Danielsson, K.; Rickardson, L.; Gullbo, J.; Nygren, P.; Isaksson, A.; Larsson, R.; Lövborg, H. Pharmacological profiling of disulfiram using human tumor cell lines and human tumor cells from patients. Biochem. Pharmacol. 2007, 73, 25–33. [Google Scholar] [CrossRef]
- Li, H.; Wang, J.; Wu, C.; Wang, L.; Chen, Z.-S.; Cui, W. The combination of disulfiram and copper for cancer treatment. Drug Discov. Today 2020, 25, 1099–1108. [Google Scholar] [CrossRef]
- Ren, X.; Li, Y.; Zhou, Y.; Hu, W.; Yang, C.; Jing, Q.; Zhou, C.; Wang, X.; Hu, J.; Wang, L.; et al. Overcoming the compensatory elevation of NRF2 renders hepatocellular carcinoma cells more vulnerable to disulfiram/copper-induced ferroptosis. Redox Biol. 2021, 46, 102122. [Google Scholar] [CrossRef] [PubMed]
- Guo, F.; Yang, Z.; Kulbe, H.; Albers, A.E.; Sehouli, J.; Kaufmann, A.M. Inhibitory effect on ovarian cancer ALDH+ stem-like cells by Disulfiram and Copper treatment through ALDH and ROS modulation. Biomed. Pharmacother. 2019, 118, 109371. [Google Scholar] [CrossRef]
- Zhao, P.; Zhang, J.; Wu, A.; Zhang, M.; Zhao, Y.; Tang, Y.; Wang, B.; Chen, T.; Li, F.; Zhao, Q. Biomimetic codelivery overcomes osimertinib-resistant NSCLC and brain metastasis via macrophage-mediated innate immunity. J. Control. Release 2021, 329, 1249–1261. [Google Scholar] [CrossRef]
- Zheng, Z.; Zhang, J.; Jiang, J.; He, Y.; Zhang, W.; Mo, X.; Kang, X.; Xu, Q.; Wang, B.; Huang, Y. Remodeling tumor immune microenvironment (TIME) for glioma therapy using multi-targeting liposomal codelivery. J. Immunother. Cancer 2020, 8, e000207. [Google Scholar] [CrossRef] [PubMed]
- Morrison, B.W.; Doudican, N.A.; Patel, K.R.; Orlow, S.J. Disulfiram induces copper-dependent stimulation of reactive oxygen species and activation of the extrinsic apoptotic pathway in melanoma. Melanoma Res. 2010, 20, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Brown, S.; Goktug, T.; Channathodiyil, P.; Kannappan, V.; Hugnot, J.P.; Guichet, P.O.; Bian, X.; Armesilla, A.L.; Darling, J.L. Cytotoxic effect of disulfiram/copper on human glioblastoma cell lines and ALDH-positive cancer-stem-like cells. Br. J. Cancer 2012, 107, 1488–1497. [Google Scholar] [CrossRef] [PubMed]
- Nie, D.; Chen, C.; Li, Y.; Zeng, C. Disulfiram, an aldehyde dehydrogenase inhibitor, works as a potent drug against sepsis and cancer via NETosis, pyroptosis, apoptosis, ferroptosis, and cuproptosis. Blood Sci. 2022, 4, 152–154. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Chaudhary, R.; Cohen, A.L.; Fink, K.; Goldlust, S.; Boockvar, J.; Chinnaiyan, P.; Wan, L.; Marcus, S.; Campian, J.L. A multicenter phase II study of temozolomide plus disulfiram and copper for recurrent temozolomide-resistant glioblastoma. J. Neuro-Oncol. 2019, 142, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Campian, J.L.; Gujar, A.D.; Tsien, C.; Ansstas, G.; Tran, D.D.; DeWees, T.A.; Lockhart, A.C.; Kim, A.H. Final results of a phase I dose-escalation, dose-expansion study of adding disulfiram with or without copper to adjuvant temozolomide for newly diagnosed glioblastoma. J. Neuro-Oncol. 2018, 138, 105–111. [Google Scholar] [CrossRef]
- Nechushtan, H.; Hamamreh, Y.; Nidal, S.; Gotfried, M.; Baron, A.; Shalev, Y.I.; Nisman, B.; Peretz, T.; Peylan-Ramu, N. A phase IIb trial assessing the addition of disulfiram to chemotherapy for the treatment of metastatic non-small cell lung cancer. Oncologist 2015, 20, 366–367. [Google Scholar] [CrossRef]
- Wang, L.; Yu, Y.; Zhou, C.; Wan, R.; Li, Y. Anticancer effects of disulfiram: A systematic review of in vitro, animal, and human studies. Syst. Rev. 2022, 11, 109. [Google Scholar] [CrossRef]
- Liou, G.-Y.; Storz, P. Reactive oxygen species in cancer. Free. Radic. Res. 2010, 44, 479–496. [Google Scholar] [CrossRef]
- Oberley, T.D. Oxidative damage and cancer. Am. J. Pathol. 2002, 160, 403–408. [Google Scholar] [CrossRef]
- Trachootham, D.; Alexandre, J.; Huang, P. Targeting cancer cells by ROS-mediated mechanisms: A radical therapeutic approach? Nat. Rev. Drug Discov. 2009, 8, 579–591. [Google Scholar] [CrossRef]
- Roy, D.; Sheng, G.Y.; Herve, S.; Carvalho, E.; Mahanty, A.; Yuan, S.; Sun, L. Interplay between cancer cell cycle and metabolism: Challenges, targets and therapeutic opportunities. Biomed. Pharmacother. 2017, 89, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Yi, J. Cancer cell killing via ROS: To increase or decrease, that is the question. Cancer Biol. Ther. 2008, 7, 1875–1884. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Guo, F.; Albers, A.E.; Sehouli, J.; Kaufmann, A.M. Disulfiram modulates ROS accumulation and overcomes synergistically cisplatin resistance in breast cancer cell lines. Biomed. Pharmacother. 2019, 113, 108727. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chen, F.; Chen, J.; Chan, S.; He, Y.; Liu, W.; Zhang, G. Disulfiram/copper induces antitumor activity against both nasopharyngeal cancer cells and cancer-associated fibroblasts through ROS/MAPK and ferroptosis pathways. Cancers 2020, 12, 138. [Google Scholar] [CrossRef] [PubMed]
- Allensworth, J.L.; Evans, M.K.; Bertucci, F.; Aldrich, A.J.; Festa, R.A.; Finetti, P.; Ueno, N.T.; Safi, R.; McDonnell, D.P.; Thiele, D.J. Disulfiram (DSF) acts as a copper ionophore to induce copper-dependent oxidative stress and mediate anti-tumor efficacy in inflammatory breast cancer. Mol. Oncol. 2015, 9, 1155–1168. [Google Scholar] [CrossRef]
- Calderon-Aparicio, A.; Strasberg-Rieber, M.; Rieber, M. Disulfiram anti-cancer efficacy without copper overload is enhanced by extracellular H2O2 generation: Antagonism by tetrathiomolybdate. Oncotarget 2015, 6, 29771–29781. [Google Scholar] [CrossRef]
- Cen, D.; Brayton, D.; Shahandeh, B.; Meyskens, F.L.; Farmer, P.J. Disulfiram facilitates intracellular Cu uptake and induces apoptosis in human melanoma cells. J. Med. Chem. 2004, 47, 6914–6920. [Google Scholar] [CrossRef]
- Fruehauf, J.P.; Trapp, V. Reactive oxygen species: An Achilles’ heel of melanoma? Expert Rev. Anticancer. Ther. 2008, 8, 1751–1757. [Google Scholar] [CrossRef]
- Cen, D.; Gonzalez, R.I.; Buckmeier, J.A.; Kahlon, R.S.; Tohidian, N.B.; Meyskens, F.L., Jr. Disulfiram induces apoptosis in human melanoma cells: A redox-related process. Mol. Cancer Ther. 2002, 1, 197–204. [Google Scholar]
- Leon, G.; MacDonagh, L.; Finn, S.P.; Cuffe, S.; Barr, M.P. Cancer stem cells in drug resistant lung cancer: Targeting cell surface markers and signaling pathways. Pharmacol. Ther. 2016, 158, 71–90. [Google Scholar] [CrossRef] [PubMed]
- Moreb, J.S.; Ucar, D.; Han, S.; Amory, J.K.; Goldstein, A.S.; Ostmark, B.; Chang, L.-J. The enzymatic activity of human aldehyde dehydrogenases 1A2 and 2 (ALDH1A2 and ALDH2) is detected by Aldefluor, inhibited by diethylaminobenzaldehyde and has significant effects on cell proliferation and drug resistance. Chem.-Biol. Interact. 2012, 195, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Jin, N.; Zhu, X.; Cheng, F.; Zhang, L. Disulfiram/copper targets stem cell-like ALDH+ population of multiple myeloma by inhibition of ALDH1A1 and Hedgehog pathway. J. Cell. Biochem. 2018, 119, 6882–6893. [Google Scholar] [CrossRef] [PubMed]
- Yan, Z.; Xu, L.; Zhang, J.; Lu, Q.; Luo, S.; Xu, L. Aldehyde dehydrogenase 1A1 stabilizes transcription factor Gli2 and enhances the activity of Hedgehog signaling in hepatocellular cancer. Biochem. Biophys. Res. Commun. 2016, 471, 466–473. [Google Scholar] [CrossRef]
- Delude, C. Tumorigenesis: Testing ground for cancer stem cells. Nature 2011, 480, S43–S45. [Google Scholar] [CrossRef]
- Sharma, V.; Verma, V.; Lal, N.; Yadav, S.K.; Sarkar, S.; Mandalapu, D.; Porwal, K.; Rawat, T.; Maikhuri, J.P.; Rajender, S. Disulfiram and its novel derivative sensitize prostate cancer cells to the growth regulatory mechanisms of the cell by re-expressing the epigenetically repressed tumor suppressor—Estrogen receptor β. Mol. Carcinog. 2016, 55, 1843–1857. [Google Scholar] [CrossRef]
- Tesson, M.; Anselmi, G.; Bell, C.; Mairs, R. Cell cycle specific radiosensitisation by the disulfiram and copper complex. Oncotarget 2017, 8, 65900–65916. [Google Scholar] [CrossRef]
- Pegg, A.E. Repair of O6-alkylguanine by alkyltransferases. Mutat. Res./Rev. Mutat. Res. 2000, 462, 83–100. [Google Scholar] [CrossRef]
- Mishina, Y.; Duguid, E.M.; He, C. Direct reversal of DNA alkylation damage. Chem. Rev. 2006, 106, 215–232. [Google Scholar] [CrossRef]
- Gerson, S.L. Clinical relevance of MGMT in the treatment of cancer. J. Clin. Oncol. 2002, 20, 2388–2399. [Google Scholar] [CrossRef]
- Paranjpe, A.; Zhang, R.; Ali-Osman, F.; Bobustuc, G.C.; Srivenugopal, K.S. Disulfiram is a direct and potent inhibitor of human O 6-methylguanine-DNA methyltransferase (MGMT) in brain tumor cells and mouse brain and markedly increases the alkylating DNA damage. Carcinogenesis 2014, 35, 692–702. [Google Scholar] [CrossRef] [PubMed]
- Locasale, J.W.; Grassian, A.R.; Melman, T.; Lyssiotis, C.A.; Mattaini, K.R.; Bass, A.J.; Heffron, G.; Metallo, C.M.; Muranen, T.; Sharfi, H. Phosphoglycerate dehydrogenase diverts glycolytic flux and contributes to oncogenesis. Nat. Genet. 2011, 43, 869–874. [Google Scholar] [CrossRef]
- Spillier, Q.; Vertommen, D.; Ravez, S.; Marteau, R.; Thémans, Q.; Corbet, C.; Feron, O.; Wouters, J.; Frédérick, R. Anti-alcohol abuse drug disulfiram inhibits human PHGDH via disruption of its active tetrameric form through a specific cysteine oxidation. Sci. Rep. 2019, 9, 4737. [Google Scholar] [CrossRef] [PubMed]
- Turner, N.; Tutt, A.; Ashworth, A. Targeting the DNA repair defect of BRCA tumours. Curr. Opin. Pharmacol. 2005, 5, 388–393. [Google Scholar] [CrossRef]
- Tutt, A.; Ashworth, A. The relationship between the roles of BRCA genes in DNA repair and cancer predisposition. Trends Mol. Med. 2002, 8, 571–576. [Google Scholar] [CrossRef]
- Majera, D.; Skrott, Z.; Chroma, K.; Merchut-Maya, J.M.; Mistrik, M.; Bartek, J. Targeting the NPL4 Adaptor of p97/VCP Segregase by Disulfiram as an Emerging Cancer Vulnerability Evokes Replication Stress and DNA Damage while Silencing the ATR Pathway. Cells 2020, 9, 469. [Google Scholar] [CrossRef] [PubMed]
- Lecker, S.H.; Goldberg, A.L.; Mitch, W.E. Protein degradation by the ubiquitin–proteasome pathway in normal and disease states. J. Am. Soc. Nephrol. 2006, 17, 1807–1819. [Google Scholar] [CrossRef]
- Wang, F.; Zhai, S.; Liu, X.; Li, L.; Wu, S.; Dou, Q.P.; Yan, B. A novel dithiocarbamate analogue with potentially decreased ALDH inhibition has copper-dependent proteasome-inhibitory and apoptosis-inducing activity in human breast cancer cells. Cancer Lett. 2011, 300, 87–95. [Google Scholar] [CrossRef]
- Kleiger, G.; Mayor, T. Perilous journey: A tour of the ubiquitin–proteasome system. Trends Cell Biol. 2014, 24, 352–359. [Google Scholar] [CrossRef]
- Wang, H.; Yang, Q.; Dou, Q.P.; Yang, H. Discovery of natural proteasome inhibitors as novel anticancer therapeutics: Current status and perspectives. Curr. Protein Pept. Sci. 2018, 19, 358–367. [Google Scholar] [CrossRef]
- Chen, D.; Cui, Q.C.; Yang, H.; Dou, Q.P. Disulfiram, a clinically used anti-alcoholism drug and copper-binding agent, induces apoptotic cell death in breast cancer cultures and xenografts via inhibition of the proteasome activity. Cancer Res. 2006, 66, 10425–10433. [Google Scholar] [CrossRef]
- Chen, D.; Peng, F.; Cui, Q.C.; Daniel, K.G.; Orlu, S.; Liu, J.; Dou, Q.P. Inhibition of prostate cancer cellular proteasome activity by a pyrrolidine dithiocarbamate-copper complex is associated with suppression of proliferation and induction of apoptosis. Front. Biosci. 2005, 10, 2932–2939. [Google Scholar] [CrossRef] [PubMed]
- Meraz-Torres, F.; Plöger, S.; Garbe, C.; Niessner, H.; Sinnberg, T. Disulfiram as a therapeutic agent for metastatic malignant melanoma—Old myth or new logos? Cancers 2020, 12, 3538. [Google Scholar] [CrossRef] [PubMed]
- Lewis, D.J.; Deshmukh, P.; Tedstone, A.A.; Tuna, F.; O’Brien, P. On the interaction of copper (II) with disulfiram. Chem. Commun. 2014, 50, 13334–13337. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Yang, H.; Chen, D.; Cui, C.; Dou, Q.P. Disulfiram promotes the conversion of carcinogenic cadmium to a proteasome inhibitor with pro-apoptotic activity in human cancer cells. Toxicol. Appl. Pharmacol. 2008, 229, 206–214. [Google Scholar] [CrossRef]
- Pham, C.G.; Bubici, C.; Zazzeroni, F.; Knabb, J.R.; Papa, S.; Kuntzen, C.; Franzoso, G. Upregulation of Twist-1 by NF-κB blocks cytotoxicity induced by chemotherapeutic drugs. Mol. Cell. Biol. 2007, 27, 3920–3935. [Google Scholar] [CrossRef]
- Cvek, B.; Dvorak, Z. The value of proteasome inhibition in cancer: Can the old drug, disulfiram, have a bright new future as a novel proteasome inhibitor? Drug Discov. Today 2008, 13, 716–722. [Google Scholar] [CrossRef]
- Henkel, T.; Machleidt, T.; Alkalay, I.; Krönke, M.; Ben-Neriah, Y.; Baeuerle, P.A. Rapid proteolysis of I κ B-α is necessary for activation of transcription factor NF-κ B. Nature 1993, 365, 182–185. [Google Scholar] [CrossRef]
- Annunziata, C.M.; Davis, R.E.; Demchenko, Y.; Bellamy, W.; Gabrea, A.; Zhan, F.; Lenz, G.; Hanamura, I.; Wright, G.; Xiao, W. Frequent engagement of the classical and alternative NF-κB pathways by diverse genetic abnormalities in multiple myeloma. Cancer Cell 2007, 12, 115–130. [Google Scholar] [CrossRef]
- Hothi, P.; Martins, T.J.; Chen, L.; Deleyrolle, L.; Yoon, J.-G.; Reynolds, B.; Foltz, G. High-throughput chemical screens identify disulfiram as an inhibitor of human glioblastoma stem cells. Oncotarget 2012, 3, 1124–1136. [Google Scholar] [CrossRef]
- Brar, S.S.; Kennedy, T.P.; Whorton, A.R.; Sturrock, A.B.; Huecksteadt, T.P.; Ghio, A.J.; Hoidal, J.R. Reactive oxygen species from NAD (P) H: Quinone oxidoreductase constitutively activate NF-κB in malignant melanoma cells. Am. J. Physiol.-Cell Physiol. 2001, 280, C659–C676. [Google Scholar] [CrossRef] [PubMed]
- Dolcet, X.; Llobet, D.; Pallares, J.; Matias-Guiu, X. NF-kB in development and progression of human cancer. Virchows Arch. 2005, 446, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Meyskens, F.L., Jr.; Buckmeier, J.A.; McNulty, S.E.; Tohidian, N.B. Activation of nuclear factor-κB in human metastatic melanoma cells and the effect of oxidative stress. Clin. Cancer Res. 1999, 5, 1197–1202. [Google Scholar]
- Askgaard, G.; Friis, S.; Hallas, J.; Thygesen, L.C.; Pottegård, A. Use of disulfiram and risk of cancer. Eur. J. Cancer Prev. 2014, 23, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Pan, Q.; Kleer, C.G.; van Golen, K.L.; Irani, J.; Bottema, K.M.; Bias, C.; De Carvalho, M.; Mesri, E.A.; Robins, D.M.; Dick, R.D. Copper deficiency induced by tetrathiomolybdate suppresses tumor growth and angiogenesis. Cancer Res. 2002, 62, 4854–4859. [Google Scholar] [PubMed]
- Xu, B.; Wang, S.; Li, R.; Chen, K.; He, L.; Deng, M.; Kannappan, V.; Zha, J.; Dong, H.; Wang, W. Disulfiram/copper selectively eradicates AML leukemia stem cells in vitro and in vivo by simultaneous induction of ROS-JNK and inhibition of NF-κB and Nrf2. Cell Death Dis. 2017, 8, e2797. [Google Scholar] [CrossRef] [PubMed]
- Quail, D.F.; Joyce, J.A. Microenvironmental regulation of tumor progression and metastasis. Nat. Med. 2013, 19, 1423–1437. [Google Scholar] [CrossRef]
- Ostuni, R.; Kratochvill, F.; Murray, P.J.; Natoli, G. Macrophages and cancer: From mechanisms to therapeutic implications. Trends Immunol. 2015, 36, 229–239. [Google Scholar] [CrossRef]
- Yang, M.; Li, J.; Gu, P.; Fan, X. The application of nanoparticles in cancer immunotherapy: Targeting tumor microenvironment. Bioact. Mater. 2021, 6, 1973–1987. [Google Scholar] [CrossRef]
- Terashima, Y.; Toda, E.; Itakura, M.; Otsuji, M.; Yoshinaga, S.; Okumura, K.; Shand, F.H.W.; Komohara, Y.; Takeda, M.; Kokubo, K.; et al. Targeting FROUNT with disulfiram suppresses macrophage accumulation and its tumor-promoting properties. Nat. Commun. 2020, 11, 609. [Google Scholar] [CrossRef]
- Kang, X.; Cai, Y.; Wang, Q.; Wang, C.; Chen, W.; Yang, W.; Suryawanshi, A.; Zhou, G.; Chen, P.; Li, F. Near-infrared light triggered activation of pro-drug combination cancer therapy and induction of immunogenic cell death. Int. J. Pharm. 2021, 607, 120972. [Google Scholar] [CrossRef]
- You, S.-Y.; Rui, W.; Chen, S.-T.; Chen, H.-C.; Liu, X.-W.; Huang, J.; Chen, H.-Y. Process of immunogenic cell death caused by disulfiram as the anti-colorectal cancer candidate. Biochem. Biophys. Res. Commun. 2019, 513, 891–897. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Hu, P.; Ding, S.-Y.; Sun, T.; Liu, L.; Han, S.; DeLeo, A.B.; Sadagopan, A.; Guo, W.; Wang, X. Induction of autophagy-dependent apoptosis in cancer cells through activation of ER stress: An uncovered anti-cancer mechanism by anti-alcoholism drug disulfiram. Am. J. Cancer Res. 2019, 9, 1266–1281. [Google Scholar] [PubMed]
- Guo, Y.; Wang, S.-Z.; Zhang, X.; Jia, H.-R.; Zhu, Y.-X.; Zhang, X.; Gao, G.; Jiang, Y.-W.; Li, C.; Chen, X.; et al. In situ generation of micrometer-sized tumor cell-derived vesicles as autologous cancer vaccines for boosting systemic immune responses. Nat. Commun. 2022, 13, 6534. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Huang, H.; Pan, C.; Mei, Z.; Yin, S.; Zhou, L.; Zheng, S. Disulfiram/Copper Induces Immunogenic Cell Death and Enhances CD47 Blockade in Hepatocellular Carcinoma. Cancers 2022, 14, 4715. [Google Scholar] [CrossRef]
- Wu, X.; Xue, X.; Wang, L.; Wang, W.; Han, J.; Sun, X.; Zhang, H.; Liu, Y.; Che, X.; Yang, J. Suppressing autophagy enhances disulfiram/copper-induced apoptosis in non-small cell lung cancer. Eur. J. Pharmacol. 2018, 827, 1–12. [Google Scholar] [CrossRef]
- Yang, Y.; Deng, Q.; Feng, X.; Sun, J. Use of the disulfiram/copper complex for breast cancer chemoprevention in MMTV-erbB2 transgenic mice. Mol. Med. Rep. 2015, 12, 746–752. [Google Scholar] [CrossRef]
- Cheriyan, V.T.; Wang, Y.; Muthu, M.; Jamal, S.; Chen, D.; Yang, H.; Polin, L.A.; Tarca, A.L.; Pass, H.I.; Dou, Q.P. Disulfiram suppresses growth of the malignant pleural mesothelioma cells in part by inducing apoptosis. PLoS ONE 2014, 9, e93711. [Google Scholar] [CrossRef]
- Lin, Y.; Bai, L.; Chen, W.; Xu, S. The NF-κB activation pathways, emerging molecular targets for cancer prevention and therapy. Expert Opin. Ther. Targets 2010, 14, 45–55. [Google Scholar] [CrossRef]
- Li, Y.; Wang, L.H.; Zhang, H.T.; Wang, Y.T.; Liu, S.; Zhou, W.L.; Yuan, X.Z.; Li, T.Y.; Wu, C.F.; Yang, J.Y. Disulfiram combined with copper inhibits metastasis and epithelial–mesenchymal transition in hepatocellular carcinoma through the NF-κB and TGF-β pathways. J. Cell. Mol. Med. 2018, 22, 439–451. [Google Scholar] [CrossRef]
- Bao, B.; Wang, Z.; Ali, S.; Ahmad, A.; Azmi, A.S.; Sarkar, S.H.; Banerjee, S.; Kong, D.; Li, Y.; Thakur, S. Metformin inhibits cell proliferation, migration and invasion by attenuating CSC function mediated by deregulating miRNAs in pancreatic cancer cells. Cancer Prev. Res. 2012, 5, 355–364. [Google Scholar] [CrossRef] [PubMed]
- Bleau, A.-M.; Hambardzumyan, D.; Ozawa, T.; Fomchenko, E.I.; Huse, J.T.; Brennan, C.W.; Holland, E.C. PTEN/PI3K/Akt Pathway Regulates the Side Population Phenotype and ABCG2 Activity in Glioma Tumor Stem-like Cells. Cell Stem Cell 2009, 4, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Venere, M.; Hamerlik, P.; Wu, Q.; Rasmussen, R.D.; Song, L.A.; Vasanji, A.; Tenley, N.; Flavahan, W.A.; Hjelmeland, A.B.; Bartek, J.; et al. Therapeutic targeting of constitutive PARP activation compromises stem cell phenotype and survival of glioblastoma-initiating cells. Cell Death Differ. 2014, 21, 258–269. [Google Scholar] [CrossRef] [PubMed]
- Petersen, E.N. The pharmacology and toxicology of disulfiram and its metabolites. Acta Psychiatr. Scand. 1992, 86, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Ginestier, C.; Hur, M.H.; Charafe-Jauffret, E.; Monville, F.; Dutcher, J.; Brown, M.; Jacquemier, J.; Viens, P.; Kleer, C.G.; Liu, S. ALDH1 is a marker of normal and malignant human mammary stem cells and a predictor of poor clinical outcome. Cell Stem Cell 2007, 1, 555–567. [Google Scholar] [CrossRef] [PubMed]
- Moreb, J.S. Aldehyde dehydrogenase as a marker for stem cells. Curr. Stem Cell Res. Ther. 2008, 3, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; Xiao, J.; Yin, Q.; Zhang, Z.; Yu, H.; Mao, S.; Li, Y. Multi-targeted inhibition of tumor growth and lung metastasis by redox-sensitive shell crosslinked micelles loading disulfiram. Nanotechnology 2014, 25, 125102. [Google Scholar] [CrossRef]
- Chiba, T.; Suzuki, E.; Yuki, K.; Zen, Y.; Oshima, M.; Miyagi, S.; Saraya, A.; Koide, S.; Motoyama, T.; Ogasawara, S. Disulfiram eradicates tumor-initiating hepatocellular carcinoma cells in ROS-p38 MAPK pathway-dependent and-independent manners. PLoS ONE 2014, 9, e84807. [Google Scholar] [CrossRef]
- Triscott, J.; Lee, C.; Hu, K.; Fotovati, A.; Berns, R.; Pambid, M.; Luk, M.; Kast, R.E.; Kong, E.; Toyota, E. Disulfiram, a drug widely used to control alcoholism, suppresses self-renewal of glioblastoma and overrides resistance to temozolomide. Oncotarget 2012, 3, 1112–1123. [Google Scholar] [CrossRef]
- Mimeault, M.; Batra, S.K. Recent advances in the development of novel anti-cancer drugs targeting cancer stem/progenitor cells. Drug Dev. Res. 2008, 69, 415–430. [Google Scholar] [CrossRef]
- Manders, P.; Beex, L.; Tjan-Heijnen, V.C.G.; Geurts-Moespot, J.; Van Tienoven, T.; Foekens, J.A.; Sweep, C.G.J. The prognostic value of vascular endothelial growth factor in 574 node-negative breast cancer patients who did not receive adjuvant systemic therapy. Br. J. Cancer 2002, 87, 772–778. [Google Scholar] [CrossRef] [PubMed]
- Schreier, S.M.; Muellner, M.K.; Steinkellner, H.; Hermann, M.; Esterbauer, H.; Exner, M.; Gmeiner, B.M.K.; Kapiotis, S.; Laggner, H. Hydrogen sulfide scavenges the cytotoxic lipid oxidation product 4-HNE. Neurotox. Res. 2010, 17, 249–256. [Google Scholar] [CrossRef]
- Ayala, A.; Muñoz, M.F.; Argüelles, S. Lipid peroxidation: Production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxidative Med. Cell. Longev. 2014, 2014, 360438. [Google Scholar] [CrossRef] [PubMed]
- Chapple, S.J.; Cheng, X.; Mann, G.E. Effects of 4-hydroxynonenal on vascular endothelial and smooth muscle cell redox signaling and function in health and disease. Redox Biol. 2013, 1, 319–331. [Google Scholar] [CrossRef] [PubMed]
- Camaré, C.; Vanucci-Bacqué, C.; Augé, N.; Pucelle, M.; Bernis, C.; Swiader, A.; Baltas, M.; Bedos-Belval, F.; Salvayre, R.; Nègre-Salvayre, A. 4-Hydroxynonenal contributes to angiogenesis through a redox-dependent sphingolipid pathway: Prevention by hydralazine derivatives. Oxidative Med. Cell. Longev. 2017, 2017, 9172741. [Google Scholar] [CrossRef]
- Liu, X.; Sun, X.; Liao, H.; Dong, Z.; Zhao, J.; Zhu, H.; Wang, P.; Shen, L.; Xu, L.; Ma, X. Mitochondrial aldehyde dehydrogenase 2 regulates revascularization in chronic ischemia: Potential impact on the development of coronary collateral circulation. Arterioscler. Thromb. Vasc. Biol. 2015, 35, 2196–2206. [Google Scholar] [CrossRef] [PubMed]
- Marikovsky, M.; Nevo, N.; Vadai, E.; Harris-Cerruti, C. Cu/Zn superoxide dismutase plays a role in angiogenesis. Int. J. Cancer 2002, 97, 34–41. [Google Scholar] [CrossRef]
- Shian, S.-G.; Kao, Y.-R.; Wu, F.Y.-H.; Wu, C.-W. Inhibition of invasion and angiogenesis by zinc-chelating agent disulfiram. Mol. Pharmacol. 2003, 64, 1076–1084. [Google Scholar] [CrossRef]
- Kast, R.E.; Halatsch, M.-E. Matrix Metalloproteinase-2 and-9 in glioblastoma: A trio of old drugs—Captopril, disulfiram and nelfinavir—Are inhibitors with potential as adjunctive treatments in glioblastoma. Arch. Med. Res. 2012, 43, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Fu, S.-Y.; Wang, L.-H.; Wang, F.-Y.; Wang, N.-N.; Cao, Q.; Wang, Y.-T.; Yang, J.-Y.; Wu, C.-F. Copper improves the anti-angiogenic activity of disulfiram through the EGFR/Src/VEGF pathway in gliomas. Cancer Lett. 2015, 369, 86–96. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhou, Y.; Sun, X.; Zhou, J.; Yang, P. CXCL12 overexpression promotes the angiogenesis potential of periodontal ligament stem cells. Sci. Rep. 2017, 7, 10286. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Cao, Y.; Zhang, S.; Chen, Z.; Fan, L.; Shen, X.; Zhou, S.; Chen, D. Stem cell autocrine CXCL12/CXCR4 stimulates invasion and metastasis of esophageal cancer. Oncotarget 2017, 8, 36149–36160. [Google Scholar] [CrossRef]
- Ponti, D.; Costa, A.; Zaffaroni, N.; Pratesi, G.; Petrangolini, G.; Coradini, D.; Pilotti, S.; Pierotti, M.A.; Daidone, M.G. Isolation and in vitro propagation of tumorigenic breast cancer cells with stem/progenitor cell properties. Cancer Res. 2005, 65, 5506–5511. [Google Scholar] [CrossRef] [PubMed]
- Beckermann, B.M.; Kallifatidis, G.; Groth, A.; Frommhold, D.; Apel, A.; Mattern, J.; Salnikov, A.V.; Moldenhauer, G.; Wagner, W.; Diehlmann, A. VEGF expression by mesenchymal stem cells contributes to angiogenesis in pancreatic carcinoma. Br. J. Cancer 2008, 99, 622–631. [Google Scholar] [CrossRef]
- O’Brien, A.; Barber, J.E.B.; Reid, S.; Niknejad, N.; Dimitroulakos, J. Enhancement of cisplatin cytotoxicity by disulfiram involves activating transcription factor 3. Anticancer. Res. 2012, 32, 2679–2688. [Google Scholar] [PubMed]
- Olmo, F.; Urbanová, K.; Rosales, M.J.; Martín-Escolano, R.; Sánchez-Moreno, M.; Marín, C. An in vitro iron superoxide dismutase inhibitor decreases the parasitemia levels of Trypanosoma cruzi in BALB/c mouse model during acute phase. Int. J. Parasitol. Drugs Drug Resist. 2015, 5, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Schmidtova, S.; Kalavska, K.; Gercakova, K.; Cierna, Z.; Miklikova, S.; Smolkova, B.; Buocikova, V.; Miskovska, V.; Durinikova, E.; Burikova, M. Disulfiram overcomes cisplatin resistance in human embryonal carcinoma cells. Cancers 2019, 11, 1224. [Google Scholar] [CrossRef]
- Lun, X.; Wells, J.C.; Grinshtein, N.; King, J.C.; Hao, X.; Dang, N.-H.; Wang, X.; Aman, A.; Uehling, D.; Datti, A. Disulfiram when Combined with Copper Enhances the Therapeutic Effects of Temozolomide for the Treatment of GlioblastomaDisulfiram/Copper Enhance Temozolomide Treatment for Glioblastoma. Clin. Cancer Res. 2016, 22, 3860–3875. [Google Scholar] [CrossRef]
- Thiery, J.P. Epithelial–mesenchymal transitions in development and pathologies. Curr. Opin. Cell Biol. 2003, 15, 740–746. [Google Scholar] [CrossRef]
- Thiery, J.P.; Acloque, H.; Huang, R.Y.J.; Nieto, M.A. Epithelial-mesenchymal transitions in development and disease. Cell 2009, 139, 871–890. [Google Scholar] [CrossRef]
- Kang, X.; Wang, J.; Huang, C.-H.; Wibowo, F.S.; Amin, R.; Chen, P.; Li, F. Diethyldithiocarbamate copper nanoparticle overcomes resistance in cancer therapy without inhibiting P-glycoprotein. Nanomed. Nanotechnol. Biol. Med. 2023, 47, 102620. [Google Scholar] [CrossRef] [PubMed]
- Han, D.; Wu, G.; Chang, C.; Zhu, F.; Xiao, Y.; Li, Q.; Zhang, T.; Zhang, L. Disulfiram inhibits TGF-β-induced epithelial-mesenchymal transition and stem-like features in breast cancer via ERK/NF-κB/Snail pathway. Oncotarget 2015, 6, 40907–40919. [Google Scholar] [CrossRef] [PubMed]
- Krasnovskaya, O.; Naumov, A.; Guk, D.; Gorelkin, P.; Erofeev, A.; Beloglazkina, E.; Majouga, A. Copper Coordination Compounds as Biologically Active Agents. Int. J. Mol. Sci. 2020, 21, 3965. [Google Scholar] [CrossRef] [PubMed]
- Kang, X.-j.; Wang, H.-y.; Peng, H.-g.; Chen, B.-f.; Zhang, W.-y.; Wu, A.-h.; Xu, Q.; Huang, Y.-z. Codelivery of dihydroartemisinin and doxorubicin in mannosylated liposomes for drug-resistant colon cancer therapy. Acta Pharmacol. Sin. 2017, 38, 885–896. [Google Scholar] [CrossRef]
- Alisi, A.; Cho, W.C.; Locatelli, F.; Fruci, D. Multidrug resistance and cancer stem cells in neuroblastoma and hepatoblastoma. Int. J. Mol. Sci. 2013, 14, 24706–24725. [Google Scholar] [CrossRef] [PubMed]
- Siddique, M.R. Improving Leukaemia Diagnosis and Management with Selected Ion Flow Tube Mass Spectrometry and Vibrational Spectroscopy Techniques. Ph.D. Thesis, Keele University, Newcastle, UK, 2017. [Google Scholar]
- Mafficini, A.; Scarpa, A. Genetics and Epigenetics of Gastroenteropancreatic Neuroendocrine Neoplasms. Endocr. Rev. 2019, 40, 506–536. [Google Scholar] [CrossRef]
- Farooq, M.A.; Aquib, M.; Khan, D.H.; Hussain, Z.; Ahsan, A.; Baig, M.M.F.A.; Wande, D.P.; Ahmad, M.M.; Ahsan, H.M.; Jiajie, J. Recent advances in the delivery of disulfiram: A critical analysis of promising approaches to improve its pharmacokinetic profile and anticancer efficacy. DARU J. Pharm. Sci. 2019, 27, 853–862. [Google Scholar] [CrossRef]
- Banerjee, P.; Geng, T.; Mahanty, A.; Li, T.; Zong, L.; Wang, B. Integrating the drug, disulfiram into the vitamin E-TPGS-modified PEGylated nanostructured lipid carriers to synergize its repurposing for anti-cancer therapy of solid tumors. Int. J. Pharm. 2019, 557, 374–389. [Google Scholar] [CrossRef]
- Zhong, Y.; Sun, R.; Geng, Y.; Zhou, Q.; Piao, Y.; Xie, T.; Zhou, R.; Shen, Y. N-Oxide polymer–cupric ion nanogels potentiate disulfiram for cancer therapy. Biomater. Sci. 2020, 8, 1726–1733. [Google Scholar] [CrossRef]
- Liu, X.; Chu, H.; Cui, N.; Wang, T.; Dong, S.; Cui, S.; Dai, Y.; Wang, D. In vitro and in vivo evaluation of biotin-mediated PEGylated nanostructured lipid as carrier of disulfiram coupled with copper ion. J. Drug Deliv. Sci. Technol. 2019, 51, 651–661. [Google Scholar] [CrossRef]
- Farooq, M.A.; Li, L.; Parveen, A.; Wang, B. Globular protein stabilized nanoparticles for delivery of disulfiram: Fabrication, characterization, in vitro toxicity, and cellular uptake. RSC Adv. 2020, 10, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Tao, X.; Gou, J.; Zhang, Q.; Tan, X.; Ren, T.; Yao, Q.; Tian, B.; Kou, L.; Zhang, L.; Tang, X. Synergistic breast tumor cell killing achieved by intracellular co-delivery of doxorubicin and disulfiram via core–shell–corona nanoparticles. Biomater. Sci. 2018, 6, 1869–1881. [Google Scholar] [CrossRef] [PubMed]
- Song, W.; Tang, Z.; Lei, T.; Wen, X.; Wang, G.; Zhang, D.; Deng, M.; Tang, X.; Chen, X. Stable loading and delivery of disulfiram with mPEG-PLGA/PCL mixed nanoparticles for tumor therapy. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 377–386. [Google Scholar] [CrossRef]
- Fasehee, H.; Zarrinrad, G.; Tavangar, S.M.; Ghaffari, S.H.; Faghihi, S. The inhibitory effect of disulfiram encapsulated PLGA NPs on tumor growth: Different administration routes. Mater. Sci. Eng. C 2016, 63, 587–595. [Google Scholar] [CrossRef] [PubMed]
- Fasehee, H.; Dinarvand, R.; Ghavamzadeh, A.; Esfandyari-Manesh, M.; Moradian, H.; Faghihi, S.; Ghaffari, S.H. Delivery of disulfiram into breast cancer cells using folate-receptor-targeted PLGA-PEG nanoparticles: In vitro and in vivo investigations. J. Nanobiotechnol. 2016, 14, 32. [Google Scholar] [CrossRef]
- Abu-Serie, M.M.; El-Fakharany, E.M. Efficiency of novel nanocombinations of bovine milk proteins (lactoperoxidase and lactoferrin) for combating different human cancer cell lines. Sci. Rep. 2017, 7, 16769. [Google Scholar] [CrossRef]
- Wang, Z.; Tan, J.; McConville, C.; Kannappan, V.; Tawari, P.E.; Brown, J.; Ding, J.; Armesilla, A.L.; Irache, J.M.; Mei, Q.-B. Poly lactic-co-glycolic acid controlled delivery of disulfiram to target liver cancer stem-like cells. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 641–657. [Google Scholar] [CrossRef]
- Hoda, M.; Pajaniradje, S.; Shakya, G.; Mohankumar, K.; Rajagopalan, R. Anti-proliferative and apoptosis-triggering potential of disulfiram and disulfiram-loaded polysorbate 80-stabilized PLGA nanoparticles on hepatocellular carcinoma Hep3B cell line. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 1641–1650. [Google Scholar] [CrossRef]
- Zhang, L.; Tian, B.; Li, Y.; Lei, T.; Meng, J.; Yang, L.; Zhang, Y.; Chen, F.; Zhang, H.; Xu, H. A copper-mediated disulfiram-loaded pH-triggered PEG-shedding TAT peptide-modified lipid nanocapsules for use in tumor therapy. ACS Appl. Mater. Interfaces 2015, 7, 25147–25161. [Google Scholar] [CrossRef]
- Zhuo, X.; Lei, T.; Miao, L.; Chu, W.; Li, X.; Luo, L.; Gou, J.; Zhang, Y.; Yin, T.; He, H.; et al. Disulfiram-loaded mixed nanoparticles with high drug-loading and plasma stability by reducing the core crystallinity for intravenous delivery. J. Colloid Interface Sci. 2018, 529, 34–43. [Google Scholar] [CrossRef]
- Mohammad, I.S.; Teng, C.; Chaurasiya, B.; Yin, L.; Wu, C.; He, W. Drug-delivering-drug approach-based codelivery of paclitaxel and disulfiram for treating multidrug-resistant cancer. Int. J. Pharm. 2019, 557, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Najlah, M.; Ahmed, Z.; Iqbal, M.; Wang, Z.; Tawari, P.; Wang, W.; McConville, C. Development and characterisation of disulfiram-loaded PLGA nanoparticles for the treatment of non-small cell lung cancer. Eur. J. Pharm. Biopharm. 2017, 112, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Aquib, M.; Zhang, H.; Raza, F.; Banerjee, P.; Bavi, R.; Kesse, S.; Boakye-Yiadom, K.O.; Filli, M.S.; Farooq, M.A.; Wang, B. Delivery of repurposed disulfiram by aminated mesoporous silica nanoparticles for anticancer therapy. J. Mol. Liq. 2022, 346, 117065. [Google Scholar] [CrossRef]
- Madala, H.R.; Punganuru, S.R.; Ali-Osman, F.; Zhang, R.; Srivenugopal, K.S. Brain-and brain tumor-penetrating disulfiram nanoparticles: Sequence of cytotoxic events and efficacy in human glioma cell lines and intracranial xenografts. Oncotarget 2018, 9, 3459–3482. [Google Scholar] [CrossRef] [PubMed]
- Cui, J.; Li, W.; Bu, W.; Liu, J.; Chen, X.; Li, X.; Liu, C.; Meng, L.; Chen, M.; Sun, H. Folic acid-modified disulfiram/Zn-IRMOF3 nanoparticles for oral cancer therapy by inhibiting ALDH1A1+ cancer stem cells. Biomater. Adv. 2022, 139, 213038. [Google Scholar] [CrossRef]
- Pan, Q.; Zhang, B.; Peng, X.; Wan, S.; Luo, K.; Gao, W.; Pu, Y.; He, B. A dithiocarbamate-based H2O2-responsive prodrug for combinational chemotherapy and oxidative stress amplification therapy. Chem. Commun. 2019, 55, 13896–13899. [Google Scholar] [CrossRef]
- Bakthavatsalam, S.; Sleeper, M.L.; Dharani, A.; George, D.J.; Zhang, T.; Franz, K.J. Leveraging γ-glutamyl transferase to direct cytotoxicity of copper dithiocarbamates against prostate cancer cells. Angew. Chem. Int. Ed. 2018, 57, 12780–12784. [Google Scholar] [CrossRef]
- He, H.; Markoutsa, E.; Li, J.; Xu, P. Repurposing disulfiram for cancer therapy via targeted nanotechnology through enhanced tumor mass penetration and disassembly. Acta Biomater. 2018, 68, 113–124. [Google Scholar] [CrossRef]
- Xu, N.; Yang, Y.-F.; Chen, L.; Lin, J. A ferritin–albumin–cu nanoparticle that efficaciously delivers copper (II) ions to a tumor and improves the therapeutic efficacy of disulfiram. ACS Omega 2020, 5, 10415–10422. [Google Scholar] [CrossRef]
- Chang, Y.; Wu, F.; Pandey, N.K.; Chudal, L.; Xing, M.; Zhang, X.; Nguyen, L.; Liu, X.; Liu, J.P.; Chen, W.; et al. Combination of Disulfiram and Copper-Cysteamine Nanoparticles for an Enhanced Antitumor Effect on Esophageal Cancer. ACS Appl. Bio Mater. 2020, 3, 7147–7157. [Google Scholar] [CrossRef]
- Chen, M.; Huang, Z.; Xia, M.; Ding, Y.; Shan, T.; Guan, Z.; Dai, X.; Xu, X.; Huang, Y.; Huang, M. Glutathione-responsive copper-disulfiram nanoparticles for enhanced tumor chemotherapy. J. Control. Release 2022, 341, 351–363. [Google Scholar] [CrossRef]
- Solak, K.; Mavi, A.; Yılmaz, B. Disulfiram-loaded functionalized magnetic nanoparticles combined with copper and sodium nitroprusside in breast cancer cells. Mater. Sci. Eng. C 2021, 119, 111452. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Yu, L.; Jiang, Q.; Huo, M.; Lin, H.; Wang, L.; Chen, Y.; Shi, J. Enhanced Tumor-Specific Disulfiram Chemotherapy by In Situ Cu (II)Chelation-Initiated Nontoxicity-to-Toxicity Transition. J. Am. Chem. Soc. 2019, 141, 11531–11539. [Google Scholar] [CrossRef]
- Meng, X.; Jia, K.; Sun, K.; Zhang, L.; Wang, Z. Smart responsive nanoplatform via in situ forming disulfiram-copper ion chelation complex for cancer combination chemotherapy. Chem. Eng. J. 2021, 415, 128947. [Google Scholar] [CrossRef]
- Zhao, P.; Yin, W.; Wu, A.; Tang, Y.; Wang, J.; Pan, Z.; Lin, T.; Zhang, M.; Chen, B.; Duan, Y.; et al. Dual-Targeting to Cancer Cells and M2 Macrophages via Biomimetic Delivery of Mannosylated Albumin Nanoparticles for Drug-Resistant Cancer Therapy. Adv. Funct. Mater. 2017, 27, 1700403. [Google Scholar] [CrossRef]
- Jiapaer, Z.; Zhang, L.; Ma, W.; Liu, H.; Li, C.; Huang, W.; Shao, S. Disulfiram-loaded hollow copper sulfide nanoparticles show anti-tumor effects in preclinical models of colorectal cancer. Biochem. Biophys. Res. Commun. 2022, 635, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Chao, Y.; Liu, B.; Xiao, Z.; Yang, Z.; Wu, Y.; Liu, Z. Disulfiram loaded calcium phosphate nanoparticles for enhanced cancer immunotherapy. Biomaterials 2022, 291, 121880. [Google Scholar] [CrossRef]
- Xu, R.; Zhang, K.; Liang, J.; Gao, F.; Li, J.; Guan, F. Hyaluronic acid/polyethyleneimine nanoparticles loaded with copper ion and disulfiram for esophageal cancer. Carbohydr. Polym. 2021, 261, 117846. [Google Scholar] [CrossRef]
- Zhou, L.; Yang, L.; Yang, C.; Liu, Y.; Chen, Q.; Pan, W.; Cai, Q.; Luo, L.; Liu, L.; Jiang, S. Membrane loaded copper oleate PEGylated liposome combined with disulfiram for improving synergistic antitumor effect in vivo. Pharm. Res. 2018, 35, 147. [Google Scholar] [CrossRef]
- Marengo, A.; Forciniti, S.; Dando, I.; Dalla Pozza, E.; Stella, B.; Tsapis, N.; Yagoubi, N.; Fanelli, G.; Fattal, E.; Heeschen, C. Pancreatic cancer stem cell proliferation is strongly inhibited by diethyldithiocarbamate-copper complex loaded into hyaluronic acid decorated liposomes. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2019, 1863, 61–72. [Google Scholar] [CrossRef]
- Wehbe, M.; Anantha, M.; Backstrom, I.; Leung, A.; Chen, K.; Malhotra, A.; Edwards, K.; Bally, M.B. Nanoscale Reaction Vessels Designed for Synthesis of Copper-Drug Complexes Suitable for Preclinical Development. PLoS ONE 2016, 11, e0153416. [Google Scholar] [CrossRef] [PubMed]
- Ren, L.; Feng, W.; Shao, J.; Ma, J.; Xu, M.; Zhu, B.-Z.; Zheng, N.; Liu, S. Diethyldithiocarbamate-copper nanocomplex reinforces disulfiram chemotherapeutic efficacy through light-triggered nuclear targeting. Theranostics 2020, 10, 6384–6398. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Suo, Y.; Zhang, Z.; Liu, R.; Liu, H.; Cheng, Z. Copper (II)-disulfiram loaded melanin-dots for cancer theranostics. Nanomed. Nanotechnol. Biol. Med. 2021, 32, 102340. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Liu, P.; Meng, Y.; Hu, S.; Ding, J.; Zhou, W. Nanoscale copper (II)–diethyldithiocarbamate coordination polymer as a drug self-delivery system for highly robust and specific cancer therapy. Mol. Pharm. 2020, 17, 2864–2873. [Google Scholar] [CrossRef]
- Wehbe, M.; Anantha, M.; Shi, M.; Leung, A.W.-y.; Dragowska, W.H.; Sanche, L.; Bally, M.B. Development and optimization of an injectable formulation of copper diethyldithiocarbamate, an active anticancer agent. Int. J. Nanomed. 2017, 12, 4129–4146. [Google Scholar] [CrossRef] [PubMed]
- Fasehee, H.; Ghavamzadeh, A.; Alimoghaddam, K.; Ghaffari, S.-H.; Faghihi, S. A comparative cytotoxic evaluation of disulfiram encapsulated PLGA nanoparticles on MCF-7 cells. Int. J. Hematol.-Oncol. Stem Cell Res. 2017, 11, 102–107. [Google Scholar]
- Yin, W.; Yu, X.; Kang, X.; Zhao, Y.; Zhao, P.; Jin, H.; Fu, X.; Wan, Y.; Peng, C.; Huang, Y. Remodeling tumor-associated macrophages and neovascularization overcomes EGFRT790M-associated drug resistance by PD-L1 nanobody-mediated codelivery. Small 2018, 14, 1802372. [Google Scholar] [CrossRef]
- Li, Y.; Lu, W.; Huang, Q.; Li, C.; Chen, W. Copper sulfide nanoparticles for photothermal ablation of tumor cells. Nanomedicine 2010, 5, 1161–1171. [Google Scholar] [CrossRef]
- Chen, Y.; Zhao, X.; Xiong, T.; Du, J.; Sun, W.; Fan, J.; Peng, X. NIR photosensitizers activated by γ-glutamyl transpeptidase for precise tumor fluorescence imaging and photodynamic therapy. Sci. China Chem. 2021, 64, 808–816. [Google Scholar] [CrossRef]
- Lu, Y.; Pan, Q.; Gao, W.; Pu, Y.; Luo, K.; He, B.; Gu, Z. Leveraging disulfiram to treat cancer: Mechanisms of action, delivery strategies, and treatment regimens. Biomaterials 2022, 281, 121335. [Google Scholar] [CrossRef]
- Zhao, P.; Tang, X.; Huang, Y. Teaching new tricks to old dogs: A review of drug repositioning of disulfiram for cancer nanomedicine. View 2021, 2, 20200127. [Google Scholar] [CrossRef]
- Paun, R.A.; Dumut, D.C.; Centorame, A.; Thuraisingam, T.; Hajduch, M.; Mistrik, M.; Dzubak, P.; De Sanctis, J.B.; Radzioch, D.; Tabrizian, M. One-step synthesis of nanoliposomal copper diethyldithiocarbamate and its assessment for cancer therapy. Pharmaceutics 2022, 14, 640. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).