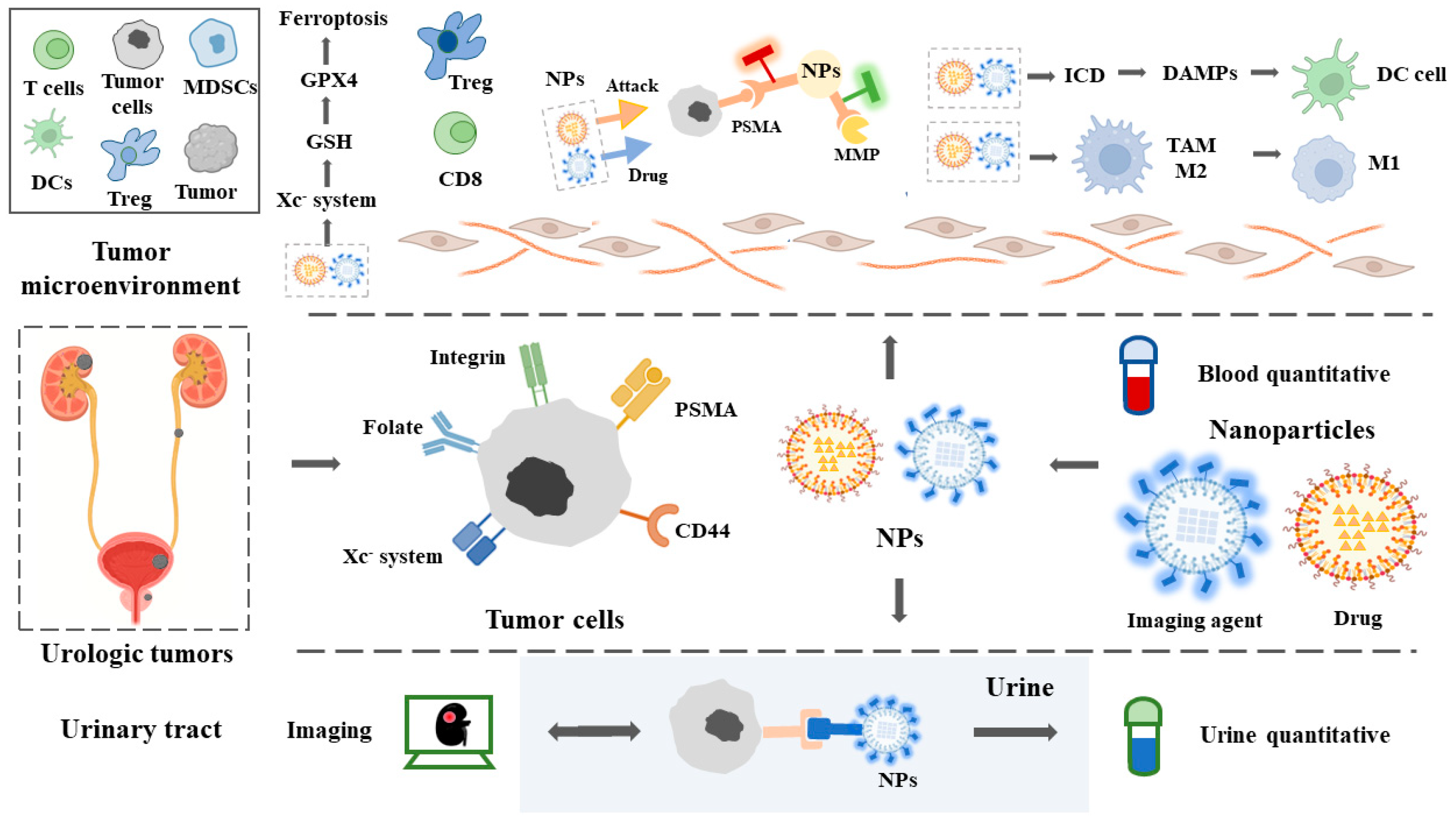
Nanomedicine for Combination Urologic Cancer Immunotherapy
Abstract
1. Introduction
2. Renal Cell Carcinoma
2.1. Immunotherapy of Renal Cell Carcinoma
2.2. Adoptive Cell Immunotherapy (ACI)
2.3. Vaccines
2.4. Nanoparticles in Renal Cell Carcinoma
2.4.1. Diagnosis
2.4.2. Treatment
3. Urothelial Carcinoma
3.1. Immunotherapy of Urothelial Carcinoma
3.2. BCG
3.3. Active Cell Immunotherapy (ACI)
3.4. Vaccines
3.5. Nanoparticles in Urothelial Carcinoma
3.5.1. Diagnosis
3.5.2. Treatment
4. Prostate Cancer
4.1. Immunotherapy for Prostate Cancer
4.2. ACI
4.3. Vaccines
4.4. Nanoparticles in Prostate Cancer
4.4.1. Diagnosis
4.4.2. Treatment
5. Conclusions and Outlook
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shao, N.; Tang, H.; Mi, Y.; Zhu, Y.; Wan, F.; Ye, D. A novel gene signature to predict immune infiltration and outcome in patients with prostate cancer. Oncoimmunology 2020, 9, 1762473. [Google Scholar] [CrossRef] [PubMed]
- Blackburn, S.D.; Shin, H.; Haining, W.N.; Zou, T.; Workman, C.J.; Polley, A.; Betts, M.R.; Freeman, G.J.; Vignali, D.A.; Wherry, E.J. Coregulation of CD8+ T cell exhaustion by multiple inhibitory receptors during chronic viral infection. Nat. Immunol. 2009, 10, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Topalian, S.L.; Drake, C.G.; Pardoll, D.M. Immune checkpoint blockade: A common denominator approach to cancer therapy. Cancer Cell 2015, 27, 450–461. [Google Scholar] [CrossRef] [PubMed]
- van der Merwe, P.A.; Bodian, D.L.; Daenke, S.; Linsley, P.; Davis, S.J. CD80 (B7-1) binds both CD28 and CTLA-4 with a low affinity and very fast kinetics. J. Exp. Med. 1997, 185, 393–404. [Google Scholar] [CrossRef]
- Ljungberg, B.; Bensalah, K.; Bex, A.; Canfield, S.; Dabestani, S.; Hofmann, F.; Hora, M.; Kuczyk, M.; Lam, T.; Marconi, L.; et al. Renal Cell Carcinoma; European Association of Urology: Arnhem, The Netherlands, 2015. [Google Scholar]
- Powles, T. Recent eUpdate to the ESMO Clinical Practice Guidelines on renal cell carcinoma on cabozantinib and nivolumab for first-line clear cell renal cancer: Renal cell carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up1. Ann. Oncol. 2021, 32, 422–423. [Google Scholar] [CrossRef]
- Motzer, R.J.; Jonasch, E.; Agarwal, N.; Alva, A.; Baine, M.; Beckermann, K.; Carlo, M.I.; Choueiri, T.K.; Costello, B.A.; Derweesh, I.H.; et al. Kidney cancer, version 3.2022, nccn clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2022, 20, 71–90. [Google Scholar] [CrossRef]
- Balar, A.V.; Castellano, D.; O’Donnell, P.H.; Grivas, P.; Vuky, J.; Powles, T.; Plimack, E.R.; Hahn, N.M.; de Wit, R.; Pang, L.; et al. First-line pembrolizumab in cisplatin-ineligible patients with locally advanced and unresectable or metastatic urothelial cancer (KEYNOTE-052): A multicentre, single-arm, phase 2 study. Lancet Oncol. 2017, 18, 1483–1492. [Google Scholar] [CrossRef]
- National Cancer Institute. Immunotherapy to Treat Cancer [EB/OL]. 24 May 2018. Available online: www.cancer.gov/about-cancer/treatment/types/im-Munotherapy (accessed on 8 December 2020).
- Zhao, Z.; Ukidve, A.; Kim, J.; Mitragotri, S. Targeting strategies for tissue-specific drug delivery. Cell 2020, 181, 151–167. [Google Scholar] [CrossRef]
- Khan, H.; Ullah, H.; Martorell, M.; Valdes, S.E.; Belwal, T.; Tejada, S.; Sureda, A.; Kamal, M.A. Flavonoids nanoparticles in cancer: Treatment, prevention and clinical prospects. Semin. Cancer Biol. 2021, 69, 200–211. [Google Scholar] [CrossRef]
- Liu, H.; Li, X.; Ji, M.; Wang, N.; Xu, Y.; Kong, Y.; Gou, J.; Yin, T.; He, H.; Zhang, Y.; et al. Two-step fabricating micelle-like nanoparticles of cisplatin with the ‘real’long circulation and high bioavailability for cancer therapy. Colloids Surf. B Biointerfaces 2022, 210, 112225. [Google Scholar] [CrossRef]
- Johannsen, M.; Gneveckow, U.; Taymoorian, K.; Thiesen, B.; Waldöfner, N.; Scholz, R.; Jung, K.; Jordan, A.; Wust, P.; Loening, S. Morbidity and quality of life during thermotherapy using magnetic nanoparticles in locally recurrent prostate cancer: Results of a prospective phase I trial. Int. J. Hyperth. 2007, 23, 315–323. [Google Scholar] [CrossRef]
- Kader, A.; Kaufmann, J.O.; Mangarova, D.B.; Moeckel, J.; Brangsch, J.; Adams, L.C.; Zhao, J.; Reimann, C.; Saatz, J.; Traub, H.; et al. Iron Oxide Nanoparticles for Visualization of Prostate Cancer in MRI. Cancers 2022, 14, 2909. [Google Scholar] [CrossRef]
- Amin, A.; Hammers, H. The evolving landscape of immunotherapy-based combinations for frontline treatment of advanced renal cell carcinoma. Front. Immunol. 2019, 9, 3120. [Google Scholar] [CrossRef]
- Motzer, R.J.; Escudier, B.; McDermott, D.F.; George, S.; Hammers, H.J.; Srinivas, S.; Tykodi, S.S.; Sosman, J.A.; Procopio, G.; Plimack, E.; et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N. Engl. J. Med. 2015, 373, 1803–1813. [Google Scholar] [CrossRef]
- Motzer, R.J.; Rini, B.I.; McDermott, D.F.; Redman, B.G.; Kuzel, T.M.; Harrison, M.R.; Vaishampayan, U.N.; Drabkin, H.A.; George, S.; Logan, T.F.; et al. Nivolumab for metastatic renal cell carcinoma: Results of a randomized phase II trial. J. Clin. Oncol. 2015, 33, 1430–1437. [Google Scholar] [CrossRef]
- Vogelzang, N.J.; Olsen, M.R.; McFarlane, J.J.; Arrowsmith, E.; Bauer, T.M.; Jain, R.K.; Somer, B.; Lam, E.T.; Kochenderfer, M.D.; Molina, A.; et al. Safety and efficacy of nivolumab in patients with advanced non–clear cell renal cell carcinoma: Results from the phase IIIb/IV CheckMate 374 study. Clin. Genitourin. Cancer 2020, 18, 461–468. [Google Scholar] [CrossRef]
- Motzer, R.J.; Tannir, N.M.; McDermott, D.F.; Frontera, O.A.; Melichar, B.; Choueiri, T.K.; Plimack, E.R.; Barthélémy, P.; Porta, C.; George, S.; et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N. Engl. J. Med. 2018, 378, 1277–1290. [Google Scholar] [CrossRef]
- Tartarone, A.; Roviello, G.; Lerose, R.; Roudi, R.; Aieta, M.; Zoppoli, P. Anti-PD-1 versus anti-PD-L1 therapy in patients with pretreated advanced non-small-cell lung cancer: A meta-analysis. Future Oncol. 2019, 15, 2423–2433. [Google Scholar] [CrossRef]
- Petrelli, F.; Ferrara, R.; Signorelli, D.; Ghidini, A.; Proto, C.; Roudi, R.; Sabet, M.N.; Facelli, S.; Garassino, M.C.; Luciani, A.; et al. Immune checkpoint inhibitors and chemotherapy in first-line NSCLC: A meta-analysis. Immunotherapy 2021, 13, 621–631. [Google Scholar] [CrossRef]
- McDermott, D.F.; Sosman, J.A.; Sznol, M.; Massard, C.; Gordon, M.S.; Hamid, O.; Powderly, J.D.; Infante, J.R.; Fassò, M.; Wang, Y.V.; et al. Atezolizumab, an anti-programmed death-ligand 1 antibody, in metastatic renal cell carcinoma: Long-term safety, clinical activity, and immune correlates from a phase Ia study. J. Clin. Oncol. 2016, 34, 833–842. [Google Scholar] [CrossRef]
- Rini, B.I.; Powles, T.; Atkins, M.B.; Escudier, B.; McDermott, D.F.; Suarez, C.; Bracarda, S.; Stadler, W.M.; Donskov, F.; Lee, J.L.; et al. Atezolizumab plus bevacizumab versus sunitinib in patients with previously untreated metastatic renal cell carcinoma (IMmotion151): A multicentre, open-label, phase 3, randomised controlled trial. Lancet 2019, 393, 2404–2415. [Google Scholar] [CrossRef] [PubMed]
- Voss, M.H.; Azad, A.A.; Hansen, A.R.; Gray, J.E.; Welsh, S.J.; Song, X.; Kuziora, M.; Meinecke, L.; Blando, J.; Achour, I.; et al. A Randomized Ph2 Study of MEDI0680 in Combination With Durvalumab vs. Nivolumab Monotherapy in Patients With Advanced or Metastatic Clear Cell Renal Cell Carcinoma. Clin. Cancer Res. 2022, 28, 3032–3041. [Google Scholar] [CrossRef] [PubMed]
- NCCN Clinical Practice Guideline–Melanoma. V3.2012. Available online: www.nccn.org (accessed on 10 September 2022).
- Rosenberg, S.A.; Lotze, M.T.; Muul, L.M.; Leitman, S.; Chang, A.E.; Ettinghausen, S.E.; Matory, Y.L.; Skibber, J.M.; Shiloni, E.; Vetto, J.T.; et al. Observations on the systemic administration of autologous lymphokine-activated killer cells and recombinant interleukin-2 to patients with metastatic cancer. N. Engl. J. Med. 1985, 313, 1485–1492. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, S.A.; Lotze, M.T.; Muul, L.M.; Chang, A.E.; Avis, F.P.; Leitman, S.; Linehan, W.M.; Robertson, C.N.; Lee, R.E.; Rubin, J.T.; et al. A progress report on the treatment of 157 patients with advanced cancer using lymphokine-activated killer cells and interleukin-2 or high-dose interleukin-2 alone. N. Engl. J. Med. 1987, 316, 889–897. [Google Scholar] [CrossRef]
- Rosenberg, S.A.; Spiess, P.; Lafreniere, R. A new approach to the adoptive immunotherapy of cancer with tumor-infiltrating lymphocytes. Science 1986, 233, 1318–1321. [Google Scholar] [CrossRef]
- Hayakawa, K.; Salmeron, M.; Parkinson, D.; Markowitz, A.; Von Eschenbach, A.; Legha, S.; Balch, C.; Ross, M.; Augustus, L.; Itoh, K. Study of tumor-infiltrating lymphocytes for adoptive therapy of renal cell carcinoma (RCC) and metastatic melanoma: Sequential proliferation of cytotoxic natural killer and noncytotoxic T cells in RCC. J. Immunother. Off. J. Soc. Biol. Ther. 1991, 10, 313–325. [Google Scholar] [CrossRef]
- Figlin, R.A.; Thompson, J.A.; Bukowski, R.M.; Vogelzang, N.J.; Novick, A.C.; Lange, P.; Steinberg, G.D.; Belldegrun, A.S. Multicenter, randomized, phase III trial of CD8+ tumor-infiltrating lymphocytes in combination with recombinant interleukin-2 in metastatic renal cell carcinoma. J. Clin. Oncol. 1999, 17, 2521–2529. [Google Scholar] [CrossRef]
- Liu, L.; Zhang, W.; Qi, X.; Li, H.; Yu, J.; Wei, S.; Hao, X.; Ren, X. Randomized Study of Autologous Cytokine-Induced Killer Cell Immunotherapy in Metastatic Renal CarcinomaTreatment with CIK Cell in Metastatic RCC. Clin. Cancer Res. 2012, 18, 1751–1759. [Google Scholar] [CrossRef]
- Wang, M.; Cao, J.X.; Pan, J.H.; Liu, Y.S.; Xu, B.L.; Li, D.; Zhang, X.Y.; Li, J.L.; Liu, J.L.; Wang, H.B.; et al. Adoptive immunotherapy of cytokine-induced killer cell therapy in the treatment of non-small cell lung cancer. PLoS ONE 2014, 9, e112662. [Google Scholar] [CrossRef]
- Jia, H.; Tian, Y.; Jiang, C.G.; Han, W. Evaluation of 29 indicators for the prognosis of advanced non-small cell lung cancer with cytokine-induced killer cell therapy combined with chemotherapy. Exp. Ther. Med. 2016, 11, 1601–1610. [Google Scholar] [CrossRef]
- Zhou, L.; Xiong, Y.; Wang, Y.; Meng, Y.; Zhang, W.; Shen, M.; Zhang, X.; Li, S.; Ren, B.; Li, R.; et al. A phase IB trial of autologous cytokine-induced killer cells in combination with sintilimab, monoclonal antibody against programmed cell death-1, plus chemotherapy in patients with advanced non-small-cell lung cancer. Clin. Lung Cancer 2022, 23, 709–719. [Google Scholar] [CrossRef]
- Ji, F.; Zhang, F.; Zhang, M.; Long, K.; Xia, M.; Lu, F.; Li, E.; Chen, J.; Li, J.; Chen, Z.; et al. Targeting the DNA damage response enhances CD70 CAR-T cell therapy for renal carcinoma by activating the cGAS-STING pathway. J. Hematol. Oncol. 2021, 14, 152. [Google Scholar] [CrossRef]
- Amin, A.; Dudek, A.Z.; Logan, T.F.; Lance, R.S.; Holzbeierlein, J.M.; Knox, J.J.; Master, V.A.; Pal, S.K.; Miller, W.H.; Karsh, L.I.; et al. Survival with AGS-003, an autologous dendritic cell–based immunotherapy, in combination with sunitinib in unfavorable risk patients with advanced renal cell carcinoma (RCC): Phase 2 study results. J. Immunother. Cancer 2015, 3, 14. [Google Scholar] [CrossRef]
- Figlin, R.A.; Tannir, N.M.; Uzzo, R.G.; Tykodi, S.S.; Chen, D.Y.; Master, V.; Kapoor, A.; Vaena, D.; Lowrance, W.; Bratslavsky, G.; et al. Results of the ADAPT Phase 3 Study of Rocapuldencel-T in Combination with Sunitinib as First-Line Therapy in Patients with Metastatic Renal Cell CarcinomaRocapuldencel-T in Combination Therapy for mRCC. Clin. Cancer Res. 2020, 26, 2327–2336. [Google Scholar] [CrossRef]
- Rini, B.I.; Stenzl, A.; Zdrojowy, R.; Kogan, M.; Shkolnik, M.; Oudard, S.; Weikert, S.; Bracarda, S.; Crabb, S.J.; Bedke, J.; et al. IMA901, a multipeptide cancer vaccine, plus sunitinib versus sunitinib alone, as first-line therapy for advanced or metastatic renal cell carcinoma (IMPRINT): A multicentre, open-label, randomised, controlled, phase 3 trial. Lancet Oncol. 2016, 17, 1599–1611. [Google Scholar] [CrossRef]
- Faiena, I.; Comin-Anduix, B.; Berent-Maoz, B.; Bot, A.; Zomorodian, N.; Sachdeva, A.; Said, J.; Cheung-Lau, G.; Pang, J.; Macabali, M.; et al. A Phase I, Open-label, Dose-escalation, and Cohort Expansion Study to Evaluate the Safety and Immune Response to Autologous Dendritic Cells Transduced with AdGMCA9 (DC-AdGMCAIX) in Patients with Metastatic Renal Cell Carcinoma. J. Immunother. 2020, 43, 273–282. [Google Scholar] [CrossRef]
- Wang, L.; Yang, D.; Lv, J.Y.; Yu, D.; Xin, S.J. Application of carbon nanoparticles in lymph node dissection and parathyroid protection during thyroid cancer surgeries: A systematic review and meta-analysis. OncoTargets Ther. 2017, 10, 1247–1260. [Google Scholar] [CrossRef]
- Kamaly, N.; He, J.C.; Ausiello, D.A.; Farokhzad, O.C. Nanomedicines for renal disease: Current status and future applications. Nat. Rev. Nephrol. 2016, 12, 738–753. [Google Scholar] [CrossRef]
- Ehlerding, E.B.; Grodzinski, P.; Cai, W.; Liu, C.H. Big potential from small agents: Nanoparticles for imaging-based companion diagnostics. ACS Nano 2018, 12, 2106–2121. [Google Scholar] [CrossRef]
- Choi, Y.E.; Kwak, J.W.; Park, J.W. Nanotechnology for early cancer detection. Sensors 2010, 10, 428–455. [Google Scholar] [CrossRef]
- Zheng, S.; Zhang, M.; Bai, H.; He, M.; Dong, L.; Cai, L.; Zhao, M.; Wang, Q.; Xu, K.; Li, J. Preparation of AS1411 aptamer modified Mn-MoS2 QDs for targeted MR imaging and fluorescence labelling of renal cell carcinoma. Int. J. Nanomed. 2019, 14, 9513–9524. [Google Scholar] [CrossRef] [PubMed]
- Ordikhani, F.; Kasinath, V.; Uehara, M.; Akbarzadeh, A.; Yilmam, O.A.; Dai, L.; Aksu, H.; Jung, S.; Jiang, L.; Li, X.; et al. Selective trafficking of light chain-conjugated nanoparticles to the kidney and renal cell carcinoma. Nano Today 2020, 35, 100990. [Google Scholar] [CrossRef] [PubMed]
- Arendowski, A.; Ossolin´ski, K.; Ossolin´ska, A.; Ossolin´ski, T.; Nizioł, J.; Ruman, T. Serum and urine analysis with gold nanoparticle-assisted laser desorption/ionization mass spectrometry for renal cell carcinoma metabolic biomarkers discovery. Adv. Med. Sci. 2021, 66, 326–335. [Google Scholar] [CrossRef] [PubMed]
- Guimaraes, A.R.; Tabatabei, S.; Dahl, D.; McDougal, W.S.; Weissleder, R.; Harisinghani, M.G. Pilot study evaluating use of lymphotrophic nanoparticle-enhanced magnetic resonance imaging for assessing lymph nodes in renal cell cancer. Urology 2008, 71, 708–712. [Google Scholar] [CrossRef]
- Lu, C.; Li, J.; Xu, K.; Yang, C.; Wang, J.; Han, C.; Liu, X. Fabrication of mAb G250-SPIO molecular magnetic resonance imaging nanoprobe for the specific detection of renal cell carcinoma in vitro. PLoS ONE 2014, 9, e101898. [Google Scholar] [CrossRef]
- Muz, B.; de la Puente, P.; Azab, F.; Azab, A.K. The role of hypoxia in cancer progression, angiogenesis, metastasis, and resistance to therapy. Hypoxia 2015, 3, 83–92. [Google Scholar] [CrossRef]
- Grillone, A.; Riva, E.R.; Mondini, A.; Forte, C.; Calucci, L.; Innocenti, C.; de Julian Fernandez, C.; Cappello, V.; Gemmi, M.; Moscato, S.; et al. Active targeting of sorafenib: Preparation, characterization, and in vitro testing of drug-loaded magnetic solid lipid nanoparticles. Adv. Healthc. Mater. 2015, 4, 1681–1690. [Google Scholar] [CrossRef]
- Zhu, X.W.; Dong, F.M.; Liu, J.; Li, M.S. Resveratrol Nanoparticles Suppresses Migration and Invasion of Renal Cell Carcinoma Cells by Inhibiting Matrix Metalloproteinase 2 Expression and Extracellular Signal-Regulated Kinase Pathway. J. Biomed. Nanotechnol. 2022, 18, 1001–1008. [Google Scholar] [CrossRef]
- Liu, J.; Abshire, C.; Carry, C.; Sholl, A.B.; Mandava, S.H.; Datta, A.; Ranjan, M.; Callaghan, C.; Peralta, D.V.; Williams, K.S.; et al. Nanotechnology combined therapy: Tyrosine kinase-bound gold nanorod and laser thermal ablation produce a synergistic higher treatment response of renal cell carcinoma in a murine model. BJU Int. 2017, 119, 342–348. [Google Scholar] [CrossRef]
- Kim, H.; Niu, L.; Larson, P.; Kucaba, T.A.; Murphy, K.A.; James, B.R.; Ferguson, D.M.; Griffith, T.S.; Panyam, J. Polymeric nanoparticles encapsulating novel TLR7/8 agonists as immunostimulatory adjuvants for enhanced cancer immunotherapy. Biomaterials 2018, 164, 38–53. [Google Scholar] [CrossRef]
- Alsaab, H.O.; Sau, S.; Alzhrani, R.M.; Cheriyan, V.T.; Polin, L.A.; Vaishampayan, U.; Rishi, A.K.; Iyer, A.K. Tumor hypoxia directed multimodal nanotherapy for overcoming drug resistance in renal cell carcinoma and reprogramming macrophages. Biomaterials 2018, 183, 280–294. [Google Scholar] [CrossRef]
- Chai, D.; Shan, H.; Wang, G.; Zhang, Q.; Li, H.; Fang, L.; Song, J.; Liu, N.; Zhang, Q.; Yao, H.; et al. Combining DNA Vaccine and AIM2 in H1 Nanoparticles Exert Anti-Renal Carcinoma Effects via Enhancing Tumor-Specific Multi-functional CD8+ T-cell ResponsesDNA Vaccine Activating Multi-function CD8 T-cell Response. Mol. Cancer Ther. 2019, 18, 323–334. [Google Scholar] [CrossRef]
- Herr, H.W.; Morales, A. History of bacillus Calmette-Guerin and bladder cancer: An immunotherapy success story. J. Urol. 2008, 179, 53–56. [Google Scholar] [CrossRef]
- Grivas, P.; Plimack, E.R.; Balar, A.V.; Castellano, D.; O’Donnell, P.H.; Bellmunt, J.; Powles, T.; Hahn, N.M.; de Wit, R.; Bajorin, D.F.; et al. Pembrolizumab as first-line therapy in cisplatin-ineligible advanced urothelial cancer (KEYNOTE-052): Outcomes in older patients by age and performance status. Eur. Urol. Oncol. 2020, 3, 351–359. [Google Scholar] [CrossRef]
- Necchi, A.; Joseph, R.; Loriot, Y.; Hoffman-Censits, J.; Perez-Gracia, J.; Petrylak, D.; Derleth, C.; Tayama, D.; Zhu, Q.; Ding, B.; et al. Atezolizumab in platinum-treated locally advanced or metastatic urothelial carcinoma: Post-progression outcomes from the phase II IMvigor210 study. Ann. Oncol. 2017, 28, 3044–3050. [Google Scholar] [CrossRef]
- Galsky, M.D.; Arija, J.Á.A.; Bamias, A.; Davis, I.D.; De Santis, M.; Kikuchi, E.; Garcia-del Muro, X.; De Giorgi, U.; Mencinger, M.; Izumi, K.; et al. Atezolizumab with or without chemotherapy in metastatic urothelial cancer (IMvigor130): A multicentre, randomised, placebo-controlled phase 3 trial. Lancet 2020, 395, 1547–1557. [Google Scholar] [CrossRef]
- Rexer, H.; Retz, M.; Waller, C. Erstlinientherapie beim unbehandelten nicht resektablen oder metastasierten Urothelkarzinom: Eine offene, randomisierte, Phase-III Studie zu Nivolumab in Kombination mit Ipilimumab oder mit Standardchemotherapie gegenüber Standard-Chemotherapie bei Patienten mit bisher unbehandeltem inoperablen oder metastasierten Urothelkarzinom (CheckMate-901)–AB 59/17 der AUO. Aktuelle Urol. 2019, 50, 20–21. [Google Scholar]
- Sharma, P.; Siefker-Radtke, A.; de Braud, F.; Basso, U.; Calvo, E.; Bono, P.; Morse, M.A.; Ascierto, P.A.; Lopez-Martin, J.; Brossart, P.; et al. Nivolumab alone and with ipilimumab in previously treated metastatic urothelial carcinoma: CheckMate 032 nivolumab 1 mg/kg plus ipilimumab 3 mg/kg expansion cohort results. J. Clin. Oncol. 2019, 37, 1608–1616. [Google Scholar] [CrossRef]
- Babjuk, M.; Böhle, A.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Hernández, V.; Kaasinen, E.; Palou, J.; Rouprêt, M.; et al. EAU guidelines on non–muscle-invasive urothelial carcinoma of the bladder: Update 2016. Eur. Urol. 2017, 71, 447–461. [Google Scholar] [CrossRef]
- Han, J.; Gu, X.; Li, Y.; Wu, Q. Mechanisms of BCG in the treatment of bladder cancer-current understanding and the prospect. Biomed. Pharmacother. 2020, 129, 110393. [Google Scholar] [CrossRef]
- Matulewicz, R.S.; Steinberg, G.D. Non—Muscle-invasive Bladder Cancer: Overview and Contemporary Treatment Landscape of Neoadjuvant Chemoablative Therapies. Rev. Urol. 2020, 22, 43–51. [Google Scholar] [PubMed]
- Sherif, A.; Hasan, M.N.; Radecka, E.; Rodriguez, A.L.; Shabo, S.; Karlsson, M.; Schumacher, M.C.; Marits, P.; Winqvist, O. Pilot study of adoptive immunotherapy with sentinel node-derived T cells in muscle-invasive urinary bladder cancer. Scand. J. Urol. 2015, 49, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Obara, W.; Eto, M.; Mimata, H.; Kohri, K.; Mitsuhata, N.; Miura, I.; Shuin, T.; Miki, T.; Koie, T.; Fujimoto, H.; et al. A phase I/II study of cancer peptide vaccine S-288310 in patients with advanced urothelial carcinoma of the bladder. Ann. Oncol. 2017, 28, 798–803. [Google Scholar] [CrossRef] [PubMed]
- Suekane, S.; Ueda, K.; Nishihara, K.; Sasada, T.; Yamashita, T.; Koga, N.; Yutani, S.; Shichijo, S.; Itoh, K.; Igawa, T.; et al. Personalized peptide vaccination as second-line treatment for metastatic upper tract urothelial carcinoma. Cancer Sci. 2017, 108, 2430–2437. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.y.; Zhang, H.; Luo, J.; Li, Y.; Gao, T.; Lara, P.N., Jr.; de Vere White, R.; Lam, K.S.; Pan, C.X. Multifunctional targeting micelle nanocarriers with both imaging and therapeutic potential for bladder cancer. Int. J. Nanomed. 2012, 7, 2793–2804. [Google Scholar] [CrossRef]
- Eissa, S.; Matboli, M.; Essawy, N.O.; Shehta, M.; Kotb, Y.M. Rapid detection of urinary long non-coding RNA urothelial carcinoma associated one using a PCR-free nanoparticle-based assay. Biomarkers 2015, 20, 212–217. [Google Scholar] [CrossRef]
- Sweeney, S.K.; Luo, Y.; O’Donnell, M.A.; Assouline, J. Nanotechnology and cancer: Improving real-time monitoring and staging of bladder cancer with multimodal mesoporous silica nanoparticles. Cancer Nanotechnol. 2016, 7, 3. [Google Scholar] [CrossRef]
- Zhang, W.; Zhao, K.; Banks, C.E.; Zhang, Y. Antibody-modified hydroxyapatite surfaces for the efficient capture of bladder cancer cells in a patient’s urine without recourse to any sample pre-treatment. J. Mater. Chem. B 2017, 5, 8125–8132. [Google Scholar] [CrossRef]
- Azevedo, R.; Soares, J.; Gaiteiro, C.; Peixoto, A.; Lima, L.; Ferreira, D.; Relvas-Santos, M.; Fernandes, E.; Tavares, A.; Cotton, S.; et al. Glycan affinity magnetic nanoplatforms for urinary glycobiomarkers discovery in bladder cancer. Talanta 2018, 184, 347–355. [Google Scholar] [CrossRef]
- GuhaSarkar, S.; Banerjee, R. Intravesical drug delivery: Challenges, current status, opportunities and novel strategies. J. Control. Release 2010, 148, 147–159. [Google Scholar] [CrossRef]
- Zacchè, M.M.; Srikrishna, S.; Cardozo, L. Novel targeted bladder drug-delivery systems: A review. Res. Rep. Urol. 2015, 7, 169–178. [Google Scholar] [CrossRef]
- Lu, Z.; Yeh, T.K.; Wang, J.; Chen, L.; Lyness, G.; Xin, Y.; Wientjes, M.G.; Bergdall, V.; Couto, G.; Alvarez-Berger, F.; et al. Paclitaxel gelatin nanoparticles for intravesical bladder cancer therapy. J. Urol. 2011, 185, 1478–1483. [Google Scholar] [CrossRef]
- Ko, Y.J.; Canil, C.M.; Mukherjee, S.D.; Winquist, E.; Elser, C.; Eisen, A.; Reaume, M.N.; Zhang, L.; Sridhar, S.S. Nanoparticle albumin-bound paclitaxel for second-line treatment of metastatic urothelial carcinoma: A single group, multicentre, phase 2 study. Lancet Oncol. 2013, 14, 769–776. [Google Scholar] [CrossRef]
- Huang, H.H.; Kuo, S.M.; Wu, Y.J.; Su, J.H. Improvement and enhancement of antibladder carcinoma cell effects of heteronemin by the nanosized hyaluronan aggregation. Int. J. Nanomed. 2016, 11, 1237–1251. [Google Scholar] [CrossRef]
- Sahatsapan, N.; Ngawhirunpat, T.; Rojanarata, T.; Opanasopit, P.; Patrojanasophon, P. Catechol-functionalized alginate nanoparti-cles as Mucoadhesive carriers for Intravesical chemotherapy. AAPS PharmSciTech 2020, 21, 212. [Google Scholar] [CrossRef]
- Hsu, C.W.; Cheng, N.C.; Liao, M.Y.; Cheng, T.Y.; Chiu, Y.C. Development of Folic Acid-Conjugated and Methylene Blue-Adsorbed Au@ TNA Nanoparticles for Enhanced Photodynamic Therapy of Bladder Cancer Cells. Nanomaterials 2020, 10, 1351. [Google Scholar] [CrossRef]
- Zhu, Z.; Ma, A.H.; Zhang, H.; Lin, T.Y.; Xue, X.; Farrukh, H.; Zhu, S.; Shi, W.; Yuan, R.; Cao, Z.; et al. Phototherapy with cancer-specific nanoporphyrin potentiates immunotherapy in bladder cancer. Clin. Cancer Res. 2022, 28, 4820–4831. [Google Scholar] [CrossRef]
- Zhou, Q.; Ding, W.; Qian, Z.; Zhu, Q.; Sun, C.; Yu, Q.; Tai, Z.; Xu, K. Immunotherapy Strategy Targeting Programmed Cell Death Ligand 1 and CD73 with Macrophage-Derived Mimetic Nanovesicles to Treat Bladder Cancer. Mol. Pharm. 2021, 18, 4015–4028. [Google Scholar] [CrossRef]
- Terán-Navarro, H.; Zeoli, A.; Salines-Cuevas, D.; Marradi, M.; Montoya, N.; Gonzalez-Lopez, E.; Ocejo-Vinyals, J.G.; Dominguez-Esteban, M.; Gutierrez-Baños, J.L.; Campos-Juanatey, F.; et al. Gold Glyconanoparticles Combined with 91–99 Peptide of the Bacterial Toxin, Listeriolysin O, Are Efficient Immunotherapies in Experimental Bladder Tumors. Cancers 2022, 14, 2413. [Google Scholar] [CrossRef]
- Scher, H.I.; Morris, M.J.; Stadler, W.M.; Higano, C.; Basch, E.; Fizazi, K.; Antonarakis, E.S.; Beer, T.M.; Carducci, M.A.; Chi, K.N.; et al. Trial design and objectives for castration-resistant prostate cancer: Updated recommendations from the Prostate Cancer Clinical Trials Working Group 3. J. Clin. Oncol. 2016, 34, 1402–1418. [Google Scholar] [CrossRef]
- Antonarakis, E.S.; Piulats, J.M.; Gross-Goupil, M.; Goh, J.; Ojamaa, K.; Hoimes, C.J.; Vaishampayan, U.; Berger, R.; Sezer, A.; Alanko, T.; et al. Pembrolizumab for treatment-refractory metastatic castration-resistant prostate cancer: Multicohort, open-label phase II KEYNOTE-199 study. J. Clin. Oncol. 2020, 38, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Petrylak, D.P.; Ratta, R.; Gafanov, R.; Facchini, G.; Piulats, J.M.; Kramer, G.; Flaig, T.W.; Chandana, S.R.; Li, B.; Burgents, J.; et al. KEYNOTE-921: Phase III study of pembrolizumab plus docetaxel for metastatic castration-resistant prostate cancer. Future Oncol. 2021, 17, 3291–3299. [Google Scholar] [CrossRef] [PubMed]
- Tabernero, J.; Andre, F.; Blay, J.Y.; Bustillos, A.; Fear, S.; Ganta, S.; Jaeger, D.; Maio, M.; Mileshkin, L.; Melero, I. Phase II multicohort study of atezolizumab monotherapy in multiple advanced solid cancers. ESMO Open 2022, 7, 100419. [Google Scholar] [CrossRef] [PubMed]
- Small, E.J.; Tchekmedyian, N.S.; Rini, B.I.; Fong, L.; Lowy, I.; Allison, J.P. A pilot trial of CTLA-4 blockade with human anti-CTLA-4 in patients with hormone-refractory prostate cancer. Clin. Cancer Res. 2007, 13, 1810–1815. [Google Scholar] [CrossRef]
- Kwon, E.D.; Drake, C.G.; Scher, H.I.; Fizazi, K.; Bossi, A.; Van den Eertwegh, A.J.; Krainer, M.; Houede, N.; Santos, R.; Mahammedi, H.; et al. Ipilimumab versus placebo after radiotherapy in patients with metastatic castration-resistant prostate cancer that had progressed after docetaxel chemotherapy (CA184-043): A multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 2014, 15, 700–712. [Google Scholar] [CrossRef]
- Fizazi, K.; Drake, C.G.; Beer, T.M.; Kwon, E.D.; Scher, H.I.; Gerritsen, W.R.; Bossi, A.; Van den Eertwegh, A.J.; Krainer, M.; Houede, N.; et al. Final analysis of the ipilimumab versus placebo following radiotherapy phase III trial in postdocetaxel metastatic castration-resistant prostate cancer identifies an excess of long-term survivors. Eur. Urol. 2020, 78, 822–830. [Google Scholar] [CrossRef]
- Sharma, P.; Pachynski, R.K.; Narayan, V.; Fléchon, A.; Gravis, G.; Galsky, M.D.; Mahammedi, H.; Patnaik, A.; Subudhi, S.K.; Ciprotti, M.; et al. Nivolumab plus ipilimumab for metastatic castration-resistant prostate cancer: Preliminary analysis of patients in the CheckMate 650 trial. Cancer Cell 2020, 38, 489–499. [Google Scholar] [CrossRef]
- Evan, Y.Y.; Kolinsky, M.P.; Berry, W.R.; Retz, M.; Mourey, L.; Piulats, J.M.; Appleman, L.J.; Romano, E.; Gravis, G.; Gurney, H.; et al. Pembrolizumab Plus Docetaxel and Prednisone in Patients with Metastatic Castration-resistant Prostate Cancer: Long-term Results from the Phase 1b/2 KEYNOTE-365 Cohort B Study. Eur. Urol. 2022, 82, 22–30. [Google Scholar]
- Stein, M.N.; Fong, L.; Tutrone, R.; Mega, A.; Lam, E.T.; Parsi, M.; Vangala, S.; Gutierrez, A.A.; Haas, N.B. ADXS31142 Immunotherapy Pembrolizumab Treatment for Metastatic Castration-Resistant Prostate Cancer: Open-Label Phase I/II KEYNOTE-046 Study. Oncologist 2022, 27, 453–461. [Google Scholar] [CrossRef]
- McNeel, D.G.; Eickhoff, J.C.; Wargowski, E.; Johnson, L.E.; Kyriakopoulos, C.E.; Emamekhoo, H.; Lang, J.M.; Brennan, M.J.; Liu, G. Phase 2 trial of T-cell activation using MVI-816 and pembrolizumab in patients with metastatic, castration-resistant prostate cancer (mCRPC). J. Immunother. Cancer 2022, 10, e004198. [Google Scholar] [CrossRef]
- Ross, A.E.; Hurley, P.J.; Tran, P.T.; Rowe, S.P.; Benzon, B.; Neal, T.O.; Chapman, C.; Harb, R.; Milman, Y.; Trock, B.J.; et al. A pilot trial of pembrolizumab plus prostatic cryotherapy for men with newly diagnosed oligometastatic hormone-sensitive prostate cancer. Prostate Cancer Prostatic Dis. 2020, 23, 184–193. [Google Scholar] [CrossRef]
- Saeki, N.; Gu, J.; Yoshida, T.; Wu, X. Prostate Stem Cell Antigen: A Jekyll and Hyde Molecule? PSCA In Cancer Etiology, Diagnosis, Prognosis, and Therapy. Clin. Cancer Res. 2010, 16, 3533–3538. [Google Scholar] [CrossRef]
- Ristau, B.T.; O’Keefe, D.S.; Bacich, D.J. The prostate-specific membrane antigen: Lessons and current clinical implications from 20 years of research. Urol. Oncol. Semin. Orig. Investig. 2014, 32, 272–279. [Google Scholar] [CrossRef]
- Priceman, S.J.; Gerdts, E.A.; Tilakawardane, D.; Kennewick, K.T.; Murad, J.P.; Park, A.K.; Jeang, B.; Yamaguchi, Y.; Yang, X.; Urak, R.; et al. Co-stimulatory signaling determines tumor antigen sensitivity and persistence of CAR T cells targeting PSCA+metastatic prostate cancer. Oncoimmunology 2018, 7, e1380764. [Google Scholar] [CrossRef]
- Narayan, V.; Barber-Rotenberg, J.S.; Jung, I.Y.; Lacey, S.F.; Rech, A.J.; Davis, M.M.; Hwang, W.T.; Lal, P.; Carpenter, E.L.; Maude, S.L.; et al. PSMA-targeting TGFβ-insensitive armored CAR T cells in metastatic castration-resistant prostate cancer: A phase 1 trial. Nat. Med. 2022, 28, 724–734. [Google Scholar] [CrossRef]
- Nada, M.H.; Wang, H.; Workalemahu, G.; Tanaka, Y.; Morita, C.T. Enhancing adoptive cancer immunotherapy with Vγ2Vδ2 T cells through pulse zoledronate stimulation. J. Immunother. Cancer 2017, 5, 9. [Google Scholar] [CrossRef]
- Labeur, M.S.; Roters, B.; Pers, B.; Mehling, A.; Luger, T.A.; Schwarz, T.; Grabbe, S. Generation of tumor immunity by bone marrow-derived dendritic cells correlates with dendritic cell maturation stage. J. Immunol. 1999, 162, 168–175. [Google Scholar] [CrossRef]
- Small, E.J.; Schellhammer, P.F.; Higano, C.S.; Redfern, C.H.; Nemunaitis, J.J.; Valone, F.H.; Verjee, S.S.; Jones, L.A.; Hershberg, R.M. Placebo-controlled phase III trial of immunologic therapy with sipuleucel-T (APC8015) in patients with metastatic, asymptomatic hormone refractory prostate cancer. J. Clin. Oncol. 2006, 24, 3089–3094. [Google Scholar] [CrossRef]
- Weber, J.S.; Vogelzang, N.J.; Ernstoff, M.S.; Goodman, O.B.; Cranmer, L.D.; Marshall, J.L.; Miles, S.; Rosario, D.; Diamond, D.C.; Qiu, Z.; et al. A phase 1 study of a vaccine targeting preferentially expressed antigen in melanoma and prostate-specific membrane antigen in patients with advanced solid tumors. J. Immunother. 2011, 34, 556–567. [Google Scholar] [CrossRef]
- Filaci, G.; Fenoglio, D.; Nolè, F.; Zanardi, E.; Tomasello, L.; Aglietta, M.; Del Conte, G.; Carles, J.; Morales-Barrera, R.; Guglielmini, P.; et al. Telomerase-based GX301 cancer vaccine in patients with metastatic castration-resistant prostate cancer: A randomized phase II trial. Cancer Immunol. Immunother. 2021, 70, 3679–3692. [Google Scholar] [CrossRef]
- Bilusic, M.; McMahon, S.; Madan, R.A.; Karzai, F.; Tsai, Y.T.; Donahue, R.N.; Palena, C.; Jochems, C.; Marté, J.L.; Floudas, C.; et al. Phase I study of a multitargeted recombinant Ad5 PSA/MUC-1/brachyury-based immunotherapy vaccine in patients with metastatic castration-resistant prostate cancer (mCRPC). J. Immunother. Cancer 2021, 9, e002374. [Google Scholar] [CrossRef] [PubMed]
- Litwin, M.S.; Tan, H.J. The diagnosis and treatment of prostate cancer: A review. JAMA 2017, 317, 2532–2542. [Google Scholar] [CrossRef] [PubMed]
- Yan, R.; Lu, N.; Han, S.; Lu, Z.; Xiao, Y.; Zhao, Z.; Zhang, M. Simultaneous detection of dual biomarkers using hierarchical MoS2 nanostructuring and nano-signal amplification-based electrochemical aptasensor toward accurate diagnosis of prostate cancer. Biosens. Bioelectron. 2022, 197, 113797. [Google Scholar] [CrossRef] [PubMed]
- Hara, D.; Tao, W.; Totiger, T.M.; Pourmand, A.; Dogan, N.; Ford, J.C.; Shi, J.; Pollack, A. Prostate Cancer Targeted X-ray Fluorescence Imaging via Gold Nanoparticles Functionalized with Prostate-Specific Membrane Antigen (PSMA). Int. J. Radiat. Oncol. Biol. Phys. 2021, 111, 220–232. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Ding, J.; Deng, L.; Xiang, Y.; Liu, D.; Zhang, Y.; Chen, X.; Yang, Q. Selection of DNA aptamers recognizing EpCAM-positive prostate cancer by cell-SELEX for in vitro and in vivo MR imaging. Drug Des. Dev. Ther. 2021, 15, 3985–3996. [Google Scholar] [CrossRef]
- Winter, A.; Chavan, A.; Wawroschek, F. Magnetic resonance imaging of sentinel lymph nodes using intraprostatic injection of superparamagnetic iron oxide nanoparticles in prostate cancer patients: First-in-human results. Eur. Urol. 2018, 73, 813–814. [Google Scholar] [CrossRef]
- Tanaudommongkon, I.; Tanaudommongkon, A.; Prathipati, P.; Nguyen, J.T.; Keller, E.T.; Dong, X. Curcumin nanoparticles and their cytotoxicity in docetaxel-resistant castration-resistant prostate cancer cells. Biomedicines 2020, 8, 253. [Google Scholar] [CrossRef]
- Singh, S.P.; Mishra, A.; Shyanti, R.K.; Singh, R.P.; Acharya, A. Silver nanoparticles synthesized using Carica papaya leaf extract (AgNPs-PLE) causes cell cycle arrest and apoptosis in human prostate (DU145) cancer cells. Biol. Trace Elem. Res. 2021, 199, 1316–1331. [Google Scholar] [CrossRef]
- Sharma, A.N.; Upadhyay, P.K.; Dewangan, H.K. Development, Evaluation, Pharmacokinetic and Biodistribution Estimation of Resveratrol Loaded Solid Lipid Nanoparticles for Prostate Cancer Targeting. J. Microencapsul. 2022, 39, 563–574. [Google Scholar] [CrossRef]
- Khoobchandani, M.; Khan, A.; Katti, K.K.; Thipe, V.C.; Al-Yasiri, A.Y.; MohanDoss, D.K.; Nicholl, M.B.; Lugão, A.B.; Hans, C.P.; Katti, K.V. Green nanotechnology of MGF-AuNPs for immunomodulatory intervention in prostate cancer therapy. Sci. Rep. 2021, 11, 16797. [Google Scholar] [CrossRef]
- Conte, R.; Valentino, A.; Di Cristo, F.; Peluso, G.; Cerruti, P.; Di Salle, A.; Calarco, A. Cationic polymer nanoparticles-mediated delivery of miR-124 impairs tumorigenicity of prostate cancer cells. Int. J. Mol. Sci. 2020, 21, 869. [Google Scholar] [CrossRef]
- Guo, Q.; Dong, Y.; Zhang, Y.; Fu, H.; Chen, C.; Wang, L.; Yang, X.; Shen, M.; Yu, J.; Chen, M.; et al. Sequential Release of Pooled siRNAs and Paclitaxel by Aptamer-Functionalized Shell–Core Nanoparticles to Overcome Paclitaxel Resistance of Prostate Cancer. ACS Appl. Mater. Interfaces 2021, 13, 13990–14003. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, Y.; Liu, C.; Zha, W.; Dong, S.; Xing, H.; Li, X. Multifunctional Lipid Nanoparticles for Protein Kinase N3 shRNA Delivery and Prostate Cancer Therapy. Mol. Pharm. 2022, 19, 4588–4600. [Google Scholar] [CrossRef]
- Akkurt, M.G.; Gülsoy, M. Polylactide nanoparticles encapsulating indocyanine green for photothermal therapy of prostate cancer cells. Photodiagnosis Photodyn. Ther. 2022, 37, 102693. [Google Scholar] [CrossRef]
- Islam, M.A.; Rice, J.; Reesor, E.; Zope, H.; Tao, W.; Lim, M.; Ding, J.; Chen, Y.; Aduluso, D.; Zetter, B.R.; et al. Adjuvant-pulsed mRNA vaccine nanoparticle for immunoprophylactic and therapeutic tumor suppression in mice. Biomaterials 2021, 266, 120431. [Google Scholar] [CrossRef]
- Cole, G.; Ali, A.A.; McErlean, E.; Mulholland, E.J.; Short, A.; McCrudden, C.M.; McCaffrey, J.; Robson, T.; Kett, V.L.; Coulter, J.A.; et al. DNA vaccination via RALA nanoparticles in a microneedle delivery system induces a potent immune response against the endogenous prostate cancer stem cell antigen. Acta Biomater. 2019, 96, 480–490. [Google Scholar] [CrossRef]
| Tumor Type | Nanoparticles | Use | References |
|---|---|---|---|
| Renal cell carcinoma | Sor-Mag-SLNs | Enhances drug delivery to tumors while reducing damage to normal tissues | [50] |
| Resveratrol nanoparticles | Inhibition of RCC cell migration and invasion through regulation of MMP2 expression and the ERK pathway | [51] | |
| HSA-AuNR-TKI | When irradiation is paired with gold particles and drug-loaded nanoparticles, the combined therapy showed the most significant and synergistic complete tumor necrosis of 100% (p < 0.05) | [52] | |
| TLR7/8 agonists encapsulated in PLGA nanoparticles | Trigger a robust antigen-specific immune response and are highly effective as vaccine adjuvants for cancer immunotherapy | [53] | |
| CA IX-C4.16 NPs | Combination of CA IX-C4.16 with Sor showed targeted delivery of payload in hypoxic tumors, resulting in induction of multimodal anticancer effects, including the resurrection of apoptosis, reversal of drug resistance, and reprogramming of malfunction macrophages. | [54] | |
| H1-pAIM2/pCAIX | Exhibits the therapeutic efficacy of anti-renal carcinoma by enhancing tumor-specific multi-functional CD8 T cell responses | [55] | |
| Urothelial carcinoma | Paclitaxel gelatin nanoparticles | Overcome the problem of drug dilution by newly produced urine and the sustained drug levels in tumors may decrease treatment frequency | [75] |
| HA/CHI nanoparticle-aggregated HET | HA nanoparticle aggregation reinforced the cytotoxic, antimigratory, and apoptosis-inducing activities against bladder carcinoma cells and attenuated the viability–inhibitory effects on normal fibroblasts. | [77] | |
| Cat-Alg NPs | These NPs have the potential to be a mucoadhesive drug delivery system for bladder cancer treatment | [78] | |
| Au@TNA NPs | Enhance the PDT-related cytotoxicity to cancer cells, but retain a very low dark toxicity to normal cells | [79] | |
| PLZ4 nanoparticles | Generate ROS and induce protein carbonylation and dendritic cell maturation | [80] | |
| AB680@EMVs-aPDL1 | Provided adequate biosafety, and enhanced tumor targeting in a mouse model of bladder cancer | [81] | |
| GNP-LLO91–99 | Reduced tumor burden 4.7-fold and stimulated systemic Th1-type immune responses | [82] | |
| Prostate cancer | CUR NPs | Restored CUR potency in both resistant DU145 and PC3 cells. | [110] |
| AgNPs-PLE | Causes cell cycle arrest and apoptosis in human prostate cancer cells | [111] | |
| RSV-SLN | As potential carriers for drug delivery of chemotherapeutics at an extended systemic circulation and targeting efficiency at the tumor site | [112] | |
| MGF-AuNPs | Polarized M2-type macrophages enhance the immune response | [113] | |
| PHB-PEI NPs | Excellent biocompatibility and high transfection efficiency for cancer therapy | [114] | |
| PTX/siRNA NPs-Apt | Enhanced tumor-targeting ability and achieved superior efficacy in the subcutaneous and orthotopic PCa tumor model with minimal side effects. | [115] | |
| DDA-SS-DMA based delivery system encapsulating shPKN3-2459 | High tumor suppression (65.8%) and treatment safety | [116] | |
| ICGNP | Enhance photothermal therapy | [117] | |
| mRNA vaccine NP | Increasing the tumor-associated antigen presentation, also promoting CD8 T cell recruitment into the tumor and enhancing the overall anti-tumor response | [118] | |
| RALA/pDNA NPs | Induced a tumor-specific cellular immune response, and inhibited the growth of TRAMP-C1 prostate tumors in both prophylactic and therapeutic challenge models in vivo | [119] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tian, Y.; Liu, Z.; Wang, J.; Li, L.; Wang, F.; Zhu, Z.; Wang, X. Nanomedicine for Combination Urologic Cancer Immunotherapy. Pharmaceutics 2023, 15, 546. https://doi.org/10.3390/pharmaceutics15020546
Tian Y, Liu Z, Wang J, Li L, Wang F, Zhu Z, Wang X. Nanomedicine for Combination Urologic Cancer Immunotherapy. Pharmaceutics. 2023; 15(2):546. https://doi.org/10.3390/pharmaceutics15020546
Chicago/Turabian StyleTian, Yun, Zhenzhu Liu, Jianbo Wang, Linan Li, Fuli Wang, Zheng Zhu, and Xuejian Wang. 2023. "Nanomedicine for Combination Urologic Cancer Immunotherapy" Pharmaceutics 15, no. 2: 546. https://doi.org/10.3390/pharmaceutics15020546
APA StyleTian, Y., Liu, Z., Wang, J., Li, L., Wang, F., Zhu, Z., & Wang, X. (2023). Nanomedicine for Combination Urologic Cancer Immunotherapy. Pharmaceutics, 15(2), 546. https://doi.org/10.3390/pharmaceutics15020546





