In Vivo Relevance of a Biphasic In Vitro Dissolution Test for the Immediate Release Tablet Formulations of Lamotrigine
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Single Phase In Vitro Dissolution Test
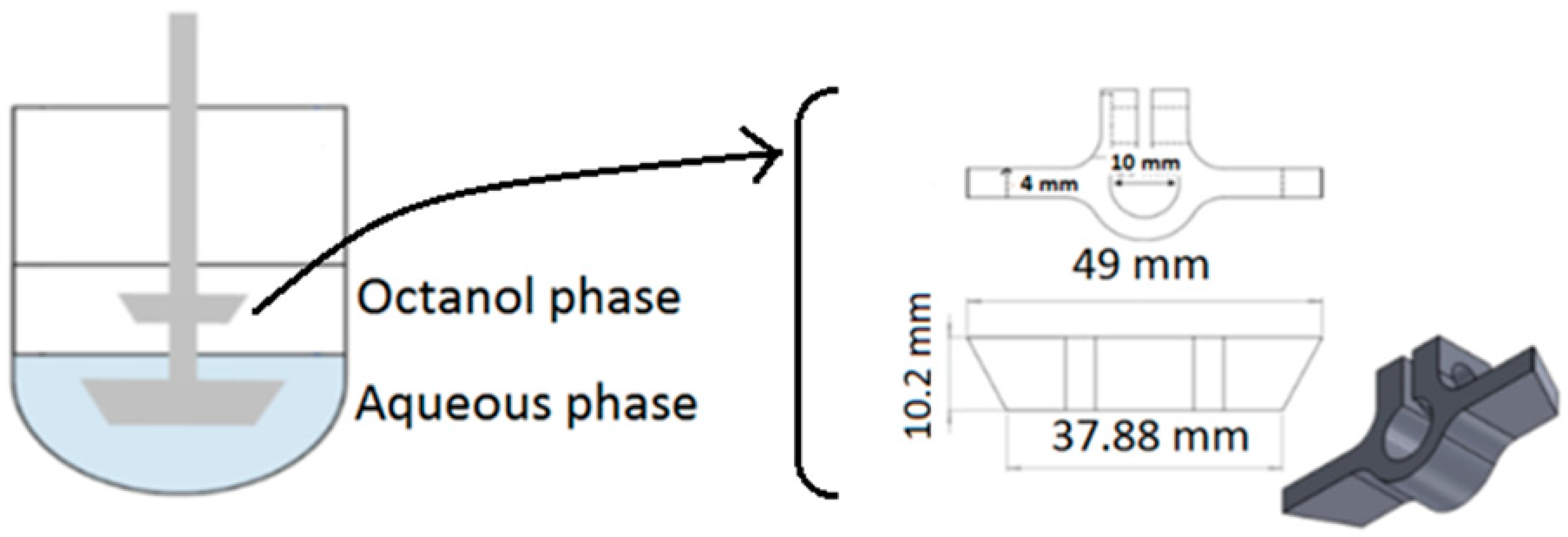
2.3. Biphasic In Vitro Dissolution Test
2.4. Assay
2.5. In Vitro Data Analysis
2.6. Prediction of In Vivo Plasma Profiles from the Correlation Between Absorption and In Vitro Partitioning Data
2.7. Bioequivalence (BE) Analysis
3. Results
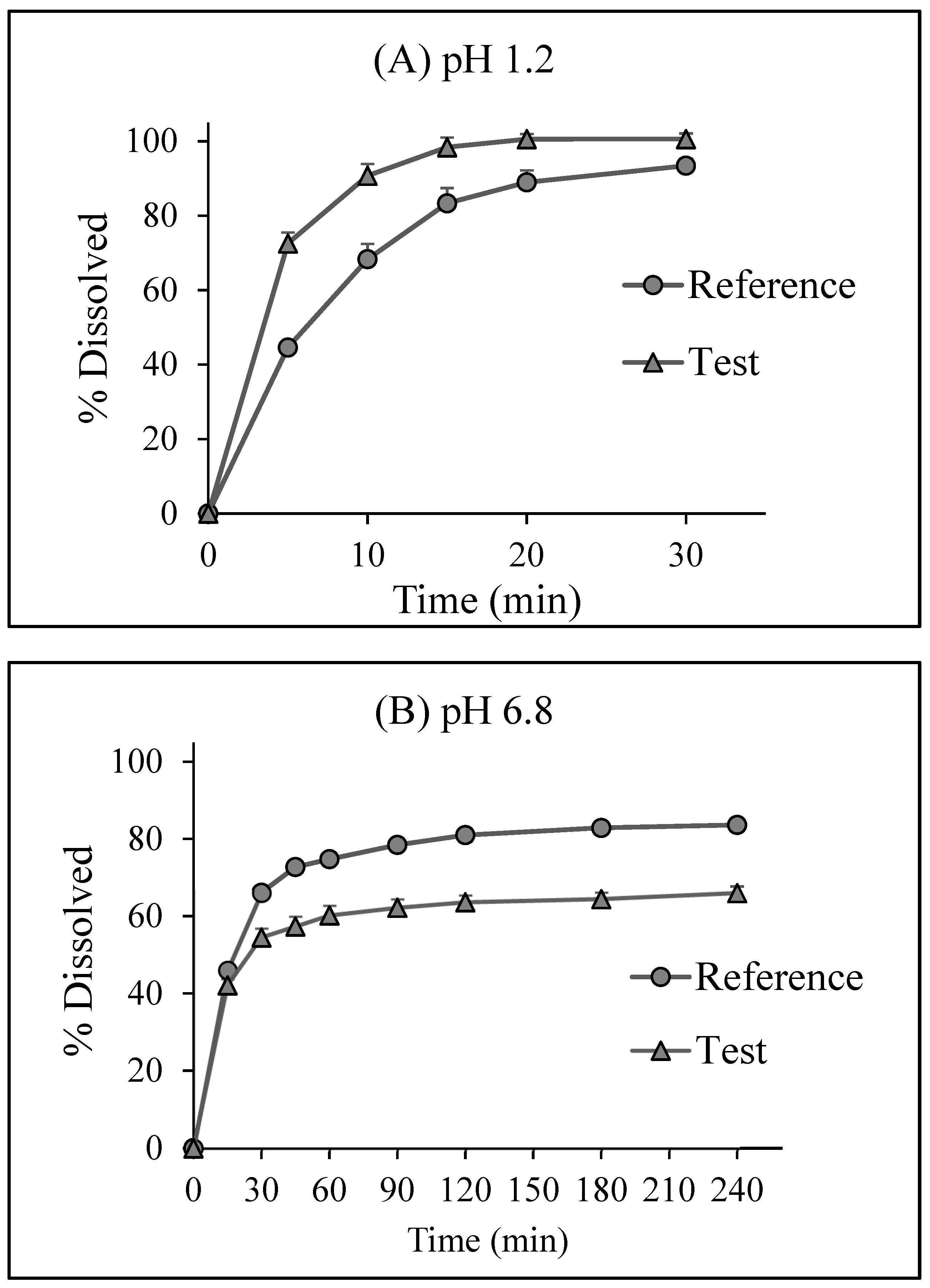
3.1. Single Phase In Vitro Dissolution Test
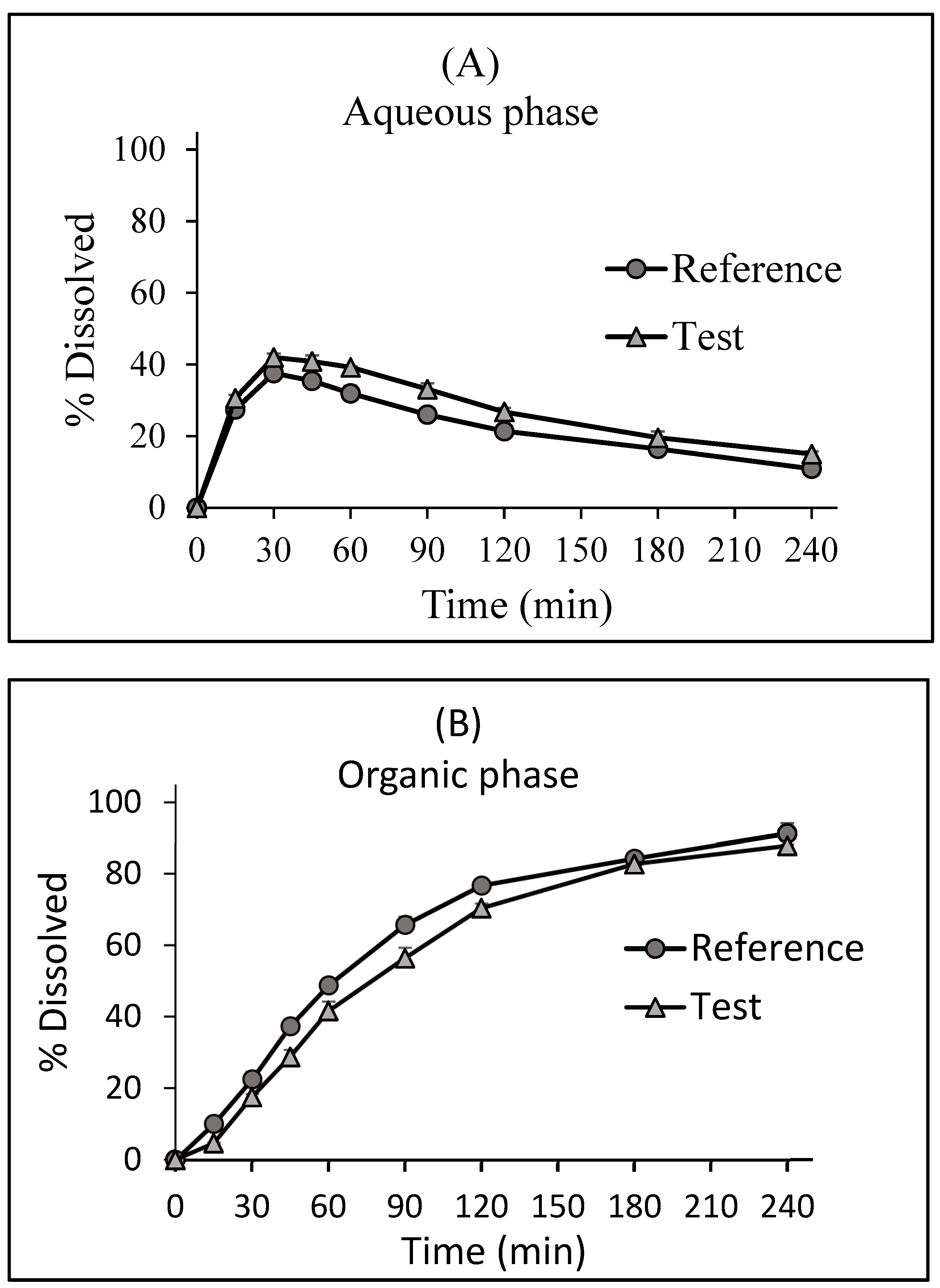
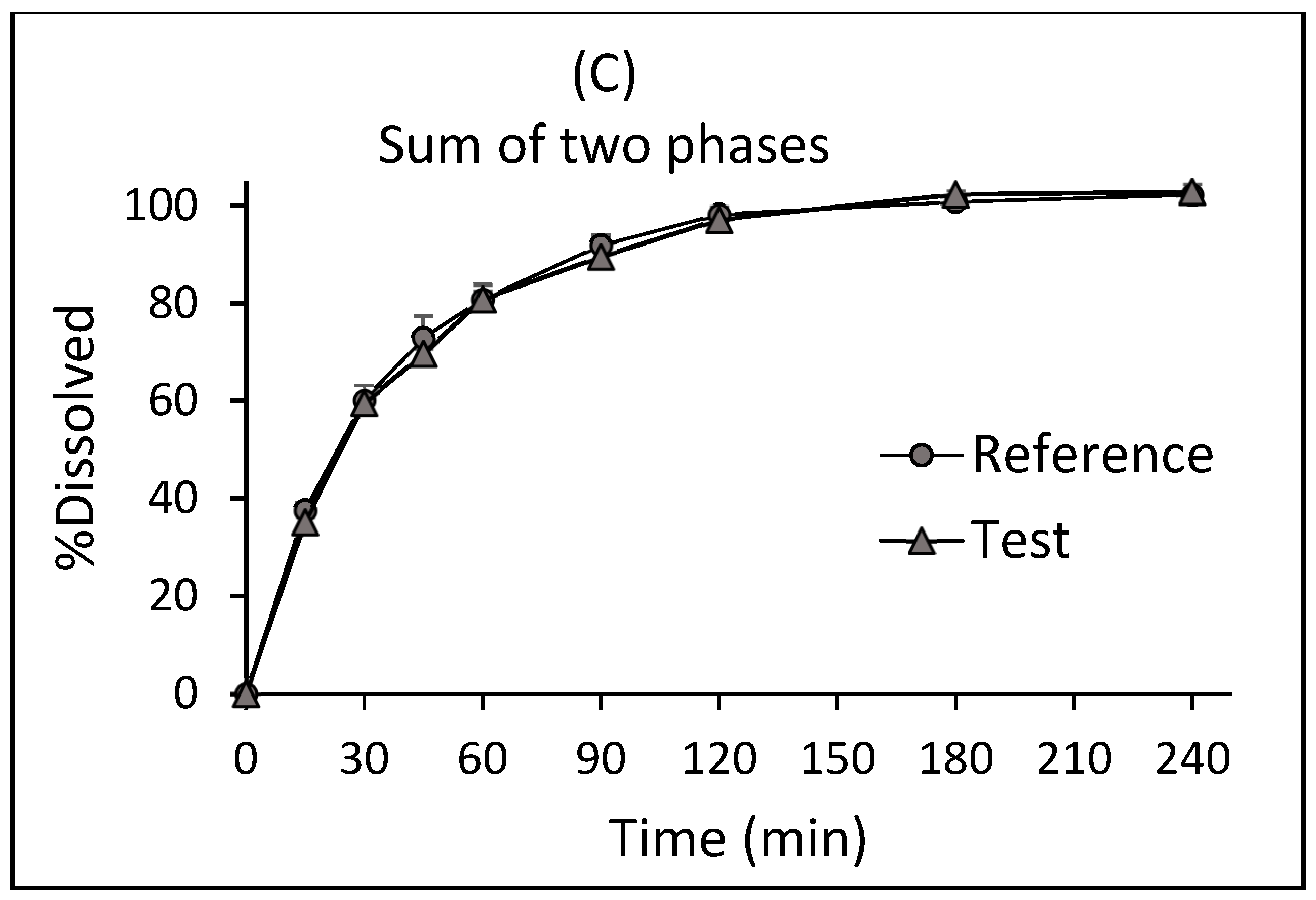
3.2. Biphasic In Vitro Dissolution Test
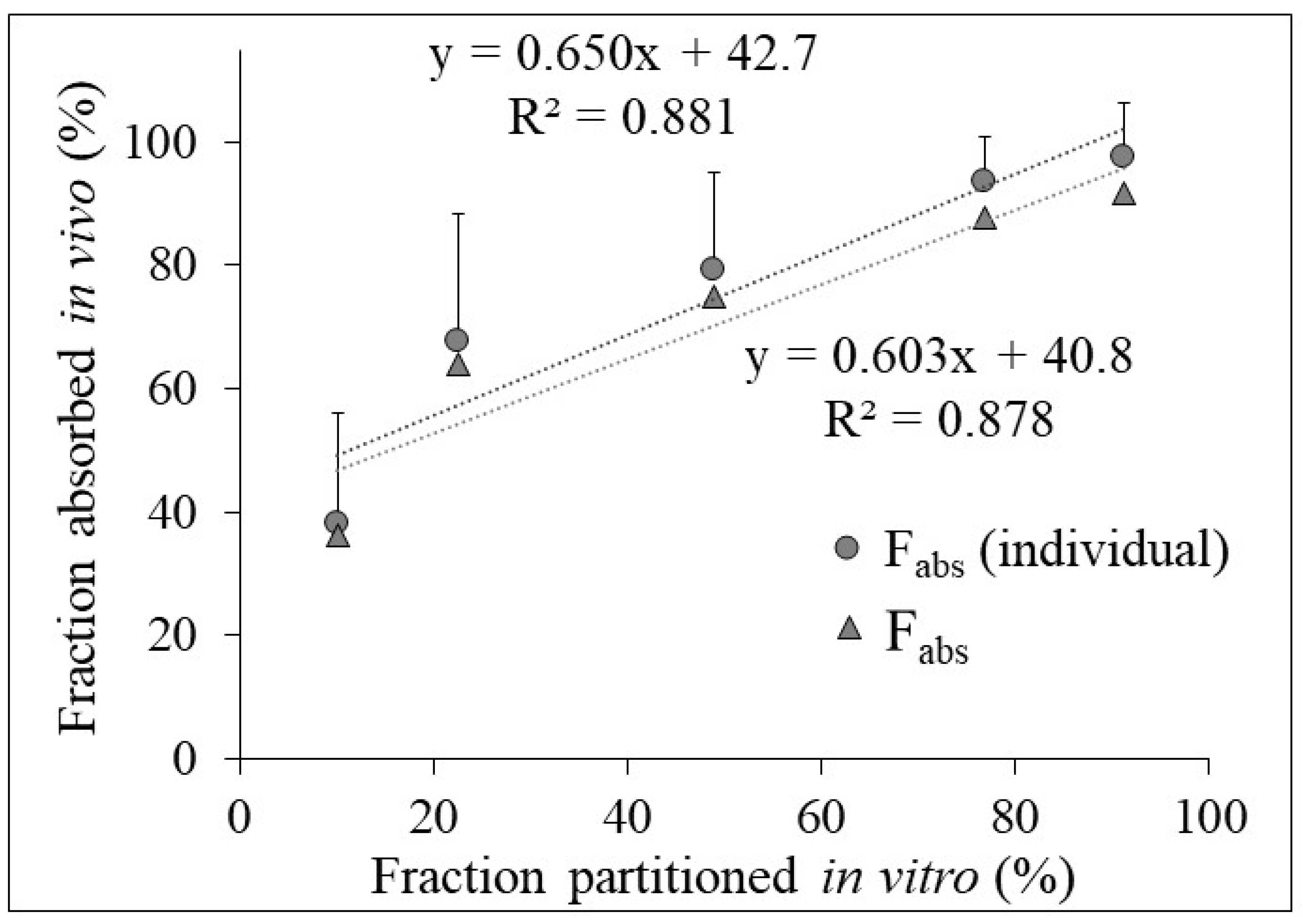
3.3. Relation between In Vivo Absorption and In Vitro Partitioning Data
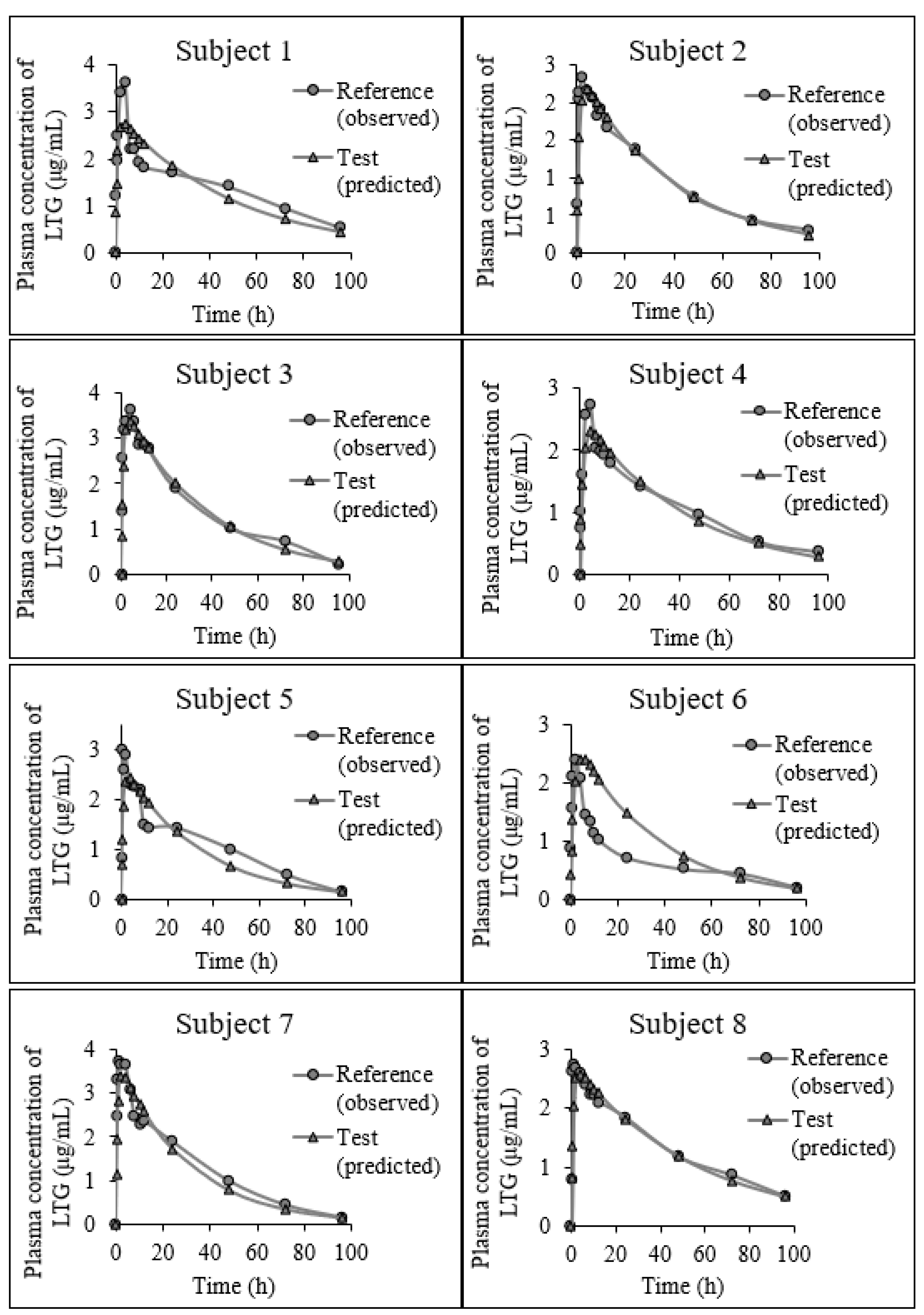
3.4. Prediction of In Vivo Plasma Profiles from the Biphasic In Vitro Data
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grady, H.; Elder, D.; Webster, G.K.; Mao, Y.; Lin, Y.; Flanagan, T.; Mann, J.; Blanchard, A.; Cohen, M.J.; Lin, J.; et al. Industry’s view on using quality control, biorelevant, and clinically relevant dissolution tests for pharmaceutical development, registration, and commercialization. J. Pharm. Sci. 2018, 107, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Galia, E.; Nicolaides, E.; Hörter, D.; Löbenberg, R.; Reppas, C.; Dressman, J.B. Evaluation of various dissolution media for predicting in vivo performance of class I and II drugs. Pharm. Res. 1998, 15, 698–705. [Google Scholar] [CrossRef] [PubMed]
- Klein, S. The use of biorelevant dissolution media to forecast the in vivo performance of a drug. AAPS J. 2010, 12, 397–406. [Google Scholar] [CrossRef]
- Lehto, P.; Kortejärvi, H.; Liimatainen, A.; Ojala, K.; Kangas, H.; Hirvonen, J.; Tanninen, V.P.; Peltonen, L. Use of conventional surfactant media as surrogates for FaSSIF in simulating in vivo dissolution of BCS class II drugs. Eur. J. Pharm. Biopharm. 2011, 78, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Matsui, K.; Tsume, Y.; Amidon, G.E.; Amidon, G.L. In vitro dissolution of fluconazole and dipyridamole in gastrointestinal simulator (GIS), predicting in vivo dissolution and drug-drug interaction caused by acid-reducing agents. Mol. Pharm. 2015, 12, 2418–2428. [Google Scholar] [CrossRef] [PubMed]
- Hens, B.; Sinko, P.D.; Job, N.; Dean, M.; Al-Gousous, J.; Salehi, N.; Ziff, R.M.; Tsume, Y.; Bermejo, M.; Paixão, P.; et al. Formulation predictive dissolution (fPD) testing to advance oral drug product development: An introduction to the US FDA funded ‘21st Century BA/BE’ project. Int. J. Pharm. 2018, 548, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.X.; Amidon, G.L.; Polli, J.E.; Zhao, H.; Mehta, M.U.; Conner, D.P.; Shah, V.P.; Lesko, L.J.; Chen, M.-L.; Lee, V.H.L.; et al. Biopharmaceutics classification system: The scientific basis for biowaiver extensions. Pharm. Res. 2002, 19, 921–925. [Google Scholar] [CrossRef]
- Hanif, M.; Shoaib, M.H.; Yousuf, R.I.; Zafar, F. Development of in vitro-in vivo correlations for newly optimized nimesulide formulations. PLoS ONE 2018, 13, e0203123. [Google Scholar] [CrossRef]
- Phillips, D.J.; Pygall, S.R.; Cooper, V.B.; Mann, J.C. Overcoming sink limitations in dissolution testing: A review of traditional methods and the potential utility of biphasic systems. J. Pharm. Pharmacol. 2012, 64, 1549–1559. [Google Scholar] [CrossRef]
- Xu, H.; Vela, S.; Shi, Y.; Marroum, P.; Gao, P. In vitro characterization of ritonavir drug products and correlation to human in vivo performance. Mol. Pharm. 2017, 14, 3801–3814. [Google Scholar] [CrossRef]
- Jede, C.; Henze, L.J.; Meiners, K.; Bogdahn, M.; Wedel, M.; van Axel, V. Development and application of a dissolution-transfer-partitioning system (DTPS) for biopharmaceutical drug characterization. Pharmaceutics 2023, 15, 1069. [Google Scholar] [CrossRef] [PubMed]
- Gabriëls, M.; Plaizier-Vercammen, J. Design of a dissolution system for the evaluation of the release rate characteristics of artemether and dihydroartemisinin from tablets. Int. J. Pharm. 2004, 274, 245–260. [Google Scholar] [CrossRef] [PubMed]
- Grundy, J.S.; Anderson, K.E.; Rogers, J.A.; Foster, R.T. Studies on dissolution testing of the nifedipine gastrointestinal therapeutic system. I. Description of a two-phase in vitro dissolution test. J. Control. Release 1997, 48, 1–8. [Google Scholar] [CrossRef]
- Heigoldt, U.; Sommer, F.; Daniels, R.; Wagner, K.-G. Predicting in vivo absorption behavior of oral modified release dosage forms containing pH-dependent poorly soluble drugs using a novel pH-adjusted biphasic in vitro dissolution test. Eur. J. Pharm. Biopharm. 2010, 76, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Niebergall, P.J.; Patil, M.Y.; Sugita, E.T. Simultaneous determination of dissolution and partitioning rates in vitro. J. Pharm. Sci. 1967, 56, 943–947. [Google Scholar] [CrossRef] [PubMed]
- Gibaldi, M.; Feldman, S. Establishment of sink conditions in dissolution rate determinations. Theoretical considerations and application to nondisintegrating dosage forms. J. Pharm. Sci. 1967, 56, 1238–1242. [Google Scholar] [CrossRef]
- Stead, J.A.; Freeman, M.; John, E.G.; Ward, G.T.; Whiting, B. Ibuprofen tablets: Dissolution and bioavailability studies. Int. J. Pharm. 1983, 14, 59–72. [Google Scholar] [CrossRef]
- Chaudhary, R.S.; Gangwal, S.S.; Gupta, V.K.; Shah, Y.N.; Jindal, K.C.; Khanna, S. Dissolution system for nifedipine sustained release formulations. Drug Dev. Ind. Pharm. 1994, 20, 1267–1274. [Google Scholar] [CrossRef]
- Vangani, S.; Li, X.; Zhou, P.; Del-Barrio, M.-A.; Chiu, R.; Cauchon, N.; Gao, P.; Medina, C.; Jasti, B. Dissolution of poorly water-soluble drugs in biphasic media using USP 4 and fiber optic system. Clin. Res. Regul. Aff. 2009, 26, 8–19. [Google Scholar] [CrossRef]
- Frank, K.J.; Locher, K.; Zecevic, D.E.; Fleth, J.; Wagner, K.G. In vivo predictive mini-scale dissolution for weak bases: Advantages of pH-shift in combination with an absorptive compartment. Eur. J. Pharm. Sci. 2014, 61, 32–39. [Google Scholar] [CrossRef]
- Locher, K.; Borghardt, J.M.; Frank, K.J.; Kloft, C.; Wagner, K.G. Evolution of a mini-scale biphasic dissolution model: Impact of model parameters on partitioning of dissolved API and modelling of in vivo-relevant kinetics. Eur. J. Pharm. Biopharm. 2016, 105, 166–175. [Google Scholar] [CrossRef] [PubMed]
- O’Dwyer, P.J.; Box, K.J.; Imanidis, G.; Vertzoni, M.; Reppas, C. On the usefulness of four in vitro methods in assessing the intraluminal performance of poorly soluble, ionisable compounds in the fasted state. Eur. J. Pharm. Sci. 2022, 168, 106034. [Google Scholar] [CrossRef]
- Grassi, M.; Coceani, N.; Magarotto, L. Modelling partitioning of sparingly soluble drugs in a two-phase liquid system. Int. J. Pharm. 2002, 239, 157–169. [Google Scholar] [CrossRef] [PubMed]
- Mudie, D.M.; Shi, Y.; Ping, H.; Gao, P.; Amidon, G.L.; Amidon, G.E. Mechanistic analysis of solute transport in an in vitro physiological two-phase dissolution apparatus. Biopharm. Drug Dispos. 2012, 33, 378–402. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Mochizuki, M.; Itoh, T.; Ohta, M. Studies on dissolution tests for soft gelatin capsules. IV. Dissolution test of nifedipine soft gelatin capsule containing water soluble vehicles by the rotating dialysis cell method. Chem. Pharm. Bull. 1994, 42, 333–336. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hoa, N.T.; Kinget, R. Design and evaluation of two-phase partition–dissolution method and its use in evaluating artemisinin tablets. J. Pharm. Sci. 1996, 85, 1060–1063. [Google Scholar] [CrossRef] [PubMed]
- Pillay, V.; Fassihi, R. A new method for dissolution studies of lipid-filled capsules employing nifedipine as a model drug. Pharm. Res. 1999, 16, 333–337. [Google Scholar] [CrossRef]
- Shi, Y.; Gao, P.; Gong, Y.; Ping, H. Application of a biphasic test for characterization of in vitro drug release of immediate release formulations of celecoxib and its relevance to in vivo absorption. Mol. Pharm. 2010, 7, 1458–1465. [Google Scholar] [CrossRef]
- Yukuyama, M.N.; Zuo, J.; Park, C.; Yousef, M.; Henostroza, M.A.B.; de Araujo, G.L.B.; Bou-Chacra, N.A.; Löbenberg, R. Biphasic dissolution combined with modified cylinder method-A new promising method for dissolution test in drug-loaded nanoemulsions. Int. J. Pharm. 2023, 632, 122554. [Google Scholar] [CrossRef]
- Pestieau, A.; Krier, F.; Lebrun, P.; Brouwers, A.; Streel, B.; Evrard, B. Optimization of a PGSS (particles from gas saturated solutions) process for a fenofibrate lipid-based solid dispersion formulation. Int. J. Pharm. 2015, 485, 295–305. [Google Scholar] [CrossRef]
- Denninger, A.; Becker, T.; Westedt, U.; Wagner, K.G. Advanced in vivo prediction by introducing biphasic dissolution data into PBPK models. Pharmaceutics 2023, 15, 1978. [Google Scholar] [CrossRef] [PubMed]
- Fitton, A.; Goa, K.L. Lamotrigine. An update of its pharmacology and therapeutic use in epilepsy. Drugs 1995, 50, 691–713. [Google Scholar] [CrossRef] [PubMed]
- Rambeck, B.; Wolf, P. Lamotrigine clinical pharmacokinetics. Clin. Pharmacokinet. 1993, 25, 433–443. [Google Scholar] [CrossRef]
- Vaithianathan, S.; Raman, S.; Jiang, W.; Ting, T.Y.; Kane, M.A.; Polli, J.E.; Raman, S.; Jiang, W.; Ting, T.Y.; Kane, M.A.; et al. Biopharmaceutic risk assessment of brand and generic lamotrigine tablets. Mol. Pharm. 2015, 12, 2436–2443. [Google Scholar] [CrossRef] [PubMed]
- Goa, K.L.; Ross, S.R.; Chrisp, P. Lamotrigine: A review of its pharmacological properties and clinical efficacy in epilepsy. Drugs 1993, 46, 152–176. [Google Scholar] [CrossRef]
- Cohen, A.F.; Land, G.S.; Breimer, D.D.; Yuen, W.C.; Winton, C.; Peck, A.W. Lamotrigine, a new anticonvulsant: Pharmacokinetics in normal humans. Clin. Pharmacol. Ther. 1987, 42, 535–541. [Google Scholar] [CrossRef]
- Incecayir, T.; Agabeyoglu, I.; Gucuyener, K. Comparison of plasma and saliva concentrations of lamotrigine in healthy volunteers. Arzneimittelforschung 2007, 57, 517–521. [Google Scholar] [CrossRef]
- Amidon, G.L.; Lennernäs, H.; Shah, V.P.; Crison, J.R. A theoretical basis for a biopharmaceutic drug classification: The correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm. Res. 1995, 12, 413–420. [Google Scholar] [CrossRef]
- United States Food and Drug Administration, Department of Health and Human Services, Center for Drug Evaluation and Research (CDER). Dissolution Testing of Immediate Release Solid Oral Dosage Forms, Guidance for Industry; U.S. Government Printing Office: Washington, DC, USA, 1997.
- Wagner, J.G. Estimation of theophylline absorption rate by means of the Wagner-Nelson equation. J. Allergy Clin. Immunol. 1986, 78, 681–688. [Google Scholar] [CrossRef]
- United States Food and Drug Administration. Dissolution Methods for Lamotrigine. 2008. Available online: https://www.accessdata.fda.gov/scripts/cder/dissolution/dsp_SearchResults.cfm (accessed on 15 August 2023).
- The United States Pharmacopeial Convention. General Chapter <1092> The Dissolution Procedure: Development and Vali-dation. In United States Pharmacopoeia and National Formulary-USP 44-NF 39; The United States Pharmacopeial Convention: North Bethesda, MD, USA, 2021; p. 4/23.
- United States Food and Drug Administration. Approved Label Text. 2015. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/020241s045s051lbl.pdf (accessed on 15 August 2023).
- The Metabolomics Innovation Centre. The Toxin and Toxin Target Database (T3DB). Lamotrigine. 2014. Available online: http://www.t3db.ca/toxins/T3D2570 (accessed on 15 August 2023).
- Malan, S.F.; Chetty, D.J.; du Plessis, J. Physicochemical properties of drugs and membrane permeability. S. Afr. J. Sci. 2002, 98, 385–391. Available online: https://hdl.handle.net/10520/EJC97511 (accessed on 11 October 2023).
- Btaiche, I.F.; Woster, P.S. Gabapentin and lamotrigine: Novel antiepileptic drugs. Am. J. Health-Syst. Pharm. 1995, 52, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Dressman, J.B.; Amidon, G.L.; Reppas, C.; Shah, V.P. Dissolution testing as a prognostic tool for oral drug absorption: Immediate release dosage forms. Pharm. Res. 1998, 15, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Bevernage, J.; Brouwers, J.; Brewster, M.E.; Augustijns, P. Evaluation of gastrointestinal drug supersaturation and precipitation: Strategies and issues. Int. J. Pharm. 2013, 453, 25–35. [Google Scholar] [CrossRef]
- Incecayir, T. The effects of surfactants on the solubility and dissolution profiles of a poorly water-soluble basic drug, carvedilol. Pharmazie 2015, 70, 784–790. Available online: https://pubmed.ncbi.nlm.nih.gov/26817275/ (accessed on 11 October 2023). [PubMed]
- Franc, A.; Muselík, J.; Goněc, R.; Vetchý, D. Biphasic dissolution method for quality control and assurance of drugs containing active substances in the form of weak acid salts. Acta Pharm. 2016, 66, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Staufenbiel, S.; Hao, S.; Wang, B.; Dashevskiy, A.; Bodmeier, R. Development of a discriminative biphasic in vitro dissolution test and correlation with in vivo pharmacokinetic studies for differently formulated racecadotril granules. J. Control. Rel. 2017, 255, 202–209. [Google Scholar] [CrossRef]
- Silva, D.A.; Al-Gousous, J.; Davies, N.M.; Chacra, N.B.; Webster, G.K.; Lipka, E.; Amidon, G.L.; Löbenberg, R. Biphasic dissolution as an exploratory method during early drug product development. Pharmaceutics 2020, 12, 420. [Google Scholar] [CrossRef]
- Rothwell, J.A.; Day, A.J.; Morgan, M.R.A. Experimental determination of octanol−water partition coefficients of quercetin and related flavonoids. J. Agric. Food Chem. 2005, 53, 4355–4360. [Google Scholar] [CrossRef]
- Al Durdunji, A.; AlKhatib, H.S.; Al-Ghazawi, M. Development of a biphasic dissolution test for deferasirox dispersible tablets and its application in establishing an in vitro-in vivo correlation. Eur. J. Pharm. Biopharm. 2016, 102, 9–18. [Google Scholar] [CrossRef]
- Xu, H.; Shi, Y.; Vela, S.; Marroum, P.; Gao, P. Developing quantitative in vitro-in vivo correlation for fenofibrate immediate-release formulations with the biphasic dissolution-partition test method. J. Pharm. Sci. 2018, 107, 476–487. [Google Scholar] [CrossRef]
- Denninger, A.; Westedt, U.; Rosenberg, J.; Wagner, K.G. A rational design of a biphasic dissolution setup-modelling of biorelevant kinetics for a ritonavir hot-melt extruded amorphous solid dispersion. Pharmaceutics 2020, 12, 237. [Google Scholar] [CrossRef] [PubMed]
- Koziolek, M.; Grimm, M.; Becker, D.; Iordanov, V.; Zou, H.; Shimizu, J.; Wanke, C.; Garbacz, G.; Weitschies, W. Investigation of pH and temperature profiles in the GI tract of fasted human subjects using the Intellicap® system. J. Pharm. Sci. 2015, 104, 2855–2863. [Google Scholar] [CrossRef] [PubMed]
- Denninger, A.; Westedt, U.; Wagner, K.G. Shared IVIVR for five commercial enabling formulations using the BiPHa+ biphasic dissolution assay. Pharmaceutics 2021, 13, 285. [Google Scholar] [CrossRef] [PubMed]


| Medium | CS 1 (mg/mL) | CS/CD 2 | DO 3 |
|---|---|---|---|
| pH 1.2 hydrochloric acid | 3.63 ± 0.01 | 16.3 | 0.22 |
| pH 6.8 phosphate buffer | 0.136 ± 0.001 | 0.611 | 5.9 |
| Test | Reference | ||||
|---|---|---|---|---|---|
| BA Criteria | Mean ± SD 1 | CV% 2 | Mean ± SD | CV% | BE Limits for 90 % CI 3 |
| AUC (µg/mL.h) 4 | 119 ± 24.9 | 21.0 | 123 ± 14.3 * | 11.6 | 85.9–107 |
| Cmax (µg/mL) 5 | 2.61 ± 0.39 | 15.1 | 2.90 ± 0.26 * | 8.96 | 82.7–97.6 |
| tmax (h) 6 | 3.7 ± 1.1 | 28.8 | 2.4 ± 0.7 * | 29.2 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Incecayir, T.; Demir, M.E. In Vivo Relevance of a Biphasic In Vitro Dissolution Test for the Immediate Release Tablet Formulations of Lamotrigine. Pharmaceutics 2023, 15, 2474. https://doi.org/10.3390/pharmaceutics15102474
Incecayir T, Demir ME. In Vivo Relevance of a Biphasic In Vitro Dissolution Test for the Immediate Release Tablet Formulations of Lamotrigine. Pharmaceutics. 2023; 15(10):2474. https://doi.org/10.3390/pharmaceutics15102474
Chicago/Turabian StyleIncecayir, Tuba, and Muhammed Enes Demir. 2023. "In Vivo Relevance of a Biphasic In Vitro Dissolution Test for the Immediate Release Tablet Formulations of Lamotrigine" Pharmaceutics 15, no. 10: 2474. https://doi.org/10.3390/pharmaceutics15102474
APA StyleIncecayir, T., & Demir, M. E. (2023). In Vivo Relevance of a Biphasic In Vitro Dissolution Test for the Immediate Release Tablet Formulations of Lamotrigine. Pharmaceutics, 15(10), 2474. https://doi.org/10.3390/pharmaceutics15102474







