Evaluation of Topical and Subconjunctival Injection of Hyaluronic Acid-Coated Nanoparticles for Drug Delivery to Posterior Eye
Abstract
:1. Introduction
2. Materials and Methods
2.1. Reagent and Chemicals
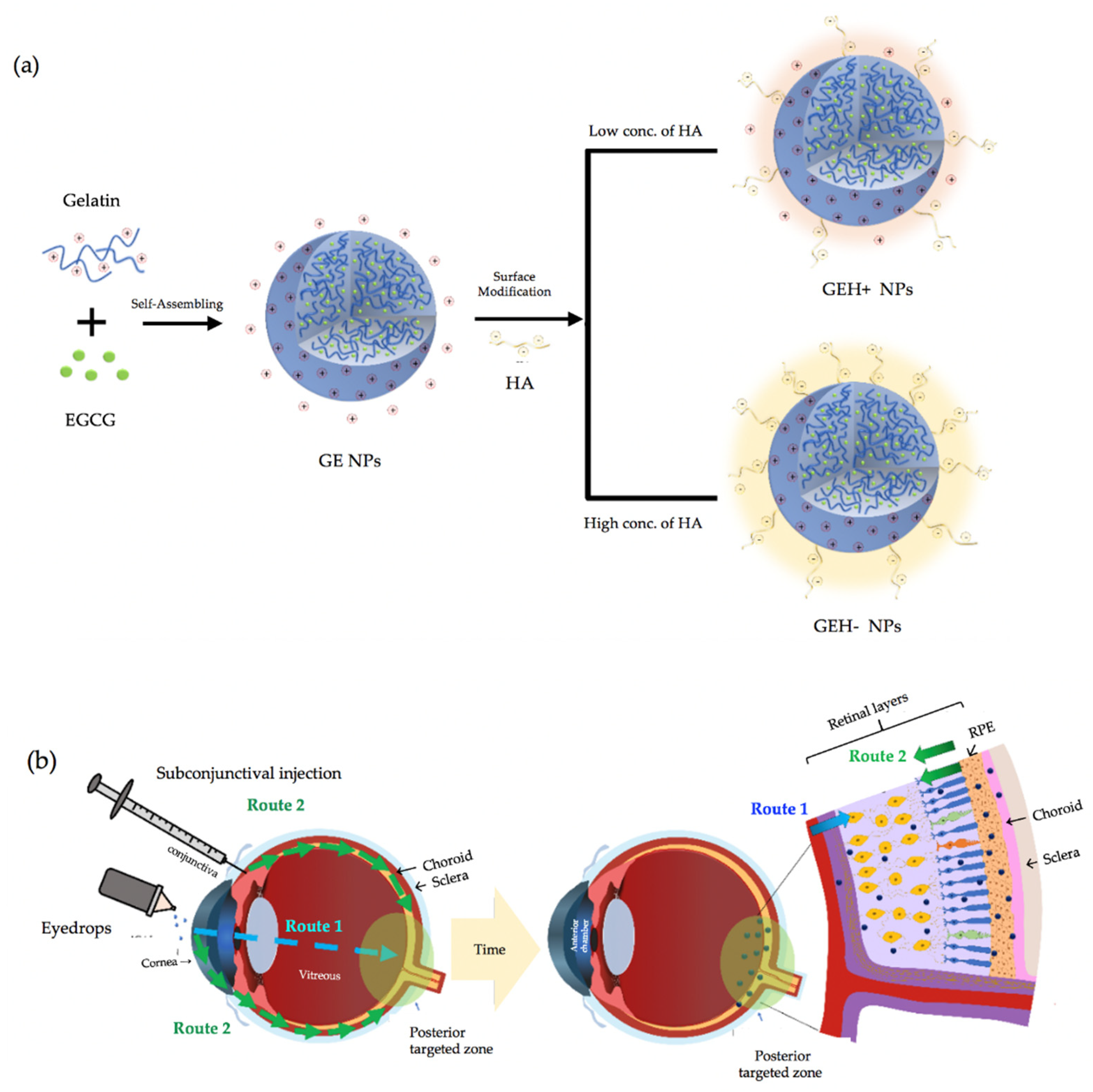
2.2. Preparation and Characterization of GE NPs with/without HA Coating
2.3. In-Vitro Test
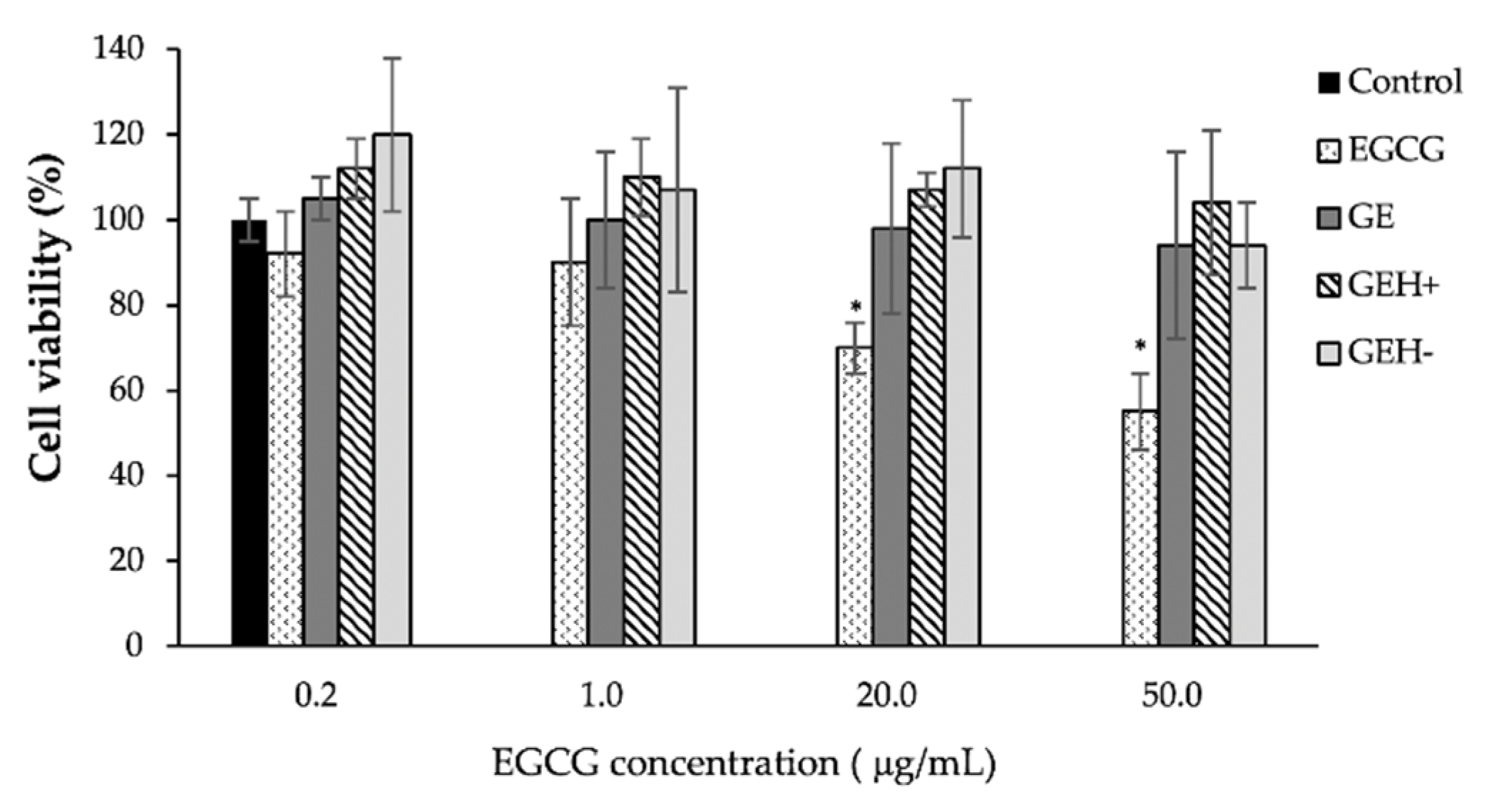
2.3.1. Cytotoxicity Evaluation
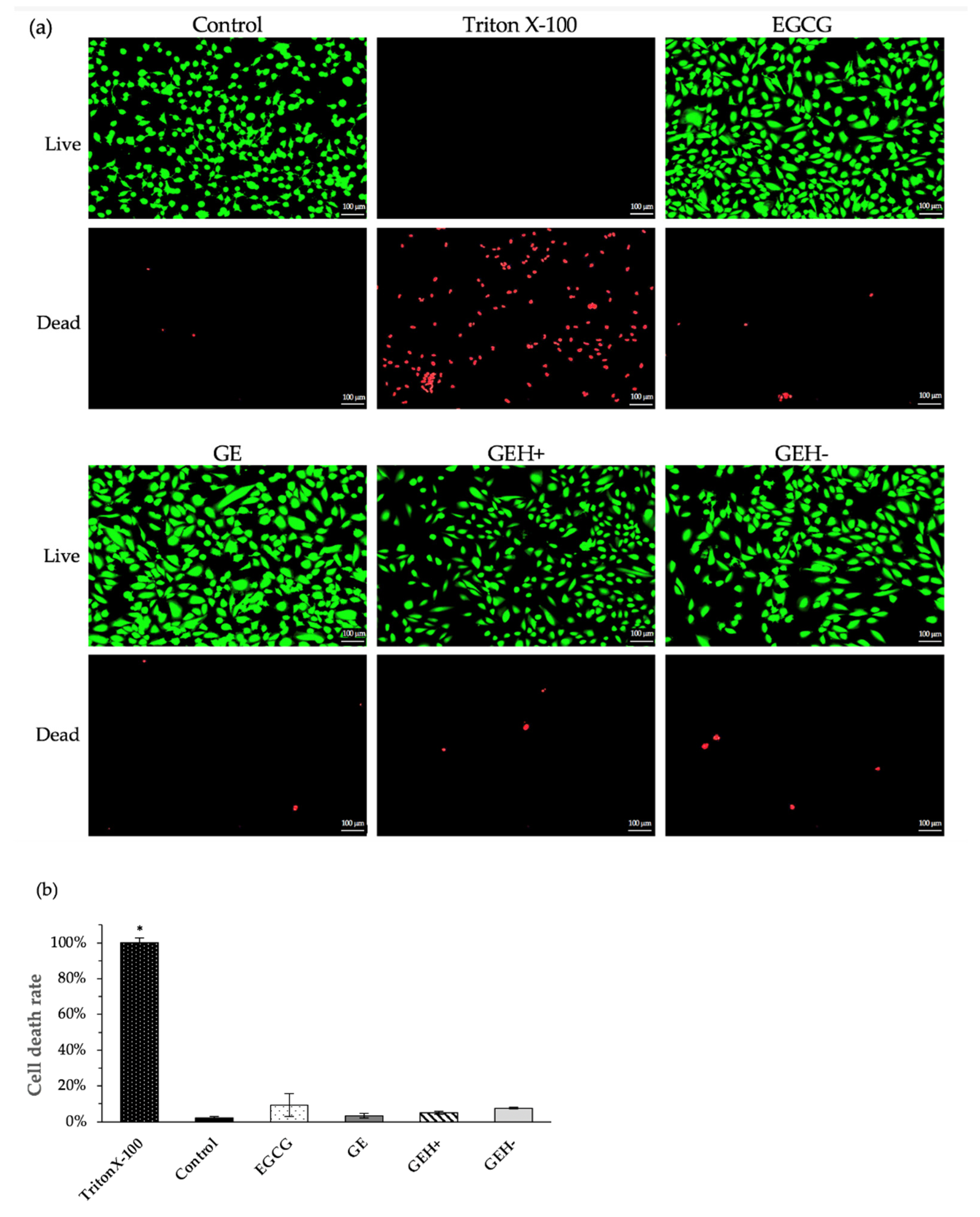
2.3.2. Viable Cells Staining
2.3.3. Cellular Uptake of NPs
2.4. In-Vivo Test
2.4.1. Topical Administration—Eye Drops
2.4.2. Subconjunctival Injection (SCI)
2.4.3. Cryosection Examination via Slide-Based Tissue Cytometry
2.5. Statistical Analysis and Visualizations
3. Results
3.1. Characterization of NPs
3.2. Cytotoxicity and Cell Viability
3.3. GEH+ NPs Highly Uptake
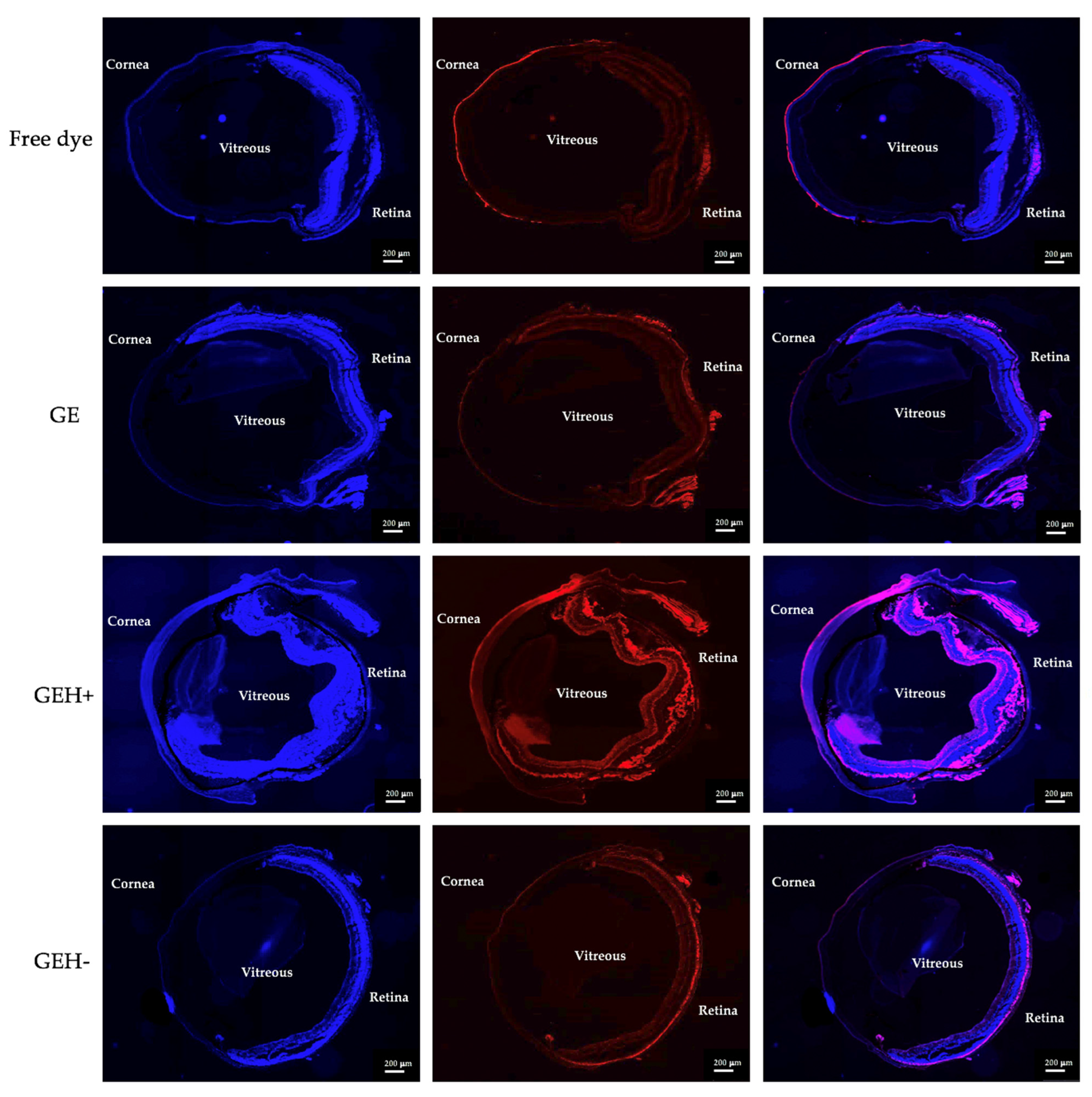
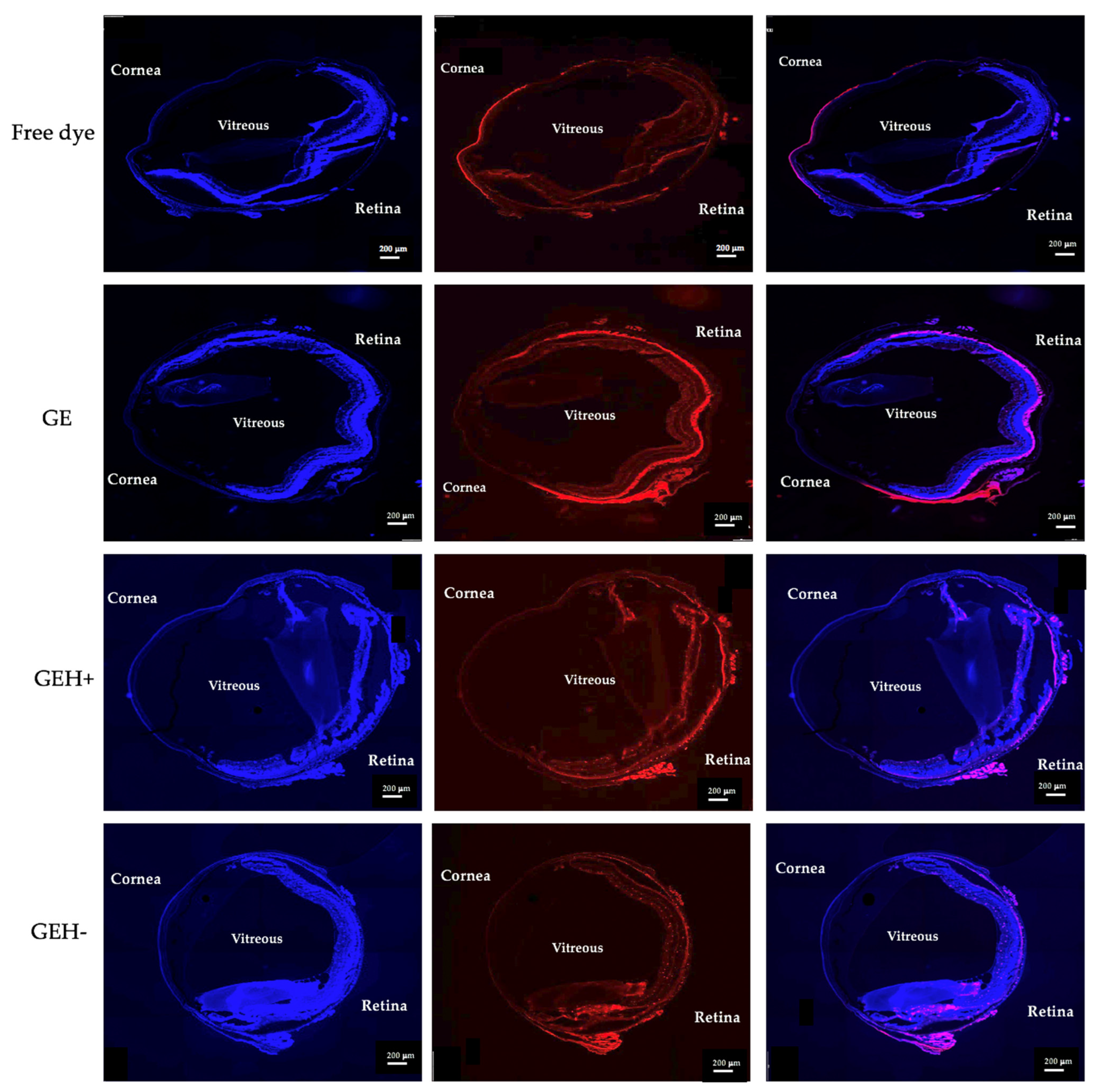
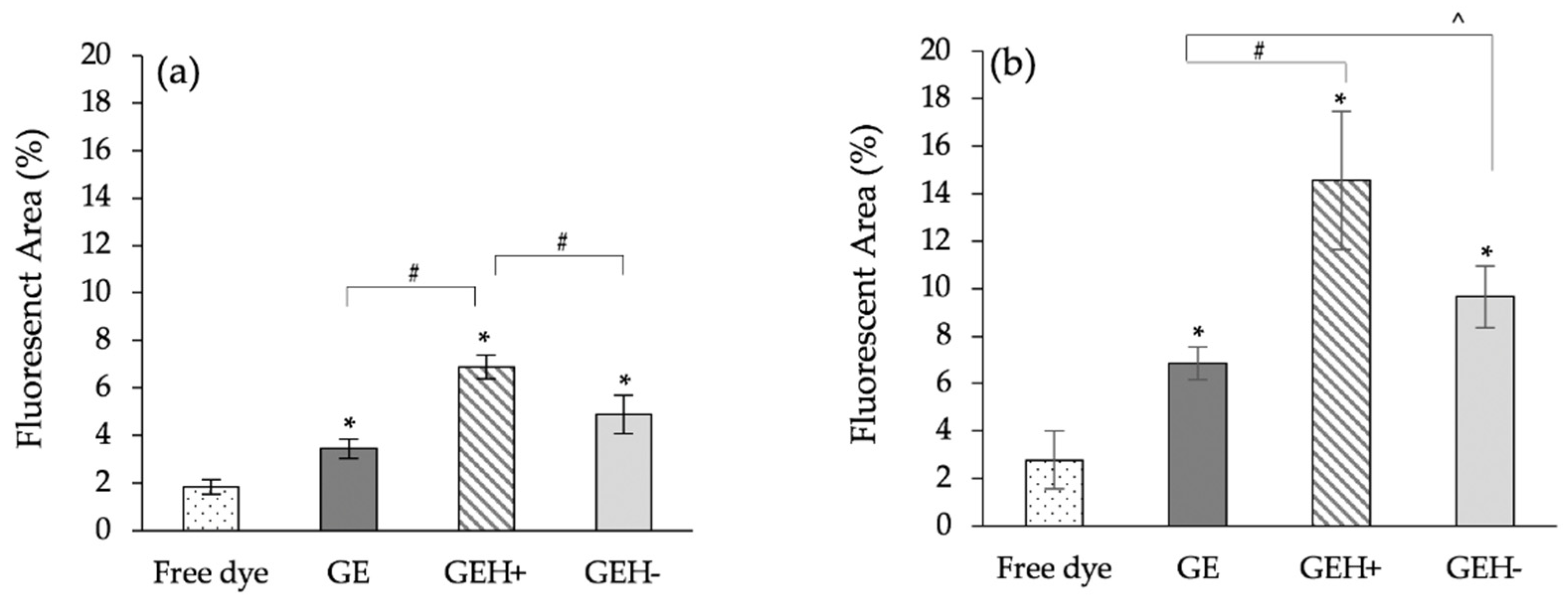
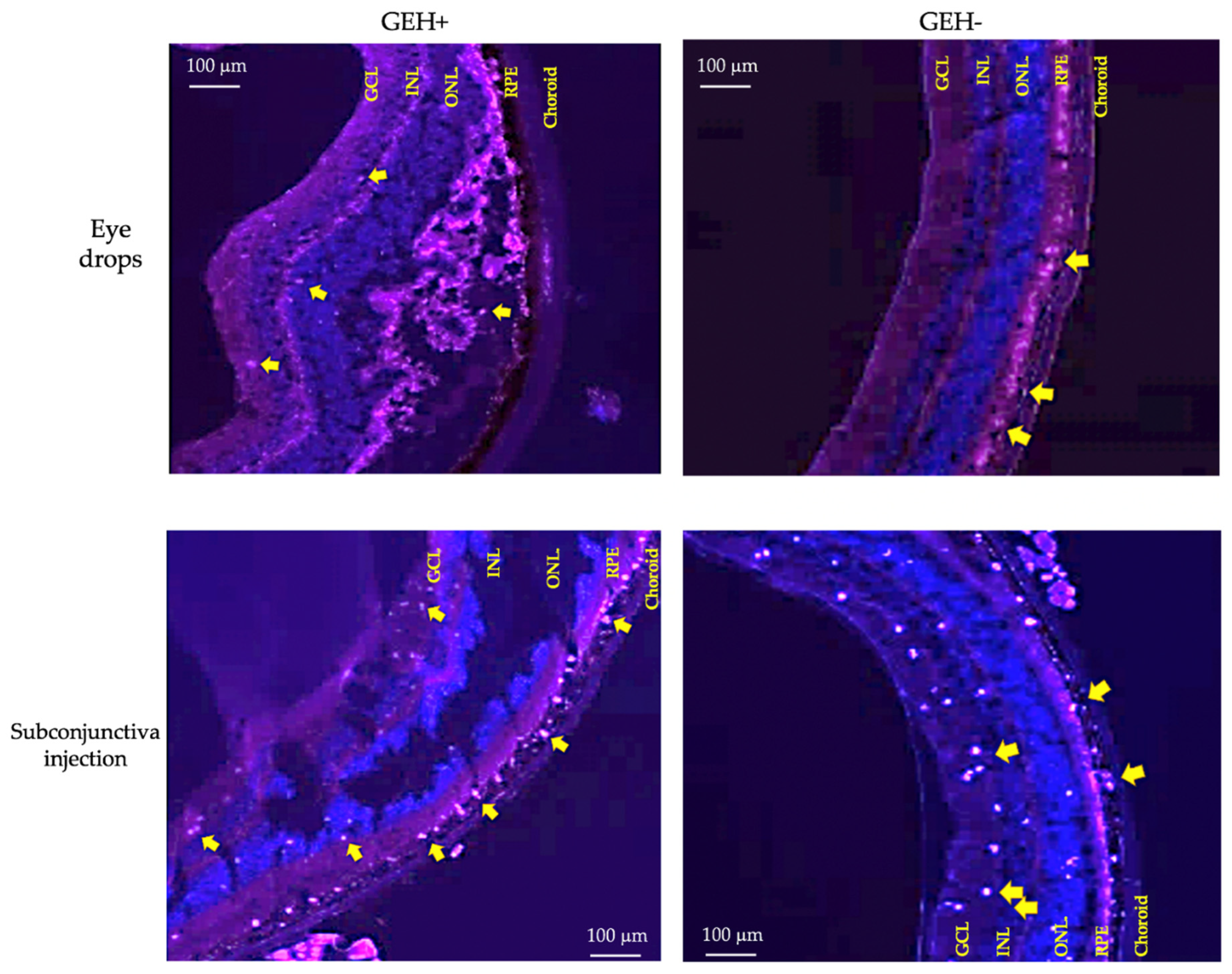
3.4. NPs’ Distribution in Eyes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ono, K.; Hiratsuka, Y.; Murakami, A. Global inequality in eye health: Country-level analysis from the Global Burden of Disease Study. Am. J. Public Health 2010, 100, 1784–1788. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.-F.; Hao, J.-L.; Xie, T.; Mukhtar, N.J.; Zhang, W.; Malik, T.H.; Lu, C.-W.; Zhou, D.-D. Curcumin, a potential therapeutic candidate for anterior segment eye diseases: A review. Front. Pharmacol. 2017, 8, 66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molokhia, S.A.; Thomas, S.C.; Garff, K.J.; Mandell, K.J.; Wirostko, B.M. Anterior eye segment drug delivery systems: Current treatments and future challenges. J. Ocul. Pharmacol. Ther. 2013, 29, 92–105. [Google Scholar] [CrossRef]
- Sacca, S.; Izzotti, A.J. Oxidative stress and glaucoma: Injury in the anterior segment of the eye. Prog. Brain Res. 2008, 173, 385–407. [Google Scholar] [CrossRef] [PubMed]
- Berger, W.; Kloeckener-Gruissem, B.; Neidhardt, J.J. The molecular basis of human retinal and vitreoretinal diseases. Prog. Retin. Eye Res. 2010, 29, 335–375. [Google Scholar] [CrossRef] [Green Version]
- Joussen, A.M.; Gardner, T.W.; Kirchhof, B.; Ryan, S.J. Retinal Vascular Disease; Springer: Berlin/Heidelberg, Germany, 2007; Volume 75. [Google Scholar]
- Ruby, A.J.; Jampol, L.M. Crohn’s disease and retinal vascular disease. Am. J. Ophthalmol. 1990, 110, 349–353. [Google Scholar] [CrossRef]
- Miller, J.W.; Le Couter, J.; Strauss, E.C.; Ferrara, N.J.O. Vascular endothelial growth factor a in intraocular vascular disease. Ophthalmology 2013, 120, 106–114. [Google Scholar] [CrossRef]
- Tsai, C.-H.; Wang, P.-Y.; Lin, I.; Huang, H.; Liu, G.-S.; Tseng, C.-L. Ocular drug delivery: Role of degradable polymeric nanocarriers for ophthalmic application. Int. J. Mol. Sci. 2018, 19, 2830. [Google Scholar] [CrossRef] [Green Version]
- Bisht, R.; Mandal, A.; Jaiswal, J.K.; Rupenthal, I.D. Nanocarrier mediated retinal drug delivery: Overcoming ocular barriers to treat posterior eye diseases. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2018, 10, e1473. [Google Scholar] [CrossRef]
- Chen, B.; Chen, H.F.; Lu, J.Q.; Xu, B. Pharmacogenomics in Therapeutic Drug Monitoring. In Pharmacogenomics in Precision Medicine; Springer: Berlin/Heidelberg, Germany, 2020; pp. 155–179. [Google Scholar]
- Ustundag Okur, N.; Caglar, E.S.; Siafaka, P.I. Novel ocular drug delivery systems: An update on microemulsions. J. Ocul. Pharmacol. Ther. 2020, 36, 342–354. [Google Scholar] [CrossRef]
- Wang, R.; Gao, Y.; Liu, A.; Zhai, G. A review of nanocarrier mediated drug delivery systems for posterior segment eye disease: Challenges analysis and recent advances. J. Drug Target. 2021, 29, 687–702. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Emi, K.; Ikeda, T.; Bando, H.; Sato, S.; Morita, S.-I.; Oyagi, T.; Sawada, K.J.O. Severe intraocular inflammation after intravitreal injection of bevacizumab. Ophthalmology 2010, 117, 512–516. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Yu, S.; Liu, K.; Chen, F.-E.; Song, Z.; Zhang, X.; Xu, X.; Sun, X.J.O. Acute intraocular inflammation caused by endotoxin after intravitreal injection of counterfeit bevacizumab in Shanghai, China. Ophthalmology 2013, 120, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.M.; Woo, S.J. Ocular Drug Delivery to the Retina: Current Innovations and Future Perspectives. Pharmaceutics 2021, 13, 108. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.S.; Denham, L.V.; Elison, J.R.; Bhattacharjee, P.S.; Clement, C.; Huq, T.; Hill, J.M. Drug delivery to the posterior segment of the eye for pharmacologic therapy. Expert Rev. Ophthalmol. 2010, 5, 75–93. [Google Scholar] [CrossRef] [Green Version]
- Thrimawithana, T.R.; Young, S.; Bunt, C.R.; Green, C.; Alany, R.G. Drug delivery to the posterior segment of the eye. Drug Discov. Today 2011, 16, 270–277. [Google Scholar] [CrossRef]
- Tran, D.H.N.; Nguyen, T.H.; Vo, T.N.N.; Pham, L.P.T.; Vo, D.M.H.; Nguyen, C.K.; Bach, L.G.; Nguyen, D.H. Self-assembled poly (ethylene glycol) methyl ether-grafted gelatin nanogels for efficient delivery of curcumin in cancer treatment. J. Appl. Polym. Sci. 2019, 136, 47544. [Google Scholar] [CrossRef] [Green Version]
- Tran, H.D.; Park, K.D.; Ching, Y.C.; Huynh, C.; Nguyen, D.H. A comprehensive review on polymeric hydrogel and its composite: Matrices of choice for bone and cartilage tissue engineering. J. Ind. Eng. Chem. 2020, 89, 58–82. [Google Scholar] [CrossRef]
- Omerović, N.; Vranić, E.J.H. Application of nanoparticles in ocular drug delivery systems. Health Technol. 2019, 10, 61–78. [Google Scholar] [CrossRef]
- Huang, H.-Y.; Wang, M.-C.; Chen, Z.-Y.; Chiu, W.-Y.; Chen, K.-H.; Lin, I.-C.; Yang, W.-C.V.; Wu, C.-C.; Tseng, C.-L. Gelatin–epigallocatechin gallate nanoparticles with hyaluronic acid decoration as eye drops can treat rabbit dry-eye syndrome effectively via inflammatory relief. Int. J. Nanomed. 2018, 13, 7251. [Google Scholar] [CrossRef] [Green Version]
- Huang, D.; Chen, Y.-S.; Rupenthal, I.D. Hyaluronic Acid Coated Albumin Nanoparticles for Targeted Peptide Delivery to the Retina. Mol. Pharm. 2017, 14, 533–545. [Google Scholar] [CrossRef]
- Tahara, K.; Karasawa, K.; Onodera, R.; Takeuchi, H. Feasibility of drug delivery to the eye’s posterior segment by topical instillation of PLGA nanoparticles. Asian J. Pharm. Sci. 2017, 12, 394–399. [Google Scholar] [CrossRef] [PubMed]
- Chuang, Y.-L.; Fang, H.-W.; Ajitsaria, A.; Chen, K.-H.; Su, C.-Y.; Liu, G.-S.; Tseng, C.-L.J.P. Development of kaempferol-loaded gelatin nanoparticles for the treatment of corneal neovascularization in mice. Pharmaceutics 2019, 11, 635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Satapathy, M.K.; Nyambat, B.; Chiang, C.-W.; Chen, C.-H.; Wong, P.-C.; Ho, P.-H.; Jheng, P.-R.; Burnouf, T.; Tseng, C.-L.; Chuang, E.-Y. A gelatin hydrogel-containing nano-organic PEI–Ppy with a photothermal responsive effect for tissue engineering applications. Molecules 2018, 23, 1256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sampat, K.M.; Garg, S.J. Complications of intravitreal injections. Curr. Opin. Ophthalmol. 2010, 21, 178–183. [Google Scholar] [CrossRef]
- Koo, H.; Moon, H.; Han, H.; Na, J.H.; Huh, M.S.; Park, J.H.; Woo, S.J.; Park, K.H.; Kwon, I.C.; Kim, K.; et al. The movement of self-assembled amphiphilic polymeric nanoparticles in the vitreous and retina after intravitreal injection. Biomaterials 2012, 33, 3485–3493. [Google Scholar] [CrossRef]
- Hillaireau, H.; Couvreur, P. Nanocarriers’ entry into the cell: Relevance to drug delivery. Cell Mol. Life Sci. 2009, 66, 2873–2896. [Google Scholar] [CrossRef]
- Battaglia, L.; Gallarate, M.; Serpe, L.; Foglietta, F.; Muntoni, E.; del Pozo Rodriguez, A.; Aspiazu, M.A.S. Ocular delivery of solid lipid nanoparticles. In Lipid Nanocarriers for Drug Targeting; Elsevier: Amsterdam, The Netherlands, 2018; pp. 269–312. [Google Scholar]
- Swetledge, S.; Jung, J.P.; Carter, R.; Sabliov, C. Distribution of polymeric nanoparticles in the eye: Implications in ocular disease therapy. J. Nanobiotechnol. 2021, 19, 1–19. [Google Scholar] [CrossRef]
- Gan, L.; Wang, J.; Zhao, Y.; Chen, D.; Zhu, C.; Liu, J.; Gan, Y. Hyaluronan-modified coreeshell liponanoparticles targeting CD44-positive retinal pigment epithelium cells via intravitreal injection. Biomaterials 2013, 34, 5978–5987. [Google Scholar] [CrossRef]
- Crane, I.J.; Liversidge, J. Mechanisms of leukocyte migration across the bloodretina barrier. Semin. Immunopathol. 2008, 30, 165–177. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, B.; Palmer, N.; Shetty, T.; Dimaras, H.; Hajrasouliha, A.; Jusufbegovic, D.; Corson, T.W. Patient preferences in retinal drug delivery. Sci. Rep. 2021, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Varela-Fernández, R.; Díaz-Tomé, V.; Luaces-Rodríguez, A.; Conde-Penedo, A.; García-Otero, X.; Luzardo-Álvarez, A.; Fernández-Ferreiro, A.; Otero-Espinar, F.J. Drug Delivery to the Posterior Segment of the Eye: Biopharmaceutic and Pharmacokinetic Considerations. Pharmaceutics 2020, 12, 269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thacker, M.; Tseng, C.-L.; Lin, F.-H. Substitutes and Colloidal System for Vitreous Replacement and Drug Delivery: Recent Progress and Future Prospective. Polymers 2021, 13, 121. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Yu, Y.; Lin, L.; Liu, X.; Zhang, X.; Wang, P.; Hoffman, P.; Kim, S.Y.; Zhang, F.; Linhardt, R.J. Glycosaminoglycans from bovine eye vitreous humour and interaction with collagen type II. Glycoconj. J. 2018, 35, 119–128. [Google Scholar] [CrossRef]
- White, C.E.; Olabisi, R.M. Scaffolds for retinal pigment epithelial cell transplantation in age-related macular degeneration. J. Tissue Eng. 2017, 8, 1–11. [Google Scholar] [CrossRef] [Green Version]
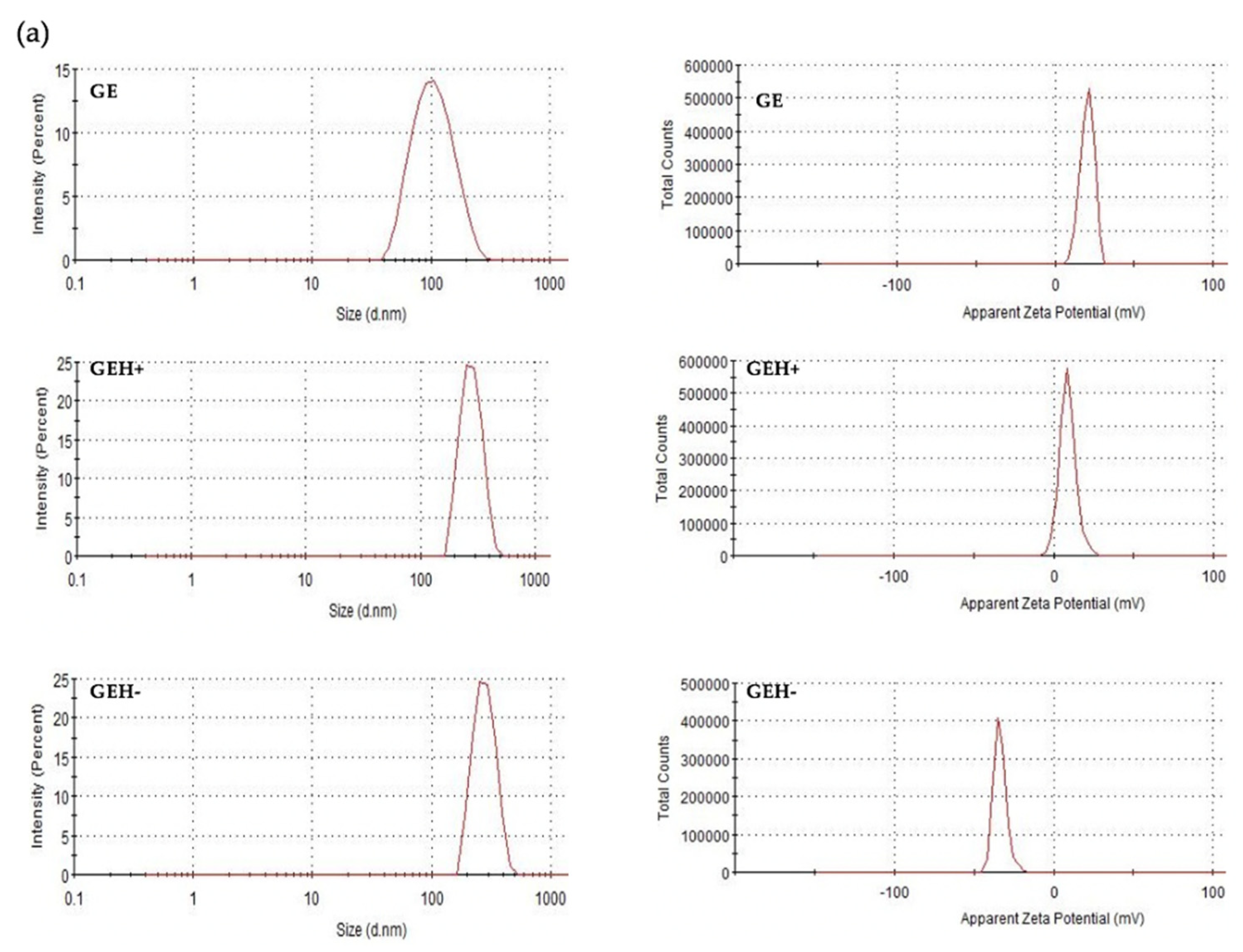


| HA [μg/mL] | Particle Size [nm] | Zeta Potential [mV] | PdI | |
|---|---|---|---|---|
| GE | 0.0 | 98.45 ± 1.37 | 20.40 ± 0.46 | 0.170 ± 0.011 |
| GEH+ | 62.5 | 273.20 ± 3.22 | 9.16 ± 0.43 | 0.042 ± 0.046 |
| GEH− | 167.0 | 353.50 ± 28.54 | −35.40 ± 1.50 | 0.306 ± 0.033 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, C.-H.; Hoang, L.N.; Lin, C.C.; Pan, L.-C.; Wu, C.-L.; Lin, I.-C.; Wang, P.-Y.; Tseng, C.-L. Evaluation of Topical and Subconjunctival Injection of Hyaluronic Acid-Coated Nanoparticles for Drug Delivery to Posterior Eye. Pharmaceutics 2022, 14, 1253. https://doi.org/10.3390/pharmaceutics14061253
Tsai C-H, Hoang LN, Lin CC, Pan L-C, Wu C-L, Lin I-C, Wang P-Y, Tseng C-L. Evaluation of Topical and Subconjunctival Injection of Hyaluronic Acid-Coated Nanoparticles for Drug Delivery to Posterior Eye. Pharmaceutics. 2022; 14(6):1253. https://doi.org/10.3390/pharmaceutics14061253
Chicago/Turabian StyleTsai, Cheng-Han, Le Ngoc Hoang, Chun Che Lin, Liang-Chen Pan, Chiao-Li Wu, I-Chan Lin, Peng-Yuan Wang, and Ching-Li Tseng. 2022. "Evaluation of Topical and Subconjunctival Injection of Hyaluronic Acid-Coated Nanoparticles for Drug Delivery to Posterior Eye" Pharmaceutics 14, no. 6: 1253. https://doi.org/10.3390/pharmaceutics14061253
APA StyleTsai, C.-H., Hoang, L. N., Lin, C. C., Pan, L.-C., Wu, C.-L., Lin, I.-C., Wang, P.-Y., & Tseng, C.-L. (2022). Evaluation of Topical and Subconjunctival Injection of Hyaluronic Acid-Coated Nanoparticles for Drug Delivery to Posterior Eye. Pharmaceutics, 14(6), 1253. https://doi.org/10.3390/pharmaceutics14061253






