1. Introduction
The development of pharmaceutical carriers has been one of the essential objectives of nanomedicine. Nanocarriers provide more efficient and less toxic treatments with cytotoxic drugs, diagnostic imaging through radionuclides or contrast agents, and the monitoring of diseases [
1,
2]. One of the most used nanocarriers is lipid-based nanosystems, such as liposomes; these particles have relevant advantages as drug delivery systems, for example, drug protection against enzymatic degradation, low toxicity, increased permeability, biocompatibility, and low immunogenicity [
2,
3]. However, some of these advantages are limited because of the low encapsulation efficiency of drugs with poor aqueous solubility.
The development of nanocarriers to transport low-solubility drugs is relevant because many drug candidates or diagnostic agents are lipophilic with poor solubility in water [
3]. The therapeutic applications of hydrophobic drugs are associated with minimal absorption and low bioavailability; in addition, the aggregation of these drugs on intravenous administration causes problems of embolism and local toxicity [
4]. On the other hand, low solubility is also an intrinsic property of many lipophilic drugs, which helps the molecule or drug penetrate the cell membrane and achieve important intracellular targets. Different micelles-forming surfactants, colloidal dispersions with a particle size of 5 to 100 nm, have been used to overcome the low solubility of certain drugs. An essential property of micelles is their ability to increase the solubility and bioavailability of poorly soluble or insoluble drugs [
2,
5].
In the present study, we describe a new system named lipomics, potentially carrying both lipophilic and hydrophilic drugs. Lipomic are lipid nanostructures composed of a mixture of phospholipids, which under specific physicochemical conditions, form a nucleus of mixed micelles (phospholipid monomers and surfactants) surrounded by a bilayer of phospholipids (a liposome membrane), which can transport hydrophilic drugs in the aqueous space of the core and lipophilic drugs within the micelles [
6].
In the manufacturing of lipomics, Taguchi’s experimental design was used to identify controllable parameters that minimize variations that could affect the method’s reproducibility. Pseudo-ternary phase diagrams were used to determine the proportion of the excipients needed to obtain the best lipomic formulation. Physicochemical techniques to determine particle size, zeta potential, morphology, and in vitro stability properties were implemented. For the in vivo biodistribution, pharmacokinetic studies of 99mTc-lipomics were performed by plasma sampling quantification and molecular imaging with a microSPECT/CT system at different times. Radiolabeling efficiency was used to compare the encapsulation efficiency of hydrophilic and lipophilic molecules in lipomics and liposomes.
3. Discussion
From a previous work [
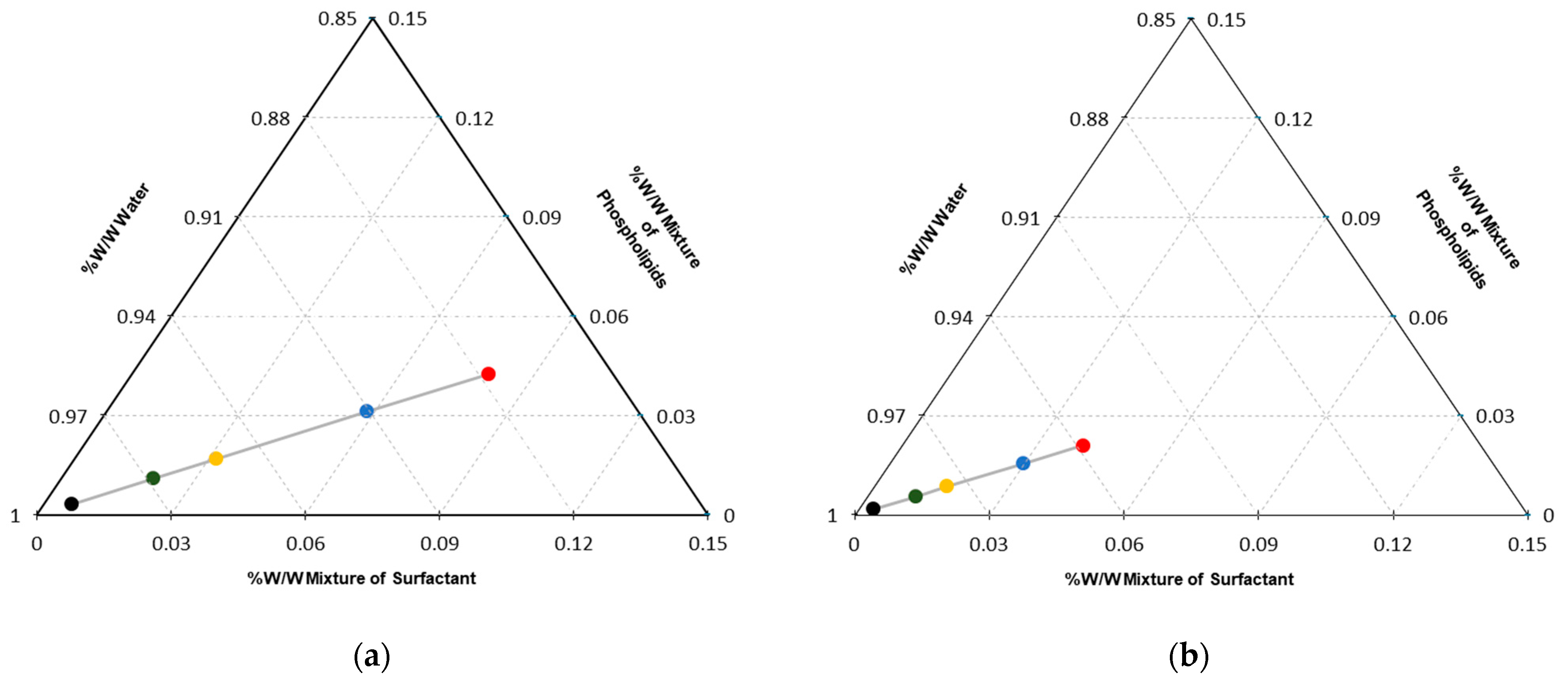
6], it was suggested that using a unique combination of physicochemical parameters, based on pseudo-ternary phase diagrams, and experimental conditions, using Taguchi’s design, lipomics can be formed reproducibly.
The Taguchi method optimizes experimental parameters to minimize variation before optimizing the design to hit target values for output parameters. The method uses unique orthogonal arrays to study all the design factors with a minimum number of experiments [
12]. Pseudo-ternary diagrams are widely used because they make it easier to understand the behavior of a system in equilibrium and determine the compositions of the phases and relative quantities of each of them [
13]. In this work, the ternary diagrams allowed us to define the trajectory points that resulted in systems with the potential for use as carriers of lipophilic and hydrophilic drugs. Each diagram contains specific points placed from the concentrations of each of the components in the system, defining zones where the concentrations of the excipients tend to behave in a specific way. Then, it was possible to define the regions of interest where it was very likely to find systems with defined characteristics (i.e., size and morphology).
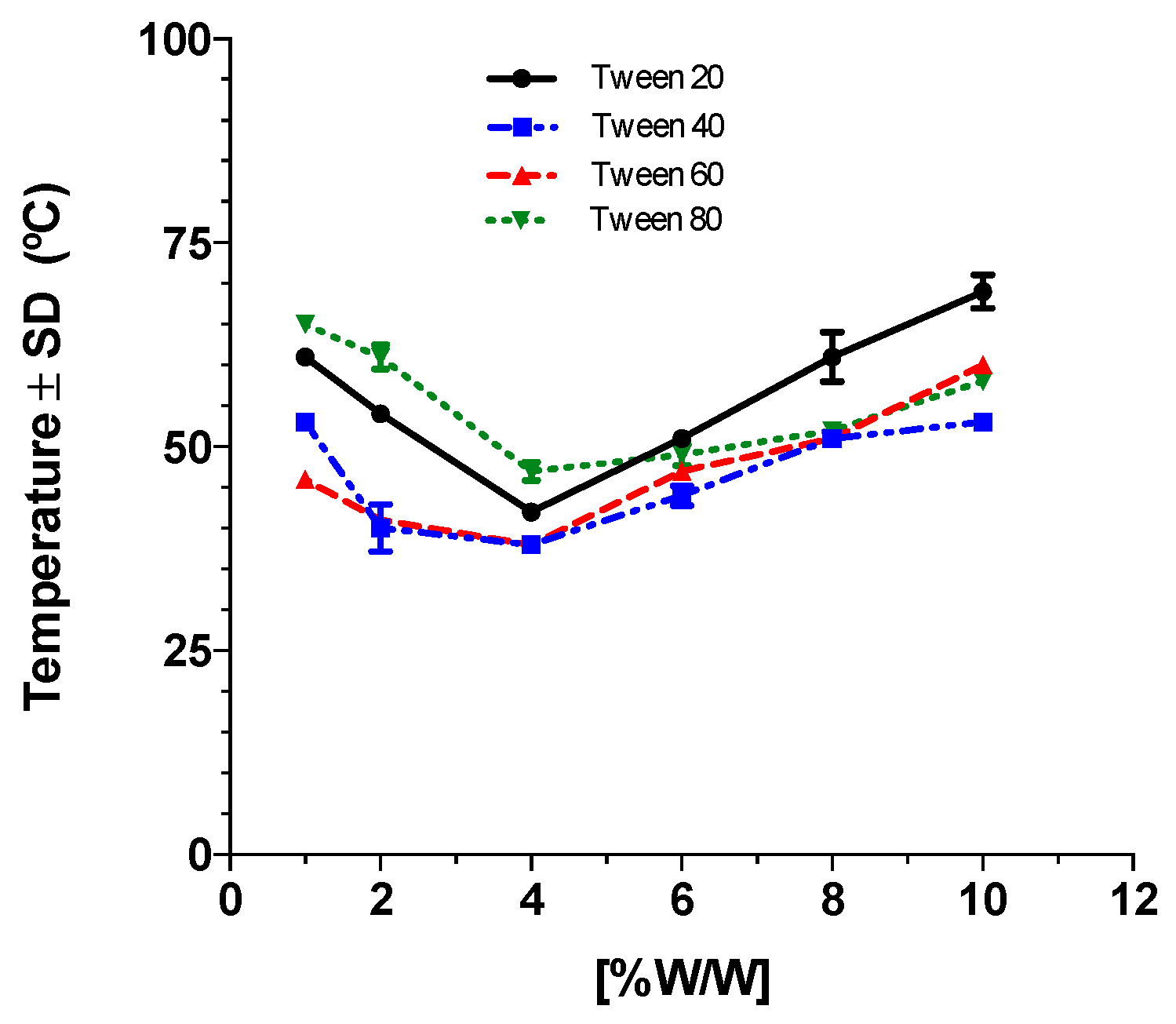
The surfactant’s cloud point (Cp) is an essential parameter in lipomic formation. When a surfactant reaches the Cp temperature, it forms a micellar network encapsulated by a lipid double bilayer of the phospholipids in the medium when the lipomic is assembled. The Cp mainly depends on surfactant concentration, its chemical structure (the extension of the carbon chain), and the concentration of ions in the medium. The surfactant concentration is directly related to the critical micellar concentration (CMC). By increasing the temperature, the CMC is increased, causing the formation of micelles. The non-ionic surfactants used in this work belonged to the family of ethoxylated surfactants; when the ethylene oxide units (hydrophilic portion) were increased and the carbon chain remained constant, the Cp increased. In contrast, by increasing the length of the carbon chain, the Cp decreased [
14]. In this study, both concentrations and types of surfactants were modified, keeping the concentration of ions in the medium constant. Our analysis of Cp with the different surfactants determined the selection of Tween 80 for the elaboration of lipomics, considering that a homogeneous solution of surfactant with a high cloud point presents better stability.
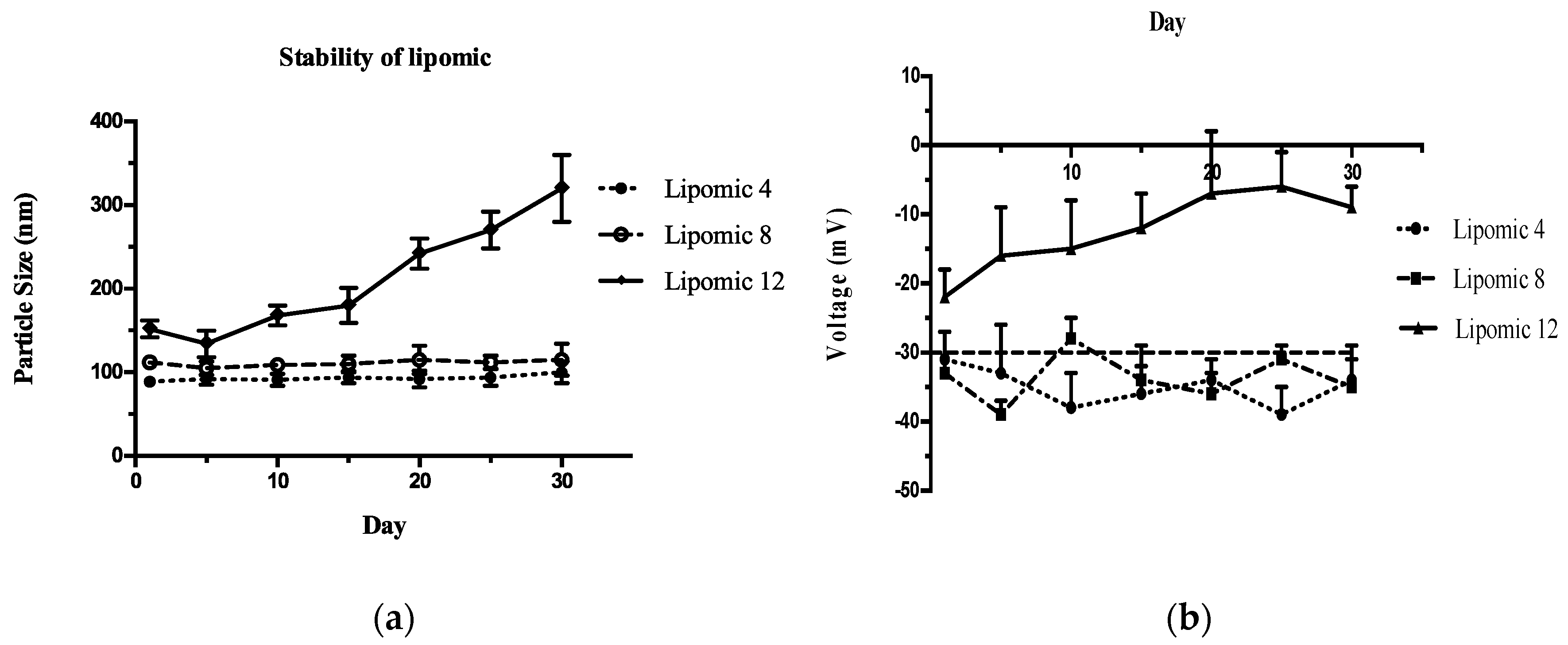
Colloidal systems, such as liposomes and lipomics, are considered thermodynamically unstable. The physical stability of these systems depends on several factors: temperature, stress during transport inside the organism, compatibility of excipients, particle size, and the Zeta potential of the system [
15]. A colloidal system ceases to be considered stable when the separation of its phases is irreversible; the most stable systems are those where the forces of repulsion predominate among the suspended particles, thus avoiding the coalescence and flocculation of the particles [
16,
17]. The physicochemical evaluation studies implemented in this work indicated that formulations 8 and 4 showed the best stability for 30 days (
Figure 2). It was considered that the electrostatic forces between the particles did not suffer from alterations because in none of the systems was an increase in particle size greater than 150 nm observed, and the Z potential was maintained at around −30 mV. Therefore, the particles’ agglomeration, fusion, coalescence, and precipitation were avoided.
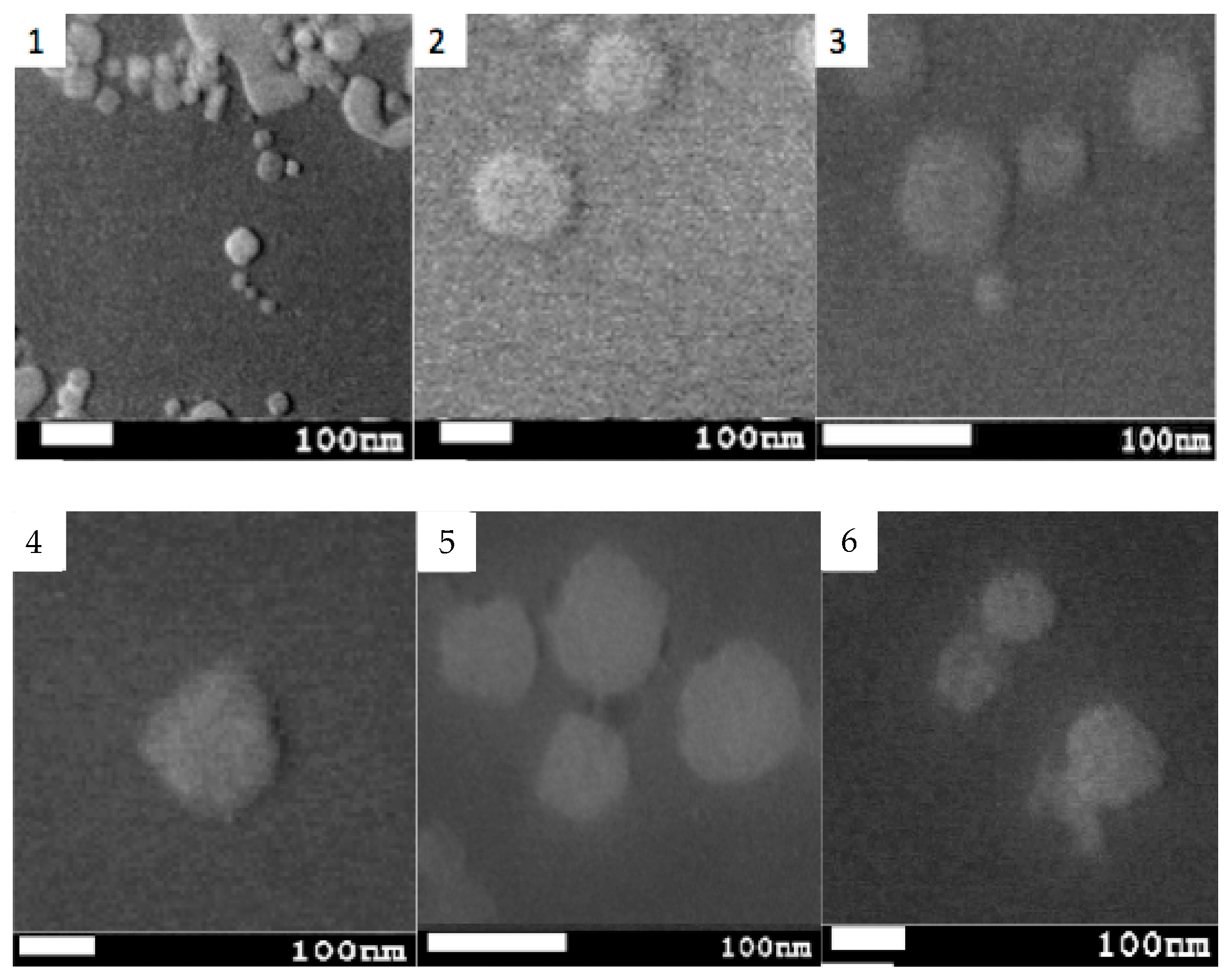
The shape and size of nanoparticles greatly influence their biodistribution and elimination from the organism [
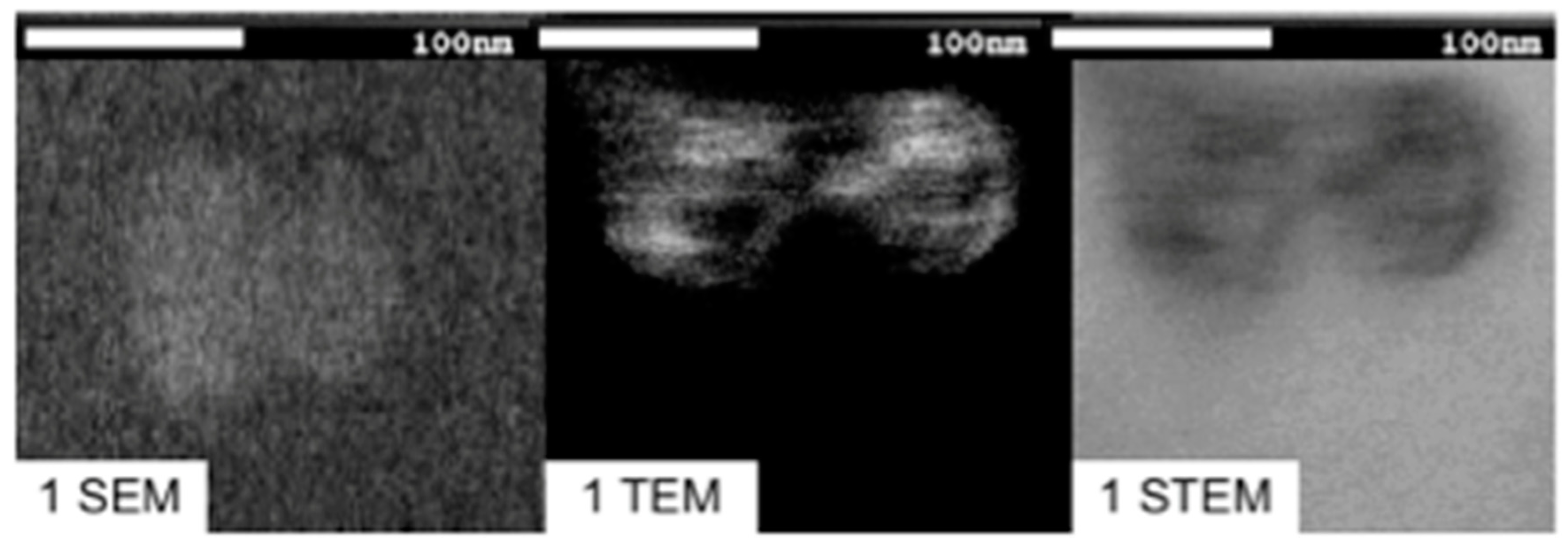
18]. Using SEM microscopy, it was possible to obtain images that allowed for the evaluation of these properties [
19]. Spherical geometry and particle sizes around 100–200 nm are qualities that allow low detection rates by the immune system and, theoretically, a prolonged circulation time in the body [
20]. With TEM/STEM microscopy, we sought to evaluate the internal structure of lipomics. Including a hydrophilic contrast medium in lipomics, such as uranyl acetate, highlights the hydrophilic regions inside. The electrons impinging on the uranyl acetate molecule are stopped, translating the image into regions with greater contrast and hydrophilic characteristics [
21].
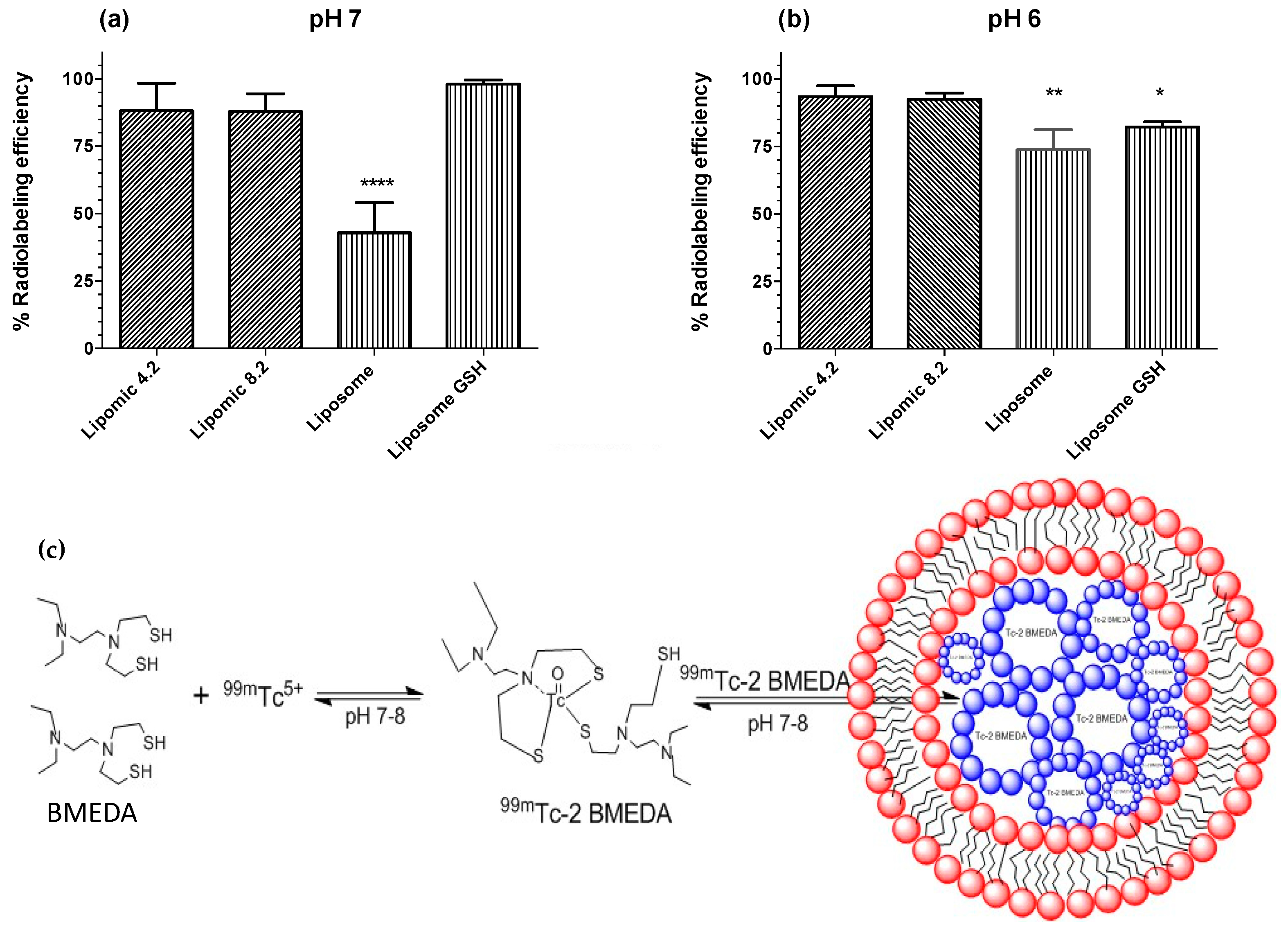
A second stage in this work was the radiolabeling process, reducing
99mTcO
4− with SnCl
2, which formed a stable octahedral complex [
22]. The
99mTc–2BMEDA complex has a complexation pattern “SNS/S” (
Figure 6c) that is the nucleus of technetium attached on the one hand to two atoms of sulfur and one of nitrogen, and is also attached to another atom of sulfur belonging to a second molecule of BMEDA [
23]. The result of the process produces a complex with a hydrophobic or hydrophilic character dependent on pH [
24]. Radiolabeling procedures also allowed us to obtain information about the structure of lipomics, considering that a hydrophilic chelator will find it more challenging to cross the lipid bilayer without the help of a concentration gradient or carrier. When performing the experiments with a concentration gradient of glucoheptonate, it was observed that the radiolabeling efficiency of hydrophilic molecules for liposomes was above 85% (
Figure 6a), observing a better efficiency in lipomics. This result suggests the presence of hydrophilic compartments within the lipomics. When the same chelator was modified to a pH 7–8, it acquired lipophilic properties, facilitating its passage through the lipid bilayer. In these conditions, lipomics and liposomes did not show statistically significant differences, since both systems could carry more than 90% of the
99mTc inside (
Figure 6b). For lipomics, once the lipophilic complex of technetium entered through the lipid bilayer, the aqueous molecules inside drove the lipophilic molecules into the micelles, where they were trapped (
Figure 6c). On the other hand, liposomes did not achieve an uptake greater than 50% in lipophilic conditions due to the repulsion of the lipophilic complex through its aqueous interior (
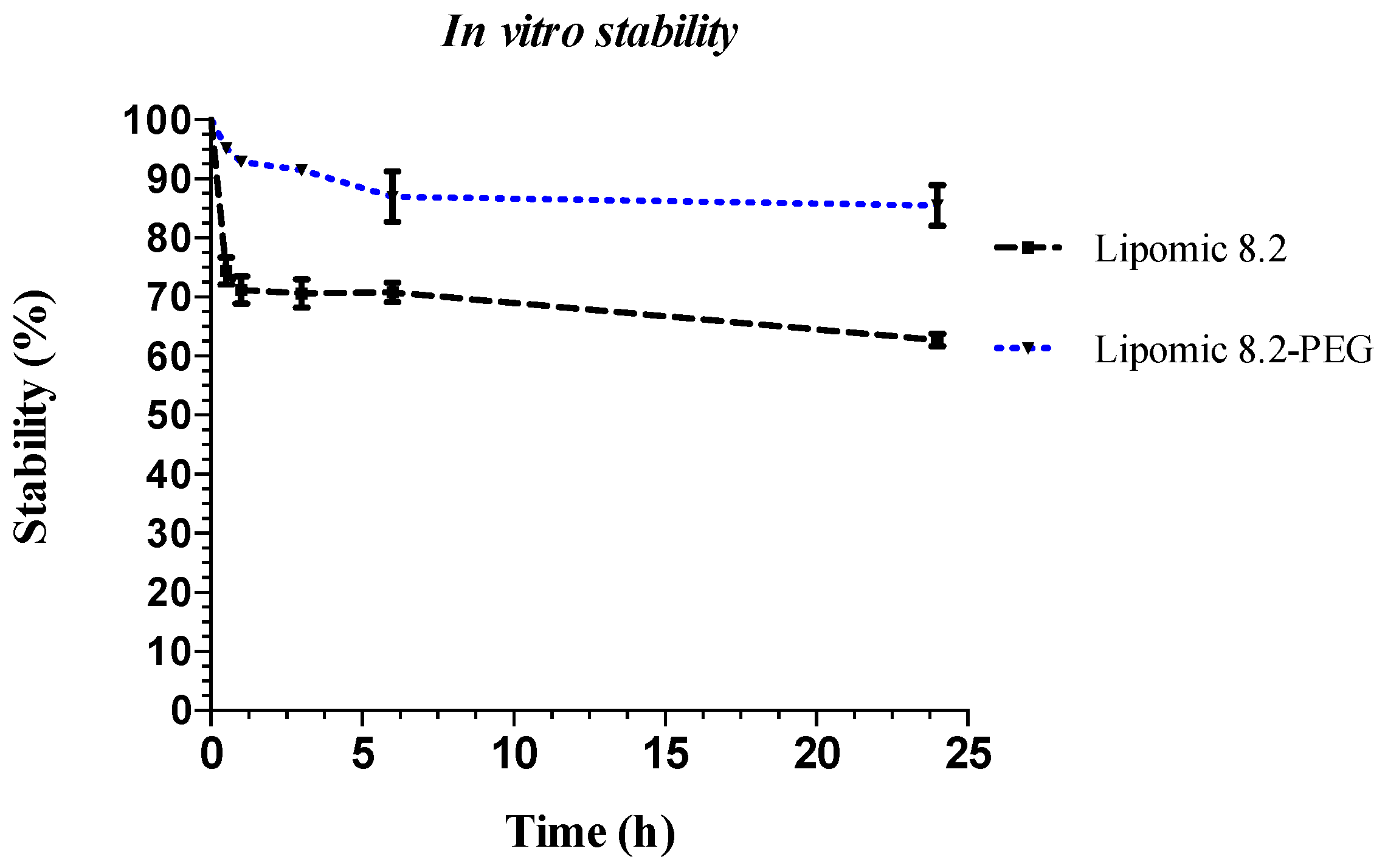
Figure 6b). The results of the radiolabeling combined with the results of electronic microscopy suggest the existence of lipomic systems, also showing its hybrid nature, being able to “load” both hydrophilic and lipophilic compounds and being more efficient than liposomes by not requiring the use of glucoheptonate.
Solubility has a crucial role in the success of any drug candidate because low solubility not only causes problems for in vitro and in vivo assays, but also adds significant burdens to drug development. The delivery of hydrophobic chemotherapeutic drugs via the intravenous route remains a great challenge as these therapeutic molecules are associated with poor pharmacokinetics and bioavailability. In the present study, we obtained a nanocarrier-based biocompatible, non-toxic, and stable system, which can potentially address some of the problems associated with hydrophobic drug encapsulation. Pegylated lipomics as nanocarrier systems are promising for drug delivery; in addition to improving the pharmacokinetics of lipophilic drugs by internalizing them in the micelles core, the lipomics may allow specific a combination of drug delivery by inherent passive-targeting and active-targeting strategies.
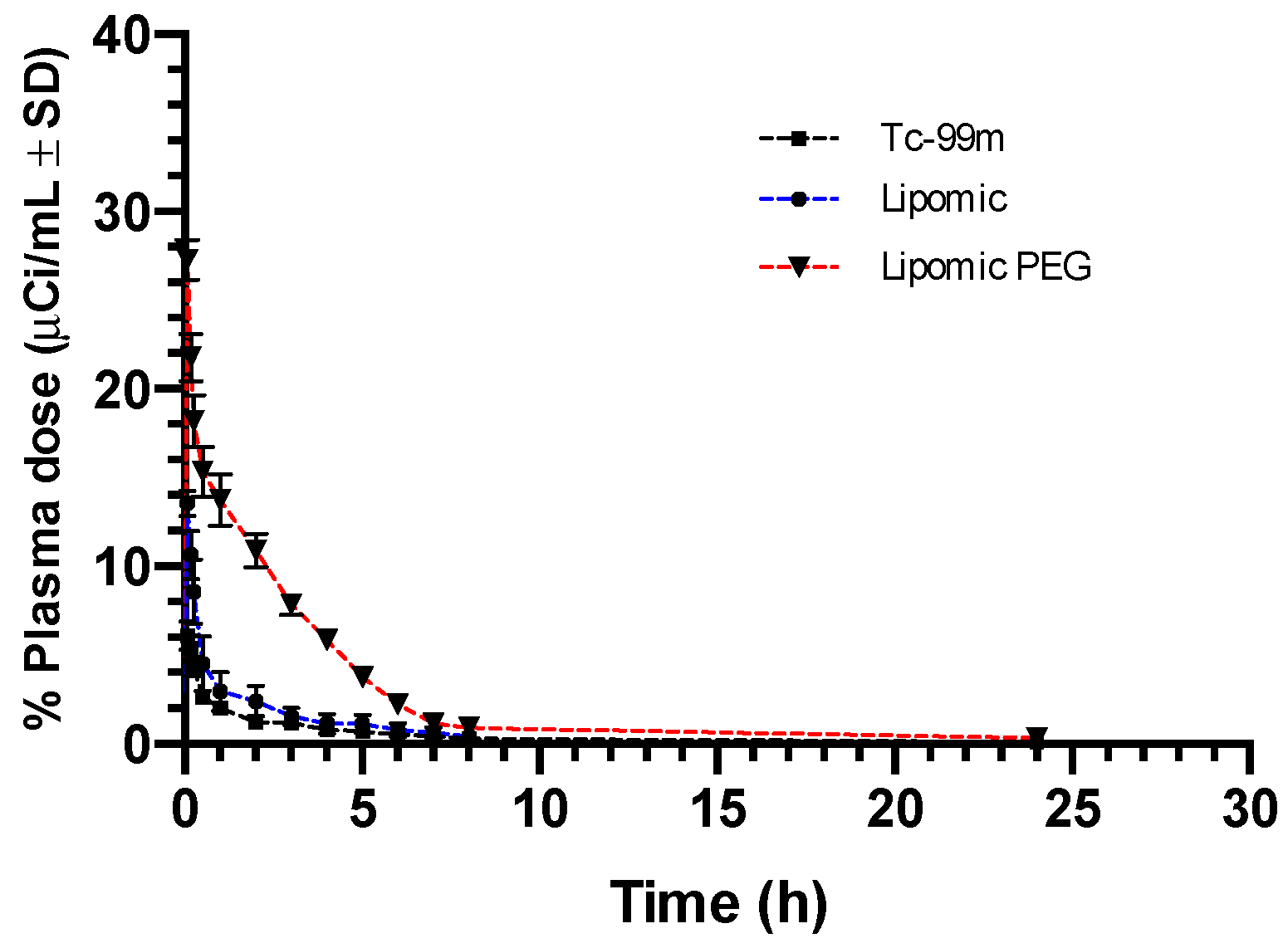
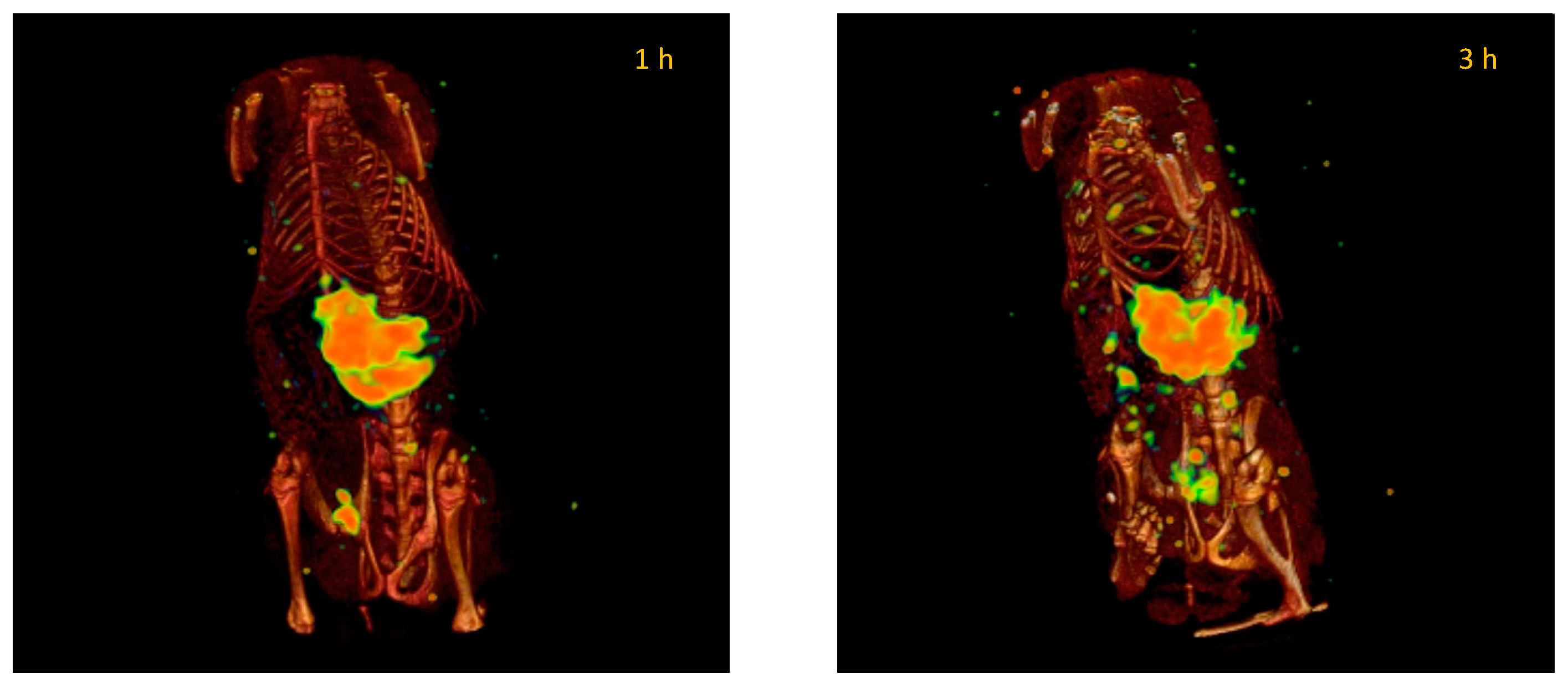
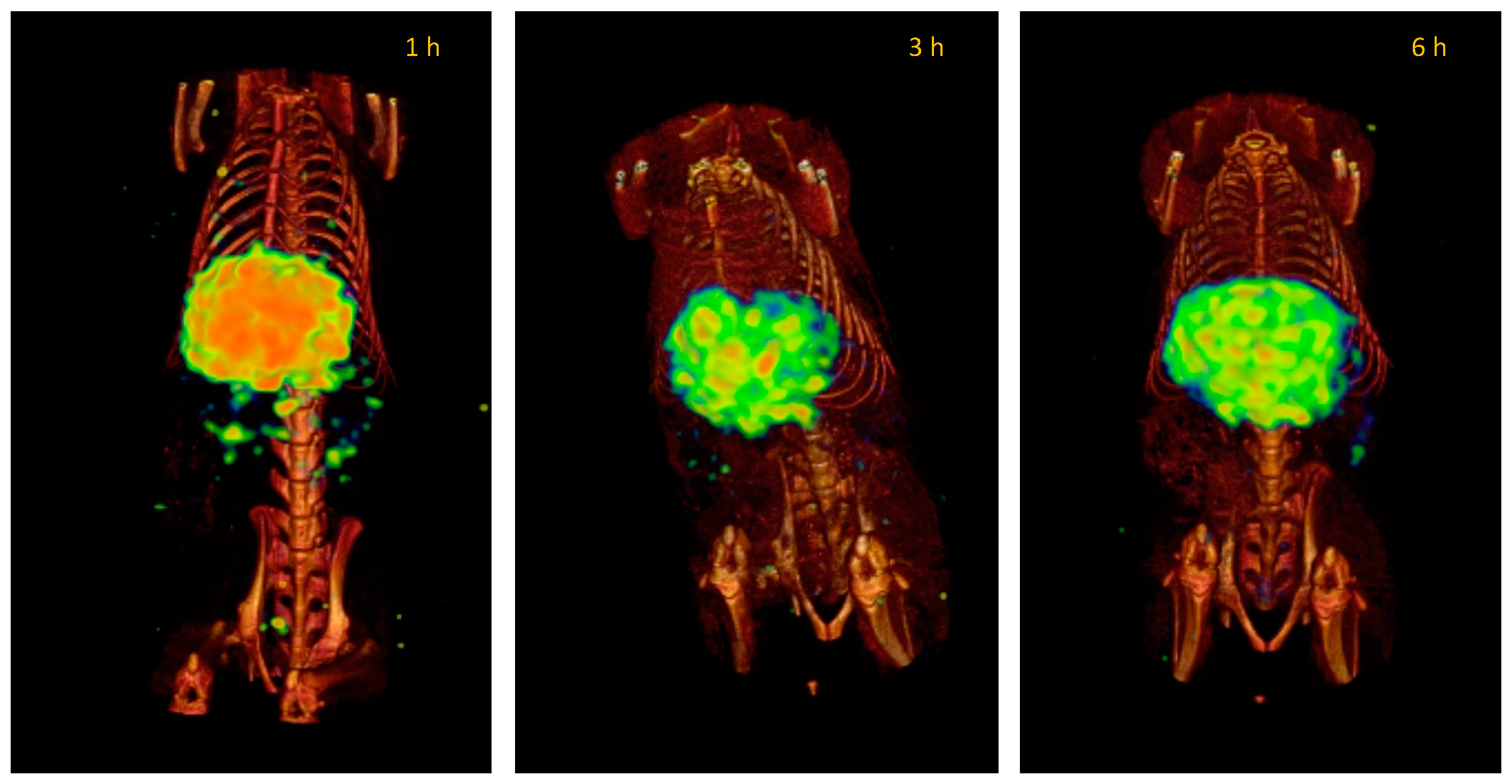
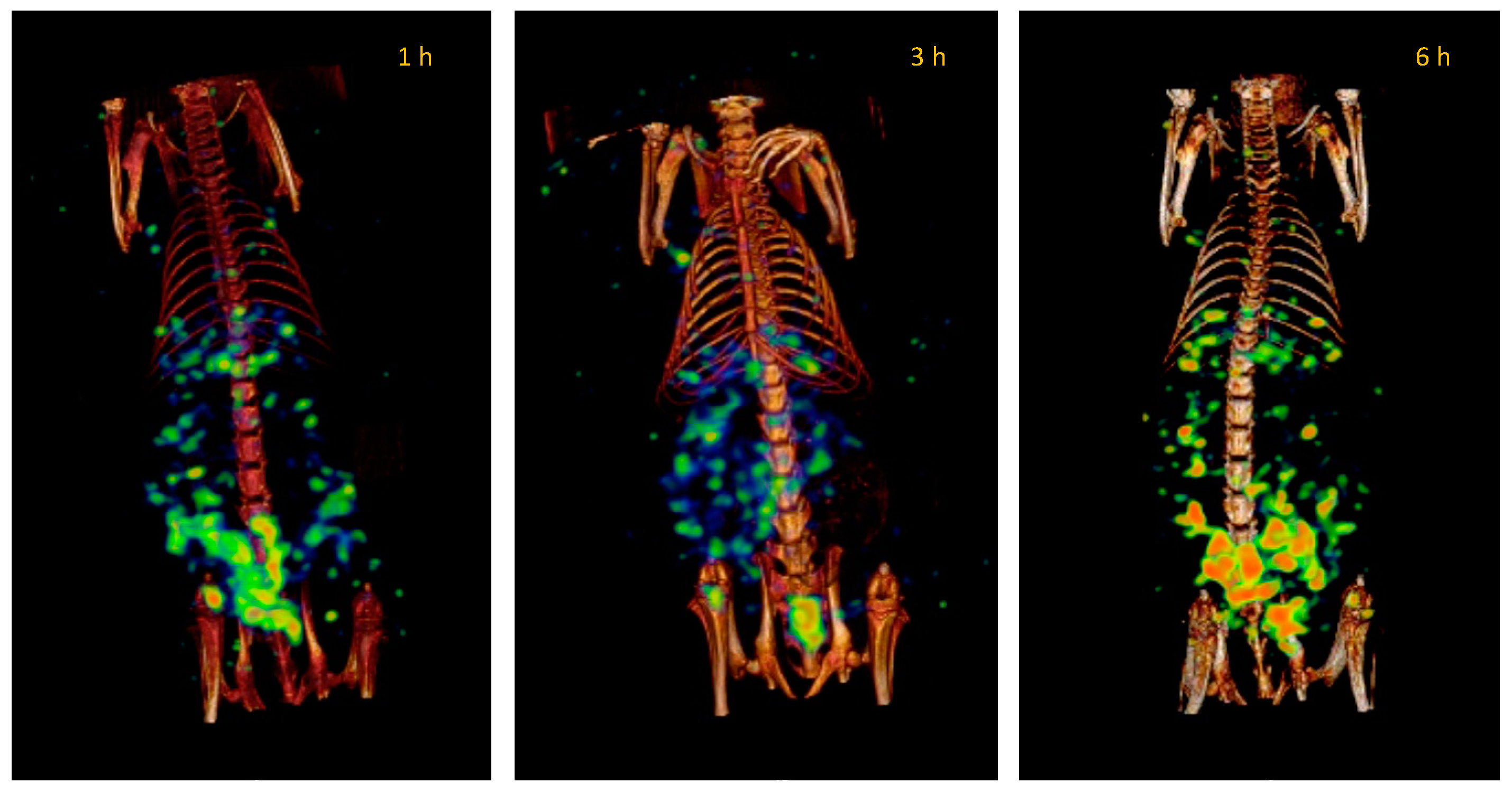
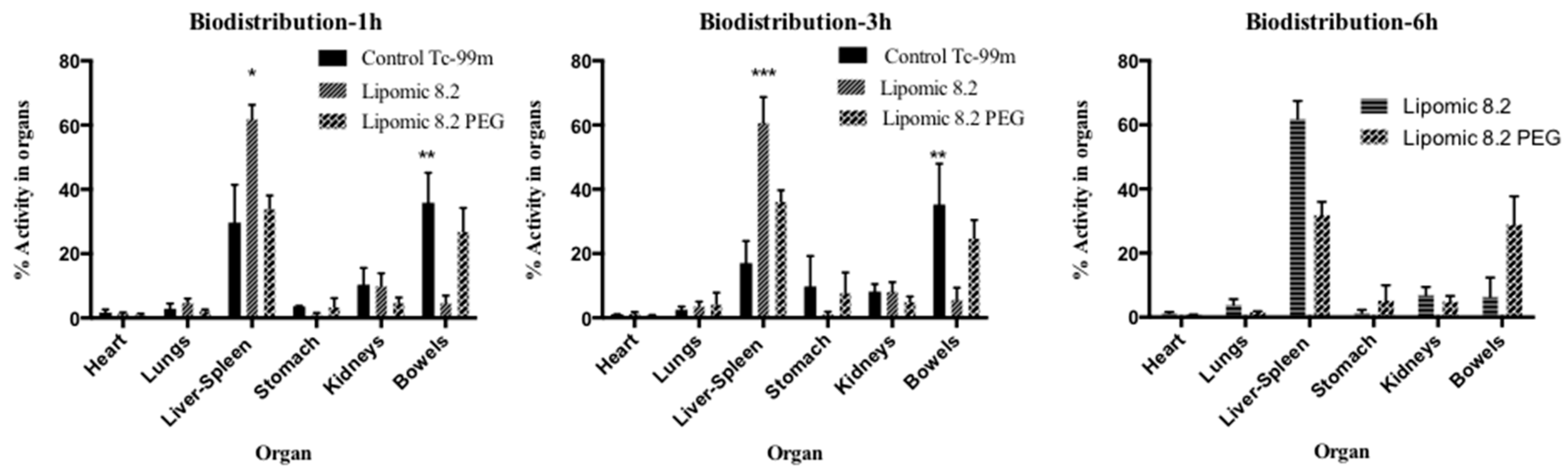
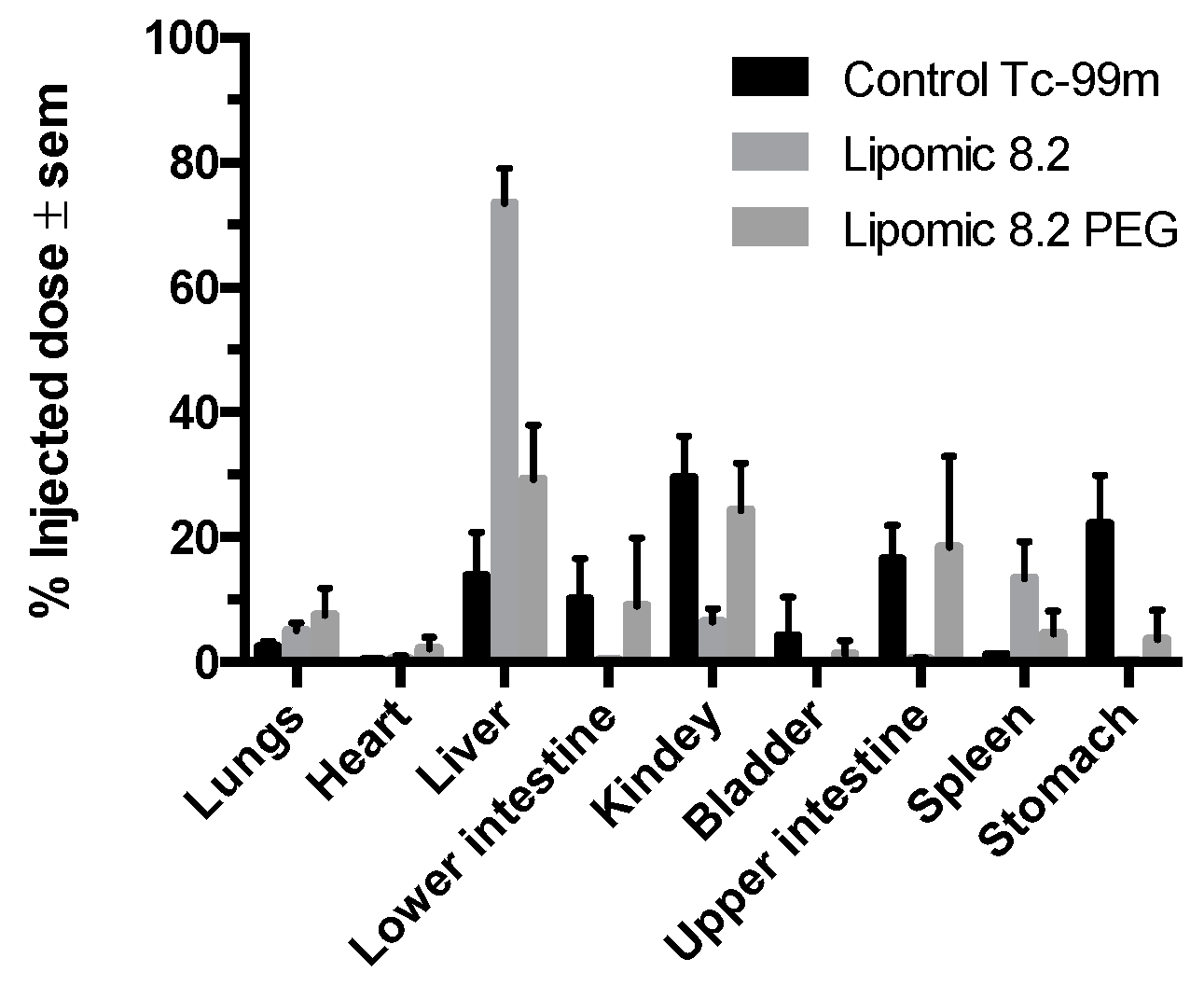
Plasma pharmacokinetics and molecular imaging studies present an overview of the kinetic behavior of systems within the organism. When comparing the biodistribution of “free”
99mTcO
− with radiolabeled lipomics, with and without PEG, pharmacokinetic differences are evident (
Figure 9,
Figure 10 and
Figure 11). By not presenting a protective coating, such as PEG, the differences in the circulation time of
99mTcO
− and
99mTc lipomics are not statistically significant. Liposomes without this coating have shown circulation for approximately 90 min [
25], matching our results (
Figure 8,
Table 3). The technetium, a free molecule smaller than lipomics, is quickly removed from circulation through the renal and glandular systems. On the other hand, pegylated lipomics accumulate in the liver and spleen, although a more heterogeneous biodistribution is observed in the intestines and stomach. Rapid metabolization in the liver and spleen may cause the release of
99mTcO- and, once free, it follows its normal metabolism pathway.
The potential of lipomics to carry both hydrophilic and lipophilic compounds needs to be evaluated with drugs commonly used in medical treatment, and cancer therapy, for example. The main limitation of anticancer drugs, such as taxanes (paclitaxel, docetaxel, and taxol), cisplatin, or gemcitabine is their lack of aqueous solubility, a magnified issue considering the need for its administration by intravenous infusions. Some solubilization strategies for these drugs include using surfactants and co-solvents that also result in adverse side effects [
26]. The implemented procedures used here to elaborate lipomics offer a novel alternative that could minimize adverse effects; no solvents were used in the lipomic elaboration, and surfactants used to form micelles were encapsulated, avoiding its direct interaction that could induce side effects.
The quantitative analysis of biodistribution at 6 h (
Figure 12 and
Figure 13) indicated that non-pegylated lipomics accumulated almost exclusively in the liver, as it is the organ responsible for the metabolism of phospholipids. These lipomics could be used as carriers for drugs related to liver fibrosis, a distinct stage of chronic liver diseases that need novel treatments to block and reverse the underlying pathological process [
27]. For example, silymarin and curcumin have promising effects for liver fibrosis; however, their poor bioavailability, water solubility, toxicity, and targeting efficiency limit their application [
27,
28]; their encapsulation in lipomics could help to reduce these limitations. Other drugs used for liver fibrosis treatment are under investigation, and nanocarriers, such as lipomics, offer a promising field of research to treat this disease. Notably, this carrier showed potential benefits similar to other carriers for poorly water-soluble drugs [
26,
29] that include improved pharmacokinetics and circulation half-life, passive targeting of the liver leading to improved treatments reducing systemic side effects, allowing the co-delivery of hydrophilic and lipophilic drug combinations in a single carrier, and the protection of drugs from quick degradation. As mentioned before, no solvents were used in its preparation, allowing us to minimize the toxic effects on the liver.
4. Materials and Methods
For the manufacturing of lipomics and liposomes, the following excipients were used: 1,2-Distearoyl-sn-Glycero-3-Phosphatidylcholine (DSPC) (Northern Lipids INC, Burnaby, BC, Canada), soy lecithin (Droguería Cosmopolitan, Ciudad de México, México), cholesterol (Chol) and N-(Carbonyl-Methoxypolyethylene glycol 2000)-Dystearoyl-Glycerophosphoethanolamine (DSPE-mPEG (2000) (T&T Scientific Corp, Knoxville, TN, USA), polyoxyethylenesorbitan monolaurate (Tween® 20), polyoxyethylene sorbite monopalmitate (Tween® 40), polyethylene glycol sorbitan monostearate (Tween® 60) and polyoxyethylenesorbitan monoeleate (Tween® 80), dextrose, glucohepptonic acid α−D-sodium salt (GSH), ammonium sulfate ((NH4)2SO4) (Sigma-Aldrich St. Louis, MO, USA), uranyl acetate (UO2(CH3COO)22H2O) (Specialty Chemistry of the Northwest, Sonora, Mexico), chloroform (CHCl3) (Reproquifin, Ecatepec de Morelos, Mexico), and methanol (CH3OH) (Honeywell Research Chemicals, Charlotte, NC, USA).
For the physicochemical evaluation, BI-ZR3 Zeta, a standard for potential (Brookhaven Instruments Corporation, USA); a particle-size reference standard made with NanospheresTM (Thermo Scientific, Waltham, MA, USA); potassium chloride (KCl); sodium chloride (NaCl); and ammonium ferrothiocyanate (NH4FeSCN) (Specialty Chemistry of the Northwest, Sonora, Mexico) were used.
In the radiolabeling, N,N-Bis(2-mercaptoethyl)-N′,N′-diethylenediamine (BMEDA), dimethylsulfoxide MB-grade (DMSO), tin chloride II (SnCl2) (Sigma-Aldrich St. Luis, MO, USA), nitrogen gas (PRAXAIR, Guildford, UK), hydrochloric acid (HCl) (Fermont, Monterrey, Mexico), acetic acid (CH3COOH) (Reproquifin, Ecatepec de Morelos, Mexico), and technetium pertechnetate (99mTcO−) (MIYMSA, CdMx, México) were used.
4.1. Taguchi’s Experimental Design
Minitab software (Minitab Inc. Version 18) was used to design Taguchi’s experimental method. Four variables, (i) surfactant concentration; (ii) phospholipid; (iii) sonication time; and (iv) flow rate, with two levels of assessment (levels 1 and 2), were considered to measure the effect of particle size (
Table 4). An orthogonal arrangement with sixteen possibilities was proposed (
Table 5).
4.2. Determination of the Cloud Point (Cp)
Four non-ionic surfactants (Tween® 20, 40, 60, and 80) were used to determine the Cp; twelve solutions were elaborated at different concentrations in a weight-to-weight ratio (%w/w) in an isotonic saline solution (0.9% NaCl).
The Cp was determined with a homemade turbidimeter. This was created with an experimental setup consisting of a heating bracket (the grill) of one piece of copper and three 5 W resistors; a magnetic stirrer consisting of a motor with speed control by non-feedback PWM with a neodymium magnet; a vial holder; a thermocouple type K; an LED (the emitter) (5 W, 475 nm wavelength); a detector with a photodiode; and microcontroller to perform measurements and control the system. The equipment was validated with standard measurements before its use.
A vial with a non-ionic surfactant sample was placed on the stand and in contact with the grill. Then, agitation and temperature measurements were initiated. The LED (emitter) turned on and off with a square signal of 500 Hz. A trans-impedance amplifier supported the photodiode (receiver), and the voltage at its output was measured with the microcontroller. The first harmonic amplitude was obtained as a measure related to light intensity. The measurement of the light sensor at 30 °C was considered the baseline for determining the change in turbidity. The turbidity point was considered when there was a change of −3 dB from the initial measurement on the light sensor. The temperature at this point was recorded as the Cp.
4.3. Elaboration of Lipomics
Empty Lipomics
The lipomics were prepared with a mixture of non-ionic surfactants (Tween 20, 40, 60, or 80) and phospholipids (DSPC, Chol, PEG-200) in a molar ratio of (DSPC/Tween/Chol/PEG-200) 60:30:5:5 mol. This mixture was placed in a ball flask, where it was homogenized using a magnetic stirring grill with moderate heating for about an hour; during this time, a volume of isotonic saline (NaCl 0.9%) was added by an infusion pump (baby-B). Subsequently, the ball flask was placed in a rotavapor (Buchi r-3, Switzerland) at 120 rpm for 1 h with sonication and at the temperature of the Cp of the non-ionic surfactant used.
4.4. Elaboration of Liposomes
4.4.1. Empty Liposomes
In a sterile glass jar, the phospholipids (DSPC/Chol/PEG-200) were placed in a molar ratio of 60:35:5 mol, respectively. The phospholipid mixture was dissolved in 15 mL of a chloroform–methanol mixture in a 2:1 ratio. This solution was added, by slow drip, in 10 mL of sterile deionized water at 60 °C. The mixture was transferred to a ball flask and held for an hour of stirring at 120 rpm in a rotavapor (Buchi r-3, Flawil, Switzerland). Subsequently, the ball flask was placed inside a desiccator for 24 h to remove the remains of the solvents.
4.4.2. Manufacture of Liposomes Loaded with Glucoheptanate
The same methodology previously described was used, but by replacing the 10 mL of deionized water with a solution of sodium glucoheptanate (GSH) with a concentration of 1 mg/mL, dissolved in a solution of ammonium sulfate ((NH4)2SO4) of 300 mM. At the end of the process, the liposomes were eluted in a PD-10 column (pH 7.4), previously balanced with a PBS solution.
4.5. Physicochemical Evaluation
4.5.1. Ternary Diagrams
For elaborating the pseudo-ternary phase diagrams, OriginPro software (OriginLab Corporation., Northampton, MA, USA) was used to visualize the variability in the proportion of components along each trajectory.
4.5.2. Particle Size and Z Potential
Dynamic Light-Scattering Spectrophotometry (DLS) determined the particle size and Z potential using Zetasizer Analyzer 90 PLUS/BI-MAS equipment (Brookhaven Instruments Corporation, Holtsville, NY, USA).
A total of 5 μL of polystyrene nanospheres were used as a reference standard (Duke Scientific, Palo Alto, CA, USA) dispersed in approximately 2 mL of KCl 10 mM, previously filtered (Millipore filter of 0.22 μm) to verify the proper functioning of the equipment. For sizing (hydrodynamic diameter), 10 μL samples of the lipomics diluted in approximately 2 mL of KCl 10 mM were used.
The Zeta potential was determined using a palladium electrode with a clear four-sided acrylic cell. As a standard, BI-ZR3 Zeta was used in a previously filtered KCl 1 mM solution (Millipore filter of 0.22). The measurement was performed with 100 μL of sample diluted in 1.5 mL of KCl 1 mM.
4.5.3. Quantification of Phospholipids
The quantification of the phospholipids was performed with Stewart’s method [
30]. Briefly, 20 μL of lipomics or liposome samples were dried and reconstituted with chloroform (1mL); ammonium ferrothiocyanate (1 mL) was added and the mixture was shaken vigorously followed by centrifugation at 4 °C, 3000 rpm for 3 min (Centrifuge 5702R rotor #A-4–38, Eppendorf AG, Germany). The absorbance of the chloroform phase was measured with a UV-Vis DUO 530 spectrophotometer (Beckman Coulter, Brea, CA, USA) at a wavelength of 480 nm. A calibration curve (Abs vs. phospholipid concentration (mg/mL)), created with known concentrations of a solution of DSPC in chloroform, was used for quantification.
4.5.4. Physicochemical Stability
All lipomic solutions were stored in conical tubes (Thermo Fisher Scientific) at 4 °C; from these samples, an aliquot was obtained every 5 days, and the Zeta potential and particle size were measured to evaluate their stability for 30 days.
4.5.5. STEM, SEM, and TEM Microscopies
Microscopy techniques were applied only to lipomic formulations with high stability over 30 days. Briefly, a dilution (1:100) was made of each sample, then a drop (~50 μL) was placed on a copper grid coated with 400-mesh carbon film and allowed to dry for 5 min. Then, the sample was stained with 2% uranyl acetate solution allowed to be absorbed by the lipomics. Subsequently, the samples were placed in an Ultra-High Resolution Scanning Electron Microscope JSM-7800F (Institute of Physics, UNAM). TEM and STEM techniques (electron beam at 30 kV) evaluated the morphology and size. No contrast medium (uranyl acetate) was used with SEM imaging.
4.6. Radiolabeling
4.6.1. Preparation of BMEDA Kits for Radiolabeling
Two kits were prepared to implement radiolabeling. Kit 1 (to radiolabel lipomics) was prepared with 70 μL of BMEDA at a concentration of 0.5 mg/mL dissolved in dimethyl sulfoxide (DMSO) and 840 μL SnCl2 with a concentration of 10 mg/mL dissolved in HCl 0.1 M. Kit 2 (to radiolabel liposomes) contained the same components as Kit 1, plus 875 μL of GSH with a concentration of 50 mg/mL dissolved in 10% acetic acid v/v. The kits were vigorously stirred and degassed with nitrogen (N2) for 15 min. The final volume of each kit was divided into 11 Eppendorf tubes (Thermo Fisher Scientific). These tubes were frozen with liquid nitrogen and subjected to lyophilization (FreeZone 2.5, Labconco, Fort Scott, KS, USA). The freeze-dried samples (BMEDA kits) were stored under vacuum conditions in a desiccator until later use.
4.6.2. Radiolabeling of Liposomes and Lipomics
BMEDA kits were resuspended in 5 mL of isotonic saline (NaCl 0.9%) and subsequently degassed for 15 min with N2. Then, HCl 1 M was added until a pH of 2 was obtained. From the above solution, an aliquot of 1 mL was obtained and placed in an Eppendorf tube, followed by adding 185 MBq (5 mCi) of technetium pertechnetate (99mTcO−); the mixture was vigorously stirred for 30 min. Later, the pH was modified by adding NaOH 1 M until reaching a value of 6 or 7, depending on the sample.
For radiolabeling, a volume of lipomics or liposomes, equivalent to 30 μmol of phospholipids (~0.5 mL), was added to
99mTc-2BMEDA Kits 1 or 2, respectively, and incubated at 39 °C for 1 h at 300 rpm. Radiolabeling efficiency (RE) was estimated by instant thin-layer chromatography on silica-impregnated glass-fiber sheets (iTLC-SG) (Agilent Technologies, Santa Clara, CA, USA). Two microliters of RIC were spotted on 10 cm strips of the chromatography sheet paper; isotonic saline was used as the mobile phase. The strips were cut in half, and the radioactivity in each segment was measured using a well-type gamma counter (Ludlum 2200, Sweetwater, TX, USA). The
%RE was calculated as:
where
B1 and
T1 represent the radioactivity (cps) measured at the bottom and top iTLC-SG segments, respectively.
4.6.3. In Vitro Radiolabeling Stability
An aliquot of 20 μL of radiolabeled lipomics was obtained and added to 250 μL of human serum. Subsequently, the mixture was incubated in a dry bath at 37 °C with a constant stirring of 300 rpm (Multi-Therm, Thermo Fisher). Aliquots of 2.5 μL were obtained at 0, 0.5, 1, 3, 6, 12, and 24 h; %RE was measured as previously described.
4.7. Pharmacokinetic Evaluation
4.7.1. Animals
Healthy male Wistar rats (6–8 weeks old) were obtained from the UNAM’s Medical School animal facility (Mexico City). The animals were kept in a pathogen-free environment and fed with autoclaved food and water ad libitum with photoperiod day/night 12/12, at a temperature of 22 °C and humidity of 40%. The procedures for the care and use of the animals were approved by the local Institutional Scientific and Ethics Committees at INCan (017/027/IBI)(CEI/1147/17), and all applicable governmental regulations (NOM-062-ZOO-1999, Ministry of Agriculture, Mexico City, Mexico) were followed. The guidelines from the Guide for the Care and Use of Laboratory Animals of the National Institute of Health (NIH, Bethesda, MD, USA) [
31] were also followed. All efforts were made to minimize animal suffering and reduce the number of animals used in the experiments.
4.7.2. Blood Pharmacokinetics and Biodistribution Studies of Rats
The rats were organized into three groups (n = 5). The control group was administered intravenously with 250 μCi of 99mTcO−, while experimental groups were intravenously injected with 300 μCi of 99mTc-lipomics or 99mTc-lipomics-PEG. Twenty microliters of blood drawn from the tail was collected at different times (min. to hours). The sample’s radioactivity was immediately measured on the well gamma counter (Ludlum 2200, Sweetwater, TX, USA). A graph of blood activity concentration (μCi/mL) against time was created, and the pharmacokinetic parameters were obtained from the calculation of a bicompartmental model. Some animals were sacrificed at 3 h, and the organs of interest were removed (spleen, heart, stomach, liver, small intestine, large intestine, lungs, kidneys, and bladder); these organs were weighed, and significant portions of the tissue were taken to quantify the activity in them.
4.7.3. Image Acquisition and Analysis
Imaging studies were performed at 1, 3, and 6 h after injection to observe the biodistribution of 99mTcO−, 99mTc-lipomics, and 99mTc-lipomics-PEG in the body. A microPET/SPECT/CT imaging system (Albira ARS, Bruker, Valencia, Spain) was used. During imaging, the rats were anesthetized using a mixture of oxygen/isoflurane at 3%. SPECT scans using a pinhole collimator were performed with 30 projections per detector at 60 s/projections. CT scans were performed with 600 projections (tube voltage 45 kV and 0.4 mA). SPECT images were reconstructed with Albira’s reconstruction software based on the ordered subsets expectation–maximization (OSEM) routine (three iterations).
The percentage of activity at some specific time t (%A(t)) in the site of interest (organs) was calculated from the images as the ratio of the detected counts in the organ and the total number of counts detected in the whole body at baseline (A0), multiplied by 100 (%A(t) = Aorgan(t)/A0 × 100). A volume of interest (VOI) was drawn around the organ and the entire body on the images using PMODE software (PMOD Technologies LLC, Zurich, Switzerland) to determine the number of counts held. A vial with 5 μCi of 99mTcO− was imaged and used to correlate counts in the VOIs with organ activity. Counts associated with the VOIs were corrected for radioactive decay with the image acquisition time.
4.8. Statistical Analysis
Values are reported as mean values ± standard deviation. Statistical analysis was performed using a one-way analysis of variance (ANOVA) on Prism 8 software (GraphPad Software, San Diego, CA, USA). The significance was determined at p < 0.05.