Cannabidiol Loaded Topical Ophthalmic Nanoemulsion Lowers Intraocular Pressure in Normotensive Dutch-Belted Rabbits
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.1.1. Chemicals and Glassware
2.1.2. Animals
2.2. Methods
2.2.1. HPLC Method
2.2.2. Preparation of CBD-NE Formulations
2.2.3. Preparation of the Mucoadhesive CBD-NE (CBD-NEC)
2.2.4. Measurement of Globule Size, Polydispersity Index (PDI), and Zeta Potential (ZP)
2.2.5. Assay (CBD Content)
2.2.6. pH Measurement
2.2.7. Viscosity Measurement
2.2.8. Sterilization Process and Stability Assessment
2.2.9. Stability Studies
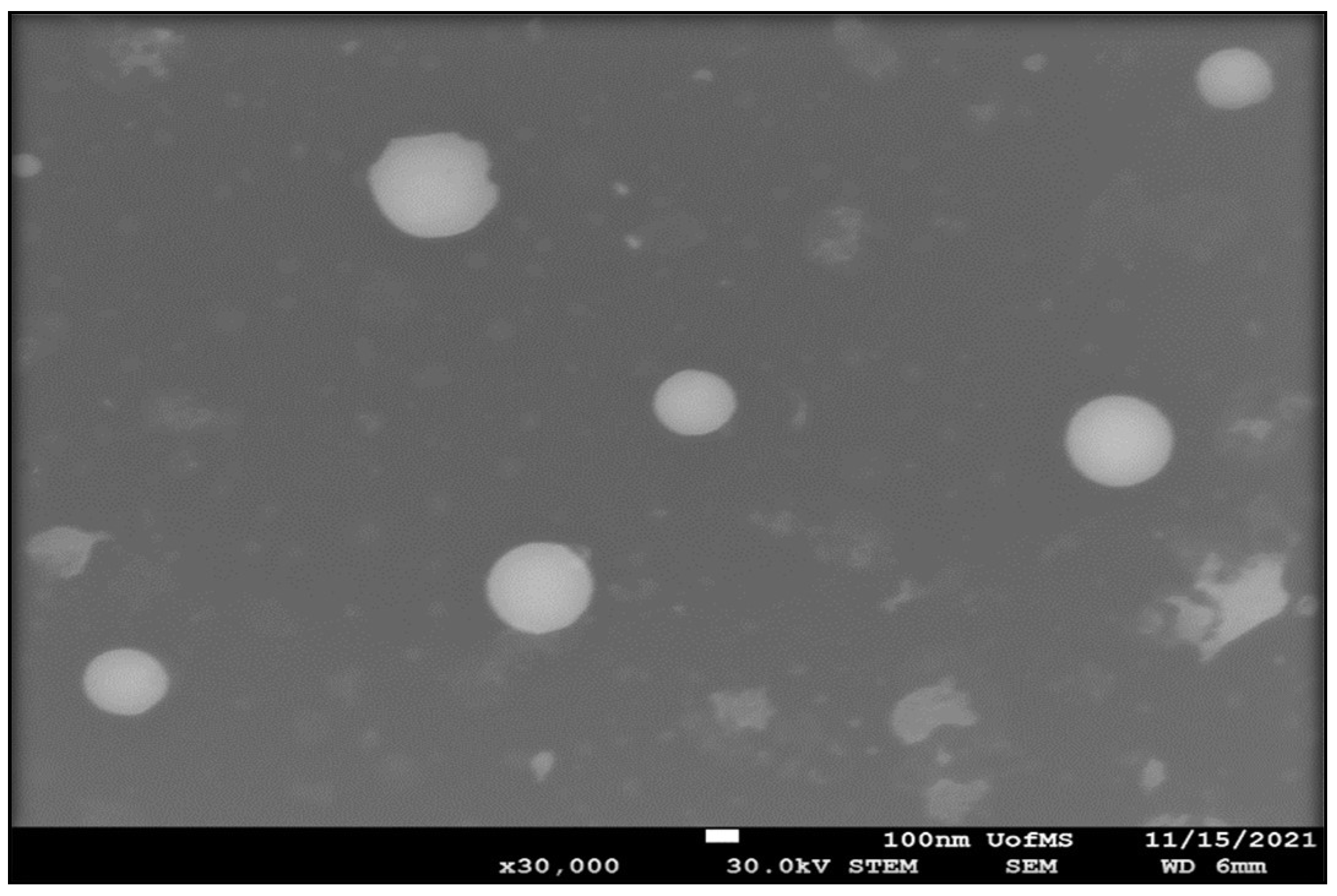
2.2.10. Scanning Transmission Electron Microscopy (STEM)
2.2.11. In Vivo Single Dose Efficacy Studies—IOP Measurement
2.2.12. Statistical Analysis
3. Results and Discussion
3.1. Formulation Development
3.2. Physicochemical Characteristics of CBD-NE and CBD-NEC Formulations
3.3. pH and Viscosity
3.4. STEM
3.5. Stability Studies
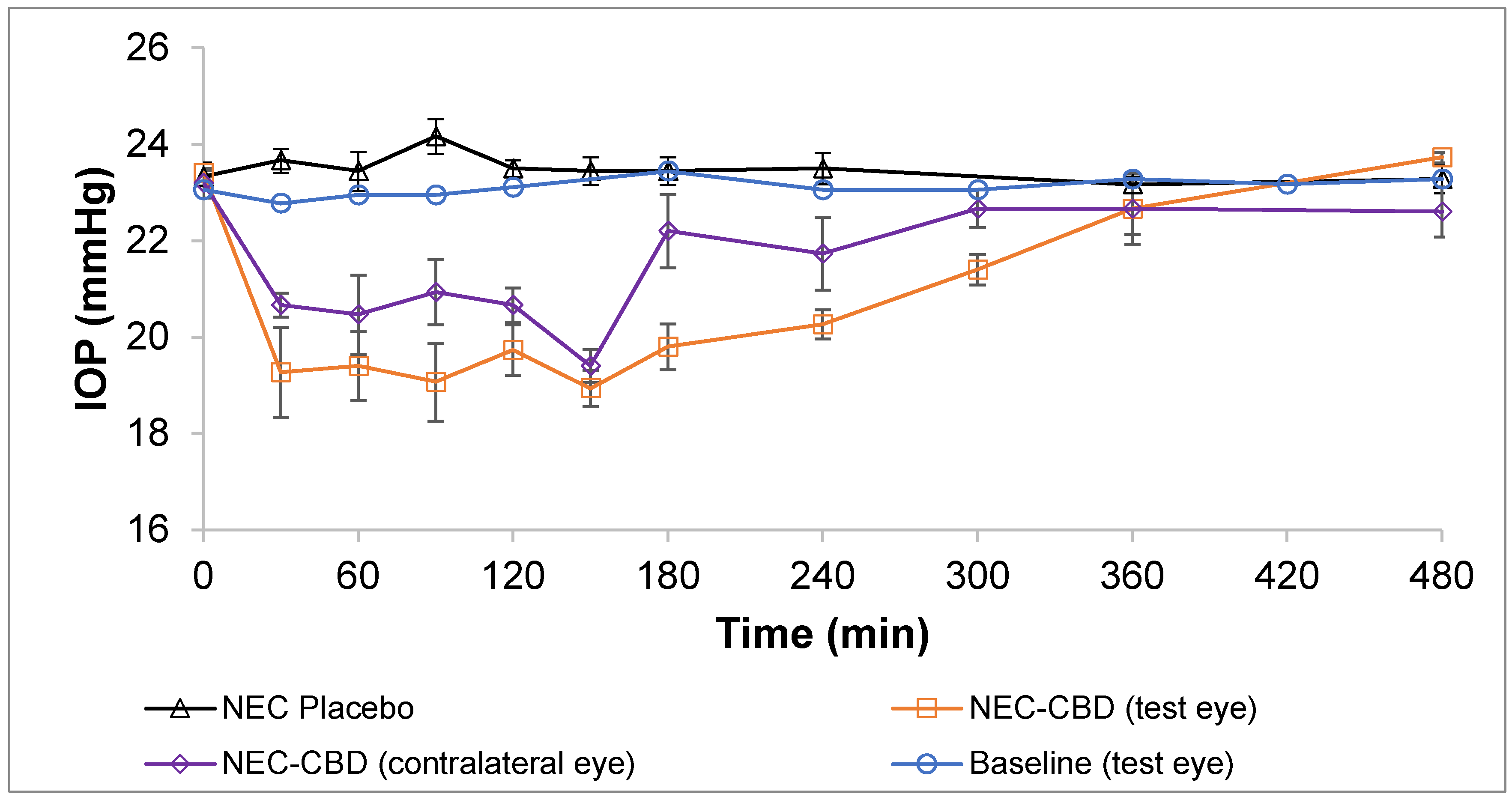
3.6. In Vivo Single-Dose Efficacy Studies—IOP Measurement
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Radwan, M.M.; ElSohly, M.A.; Slade, D.; Ahmed, S.A.; Khan, I.A.; Ross, S.A. Biologically Active Cannabinoids from High-Potency Cannabis Sativa. J. Nat. Prod. 2009, 72, 906–911. [Google Scholar] [CrossRef]
- De Almeida, D.L.; Devi, L.A. Diversity of Molecular Targets and Signaling Pathways for CBD. Pharmacol. Res. Perspect. 2020, 8, e00682. [Google Scholar] [CrossRef]
- El-Remessy, A.B.; Al-Shabrawey, M.; Khalifa, Y.; Tsai, N.-T.; Caldwell, R.B.; Liou, G.I. Neuroprotective and Blood-Retinal Barrier-Preserving Effects of Cannabidiol in Experimental Diabetes. Am. J. Pathol. 2006, 168, 235–244. [Google Scholar] [CrossRef]
- Liou, G.I.; Auchampach, J.A.; Hillard, C.J.; Zhu, G.; Yousufzai, B.; Mian, S.; Khan, S.; Khalifa, Y. Mediation of Cannabidiol Anti-Inflammation in the Retina by Equilibrative Nucleoside Transporter and A2A Adenosine Receptor. Investig. Ophthalmol. Vis. Sci. 2008, 49, 5526–5531. [Google Scholar] [CrossRef]
- Green, K.; Symonds, C.M.; Oliver, N.W.; Elijah, R.D. Intraocular Pressure Following Systemic Administration of Cannabinoids. Curr. Eye Res. 1982, 2, 247–253. [Google Scholar] [CrossRef]
- Elsohly, M.A.; Harland, E.C.; Benigni, D.A.; Waller, C.W. Cannabinoids in Glaucoma II: The Effect of Different Cannabinoids on Intraocular Pressure of the Rabbit. Curr. Eye Res. 1984, 3, 841–850. [Google Scholar] [CrossRef]
- Liu, J.H.; Dacus, A.C. Central Nervous System and Peripheral Mechanisms in Ocular Hypotensive Effect of Cannabinoids. Arch. Ophthalmol. 1987, 105, 245–248. [Google Scholar] [CrossRef]
- Green, K.; Wynn, H.; Bowman, K.A. A Comparison of Topical Cannabinoids on Intraocular Pressure. Exp. Eye Res. 1978, 27, 239–246. [Google Scholar] [CrossRef]
- Colasanti, B.K.; Powell, S.R.; Craig, C.R. Intraocular Pressure, Ocular Toxicity and Neurotoxicity after Administration of Δ9-Tetrahydrocannabinol or Cannabichromene. Exp. Eye Res. 1984, 38, 63–71. [Google Scholar] [CrossRef]
- Grotenhermen, F. Clinical Pharmacokinetics of Cannabinoids. J. Cannabis Ther. 2003, 3, 3–51. [Google Scholar] [CrossRef]
- Tomida, I.; Azuara-Blanco, A.; House, H.; Flint, M.; Pertwee, R.G.; Robson, P.J. Effect of Sublingual Application of Cannabinoids on Intraocular Pressure: A Pilot Study. J. Glaucoma 2006, 15, 349–353. [Google Scholar] [CrossRef]
- Miller, S.; Daily, L.; Leishman, E.; Bradshaw, H.; Straiker, A. Δ9-Tetrahydrocannabinol and Cannabidiol Differentially Regulate Intraocular Pressure. Investig. Ophthalmol. Vis. Sci. 2018, 59, 5904–5911. [Google Scholar] [CrossRef]
- Rebibo, L.; Frušić-Zlotkin, M.; Ofri, R.; Nassar, T.; Benita, S. The Dose-Dependent Effect of a Stabilized Cannabidiol Nanoemulsion on Ocular Surface Inflammation and Intraocular Pressure. Int. J. Pharm. 2022, 617, 121627. [Google Scholar] [CrossRef]
- Vallée, A.; Lecarpentier, Y.; Vallée, J.-N. Cannabidiol and the Canonical WNT/β-Catenin Pathway in Glaucoma. Int. J. Mol. Sci. 2021, 22, 3798. [Google Scholar] [CrossRef]
- Straiker, A.; Miller, S. Δ9-THC and CBD Differentially Regulate Intraocular Pressure. Investig. Ophthalmol. Vis. Sci. 2018, 59, 6040. [Google Scholar]
- Taskar, P.; Adelli, G.; Patil, A.; Lakhani, P.; Ashour, E.; Gul, W.; ElSohly, M.; Majumdar, S. Analog Derivatization of Cannabidiol for Improved Ocular Permeation. J. Ocul. Pharmacol. Ther. 2019, 35, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Taskar, P.S.; Patil, A.; Lakhani, P.; Ashour, E.; Gul, W.; ElSohly, M.A.; Murphy, B.; Majumdar, S. Δ9-Tetrahydrocannabinol Derivative-Loaded Nanoformulation Lowers Intraocular Pressure in Normotensive Rabbits. Trans. Vis. Sci. Tech. 2019, 8, 15. [Google Scholar] [CrossRef]
- Adelli, G.R.; Bhagav, P.; Taskar, P.; Hingorani, T.; Pettaway, S.; Gul, W.; ElSohly, M.A.; Repka, M.A.; Majumdar, S. Development of a Δ9-Tetrahydrocannabinol Amino Acid-Dicarboxylate Prodrug with Improved Ocular Bioavailability. Investig. Ophthalmol. Vis. Sci 2017, 58, 2167–2179. [Google Scholar] [CrossRef]
- Hingorani, T.; Adelli, G.R.; Punyamurthula, N.; Gul, W.; ElSohly, M.A.; Repka, M.A.; Majumdar, S. Ocular Disposition of the Hemiglutarate Ester Prodrug of ∆9-Tetrahydrocannabinol from Various Ophthalmic Formulations. Pharm. Res. 2013, 30, 2146–2156. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, C.; Dudhipala, N.; Thakkar, R.; Mehraj, T.; Marathe, S.; Gul, W.; ElSohly, M.A.; Murphy, B.; Majumdar, S. Impact of Mucoadhesive Agent Inclusion on the Intraocular Pressure Lowering Profile of Δ9-Tetrahydrocannabinol-Valine-Hemisuccinate Loaded Nanoemulsions in New Zealand White Rabbits. Int. J. Pharm. 2022, 616, 121564. [Google Scholar] [CrossRef]
- Sweeney, C.; Dudhipala, N.; Thakkar, R.; Mehraj, T.; Marathe, S.; Gul, W.; ElSohly, M.A.; Murphy, B.; Majumdar, S. Effect of Surfactant Concentration and Sterilization Process on Intraocular Pressure–Lowering Activity of Δ9-Tetrahydrocannabinol-Valine-Hemisuccinate (NB1111) Nanoemulsions. Drug Deliv. Transl. Res. 2021, 11, 2096–2107. [Google Scholar] [CrossRef]
- Youssef, A.A.A.; Cai, C.; Dudhipala, N.; Majumdar, S. Design of Topical Ocular Ciprofloxacin Nanoemulsion for the Management of Bacterial Keratitis. Pharmaceuticals 2021, 14, 210. [Google Scholar] [CrossRef] [PubMed]
- Youssef, A.A.A.; Thakkar, R.; Senapati, S.; Joshi, P.H.; Dudhipala, N.; Majumdar, S. Design of Topical Moxifloxacin Mucoadhesive Nanoemulsion for the Management of Ocular Bacterial Infections. Pharmaceutics 2022, 14, 1246. [Google Scholar] [CrossRef] [PubMed]
- Tatke, A.; Dudhipala, N.; Janga, K.Y.; Balguri, S.P.; Avula, B.; Jablonski, M.M.; Majumdar, S. In Situ Gel of Triamcinolone Acetonide-Loaded Solid Lipid Nanoparticles for Improved Topical Ocular Delivery: Tear Kinetics and Ocular Disposition Studies. Nanomaterials 2019, 9, 33. [Google Scholar] [CrossRef]
- Youssef, A.A.A.; Dudhipala, N.; Majumdar, S. Dual Drug Loaded Lipid Nanocarrier Formulations for Topical Ocular Applications. IJN 2022, 17, 2283–2299. [Google Scholar] [CrossRef] [PubMed]
- Youssef, A.; Dudhipala, N.; Majumdar, S. Ciprofloxacin Loaded Nanostructured Lipid Carriers Incorporated into In-Situ Gels to Improve Management of Bacterial Endophthalmitis. Pharmaceutics 2020, 12, 572. [Google Scholar] [CrossRef]
- Marathe, S.; Shadambikar, G.; Mehraj, T.; Sulochana, S.P.; Dudhipala, N.; Majumdar, S. Development of α-Tocopherol Succinate-Based Nanostructured Lipid Carriers for Delivery of Paclitaxel. Pharmaceutics 2022, 14, 1034. [Google Scholar] [CrossRef] [PubMed]
- Lallemand, F.; Daull, P.; Benita, S.; Buggage, R.; Garrigue, J.-S. Successfully Improving Ocular Drug Delivery Using the Cationic Nanoemulsion, Novasorb. J. Drug Deliv. 2012, 2012, 604204. [Google Scholar] [CrossRef]
- Singh, M.; Bharadwaj, S.; Lee, K.E.; Kang, S.G. Therapeutic Nanoemulsions in Ophthalmic Drug Administration: Concept in Formulations and Characterization Techniques for Ocular Drug Delivery. J. Control. Release 2020, 328, 895–916. [Google Scholar] [CrossRef] [PubMed]
- Ammar, H.O.; Salama, H.A.; Ghorab, M.; Mahmoud, A.A. Nanoemulsion as a Potential Ophthalmic Delivery System for Dorzolamide Hydrochloride. AAPS PharmSciTech 2009, 10, 808–819. [Google Scholar] [CrossRef] [PubMed]
- Naik, J.B.; Pardeshi, S.R.; Patil, R.P.; Patil, P.B.; Mujumdar, A. Mucoadhesive Micro-/Nano Carriers in Ophthalmic Drug Delivery: An Overview. BioNanoScience 2020, 10, 564–582. [Google Scholar] [CrossRef]
- Abelson, M.B.; Udell, I.J.; Weston, J.H. Normal Human Tear PH by Direct Measurement. Arch. Ophthalmol. 1981, 99, 301. [Google Scholar] [CrossRef]
- Ban, M.M.; Chakote, V.R.; Dhembre, G.N.; Rajguru, J.R.; Joshi, D.A. In-Situ Gel for Nasal Drug Delivery. Int. J. Dev. Res. 2018, 8, 18763–18769. [Google Scholar]
- Dhahir, R.K.; Al-Nima, A.M.; Yassir Al-bazzaz, F. Nanoemulsions as Ophthalmic Drug Delivery Systems. Turk. J. Pharm. Sci. 2021, 18, 652–664. [Google Scholar] [CrossRef]
- Lin, L.; Gu, Y.; Cui, H. Moringa Oil/Chitosan Nanoparticles Embedded Gelatin Nanofibers for Food Packaging against Listeria Monocytogenes and Staphylococcus Aureus on Cheese. Food Packag. Shelf Life 2019, 19, 86–93. [Google Scholar] [CrossRef]
- Mitri, K.; Shegokar, R.; Gohla, S.; Anselmi, C.; Müller, R.H. Lipid Nanocarriers for Dermal Delivery of Lutein: Preparation, Characterization, Stability and Performance. Int. J. Pharm. 2011, 414, 267–275. [Google Scholar] [CrossRef]
- Uddin, M.S.; Mamun, A.A.; Kabir, M.T.; Setu, J.R.; Zaman, S.; Begum, Y.; Amran, M.S. Quality Control Tests for Ophthalmic Pharmaceuticals: Pharmacopoeial Standards and Specifications. J. Adv. Med. Pharm. Sci. 2017, 14, 1–17. [Google Scholar] [CrossRef]
- Rai, V.K.; Mishra, N.; Yadav, K.S.; Yadav, N.P. Nanoemulsion as Pharmaceutical Carrier for Dermal and Transdermal Drug Delivery: Formulation Development, Stability Issues, Basic Considerations and Applications. J. Control. Release 2018, 270, 203–225. [Google Scholar] [CrossRef] [PubMed]
- Komaiko, J.S.; McClements, D.J. Formation of Food-Grade Nanoemulsions Using Low-Energy Preparation Methods: A Review of Available Methods. Compr. Rev. Food Sci. Food Saf. 2016, 15, 331–352. [Google Scholar] [CrossRef]
- Mishra, N.; Yadav, K.S.; Rai, V.K.; Yadav, N.P. Polysaccharide Encrusted Multilayered Nano-Colloidal System of Andrographolide for Improved Hepatoprotection. AAPS PharmSciTech 2017, 18, 381–392. [Google Scholar] [CrossRef]
- Santos, J.; Calero, N.; Trujillo-Cayado, L.A.; Martín-Piñero, M.J.; Muñoz, J. Processing and Formulation Optimization of Mandarin Essential Oil-Loaded Emulsions Developed by Microfluidization. Materials 2020, 13, 3486. [Google Scholar] [CrossRef]
- Griffin, W.C. Calculation of HLB Values of Non-Ionic Surfactants. J. Soc. Cosmet. Chem. 1954, 5, 249–256. [Google Scholar]
- Kiel, J.W.; Kopczynski, C.C. Effect of AR-13324 on episcleral venous pressure in Dutch belted rabbits. J. Ocul. Pharmacol. Ther. 2015, 31, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.-R.; Huang, S.-W.; Cui, J.-Z.; Yoshitomi, T. Effects of Brinzolamide on Rabbit Ocular Blood Flow in Vivo and Ex Vivo. Int. J. Ophthalmol. 2018, 11, 719. [Google Scholar]
- Rao, H.L.; Senthil, S.; Garudadri, C.S. Contralateral Intraocular Pressure Lowering Effect of Prostaglandin Analogues. Indian J. Ophthalmol. 2014, 62, 575–579. [Google Scholar] [CrossRef]
- Piltz, J.; Gross, R.; Shin, D.H.; Beiser, J.A.; Dorr, D.A.; Kass, M.A.; Gordon, M.O. Contralateral Effect of Topical β-Adrenergic Antagonists in Initial One-Eyed Trials in the Ocular Hypertension Treatment Study. Am. J. Ophthalmol. 2000, 130, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Dunham, C.N.; Spaide, R.F.; Dunham, G. The Contralateral Reduction of Intraocular Pressure by Timolol. Br. J. Ophthalmol. 1994, 78, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Arfaee, F.; Armin, A. A Comparison between the Effect of Topical Tafluprost and Latanoprost on Intraocular Pressure in Healthy Male Guinea Pigs. J. Exot. Pet Med. 2021, 39, 91–95. [Google Scholar] [CrossRef]
- Aihara, M.; Lindsey, J.D.; Weinreb, R.N. Reduction of Intraocular Pressure in Mouse Eyes Treated with Latanoprost. Investig. Ophthalmol. Vis. Sci. 2002, 43, 146–150. [Google Scholar]
- Ota, T.; Murata, H.; Sugimoto, E.; Aihara, M.; Araie, M. Prostaglandin Analogues and Mouse Intraocular Pressure: Effects of Tafluprost, Latanoprost, Travoprost, and Unoprostone, Considering 24-Hour Variation. Investig. Ophthalmol. Vis. Sci. 2005, 46, 2006–2011. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Weinreb, R.N.; Lindsey, J.D. The Importance of Models in Glaucoma Research. J. Glaucoma 2005, 14, 302–304. [Google Scholar] [CrossRef]
- Kim, C.Y.; Kuehn, M.H.; Anderson, M.G.; Kwon, Y.H. Intraocular Pressure Measurement in Mice: A Comparison between Goldmann and Rebound Tonometry. Eye 2007, 21, 1202–1209. [Google Scholar] [CrossRef]
| Ingredients (% w/v) | Formulations | |
|---|---|---|
| CBD-NE | CBD-NEC | |
| CBD | 1.0 | 1.0 |
| Sesame oil NF | 5.0 | 5.0 |
| Tween® 80 NF | 2.0 | 2.0 |
| Poloxamer 407 NF | 0.2 | 0.2 |
| Glycerin NF | 2.25 | 2.25 |
| Carbopol® 940 NF | – | 0.4 |
| TPGS | 0.002 | 0.002 |
| Milli-Q water q.s (mL) | 10 | 10 |
| Parameter | Formulation | |
|---|---|---|
| CBD-NE | CBD-NEC | |
| Globule size (d. nm) | 167.2 ± 4.2 | 259.5 ± 2.0 |
| Polydispersity index | 0.20 ± 0.01 | 0.27 ± 0.01 |
| Zeta potential (mV) | −19.8 ± 1.1 | −37.9 ± 0.8 |
| Drug content (%) | 100.0 ± 0.3 | 101.9 ± 0.1 |
| pH | 5.6 ± 0.02 | 3.6 ± 0.02 |
| Viscosity (cP) without STF | 11.6 ± 0.5 | 23.2 ± 0.4 |
| Viscosity (cP) with STF | 12.3 ± 1.0 | 31.2 ± 1.2 |
| Formulation | Day | Storage at 4 ± 2 °C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| DS (d, nm) | PDI | ZP (mV) | pH | Drug Content (%) | |||||||
| Sterilization Stage | |||||||||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | ||
| CBD-NE | 0 | 167.2 ± 4.2 | 167.9 ± 2.0 | 0.20 ± 0.01 | 0.21 ± 0.02 | −19.8 ± 1.1 | −21.6 ± 0.2 | 5.60 ± 0.02 | 5.62 ± 0.01 | 100.0 ± 0.3 | 97.0 ± 0.2 |
| 30 | 166.0 ± 3.7 | 163.6 ± 2.6 | 0.20 ± 0.02 | 0.23 ± 0.01 | −21.7 ± 0.5 | −20.6 ± 0.4 | 5.60 ± 0.02 | 5.64 ± 0.02 | 99.5 ± 2.1 | 99.0 ± 0.5 | |
| CBD-NEC | 0 | 259.5 ± 2.0 | 258.5 ± 0.4 | 0.26 ± 0.01 | 0.25 ± 0.02 | −33.9 ± 0.8 | −34.7 ± 0.3 | 3.60 ± 0.01 | 3.59 ± 0.03 | 101.9 ± 0.1 | 98.2 ± 0.3 |
| 30 | 252.9 ± 2.8 | 251.7 ± 3.7 | 0.25 ± 0.01 | 0.26 ± 0.01 | −35.2 ± 0.2 | −33.6 ± 0.4 | 3.60 ± 0.01 | 3.65 ± 0.01 | 101.9 ± 1.4 | 102.6 ± 1.5 | |
| Storage at 25 ± 2 °C | |||||||||||
| CBD-NE | 0 | 165.7 ± 1.8 | 166.4 ± 2.0 | 0.21 ± 0.01 | 0.22 ± 0.01 | −19.8 ± 0.9 | −21.6 ± 0.8 | 5.62 ± 0.02 | 5.63 ± 0.01 | 99.8 ± 0.1 | 97.0 ± 0.1 |
| 30 | 164.9 ± 1.0 | 161.9 ± 3.0 | 0.22 ± 0.01 | 0.22 ± 0.02 | −21.2 ± 0.3 | −20 ± 0.6 | 5.64 ± 0.02 | 5.62 ± 0.01 | 98.2 ± 1.7 | 97.6 ± 0.6 | |
| CBD-NEC | 0 | 262.9 ± 1.3 | 259.4 ± 0.8 | 0.25 ± 0.02 | 0.24 ± 0.02 | −34.3 ± 2.1 | −35.7 ± 0.8 | 3.61 ± 0.01 | 3.60 ± 0.02 | 100.8 ± 0.1 | 101.0 ± 0.1 |
| 30 | 256.8 ± 4.7 | 256.1 ± 0.8 | 0.26 ± 0.01 | 0.26 ± 0.01 | −35.8 ± 0.6 | −34.3 ± 0.8 | 3.64 ± 0.01 | 3.65 ± 0.02 | 100.2 ± 2.0 | 99.6 ± 2.1 | |
| Storage at 40 ± 2 °C | |||||||||||
| CBD-NE | 0 | 166.8 ± 2.2 | 170.2 ± 2.4 | 0.19 ± 0.01 | 0.21 ± 0.01 | −21.2 ± 0.5 | −19.6 ± 0.3 | 5.55 ± 0.01 | 5.64 ± 0.02 | 99.6 ± 0.1 | 98.0 ± 0.3 |
| 30 | 160.9 ± 2.0 | 162.2 ± 2.6 | 0.21 ± 0.01 | 0.21 ± 0.00 | −20.8 ± 0.6 | −20.6 ± 0.5 | 5.58 ± 0.01 | 5.62 ± 0.01 | 100.3 ± 3.1 | 99.8 ± 0.2 | |
| CBD-NEC | 0 | 263.1 ± 1.8 | 256.9 ± 2.9 | 0.24 ± 0.03 | 0.25 ± 0.01 | −34.4 ± 2.1 | −35.4 ± 0.3 | 3.60 ± 0.03 | 3.62 ± 0.01 | 99.9 ± 0.2 | 101.6 ± 0.5 |
| 30 | 254.9 ± 4.0 | 254.7 ± 1.8 | 0.25 ± 0.01 | 0.26 ± 0.01 | −34.6 ± 1.6 | −36.2 ± 0.8 | 3.64 ± 0.01 | 3.65 ± 0.03 | 102.9 ± 0.3 | 102.4 ± 1.2 | |
| Time Point (min) | CBD-NEC Treated Eye vs. NEC-Placebo | CBD-NEC Treated Eye vs. CBD-NEC Contralateral Eye | CBD-NEC Treated Eye vs. Baseline Treated Eye | CBD-NEC Contralateral Eye vs. Baseline Treated Eye |
|---|---|---|---|---|
| p-Value | p-Value | p-Value | p-Value | |
| 0 | 0.211 | 0.625 | 1.000 | 1.000 |
| 30 | 0.003 | 0.235 | 0.005 | <0.001 |
| 60 | 0.003 | 0.397 | 0.001 | 0.024 |
| 90 | <0.001 | 0.155 | 0.001 | 0.024 |
| 120 | <0.001 | 0.226 | <0.001 | 0.001 |
| 150 | <0.001 | 0.431 | <0.001 | <0.001 |
| 180 | <0.001 | 0.045 | <0.001 | 0.309 |
| 240 | <0.001 | 0.144 | <0.001 | 0.149 |
| 300 | – | 0.051 | <0.001 | 0.356 |
| 360 | 0.566 | 1.000 | 0.271 | 0.564 |
| 480 | 0.323 | 0.088 | 0.045 | 0.396 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Senapati, S.; Youssef, A.A.A.; Sweeney, C.; Cai, C.; Dudhipala, N.; Majumdar, S. Cannabidiol Loaded Topical Ophthalmic Nanoemulsion Lowers Intraocular Pressure in Normotensive Dutch-Belted Rabbits. Pharmaceutics 2022, 14, 2585. https://doi.org/10.3390/pharmaceutics14122585
Senapati S, Youssef AAA, Sweeney C, Cai C, Dudhipala N, Majumdar S. Cannabidiol Loaded Topical Ophthalmic Nanoemulsion Lowers Intraocular Pressure in Normotensive Dutch-Belted Rabbits. Pharmaceutics. 2022; 14(12):2585. https://doi.org/10.3390/pharmaceutics14122585
Chicago/Turabian StyleSenapati, Samir, Ahmed Adel Ali Youssef, Corinne Sweeney, Chuntian Cai, Narendar Dudhipala, and Soumyajit Majumdar. 2022. "Cannabidiol Loaded Topical Ophthalmic Nanoemulsion Lowers Intraocular Pressure in Normotensive Dutch-Belted Rabbits" Pharmaceutics 14, no. 12: 2585. https://doi.org/10.3390/pharmaceutics14122585
APA StyleSenapati, S., Youssef, A. A. A., Sweeney, C., Cai, C., Dudhipala, N., & Majumdar, S. (2022). Cannabidiol Loaded Topical Ophthalmic Nanoemulsion Lowers Intraocular Pressure in Normotensive Dutch-Belted Rabbits. Pharmaceutics, 14(12), 2585. https://doi.org/10.3390/pharmaceutics14122585







